Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) and laparoscopic gastric bypass (LRYGB) are most commonly performed bariatric procedures. Laparoscopic approach and enhanced recovery after surgery (ERAS) protocols managed to decrease length of hospital and morbidity. However, there are patients in whom, despite adherence to the protocol, the length of stay (LOS) remains longer than targeted. This study aimed to assess potential risk factors for prolonged LOS and readmissions.
Methods
The study was a prospective observation with a post-hoc analysis of bariatric patients in a tertiary referral university teaching hospital. Inclusion criteria were undergoing laparoscopic bariatric surgery. Exclusion criteria were occurrence of perioperative complications, prior bariatric procedures, and lack of necessary data. The primary endpoints were the evaluations of risk factors for prolonged LOS and readmissions.
Results
Median LOS was 3 (2–4) days. LOS > 3 days occurred in 145 (29.47%) patients, 79 after LSG (25.82%) and 66 after LRYGB (35.48%; p = 0.008). Factors significantly prolonging LOS were low oral fluid intake, high intravenous volume of fluids administered on POD0, and every additional 50 km distance from habitual residence to bariatric center. The risk of hospital readmission rises with occurrence of intraoperative adverse events and low oral fluid intake on the day of surgery on.
Conclusions
Risk factors for prolonged LOS are low oral fluid intake, high intravenous volume of fluids administered on POD0, and every additional 50 km distance from habitual residence. Risk factors for hospital readmission are intraoperative adverse events and low oral fluid intake on the day of surgery.
Keywords: Bariatric surgery, Length of hospital stay, Risk factors, Readmission
Introduction
Nowadays, laparoscopic sleeve gastrectomy (LSG) and laparoscopic gastric bypass (LRYGB) are becoming first-line treatment for morbid obesity in Poland and worldwide, with widely accepted low risk for postoperative morbidity and low mortality [1–5]. In addition, treating patients in accordance with enhanced recovery after surgery (ERAS) protocols has reduced the length of stay (LOS) and decreased morbidity [6, 7]. Despite that, some patients with successful adherence to the protocol and uneventful peri- and post-operative period fail to meet discharge criteria and remain a longer period of time than targeted LOS. Shorter LOS may be associated with an increased rate of readmissions, and in some patients it results in readmission for variety of reasons [8–10].
The relationship between perioperative complications occurrence and prolonged LOS seems to be obvious, but the interesting question is what is affecting LOS in uncomplicated patients. Therefore, we analyzed risk factors for prolonged hospitalization and hospital readmission in order to predict patients without complications who might require longer hospital observation.
Aim
Study aim was to identify risk factors for prolonged length of hospital stay and unplanned readmission after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass among patients with uncomplicated postoperative course.
Methods
The study was a prospective observation with a post-hoc analysis of patients who underwent bariatric surgery in a tertiary referral university teaching hospital. The indication for surgical treatment was taken from the IFSO-EC and EASO guidelines: body mass index (BMI) ≥ 35 kg/m2 with comorbidities or BMI of ≥ 40 kg/m2 [11, 12]. The inclusion criteria were written informed consent upon hospital admission acknowledging that the outcomes of perioperative treatment and follow-up may be analyzed retrospectively and used for research, age of 18 to 65 years, and eligibility for LSG or LRYGB. Exclusion criteria were occurrence of perioperative complications, prior bariatric procedures, and lack of necessary data. Study was designed according to STROBE Statement [13].
Patients were treated in accordance with the principles of multimodal ERAS pathway, including preoperative, intraoperative, and postoperative interventions [2, 6, 14–16]. Preoperative interventions included extensive perioperative counseling, shortened fluid fasts, preoperative high protein and carbohydrate drink, and optimized operating scheduling times. Intraoperatively, the optimized bariatric anesthetic protocol was introduced with the use of multimodal analgesia. There was no routine use of nasogastric tubes and intraabdominal drains. Postoperative interventions included early mobilization, analgesia without opioids, administration of IPP-antagonist, early enteral feeding, and discharge planning. Anti-thrombotic prophylaxis was administered up to 14 postoperative days with the use of Enoxaparine. Detailed information on protocol used in our clinic is presented below:
Preoperative counseling and patient’s education
Pre-operative carbohydrate loading (400 ml of Nutricia preOp® 2 h prior surgery)
Antithrombotic prophylaxis (Clexane® 40 mg sc. starting in the evening prior surgery)
Antibiotic prophylaxis (preoperative Ceftriaxone 2 g iv 30–60 min. prior surgery)
Laparoscopic surgery
Balanced intravenous fluid therapy (< 2500 ml intravenous fluids during the day of surgery, less than 150 mmol sodium). Indication for administration of i.v. fluids after surgery: vomiting, insufficient oral fluid intake (less than 500 ml before 7:00 pm, 7 h after surgery), insufficient diuresis (less than 500 ml of urine before 7:00 pm, 7 h after surgery). The target is to not use intravenous fluids in POD1. Fluids were given only if we observed absence of sufficient functional recovery: vomiting, insufficient oral fluid intake (less than 500 ml until 4:00 pm), insufficient diuresis, or biochemical symptoms of rhabdomyolysis
No nasogastric tubes postoperatively
No drains left routinely
TAP block and bariatric anesthesia protocol
Avoiding opioids, multimodal analgesia (oral when possible—Paracetamol 4 × 1 g, Ibuprofen 2 × 200 mg, Metamizole 2 × 500 mg, or Ketoprofen 2 × 100 mg); routine use of ondansetron, metoclopramide, and deksametazon at the end of the surgery
Postoperative oxygenation therapy (4–6 l/min)
Early oral feeding (oral nutritional supplement 4 h postoperatively—Nutrcia Nutridrink® or Nestlé Impact®, light hospital diet, and oral nutritional supplements on the first postoperative day, full hospital diet in the second postoperative day)
Early mobilization on the day of surgery (sitting on the bed 2 h after surgery, breathing exercises with physiotherapist, walking to the toilette, and walking along the corridor (at least 150 m) accompanied by an ERAS nurse or a family member. Full mobilization on the first postoperative day (getting out of bed, going to the toilette, walking along the corridor without support of the nurse, at least 4–6 h out of bed)
On admission, every patient was informed about the target length of stay of 3 days. Discharge criteria:
Oral diet tolerance (solid food consumption, drinking at least 1500 ml of fluids)
No need for i.v. drugs or fluids
Balanced diuresis
Pain of low magnitude, manageable with oral pain killers
No fever
Properly healing surgical wounds
Physical activity at a level similar to pre-surgery time
No complications requiring in-hospital observation
Other’s people help available in the first days after surgery
Possibility to return to hospital when suspecting complication development (means to contact, transportation from home)
Patients were scheduled for postoperative appointment 2 weeks after discharge, next 1 and 6 months after discharge. Surgical techniques for LSG and LRYGB were standardized in all cases to reduce study bias.
