Key Teaching Points.
-
•
Left bundle branch block or delay can occur within fibers that are predestined to become the left bundle branch in the bundle of His. This is the concept of longitudinal dissociation within the His bundle.
-
•
In such cases, permanent His bundle pacing can overcome this delay and normalize the QRS duration.
-
•
It is possible in rare and well-mapped cases to demonstrate this intra-Hisian delay during His bundle pacing lead implantation.
Introduction
Narrowing of the QRS and overcoming left bundle branch block (LBBB) with His bundle pacing (HBP) has been previously described.1, 2, 3 We present the first 2 reported cases of left bundle branch (LBB) delay with evidence of a split His electrogram during unipolar mapping from the tip of the His bundle (HB) lead during pacemaker implantation. These findings suggest that the site of LBB delay is intra-Hisian, thus further validating the theory of “longitudinal dissociation in the HB.”1
Case report
Case 1
The patient is a 94-year-old woman with ischemic cardiomyopathy and declining left ventricular ejection fraction (LVEF) despite optimal medical management. Over the past year her LVEF decreased from 35% to 20%, correlating with progression to NYHA class III heart failure. Her electrocardiogram was notable for a wide LBBB of 164 ms and she was referred for cardiac resynchronization therapy (CRT).
She was felt to be a reasonable candidate for CRT; however, given her advanced age and comorbidities a decision was made to consider a CRT pacemaker and not a CRT defibrillator. Owing to the patient’s frail stature without appreciable pectoral muscle, a decision was made to attempt resynchronization by placing the ventricular lead at the HB. We hoped to recruit the LBB and implant a smaller dual-chamber pacemaker generator.
The HB was mapped using unipolar recordings from a Medtronic 3830 lead (Medtronic Inc, Minneapolis, MN) through a His C315 sheath. HB recordings and pace mapping at different HB sites are shown in Figure 1. The final location of the HB lead resulted in nonselective HBP with recruitment of the LBBB and narrowing of the QRS to 90 ms. Total procedure time was 113 minutes and fluoroscopy time was 8.4 minutes.
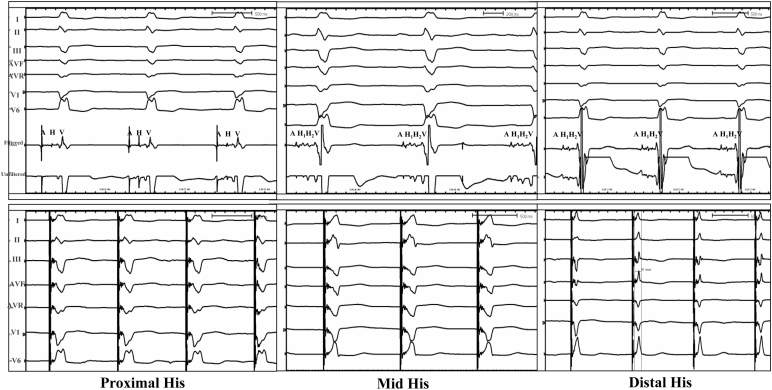
Figure 1.
Unipolar recordings from the lead tip at different sites the His bundle region. Top panel with unipolar recordings (filtered and unfiltered electrograms) from the His bundle pacing lead using alligator cables. As noted, mid and distal His electrograms reveal a split His electrogram. The bottom panel represents paced QRS morphologies at the respective mapped sites.
Case 2
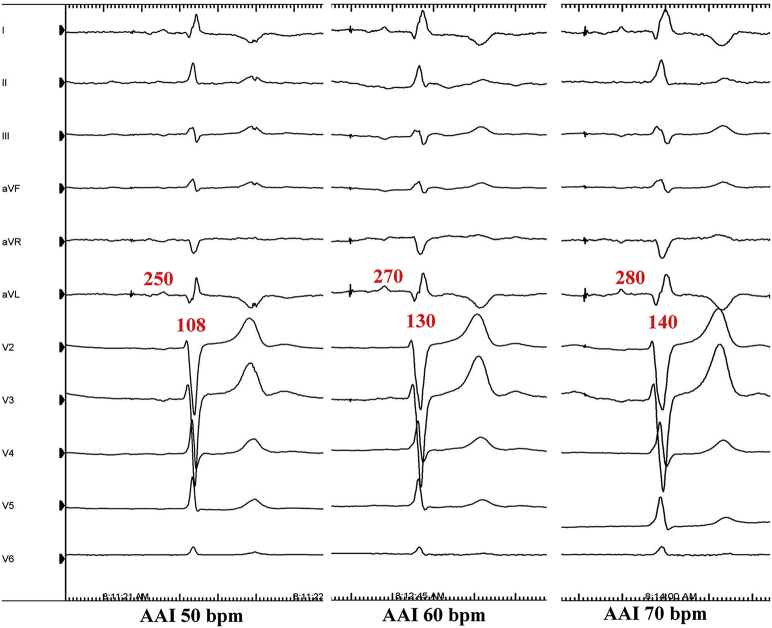
A 79-year-old man with a history of hypertension and type II diabetes was admitted with dizziness and fatigue. These episodes correlated with significant sinus bradycardia and junctional rhythm in the 30s. He was also noted to have a rate-related delay in the LBB at 60 beats per minute (bpm). A decision was made to implant a dual-chamber pacemaker for highly symptomatic sinus node dysfunction. Given the LBBB, we also planned for an HBP lead implant with an attempt to recruit the LBB delay.
