Abstract
Colorectal cancer (CRC) is a leading cause of death among Hispanics in the United States. Despite the benefits of CRC screening, many Hispanics are not being screened. Using a combined methodology of focus groups and discrete choice experiment (DCE) surveys, the objectives for this research were as follows: (1) to improve understanding of preferences regarding potential CRC screening program characteristics, and (2) to improve understanding of the barriers and facilitators around CRC screening with the Hispanic, immigrant community in North Carolina. Four gender-stratified focus groups were conducted and DCE surveys were administered to 38 Spanish-speaking individuals across four counties in North Carolina. In-depth content analysis was used to examine the focus group data; descriptive analyses and mean attribute importance scores for cost of screening and follow-up care, travel time, and test options were calculated from DCE data. Data analyses showed that this population has a strong interest in CRC screening but experience barrier such as lack of access to resources, cost uncertainty, and stigma. Some of these barriers are unique to their cultural experiences in the United States, such as an expressed lack of tailored CRC information. Based on the DCE, cost variables were more important than testing options or travel time. This study suggests that Hispanics may have a general awareness of and interest in CRC screening, but multiple barriers prevent them from getting screened. Special attention should be given to designing culturally and linguistically appropriate programs to improve access to healthcare resources, insurance, and associated costs among Hispanics.
Introduction
Among Hispanic populations living in the United States, colorectal cancer (CRC) is the second leading cause of death among Hispanic men and the third leading cause of death among Hispanic women [3]. Compared to their non-Hispanic White counterparts, Hispanics have lower CRC survival rates [21], higher CRC mortality rates [18], and are more likely to be diagnosed with distant-stage CRC [3]. CRC screening can effectively reduce mortality and improve survival rates through early detection [5]. Despite progress in CRC screening utilization over the past decade, prevalence of CRC screening remains low in the national Hispanic population [4].
North Carolina’s Hispanic population is one of the fastest growing Hispanic populations in the United States [2, 23], increasing nearly 400 % faster than any other state in the United States between 1990 and 2000. The majority of Hispanics in North Carolina are foreign-born with limited English proficiency [23]. Between 2000 and 2012, North Carolina saw continued growth in its Hispanic population, increasing 124.2 % over 12 years [2].
Given the established benefits of CRC screening, the growing Hispanic population in North Carolina, and low CRC screening rates in the Hispanic population, we sought a more in-depth understanding of this population’s CRC screening beliefs and preferences and the continued low rates of CRC screening. Numerous barriers to CRC screening among Hispanics have been reported in the literature [9, 14], specifically: access-related barriers (lack of transportation and inability to access care), limited opportunities for CRC screening education [9], cost of screening [9, 13], and the uncertainty of costs surrounding CRC screening [13]. Lack of insurance also plays a key role in CRC screening [4, 14]; the uninsured are less likely to receive CRC screening regardless of race or ethnicity. However, even among the insured in North Carolina, Hispanics are less likely to receive CRC screening [4, 23].
Additionally, many commonly reported barriers have been linked to issues surrounding immigration and culture. Attitudes such as perceived discomfort and embarrassment are associated with low rates of CRC screening among Hispanics [13]. Moreover, deliberate avoidance of screening is commonly expressed among Hispanics, often related to the fear of a cancer diagnosis, mistrust in providers, and a lack of confidence in the healthcare system [8]. Limited English proficiency and use of alternative medicine are negatively associated with CRC screening among Hispanics [7, 13, 14], and a lack of Spanish-speaking healthcare providers is also a reported barrier to screening [9]. The overarching goal of this research was to inform recommendations for how to effectively improve CRC screening rates within this population. Although prior research has documented these barriers, our understanding of how such knowledge can be linked to specific characteristics of screening programs is less well-developed. The objectives for this research project were as follows: (1) to improve understanding of screening program characteristics and preferences of the Hispanic immigrant community in North Carolina, and (2) to improve understanding of the barriers and facilitators around CRC screening within this population. Our work contributes to the literature on CRC screening program preferences and CRC screening knowledge among Hispanics.
Methods
Overview
We recruited, screened, and enrolled Spanish-speaking, average risk adults in Central North Carolina aged 50–75 for either a focus group discussion or discrete choice experiment (DCE) survey. Four focus groups were held to explore knowledge about CRC and barriers/facilitators to screening. Additionally, the 18 focus group participants pre-tested the DCE survey and discussed preferences for CRC screening programs. The DCE survey was then iteratively modified, finalized, and administered to 20 additional Spanish-speaking participants. These complementary approaches were well suited to gain a comprehensive understanding of the factors surrounding CRC screening and program preferences in Spanish-speakers. Focus groups enabled us to engage with groups of individuals who share a common language and query them about CRC screening. The DCE survey used selected attributes of CRC screening programs to explore relative values and program preferences by requiring individuals to make choices between hypothetical CRC screening programs. The results of these two approaches were triangulated to improve understanding of decision-making around CRC screening in this population.