The primary endpoints were the evaluations of risk factors for prolonged length of stay and of risk factors for readmissions in the postoperative period in the group of patients without complications.
LOS was defined as the length of inpatient episode of care, calculated from the day of admission to the day of discharge, and based on the number of nights spent in hospital. The discharge occurred regardless of the day of the week. Patients were dichotomized into group of patients whose hospital stay was shorter or equal to the target LOS (≤3 days) and group of patients with prolonged LOS, defined as total length of stay in bariatric care unit longer than 3 days. Readmission was defined as hospitalization after discharge from bariatric care unit related to bariatric treatment within 30-days postoperative period.
Comparison of baseline patients data was done using Student’s t test or Mann-Whitney’s test for quantitative variables, while χ2 with or without Yates’ correction were used for qualitative variables. Univariate and multivariate logistic regression models were built to assess influence of patient- and treatment-related parameters on odds ratios (OR) with 95% confidence intervals (95% CI) for prolonged hospital stay and hospital readmissions. P value < 0.05 was considered statistically significant. Data were analyzed using Statistica version 12.0 PL (StatSoft Inc., Tulsa, Oklahoma, USA). Quantitative data are expressed as mean ± standard deviation or medians with interquartile range.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of the Jagiellonian University.
Material
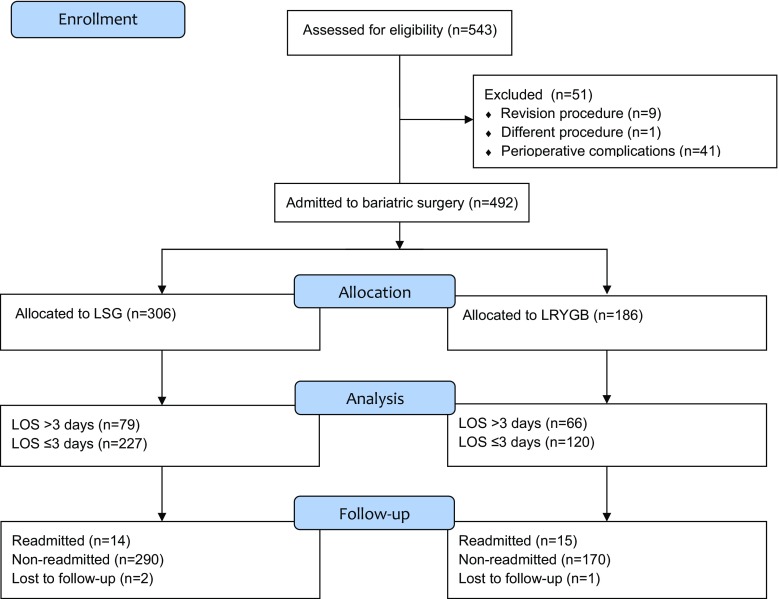
From April 2009 to July 2016, 543 patients were treated for morbid obesity. Then, 492 patients met inclusion criteria and were submitted to laparoscopic sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass [310 females, 182 males, median age 42 (34–51) years] (Table 1). Flow chart of patients in the study is shown in Fig. 1.
Table 1.
Patients and groups baseline characteristics
| Parameter | All patients | |
|---|---|---|
| 492 (100%) | ||
| Females, n (%) | 310 (63%) | |
| Males, n (%) | 182 (37%) | |
| Median age, years (IQR) | 42 (34–51) | |
| Median maximal preoperative BMI, kg/m2 (IQR) | 46.56 (42.89–51.50) | |
| Median BMI on a day of operation, kg/m2 (IQR) | 45.09 (41.31–49.74) | |
| ∆BMI (IQR) | 0.98 (0–2.42) | |
| ASA class, n (%) | 1 | 11 (2.30%) |
| 2 | 333 (69.52%) | |
| 3 | 135 (28.18%) | |
| Cardiovascular diseases, n (%) | 87 (17.68%) | |
| Hypertension, n (%) | 335 (68.23%) | |
| Prediabetes, n (%) | 22 (4.47%) | |
| Diabetes mellitus, n (%) | 168 (34.29%) | |
| Obstructive sleep apnea, n (%) | 35 (7.11%) | |
| Non-alcoholic fatty liver disease, n (%) | 306 (62.45%) | |
| Dyslipidemia, n (%) | 278 (56.85%) | |
IQR interquartile range, ASA class American Society of Anesthesiologists physical status classification system
Fig. 1.
Study flowchart
Results
Median length of hospital stay (LOS) was 3 (2–4) days. LOS > 3 days occurred in 145 (29.47%) patients, 79 after LSG (25.82%), and 66 after LRYGB (35.48%; p = 0.008). Factors possibly prolonging length of hospital stay were analyzed in univariate logistic regression models. Maximal preoperative BMI > 51.50 kg/m2, LRYGB, operative time, intraoperative adverse events, high intraoperative volume of administered fluids, low postoperative oral fluid intake and diuresis, need for Furosemide forced diuresis, high postoperative intravenous fluid volume, postoperative tachycardia, occurrence of postoperative fever, postoperative nausea and vomiting, requirement for additional pain medication, every 50 km distance between place of residence and bariatric center were significantly related to the risk of prolonged LOS (LOS > 3 days vs. ≤ 3 days) (Table 2). Therefore, those possibly relevant factors were analyzed in multivariate logistic regression model (Table 3). Factors significantly prolonging LOS were low oral fluid intake, high intravenous volume of fluids administered on POD0, and every additional 50 km distance from habitual residence to bariatric center.