We started with implantation of the atrial lead so as to unmask the rate-related delay in LBB. AAI pacing at different rates showed progressive delay in the LBB (Supplemental Figure 1). The HB was mapped using unipolar recordings from a Medtronic 3830 lead (Medtronic Inc, Minneapolis, MN) through a His C315 sheath. Figure 2 demonstrates HB recordings and pace mapping (5 V at 1 ms) at different HB sites. The final location of the HB lead resulted in selective HBP with recruitment of the LBBB and narrowing of the QRS to 90 ms. Total procedure time was 105 minutes and fluoroscopy time was 7 minutes.
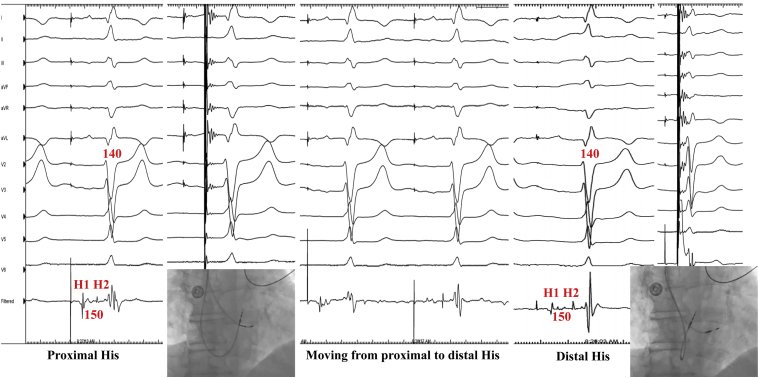
Figure 2.
Unipolar recordings and pacing from the lead tip at different sites in the His bundle (HB) region. Proximal HB electrograms demonstrate a split HB (H1-H2 of 150 ms). Right anterior oblique fluoroscopic view demonstrates location of the tip electrode. Pacing at this site demonstrates a similar QRS with left bundle branch (LBB) delay. Moving from proximal to distal HB position results in a distal site that in 0.5 ms more distal fluoroscopically, with a larger distal HB electrogram. Pacing at this site results in narrowing of the QRS and loss of LBB delay. There is no local ventricular capture, suggesting selective HB capture and LBB recruitment.
Discussion
We present 2 patients with a wide LBBB in whom unipolar mapping from the HB pacing lead identified a split His potential. Pacing at a site distal to the split His recruited the LB. This suggests that the level of block/delay in the left bundle was likely within the HB in fibers that were predestined to the LB.
In case 1, Figure 1 demonstrates proximal, mid, and distal HB recordings with corresponding paced morphologies (5 V at 1 ms). The mid and distal recordings revealed a split His potential, suggesting intra-Hisian disease as the possible site of the LBBB or left bundle delay. Pacing from the distal His site resulted in both capture of the HB and local right ventricular capture (nonselective HB capture) and successful recruitment of intra-Hisian LBBB (Figure 1). Distal HBP provided successful CRT with a narrowing of the QRS from 164 ms to 90 ms. HBP resulted in normalization of LVEF to 55% and clinical improvement to NYHA class I.
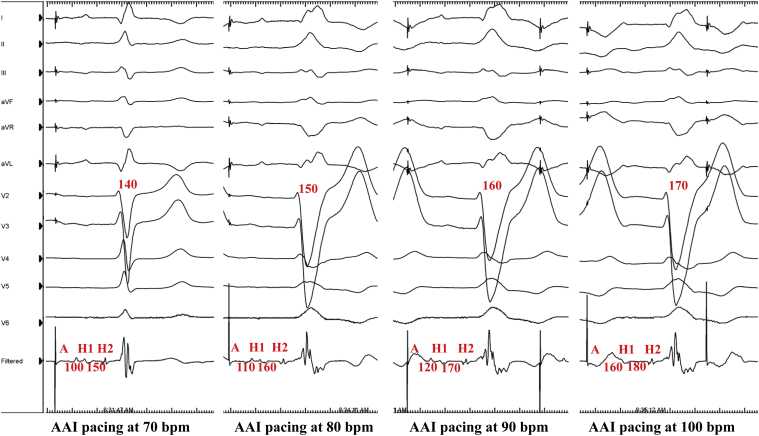
Case 2 demonstrates a patient with a rate-related LBB delay who was noted to have a split HB electrogram with a wide separation (H1-H2 interval of 150 ms at 60 bpm, Figure 2) during HB mapping from the tip of the pace/sense lead. As seen in Figure 3, pacing the atrium at faster rates (from AAI 70 bpm to 100 bpm) resulted not only in A-H1 prolongation (representing normal atrioventricular nodal physiology), but also in a prolongation of H1-H2 interval from 150 ms to 180 ms. This increase in H1-H2 intervals corresponded precisely with a progressive delay in the LBBB and QRS prolongation from 140 ms to 170 ms, suggesting that the delay was within the His bundle. Pacing at the distal HB (H2) resulted in complete recruitment of LBB delay (Figure 2) and normalization of the QRS duration, confirming the intra-His site of delay.
