Introduction
His bundle pacing is gaining popularity in patients receiving cardiac resynchronization therapy (CRT) devices.1, 2 The present case highlights a unique challenge in patients with a His bundle lead in the left ventricular (LV) port who are programmed to subthreshold right ventricular (RV) outputs to promote His bundle–only pacing.
Case report
A 34-year-old man with a history of congenital complete heart block who underwent dual-chamber pacemaker implant at age 6 and multiple generator changes was referred for device replacement and lead extraction owing to malfunctioning atrial and ventricular leads. He underwent lead extraction of a dual-chamber pacing system with subsequent reimplantation of a Medtronic Viva CRT pacemaker (CRT-P) generator and bipolar active fixation leads in the right atrium, right ventricle, and His bundle (LV port). The sensing, pacing threshold, and impedance measurements for all 3 leads were stable. On postoperative day 1, to promote His bundle–only pacing without RV pacing, the device was reprogrammed to have a subthreshold RV output of 0.50 V at 0.03 ms. Device parameters are shown in Table 1. On postoperative day 2, rhythm strips were obtained (Figure 1) on telemetry. What is the cause of intermittent loss of capture, and what programming changes would be most appropriate to resolve the issue?
Table 1.
Device parameters on postoperative day 1
| Mode = DDDR | AP = 1%, VP = 99.9% |
|---|---|
| Lower rate limit = 60 bpm | RA lead Sensing = 2.6 mV Threshold = 0.75 V @ 0.4 ms Impedance = 325 ohms |
| Maximum tracking rate = 150 beats/min | |
| Maximum sensor rate = 140 beats/min | RV lead Sensing = 8.2 mV Threshold = 0.375 V @ 0.4 ms Impedance = 532 ohms |
| Paced AV delay = 150 ms Sensed AV delay = 120 ms | |
| His bundle lead Threshold = 0.375 V @ 1.00 ms Impedance = 570 ohms | |
| Capture management Atrial Capture Management: On Right Ventricular Capture Management: On CRT: Nonadaptive CRT LV → RV offset 80 ms |
Programmed Settings Sensing RA lead = 0.30 mV RV lead = 0.90 mV Outputs RA lead = 3.5 V @ 0.4 ms RV lead = 0.50 V @ 0.03 ms His lead = 2.50 V @ 1.00 ms |
AP = atrial pacing; AV = atrioventricular; CRT = cardiac resynchronization therapy; LV = left ventricular; RA = right atrial; RV = right ventricular; VP = ventricular pacing.
Figure 1.
Telemetry strips showing intermittent third-degree atrioventricular block.
Discussion
Telemetry strips are consistent with an AS-VP rhythm depicting nonselective His bundle pacing followed by third-degree atrioventricular block. Ventricular capture is lost for 2.5–3.0 seconds, followed by a junctional escape rhythm at around 46 beats per minute and subsequent resumption of an AS-VP rhythm.
Loss of ventricular pacing in a newly implanted device warrants investigation to ensure system integrity and appropriate programming. The absence of ventricular pacing spikes on the surface electrocardiogram (ECG) can be a sign of oversensing of either intracardiac or extracardiac signals. However, R waves were found to be adequate in size (8 mV) and oversensing was not noted during troubleshooting. No sources of environmental electromagnetic interference were noted, nor was a competing temporary transvenous pacemaker in use. A posteroanterior and lateral chest radiograph did not demonstrate gross dislodgement of the His bundle lead.
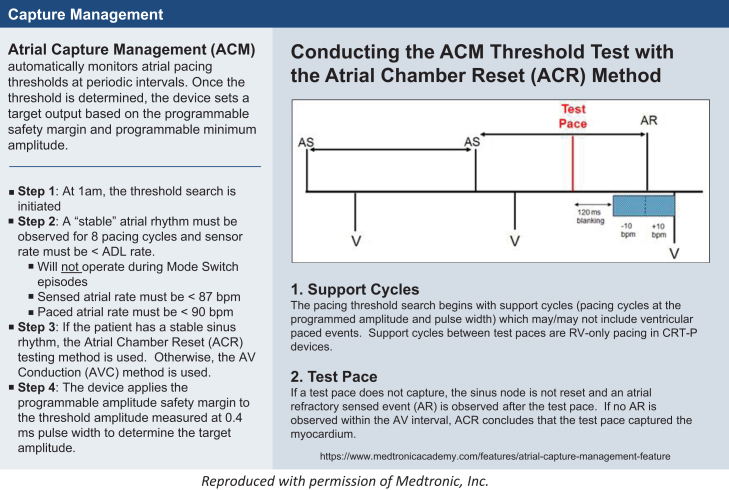
The temporal sequence of these episodes (6:31 AM, 7:01 AM, and 7:31 AM) raised the possibility that a device algorithm could be playing a role. A careful review of the rhythm strips showed that the likely cause of these episodes was Atrial Capture Management (ACM) in the setting of subthreshold RV output programming. With ACM “on,” the device performs an atrial threshold search starting at 1 AM every morning. If a “stable” atrial rhythm is observed, ACM assesses atrial capture thresholds (Figure 2) and can adapt programmed outputs to achieve adequate pacing safety margins. For ACM to run there must be minimal beat-to-beat variation and the sensed atrial rate cannot be faster than 87 beats per minute (Figure 2). In the present case, it is likely that the patient did not meet the abovementioned stability requirements when the threshold search began at 1 AM. When this occurs, the device checks again for stability every 30 minutes thereafter. When stability requirements were finally satisfied at 6:30 AM, the capture threshold test ran and loss of capture was subsequently noted on telemetry.