Table 2.
Univariate logistic regression models for odds ratio of prolonged LOS (> 3 vs. ≤ 3 days)
| Factors | OR | 95% CI | P | |
|---|---|---|---|---|
| Patient-related | Sex (M = 0, F = 1) | 0.91 | 0.61–1.35 | 0.629 |
| Age (with every 1 year) | 0.99 | 0.97–1.01 | 0.374 | |
| Age (> 51 vs. ≤ 51 years) | 1.07 | 0.68–1.70 | 0.761 | |
| Maximal preoperative BMI (1 kg/m2) | 1.03 | 0.99–1.06 | 0.056 | |
| Maximal preoperative BMI (> 51.50 vs. ≤ 51.50 kg/m2) | 1.55 | 1.01–2.39 | 0.047 | |
| BMI on the day of operation (1 kg/m2) | 1.02 | 0.99–1.06 | 0.119 | |
| BMI on the day of operation (> 49.74 vs. ≤ 49.74 kg/m2) | 1.41 | 0.91–2.18 | 0.124 | |
| Co-morbidities | ASA class (with every point) | 1.36 | 0.91–2.04 | 0.133 |
| Cardio-vascular diseases (yes = 1, no = 0) | 1.60 | 0.98–2.60 | 0.058 | |
| Arterial hypertension (yes = 1, no = 0) | 1.21 | 0.79–1.84 | 0.388 | |
| Prediabetes (yes = 1, no = 0) | 1.39 | 0.57–3.39 | 0.470 | |
| Diabetes mellitus (yes = 1, no = 0) | 1.25 | 0.84–1.88 | 0.271 | |
| Obstructive sleep apnea (yes = 1, no = 0) | 1.27 | 0.61–2.63 | 0.518 | |
| Non-alcoholic fatty liver disease (yes = 1, no = 0) | 0.94 | 0.63–1.40 | 0.752 | |
| Dyslipidemia (yes = 1, no = 0) | 1.36 | 0.91–2.02 | 0.131 | |
| Malnutrition (yes = 1, no = 0) | 1.42 | 0.92–2.19 | 0.113 | |
| Treatment-related | Type of procedure (LRYGB vs. LSG) | 1.58 | 1.06–2.35 | 0.023 |
| Operative time (with every 1 min) | 1.01 | 1.00–1.01 | <0.001 | |
| Operative time (> 150 vs. ≤ 150 min) | 2.05 | 1.29–3.24 | 0.002 | |
| Intraoperative adverse effects (yes = 1, no = 0) | 3.99 | 1.51–10.53 | 0.005 | |
| Intraoperative fluid volume administered (500 ml) | 1.52 | 1.24–1.87 | <0.001 | |
| Postoperative period | Oral fluid intake on POD0 (100 ml) | 0.80 | 0.74–0.85 | <0.001 |
| Oral fluid intake on POD1 (100 ml) | 0.88 | 0.85–0.91 | <0.001 | |
| Oral fluid intake on POD2 (100 ml) | 0.94 | 0.91–0.97 | <0.001 | |
| Oral fluid intake on POD3 (100 ml) | 1.08 | 0.88–1.32 | 0.464 | |
| Diuresis on POD0 (1000 ml) | 1.85 | 1.44–2.40 | <0.001 | |
| Diuresis on POD1 (1000 ml) | 1.20 | 0.91–1.57 | 0.190 | |
| Diuresis on POD2 (1000 ml) | 1.29 | 0.94–1.75 | 0.111 | |
| Diuresis on POD3 (1000 ml) | 28.95 | 0.08–10,888 | 0.261 | |
| Furosemide forced diuresis (yes = 1, no = 0) | 2.52 | 1.58–4.02 | <0.001 | |
| Intravenous fluid intake on POD0 (yes = 1, no = 0) | 1.04 | 0.68–1.59 | 0.851 | |
| Intravenous fluid volume on POD0 (500 ml) | 1.55 | 1.04–2.31 | 0.032 | |
| Intravenous fluid intake on POD1 (yes = 1, no = 0) | 4.89 | 2.87–8.35 | <0.001 | |
| Intravenous fluid volume on POD1 (500 ml) | 1.57 | 1.34–1.83 | <0.001 | |
| Intravenous fluid intake on POD2 (yes = 1, no = 0) | 8.44 | 5.06–14.06 | <0.001 | |
| Intravenous fluid volume on POD2 (500 ml) | 1.56 | 1.18–2.06 | 0.002 | |
| Heart rate on POD0 (with every 1/min) | 1.01 | 0.99–1.03 | 0.452 | |
| Tachycardia on POD0 (yes = 1, no = 0) | 9.82 | 1.08–89.19 | 0.042 | |
| Heart rate on POD1 (with every 1/min) | 0.99 | 0.97–1.01 | 0.420 | |
| Tachycardia on POD1 (yes = 1, no = 0) | 1.50 | 0.48–4.69 | 0.482 | |
| Heart rate on POD2 (with every 1/min) | 1.01 | 0.99–1.03 | 0.591 | |
| Tachycardia on POD2 (yes = 1, no = 0) | 2.04 | 0.50–8.32 | 0.319 | |
| Heart rate on POD3 (with every 1/min) | 1.00 | 0.97–1.03 | 0.940 | |
| Tachycardia on POD3 (yes = 1, no = 0) | 1.22 | 0.11–13.84 | 0.874 | |
| CPK (> 1000 vs. < 1000 U/L) | 1.55 | 0.87–2.74 | 0.135 | |
| Postoperative fever (yes = 1, no = 0) | 2.50 | 1.50–4.15 | <0.001 | |
| Postoperative nausea and vomiting (yes = 1, no = 0) | 2.57 | 1.19–5.57 | 0.016 | |
| Additional pain medication required (yes = 1, no = 0) | 1.95 | 1.30–2.94 | 0.001 | |
| Distance between the hospital and place of residence (50 km) | 1.18 | 1.08–1.28 | <0.001 | |
Italic entries reached significance of p < 0.05 as stated in methodology
ASA class American Society of Anesthesiologists physical status classification system, POD0 postoperative day 0, POD1 postoperative day 1, POD2 postoperative day 2, POD3 postoperative day 3, POD4 postoperative day 4, CPK creatine phosphokinase
Table 3.