Figure 3.
AAI pacing at incremental rates with progressive intra-His and left bundle branch (LBB) delay. Similar to Figure 2, there is progressive prolongation in LBB (140 ms to 170 ms). Note the prolongation in H1-H2 intervals (from 150 ms to 180 ms) suggestive of intra-Hisian LBB delay.
The normalization of bundle branch block by distal HBP was first reported in the 1970s by Narula.1 HB pacing has also been shown to provide pacing support for heart failure patients with and without LBBB heart failure.2, 4 The ability to recruit the left bundle with pacing at the distal HB supports the concept of functional longitudinal dissociation in the HB. Previous studies on permanent HB pacing validate this concept.3, 5, 6 The postulated mechanisms for this recruitment of branches are as follows: (1) longitudinal dissociation in the HB with pacing distal to the site of delay/block, and/or (2) differential source-sink relationships during pacing vs intrinsic impulse propagation, and/or (3) virtual electrode polarization effect.6
These cases support the theory of longitudinal dissociation in the HB and provide the first documentation of the ability to record a split His potential using an HB permanent pacing lead.
Footnotes
Disclosures: Dr Sharma: honoraria: Medtronic Inc; Dr Trohman: advisor: Boston Scientific/Guidant; research grants: Boston Scientific, Medtronic Inc, St Jude Medical, Vitatron, and WyethAyerst/Wyeth Pharmaceuticals; consultant: Biosense Webster and St Jude Medical; and honoraria from Boston Scientific/Guidant CRM, Medtronic Inc, Daiichi Sankyo, and St Jude Medical.
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.hrcr.2017.02.003.
Appendix. Supplementary data
Supplemental Figure 1.
Pacing the atrial lead to unmask left bundle branch (LBB) delay. AAI pacing in the atrial lead from 50 to 70 beats per minute demonstrates progressive prolongation of A-V interval (250 ms to 280 ms) and corresponding prolongation in LBB delay (108 ms to 140 ms).
References
- 1.Narula O.S. Longitudinal dissociation in the His bundle. Bundle branch block due to asynchronous conduction within the His bundle in man. Circulation. 1977;56:996–1006. doi: 10.1161/01.cir.56.6.996. [DOI] [PubMed] [Google Scholar]
- 2.Barba-Pichardo R., Manovel Sanchez A., Fernandez-Gomez J.M., Morina-Vazquez P., Venegas-Gamero J., Herrera-Carranza M. Ventricular resynchronization therapy by direct His-bundle pacing using an internal cardioverter defibrillator. Europace. 2013;15:83–88. doi: 10.1093/europace/eus228. [DOI] [PubMed] [Google Scholar]
- 3.Vijayaraman P., Sharma P.S., Koneru J.N., Ellenbogen K.A., Dandamudi G. 2015. Chronic bundle branch blocks are due to longitudinal dissociation in the main His bundle: electrophysiological observations from correction of BBB by permanent His bundle pacing. Heart Rhythm Society Annual Scientific Sessions. San Francisco. 12 Suppl S. [Google Scholar]
- 4.Deshmukh P., Casavant D.A., Romanyshyn M., Anderson K. Permanent, direct His-bundle pacing: a novel approach to cardiac pacing in patients with normal His-Purkinje activation. Circulation. 2000;101:869–877. doi: 10.1161/01.cir.101.8.869. [DOI] [PubMed] [Google Scholar]
- 5.Lustgarten D.L., Crespo E.M., Arkhipova-Jenkins I., Lobel R., Winget J., Koehler J., Liberman E., Sheldon T. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: a crossover design comparison. Heart Rhythm. 2015;12:1548–1557. doi: 10.1016/j.hrthm.2015.03.048. [DOI] [PubMed] [Google Scholar]
- 6.Sharma P.S., Huizar J., Ellenbogen K.A., Tan A.Y. Recruitment of bundle branches with permanent His bundle pacing in a patient with advanced conduction system disease: what is the mechanism? Heart Rhythm. 2016;13:623–625. doi: 10.1016/j.hrthm.2015.11.012. [DOI] [PubMed] [Google Scholar]