Figure 2.
Atrial Capture Management algorithm.
It is important to note that when ACM is running in Viva CRT-P devices, the device switches to RV-only pacing during ventricular support cycles for the duration of the test and does not pace from the LV port. In the present case, when the atrial threshold test was initiated, the LV port was not used for pacing and the subthreshold RV pacing outputs were insufficient to capture the myocardium. This led to loss of ventricular capture for the duration of the test (Figure 3A). Furthermore, the absence of ventricular pacing spikes on telemetry was due to the subthreshold RV stimulus, which was of such a low voltage and short pulse width duration (0.50 V/0.03 ms) that the pacing spike could not be visualized on the surface ECG. The absence of “visible” pacing artifacts may mislead the ECG interpreter to conclude that loss of capture is due to oversensing with associated inhibition of ventricular pacing. ACM perceives the underlying escape rhythm as “premature ventricular contractions” and eventually aborts the test sequence (Figure 3B) and reschedules ACM to run again in 30 minutes. This pattern occurred 3 times before the issue was resolved by turning the ACM algorithm off. This phenomenon could also have been corrected by leaving ACM on and programming the RV output to a value above pacing threshold. We did not opt to do this, as the patient had a narrow, more physiologic QRS with nonselective His pacing.
Figure 3.
A: Subthreshold right ventricular support paces during Atrial Capture Management algorithm. B: Enough device-determined “premature ventricular contractions” occur in each episode that the Atrial Capture Management test is aborted. The device returns to “biventricular” pacing, which in this case is His-bundle pacing. ACM = atrial capture management; AP = atrial pacing; AS = atrial sensing; LVP = left ventricular pacing; PVC = premature ventricular contraction; RVP = right ventricular pacing; VS = ventricular sensing.
It should be noted that RV Capture Management (RVCM) uses RV-only support pacing during threshold testing as well. Both RVCM and ACM switch to RV-only pacing during testing and will reattempt every 30 minutes after an aborted test. Either version of Capture Management had the potential to result in loss of capture for this patient. However, ACM is the most likely culprit owing to the location of the large pacing spike after the first 3 P waves in each episode. The timing of this pacing output is most consistent with ACM using the Atrial Chamber Reset (ACR) method (Figure 2). The ACR method measures P-wave intervals, paces the atrium before the next expected P wave, and then determines the atrial threshold by whether the sinus node was reset (capture) or not (loss of capture). Furthermore, in RVCM, a backup RV pace would have occurred 110 ms after the test pace at the programmed amplitude of 0.5 V and a pulse width of 1.0 ms. This would likely have captured the ventricle as the RV capture threshold was 0.375 V at 0.4 ms.
Alternatively, the RV lead can be programmed to pace 40–80 ms after the LV lead to avoid asystole in pacemaker-dependent patients receiving CRT devices with His bundle lead in the LV port. This would result in pacing in the absolute refractory period if His bundle capture is occurring. If the His bundle lead fails to capture, backup RV pacing would still be operational. However, battery drain is a concern with this strategy. The present case underscores the importance of turning both Atrial and Ventricular Capture Management algorithms “off” in Viva CRT-P devices with subthreshold RV output programming to avoid loss of ventricular capture and its grave consequences in pacemaker-dependent patients.
Key Teaching Points.
-
•
Loss of ventricular pacing warrants thorough investigation including reviewing the “out-of-box” algorithms that are typically turned on in newly implanted devices.
-
•
During Atrial and Ventricular Capture Management testing, the device switches to right ventricular (RV)–only pacing during ventricular support cycles for the duration of the test and does not pace from the left ventricular (LV) port in cardiac resynchronization therapy (CRT) devices.
-
•
In patients receiving CRT devices with a His bundle lead in the LV port who are programmed to subthreshold RV outputs to promote His bundle–only pacing, it is imperative to turn off Atrial and Ventricular Capture Management algorithms to avoid loss of ventricular capture, especially if they are pacemaker dependent.
Footnotes
Dr Ellenbogen received honoraria from Biotronik, Medtronic, Boston Scientific, and St. Jude Medical. Dr Koneru received honoraria from Medtronic, Boston Scientific and St. Jude Medical.
References
- 1.Ajijola O.A., Upadhyay G., Macias C., Shivkumar K., Tung R. Permanent His-bundle pacing for cardiac resynchronization therapy: initial feasibility study in lieu of left ventricular lead. Heart Rhythm. 2017;14:1353–1361. doi: 10.1016/j.hrthm.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Sharma P.S., Pugazhendhi V. His bundle pacing or biventricular pacing for cardiac resynchronization therapy in heart failure: discovering new methods for an old problem. J Atr Fibrillation. 2017;9:6–10. doi: 10.4022/jafib.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]