Multivariate logistic regression models for odds ratio of prolonged LOS (> 3 vs. ≤ 3 days)
| OR | 95% CI | P | |
|---|---|---|---|
| Maximal preoperative BMI (> 51.50 vs. ≤ 51.50 kg/m2) | 1.11 | 0.39–3.13 | 0.849 |
| Type of procedure (LRYGB vs. LSG) | 0.74 | 0.25–2.21 | 0.590 |
| Operative time (> 150 vs. ≤ 150 min) | 1.11 | 0.36–3.38 | 0.859 |
| Intraoperative adverse effects (yes = 1, no = 0) | 1.88 | 0.37–9.49 | 0.439 |
| Intraoperative fluid volume administered (500 ml) | 0.75 | 0.45–1.24 | 0.255 |
| Oral fluid intake on POD0 (100 ml) | 0.77 | 0.67–0.88 | <0.001 |
| Intravenous fluid volume on POD0 (500 ml) | 1.71 | 1.03–2.82 | 0.036 |
| Diuresis on POD0 (1000 ml) | 1.19 | 0.61–2.32 | 0.603 |
| Furosemide forced diuresis (yes = 1, no = 0) | 1.19 | 0.40–3.57 | 0.751 |
| Tachycardia on POD0 (yes = 1, no = 0) | 9.19 | 0.38–219.79 | 0.167 |
| Postoperative fever (yes = 1, no = 0) | 2.23 | 0.77–6.49 | 0.139 |
| Postoperative nausea and vomiting (yes = 1, no = 0) | 1.02 | 0.31–3.38 | 0.973 |
| Additional pain medication required (yes = 1, no = 0) | 0.88 | 0.36–2.15 | 0.775 |
| Distance between the hospital and place of residence (50 km) | 1.59 | 1.26–2.01 | <0.001 |
Italic entries reached significance of p < 0.05 as stated in methodology
POD0 postoperative day 0
Readmission rate in the study population was 5.89% (29 readmissions). Fourteen patients after LSG (4.58%) were readmitted, while 15 after LRYGB (8.06%; p = 0.172) (Table 4). Univariate logistic regression analyses revealed statistically significant impact of operative time, intraoperative adverse events, intraoperative volume of administered fluids, oral fluid intake, postoperative intravenous fluid administration, and prolonged LOS (> 3 days vs. ≤ 3 days) on the risk of hospital readmission (Table 5). Multivariate logistic regression model revealed significant impact of occurrence of intraoperative adverse events and low oral fluid intake on the day of surgery on the risk of hospital readmission (Table 6). Intraoperative adverse events which occurred in our unit are presented in Table 7.
Table 4.
Reasons for readmission
| LSG | LRYGB | |
|---|---|---|
| Operation site hernia | 2 (0.65%) | 3 (1.61%) |
| Cholecystitis | 2 (0.65%) | 3 (1.61%) |
| Linea alba herniation | 0 | 2 (1.08%) |
| Internal hernia (Petersen space hernia) | 0 | 1 (0.54%) |
| Perforated gastric ulcer | 0 | 1 (0.54%) |
| GI bleeding | 0 | 2 (1.08%) |
| Perianal abscess | 0 | 1 (0.54%) |
| Pulmonary thrombosis | 0 | 1 (0.54%) |
| Gastroesophageal reflux disease | 3 (0.98%) | 0 |
| Fever of undetermined origin | 1 (0.33%) | 0 |
| Chronic diarrhea | 1 (0.33%) | 0 |
| Suspected ileus | 1 (0.33%) | 0 |
| Dysphagia | 4 (1.31%) | 0 |
| Lower abdomen pain | 0 | 1 (0.54%) |
| Total | 14/306 (4.58%) | 15/186 (8.06%) |
Table 5.
Univariate logistic regression models of factors possibly affecting odds ratio of hospital readmission
| Factors | OR | 95% CI | P | |
|---|---|---|---|---|
| Patient-related | Sex (M = 0, F = 1) | 0.76 | 0.35–1.66 | 0.495 |
| Age (with every 1 year) | 1.02 | 0.99–1.06 | 0.208 | |
| Age (> 51 vs. ≤ 51 years) | 1.14 | 0.47–2.77 | 0.765 | |
| Maximal preoperative BMI (1 kg/m2) | 1.05 | 0.99–1.10 | 0.094 | |
| Maximal preoperative BMI (> 51.50 vs. ≤ 51.50 kg/m2) | 1.44 | 0.63–3.28 | 0.382 | |
| BMI on the day of operation (1 kg/m2) | 1.03 | 0.97–1.09 | 0.404 | |
| BMI on the day of operation (> 49.74 vs. ≤ 49.74 kg/m2) | 1.44 | 0.63–3.28 | 0.382 | |
| Co-morbidities | ASA class (with every point) | 1.54 | 0.69–3.43 | 0.287 |
| Cardio-vascular diseases (yes = 1, no = 0) | 1.93 | 0.82–4.56 | 0.130 | |
| Arterial hypertension (yes = 1, no = 0) | 1.19 | 0.51–2.77 | 0.692 | |
| Prediabetes (yes = 1, no = 0) | 2.79 | 0.77–10.10 | 0.117 | |
| Diabetes mellitus (yes = 1, no = 0) | 0.91 | 0.40–2.06 | 0.823 | |
| Obstructive sleep apnea (yes = 1, no = 0) | 0.48 | 0.06–3.67 | 0.478 | |
| Non-alcoholic fatty liver disease (yes = 1, no = 0) | 0.93 | 0.42–2.02 | 0.847 | |
| Dyslipidemia (yes = 1, no = 0) | 1.65 | 0.73–3.74 | 0.227 | |
| Malnutrition (yes = 1, no = 0) | 1.57 | 0.66–3.74 | 0.304 | |
| Treatment-related | Type of procedure (LRYGB vs. LSG) | 1.70 | 0.79–3.65 | 0.176 |
| Operative time (with every 1 min) | 1.01 | 1.00–1.01 | 0.068 | |
| Operative time (> 150 vs. ≤ 150 min) | 2.31 | 1.02–5.24 | 0.044 | |
| Intraoperative adverse effects (yes = 1, no = 0) | 5.32 | 1.62–17.45 | 0.006 | |
| Intraoperative fluid volume administered (500 ml) | 1.78 | 1.27–2.50 | 0.001 | |
| Postoperative period | Oral fluid intake on POD0 (100 ml) | 0.86 | 0.74–0.99 | 0.030 |
| Oral fluid intake on POD1 (100 ml) | 0.94 | 0.88–1.01 | 0.072 | |
| Oral fluid intake on POD2 (100 ml) | 0.91 | 0.84–0.98 | 0.010 | |
| Oral fluid intake on POD3 (100 ml) | 0.92 | 0.81–1.04 | 0.162 | |
| Diuresis on POD0 (1000 ml) | 1.56 | 0.99–2.47 | 0.056 | |
| Diuresis on POD1 (1000 ml) | 0.74 | 0.40–1.36 | 0.337 | |
| Diuresis on POD2 (1000 ml) | 0.98 | 0.52–1.87 | 0.957 | |
| Diuresis on POD3 (1000 ml) | 2.01 | 0.93–4.34 | 0.072 | |
| Furosemide-forced diuresis (yes = 1, no = 0) | 0.78 | 0.33–1.87 | 0.577 | |
| Intravenous fluid intake on POD0 (yes = 1, no = 0) | 0.88 | 0.35–2.21 | 0.781 | |
| Intravenous fluid volume on POD0 (500 ml) | 0.05 | 0.004–0.68 | 0.023 | |
| Intravenous fluid intake on POD1 (yes = 1, no = 0) | 1.54 | 0.59–4.03 | 0.379 | |
| Intravenous fluid volume on POD1 (500 ml) | 1.19 | 0.96–1.47 | 0.113 | |
| Intravenous fluid intake on POD2 (yes = 1, no = 0) | 2.31 | 0.89–5.96 | 0.083 | |
| Intravenous fluid volume on POD2 (500 ml) | 0.95 | 0.63–1.42 | 0.791 | |
| Heart rate on POD0 (with every 1/min) | 1.01 | 0.96–1.05 | 0.767 | |
| Tachycardia on POD0 (yes = 1, no = 0) | 5.14 | 0.55–48.33 | 0.151 | |
| Heart rate on POD1 (with every 1/min) | 1.00 | 0.96–1.05 | 0.832 | |
| Tachycardia on POD1 (yes = 1, no = 0) | 1.67 | 0.21–13.57 | 0.628 | |
| Heart rate on POD2 (with every 1/min) | 1.01 | 0.97–1.05 | 0.709 | |
| Tachycardia on POD2 (yes = 1, no = 0) | 0.02 | 0.008–62.24 | 0.701 | |
| Heart rate on POD3 (with every 1/min) | 1.01 | 0.95–1.07 | 0.776 | |
| Tachycardia on POD3 (yes = 1, no = 0) | 6.94 | 0.57–84.03 | 0.126 | |
| CPK (> 1000 vs. < 1000 U/L) | 2.19 | 0.85–5.67 | 0.105 | |
| Postoperative fever (yes = 1, no = 0) | 1.15 | 0.38–3.52 | 0.804 | |
| Postoperative nausea and vomiting (yes = 1, no = 0) | 1.59 | 0.35–7.19 | 0.547 | |
| Additional pain medication required (yes = 1, no = 0) | 1.71 | 0.72–4.04 | 0.221 | |
| Distance between the hospital and place of residence (50 km) | 0.91 | 0.73–1.13 | 0.389 | |
| Prolonged LOS (> 3 vs. ≤ 3 days) | 2.57 | 1.19–5.56 | 0.016 | |
Italic entries reached significance of p < 0.05 as stated in methodology
ASA class American Society of Anesthesiologists physical status classification system, POD0 postoperative day 0, POD1 postoperative day 1, POD2 postoperative day 2, POD3 postoperative day 3, POD4 postoperative day 4, LOS length of stay, CPK creatine phosphokinase, LOS length of hospital stay
Table 6.
Multivariate logistic regression model for hospital readmission
| OR | 95% CI | P | |
|---|---|---|---|
| Operative time (> 150 vs. ≤ 150 min) | 2.79 | 0.34–22.94 | 0.335 |
| Intraoperative adverse effects (yes = 1, no = 0) | 4.20 | 1.17–151.14 | 0.039 |
| Intraoperative fluid volume administered (500 ml) | 1.88 | 0.72–4.92 | 0.192 |
| Oral fluid intake on POD0 (100 ml) | 0.54 | 0.29–0.99 | 0.043 |
| Intravenous fluid volume on POD0 (500 ml) | 0.03 | 0.001–1.18 | 0.059 |
| Prolonged LOS (> 3 vs. ≤ 3 days) | 0.31 | 0.03–3.42 | 0.332 |
Italic entries reached significance of p < 0.05 as stated in methodology
POD0 postoperative day 0, POD3 postoperative day 3, LOS length of stay
Table 7.
Intraoperative adverse events
| All | Readmitted | Non-readmitted | P | |
|---|---|---|---|---|
| Total | 18/492 (3.66%) | 4/29 (13.79%) | 14/463 (3%) | 0.015 |
| Need for small intestine resection | 6 | 2 | 4 | 0.041 |
| Intraoperatively diagnosed staple line leakage | 2 | 2 | 0 | – |
| Inappropriate stapling that required modification of technique | 2 | 0 | 2 | – |
| Small intestine perforation | 2 | 0 | 2 | – |
| Excessive intraoperative bleeding | 2 | 0 | 2 | – |
| Intraoperatively diagnosed stricture | 1 | 0 | 1 | – |
| Intestinal serosa rupture | 1 | 0 | 1 | – |
| Probe immobilized with stapler | 1 | 0 | 1 | – |
| Intubation failure, cancelation of procedure | 1 | 0 | 1 | – |
Italic entries reached significance of p < 0.05 as stated in methodology
Discussion
We report outcomes of a study, where we sought to identify risk factors for prolonged length of hospital stay, despite instituted treatment according to modern model of perioperative care (ERAS). In our unit, our aim is to discharge the patient not as early as it is possible but as soon as patients reach full functional recovery. We demonstrated that with every 100 ml of oral fluid intake on the POD0, the risk for prolonged LOS decreased by 23%. As for i.v. fluids on POD0, the need for every 500 ml increased the risk for prolonged hospital stay 1.71 times. With every 50 km distance from the hospital to place of residence, the odds for prolonged LOS increased 1.59 times. We revealed that occurrence of intraoperative adverse events (after excluding patients with perioperative complications in study design) increased 4.2 times odds ratio for readmission. Additional data on which intraoperative events led to readmission are presented in Table 7. It should be emphasized that even though the result is statistically insignificant for particular types of events, the fact the readmissions occurred only after “Need for small intestine resection” or “Intraoperatively diagnosed staple line leakage” should alert the surgeon about possible readmission. High oral fluid intake on POD0 was protective factor decreasing risk for readmission 0.54 times.
Length of stay varies among bariatric centers due to differences in perioperative pathways and discharge criteria. Recent study on predictors for LOS, which included 9593 LRYGB, reported median length of stay of 2 days (range 0–544), in which 26% of patients required > 3 days of hospitalization [17]. In a study by Dallal et al., the hospital discharged 48% of bariatric patients by postoperative day (POD) 1, 85% by POD 2, and 96% by POD 3 [18]. Other studies on this matter usually reported LOS > 3 days as prolonged LOS, which is the same threshold as we had [19–21]. Different treatment protocols are administered nowadays for bariatric patients. Many researchers reported bariatric procedures performed in the fast-track surgery way; however, this requires additional actions to prepare and carry on treatment within 24-h hospital stay [22–24]. In our case, patients were admitted to the hospital in the afternoon prior to the operation day. Hospital stay was planned for 3 days and patients were obligated to follow criteria for discharge upon decision making. In summary, comparison between different bariatric centers could be troublesome, not only because of qualitative differences but also due to the applied approach to the treatment protocol.
The overall readmission rate in a study by Lois et al., which included 95,294 patients after bariatric surgery, was 5.7% [19]. Recent study by Sippey et al. reported an overall 30-day readmission rate after LSG or LRYGB of 5.1% [25]. Other authors reported readmission rates after those two procedures in the range of 1.87–14.16% [18, 26–33]. Despite many authors reporting more common readmissions after LRYGB compared with LSG [25, 27, 28, 34], one study documented higher rates after LSG [19]. In our study, overall readmission rate was 5.89%.
According to other studies, patient-related factors associated with prolonged LOS were age, higher preoperative BMI, male sex, number of preoperative comorbidities, and operative time [18, 35–38]. Regarding demographic factors in our study, they were not significantly related to the risk of prolonged LOS. Considering comorbidities, Carter et al. in a large study involving 500 hospitals in the National Surgical Quality Improvement Program (NSQIP) database showed that after gastric by-pass, longer hospitalization was predicted by diabetes, chronic obstructive pulmonary disease, hemorrhagic diathesis, chronic kidney disease, hypoalbuminemia, but with no other patient-related factors [17]. Sun et al. showed that patients with history of congestive heart failure, peripheral vascular, and kidney diseases were more prone to have longer LOS [39]. However, in our study, neither higher ASA class nor the presence of other comorbidities was related to the risk of prolonged LOS. We proved that in the end, LRYGB was not significantly related to prolonging LOS in comparison with LSG. Similar conclusions were found Weiner et al. [40]. We failed to determine what caused the lack of influence of patient’s health status or comorbidities on our endpoints. We hypothesize that it may be caused by individualized perioperative care, which was proven in another surgical disciplines [7, 41–43]. In studies by Reames et al., Carter et al., and Dallall et al., researchers concluded that the longer was the operative time, the greater was the risk for prolonged length of stay [17, 18, 20]. The same relationship was found in our study; however, a multivariate analysis revealed that it was contributing less to the risk of prolonged LOS. Nossaman et al. concluded that the volume of intravenous fluids administered during laparoscopic bariatric surgery significantly correlates to LOS and delays wound healing [37]. They showed that lower volumes of intraoperative fluid were significantly associated with longer LOS [37]. Contrary to that, we observed that patients who required larger amounts of intraoperative i.v. fluids were more prone to longer hospital stay; however, this correlation was not shown in the multivariate analysis. In our study, decreased amount of postoperative oral fluid intake (on POD0), need for i.v. fluids (POD0), and increasing distance between the hospital and place of residence were significantly contributing to increased risk of prolonged hospital stay.
In numerous papers, we found significant correlations of some patient-dependent factors and comorbidities on readmission rates, i.e., higher BMI and ASA class, diabetes mellitus, cardio-vascular, respiratory, renal co-morbidities, and chronic steroid intake, protein malnutrition were showed to be associated with increased risk of readmission [21, 25, 34, 35, 38, 39]. Treating patients in accordance to ERAS protocol probably contributed to non-significant relationship of preoperative ASA class and comorbidities with the risk of postoperative readmissions in our study [6, 7, 15, 16, 44]. We, as other researchers did, determined that BMI was not found to be a predictor of readmission [34, 45, 46].
In study by Sippey et al., the readmissions were higher after LRYGB compared with LSG [25]. In another, patients who underwent LRYGB had 60% higher risk for readmission in the 30-day postoperative time period compared to those who underwent LSG [34]. Contrary to this, we and Doumouras et al. did not observe similar relationship [26]. Operative time and intraoperative adverse events were also proved to increase risk of readmission [34, 47]. Postoperative complications were found to be associated with significant increase in readmissions in study by Khorgami et al. and other researchers [26, 34, 48–50]. In our study, multivariate analysis elicited independent influence of intraoperative adverse events and oral fluid intake on POD0 as factors associated with the risk of readmission. Regarding the fact that one of the most common reason for readmission after bariatric surgery is nausea/vomiting (12.95% in study by Aman et al. [28]), the decreased amount of oral fluid intake is a reasonable risk factor for readmission. We came to similar conclusions basing on our material.
Lois et al., Dallal et al., and Baker et al. concluded that in case of patients with LOS > 3 days, the risk of readmission was several times more greater than in on day hospitalizations [18, 19, 33]. Longer LOS was also a predictor of readmission in the study by Sun et al. [39]. In our study, patients with prolonged LOS (> 3 days) were 2.57 times more likely to be readmitted in comparison with patients whose LOS was ≤ 3 days; however, the result was only significant in the univariate analysis. Generally, it has to be emphasized that the factors we found to be increasing the risk of readmission are associated with first 24–48 after since the beginning of surgery. Early discharge is a result of how patients manages the treatment during the early hours. This way we are able to select patients who are at potentially greater risk of readmission.
Limitation of the Study
The study did not focus on the potential differences arising from the severity of diabetes. Further study on the relationship between the severity of diabetes in bariatric patients and its impact on LOS and postoperative course is needed.
Conclusion
Decreased oral fluid intake, need for increased i.v. fluid administration on the day of surgery, and longer distance from habitual residence to bariatric center are potential risk factors for prolonged hospital stay. Intraoperative adverse events increase risk for hospital readmission. Greater oral fluid intake on the day of procedure was associated with lower risk for readmission.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of the Jagiellonian University.
Contributor Information
Piotr Major, Email: majorpiotr@gmail.com.
Michał Wysocki, Email: michal92wysocki@gmail.com.
Grzegorz Torbicz, Email: grzegorz.torbicz@gmail.com.
Natalia Gajewska, Email: natgajewska92@gmail.com.
Alicja Dudek, Email: ala.ddudek@gmail.com.
Piotr Małczak, Phone: +48 601 778 388, Email: pmmalczak@gmail.com.
Michał Pędziwiatr, Email: michal.pedziwiatr@uj.edu.pl.
Magdalena Pisarska, Email: magdalenapisarska@interia.pl.
Dorota Radkowiak, Email: dradkowiak@gmail.com.
Andrzej Budzyński, Email: andrzej.budzynski@uj.edu.pl.
References
- 1.Nguyen NT, et al. Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216(2):252–257. doi: 10.1016/j.jamcollsurg.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Matłok M, et al. Reduction of the risk of rhabdomyolysis after bariatric surgery with lower fluid administration in the perioperative period: a cohort study. 2016. [DOI] [PubMed] [Google Scholar]
- 3.Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–436. doi: 10.1007/s11695-012-0864-0. [DOI] [PubMed] [Google Scholar]
- 4.Reames BN, et al. Changes in bariatric surgery procedure use in Michigan, 2006-2013. JAMA. 2014;312(9):959–961. doi: 10.1001/jama.2014.7651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lazzati A, et al. Bariatric surgery trends in France: 2005-2011. Surg Obes Relat Dis. 2014;10(2):328–334. doi: 10.1016/j.soard.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Thorell A, et al. Guidelines for perioperative Care in Bariatric Surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40(9):2065–2083. doi: 10.1007/s00268-016-3492-3. [DOI] [PubMed] [Google Scholar]
- 7.Małczak P, et al. Enhanced recovery after bariatric surgery: systematic review and meta-analysis. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaboli PJ, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 veterans affairs hospitals. Ann Intern Med. 2012;157(12):837–845. doi: 10.7326/0003-4819-157-12-201212180-00003. [DOI] [PubMed] [Google Scholar]
- 9.Carey K, Lin MY. Hospital length of stay and readmission: an early investigation. Med Care Res Rev. 2014;71(1):99–111. doi: 10.1177/1077558713504998. [DOI] [PubMed] [Google Scholar]
- 10.Carey K. Measuring the hospital length of stay/readmission cost trade-off under a bundled payment mechanism. Health Econ. 2015;24(7):790–802. doi: 10.1002/hec.3061. [DOI] [PubMed] [Google Scholar]
- 11.Yumuk V, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8(6):402–424. doi: 10.1159/000442721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fried M, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55. doi: 10.1007/s11695-013-1079-8. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Major P, et al. Quality of life after bariatric surgery. Obes Surg. 2015;25(9):1703–1710. doi: 10.1007/s11695-015-1601-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matłok M, et al. One hundred seventy-nine consecutive bariatric operations after introduction of protocol inspired by the principles of enhanced recovery after surgery (ERAS®) in bariatric surgery. Med Sci Monit. 2015;21:791–797. doi: 10.12659/MSM.893297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sinha A, et al. Enhanced recovery after bariatric surgery in the severely obese, morbidly obese, super-morbidly obese and super-super morbidly obese using evidence-based clinical pathways: a comparative study. 2016. [DOI] [PubMed] [Google Scholar]
- 17.Carter J, et al. Predictors of hospital stay following laparoscopic gastric bypass: analysis of 9,593 patients from the National Surgical Quality Improvement Program. Surg Obes Relat Dis. 2015;11(2):288–294. doi: 10.1016/j.soard.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Dallal RM, Trang A. Analysis of perioperative outcomes, length of hospital stay, and readmission rate after gastric bypass. Surg Endosc. 2012;26(3):754–758. doi: 10.1007/s00464-011-1947-z. [DOI] [PubMed] [Google Scholar]
- 19.Lois AW, et al. The relationship between duration of stay and readmissions in patients undergoing bariatric surgery. Surgery. 2015;158(2):501–507. doi: 10.1016/j.surg.2015.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reames BN, et al. Influence of median surgeon operative duration on adverse outcomes in bariatric surgery. Surg Obes Relat Dis. 2015;11(1):207–213. doi: 10.1016/j.soard.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reyes-Pérez A, et al. Analysis of causes and risk factors for hospital readmission after Roux-en-Y gastric bypass. Obes Surg. 2016;26(2):257–260. doi: 10.1007/s11695-015-1755-y. [DOI] [PubMed] [Google Scholar]
- 22.Bergland A, Gislason H, Raeder J. Fast-track surgery for bariatric laparoscopic gastric bypass with focus on anaesthesia and peri-operative care. Experience with 500 cases. Acta Anaesthesiol Scand. 2008;52(10):1394–1399. doi: 10.1111/j.1399-6576.2008.01782.x. [DOI] [PubMed] [Google Scholar]
- 23.Geubbels N, et al. Fast track care for gastric bypass patients decreases length of stay without increasing complications in an unselected patient cohort. Obes Surg. 2014;24(3):390–396. doi: 10.1007/s11695-013-1133-6. [DOI] [PubMed] [Google Scholar]
- 24.Elliott JA, et al. Fast-track laparoscopic bariatric surgery: a systematic review. Updat Surg. 2013;65(2):85–94. doi: 10.1007/s13304-012-0195-7. [DOI] [PubMed] [Google Scholar]
- 25.Sippey M, et al. 30-day readmissions after sleeve gastrectomy versus Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(5):991–996. doi: 10.1016/j.soard.2016.01.036. [DOI] [PubMed] [Google Scholar]
- 26.Doumouras AG, Saleh F, Hong D. 30-Day readmission after bariatric surgery in a publicly funded regionalized center of excellence system. Surg Endosc. 2016;30(5):2066–2072. doi: 10.1007/s00464-015-4455-8. [DOI] [PubMed] [Google Scholar]
- 27.Chen SY, et al. Assessment of postdischarge complications after bariatric surgery: a National Surgical Quality Improvement Program analysis. Surgery. 2015;158(3):777–786. doi: 10.1016/j.surg.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 28.Aman MW, et al. Early hospital readmission after bariatric surgery. Surg Endosc. 2016;30(6):2231–2238. doi: 10.1007/s00464-015-4483-4. [DOI] [PubMed] [Google Scholar]
- 29.Abraham CR, et al. Predictors of hospital readmission after bariatric surgery. J Am Coll Surg. 2015;221(1):220–227. doi: 10.1016/j.jamcollsurg.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Kellogg TA, et al. Patterns of readmission and reoperation within 90 days after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5(4):416–423. doi: 10.1016/j.soard.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg. 2007;204(3):383–391. doi: 10.1016/j.jamcollsurg.2006.12.031. [DOI] [PubMed] [Google Scholar]
- 32.Saunders JK, et al. 30-day readmission rates at a high volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and vertical banded gastroplasty-Roux-en-Y gastric bypass. Obes Surg. 2007;17(9):1171–1177. doi: 10.1007/s11695-007-9210-3. [DOI] [PubMed] [Google Scholar]
- 33.Baker MT, et al. Length of stay and impact on readmission rates after laparoscopic gastric bypass. Surg Obes Relat Dis. 2006;2(4):435–439. doi: 10.1016/j.soard.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Khorgami Z, et al. Predictors of readmission after laparoscopic gastric bypass and sleeve gastrectomy: a comparative analysis of ACS-NSQIP database. Surg Endosc. 2016;30(6):2342–2350. doi: 10.1007/s00464-015-4477-2. [DOI] [PubMed] [Google Scholar]
- 35.Jensen-Otsu E, et al. The effect of Medicaid status on weight loss, hospital length of stay, and 30-day readmission after laparoscopic Roux-en-Y gastric bypass surgery. Obes Surg. 2015;25(2):295–301. doi: 10.1007/s11695-014-1367-y. [DOI] [PubMed] [Google Scholar]
- 36.Kelles SM, Barreto SM, Guerra HL. Mortality and hospital stay after bariatric surgery in 2,167 patients: influence of the surgeon expertise. Obes Surg. 2009;19(9):1228–1235. doi: 10.1007/s11695-009-9894-7. [DOI] [PubMed] [Google Scholar]
- 37.Nossaman VE, et al. Role of intraoperative fluids on hospital length of stay in laparoscopic bariatric surgery: a retrospective study in 224 consecutive patients. Surg Endosc. 2015;29(10):2960–2969. doi: 10.1007/s00464-014-4029-1. [DOI] [PubMed] [Google Scholar]
- 38.Garg T, et al. Characterizing readmissions after bariatric surgery. J Gastrointest Surg. 2016;20(11):1797–1801. doi: 10.1007/s11605-016-3247-3. [DOI] [PubMed] [Google Scholar]
- 39.Sun SX, Hollenbeak CS, Rogers AM. Readmissions following gastric bypass surgery. Obes Surg. 2016;26(2):269–275. doi: 10.1007/s11695-015-1736-1. [DOI] [PubMed] [Google Scholar]
- 40.Weiner RA, et al. Early post-operative complications: incidence, management, and impact on length of hospital stay. A retrospective comparison between laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg. 2013;23(12):2004–12. doi: 10.1007/s11695-013-1022-z. [DOI] [PubMed] [Google Scholar]
- 41.Pędziwiatr M, et al. ERAS protocol in laparoscopic surgery for colonic versus rectal carcinoma: are there differences in short-term outcomes? Med Oncol. 2016;33(6):56. doi: 10.1007/s12032-016-0772-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pędziwiatr M, et al. Is ERAS in laparoscopic surgery for colorectal cancer changing risk factors for delayed recovery? Med Oncol. 2016;33(3):25. doi: 10.1007/s12032-016-0738-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pędziwiatr M, et al. Laparoscopic colorectal cancer surgery combined with enhanced recovery after surgery protocol (ERAS) reduces the negative impact of sarcopenia on short-term outcomes. Eur J Surg Oncol. 2016;42(6):779–787. doi: 10.1016/j.ejso.2016.03.037. [DOI] [PubMed] [Google Scholar]
- 44.Feldheiser A, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016;60(3):289–334. doi: 10.1111/aas.12651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dorman RB, et al. Risk for hospital readmission following bariatric surgery. PLoS One. 2012;7(3):e32506. doi: 10.1371/journal.pone.0032506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Telem DA, et al. Hospital admissions greater than 30 days following bariatric surgery: patient and procedure matter. Surg Endosc. 2015;29(6):1310–1315. doi: 10.1007/s00464-014-3834-x. [DOI] [PubMed] [Google Scholar]
- 47.Tayne S, et al. Risk factors for 30-day readmissions and modifying postoperative care after gastric bypass surgery. J Am Coll Surg. 2014;219(3):489–495. doi: 10.1016/j.jamcollsurg.2014.03.054. [DOI] [PubMed] [Google Scholar]
- 48.Kassin MT, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215(3):322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lawson EH, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg. 2013;258(1):10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 50.Lawson EH, et al. Identification of modifiable factors for reducing readmission after colectomy: a national analysis. Surgery. 2014;155(5):754–766. doi: 10.1016/j.surg.2013.12.016. [DOI] [PubMed] [Google Scholar]