Participants
Participant recruitment was targeted in four NC counties: Chatham, Orange, Wake, and Durham; each county has a growing Hispanic population between 8 and 13 % of the total population [6]. Eligibility criteria included speaking Spanish, being 50–75 years old, and having average risk for CRC (i.e., no personal or family history of CRC and no history of inflammatory bowel disease). Participants (1) had a low household income ($45,000/year or less), (2) were uninsured or publicly insured (Medicare, Medicaid, or Veterans benefits), and (3) were not up to date for CRC screening, per the United States Preventive Services Task Force screening guidelines (i.e., had colonoscopy more than 10 years ago, sigmoidoscopy more than 5 years ago, fecal occult blood test (FOBT) or fecal immunochemical test (FIT) more than 1 year ago) [25], or never screened.
All participants were recruited through a convenience sampling strategy and screened for eligibility. The majority of participants learned of the study through word of mouth from promotoras (community health educators), fliers, or through a text message sent out by a text message advertising service for Spanish-speakers, called PaseLaVoz (“Spread the Word”). Individuals interested in the study called a dedicated phone number were screened by study personnel and provided with a date and time for a focus group or an appointment to complete a survey. Recruitment for Spanish-speaking focus groups began on July 31, 2012 and concluded on February 28, 2013. In total, 18 participants attended one of four gender-stratified Spanish-language focus groups, three with female participants and one with male participants, in Orange and Wake counties. Focus groups were moderated by up to two trained bilingual individuals and held at a research center or in a grocery store community room. A focus group guide was used to assess participants’ knowledge of CRC, barriers/facilitators to screening, and CRC screening program preferences. Focus group participants also pre-tested a DCE preference survey. Focus group participants received a $35 incentive, which was later increased to $50 to motivate participation and compensate for potential difficulties in reaching data collection sites. Survey participants received a $35 incentive.
Focus Groups
All focus groups were recorded and transcribed verbatim by a transcription team. Following transcription, a professional translator translated all transcripts from Spanish to English. A bilingual member of the research team reviewed all translations for discrepancies. Once all discrepancies were resolved, the English versions of the four Spanish focus group transcripts were reviewed for accuracy, and identifiers were removed. Two research team members read all transcripts independently and identified emergent themes. A codebook was developed detailing operational code definitions and descriptions. The same two researchers independently coded all transcripts and reviewed all transcripts together, reconciling coding discrepancies. All changes to codes or the codebook were documented. ATLAS.ti version 7.1.6 (GmbH, Berlin) was used to store the focus group transcripts and to code documents. Emergent themes and illustrative quotations were identified through this iterative process and then examined based on relevance, frequency of mention, and depth of discussion. Three members of the team met in person and had phone conversations over 3 months to discuss the emergent theme identified by the analysis and detailed in the codebook to determine connections between themes. At the end of the code reconciliation process, 24 final codes remained, representing key themes expressed in the focus groups.
DCE
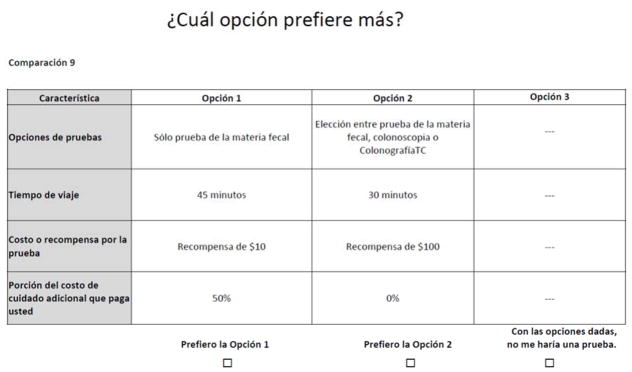
The Spanish DCE survey is a translated version of an original English CRC screening DCE survey based on previous research, expert opinion, and existing literature from a larger study conducted by our group [20]. The English DCE survey was translated into Spanish using forward translation by up to two Spanish-speakers and administered in a written format with the option of being read aloud if needed. We tested the translated DCE survey as a proof of concept to determine whether Spanish-speakers could complete the questions, given possible language and literacy barriers. A sample Spanish choice task is included in Fig. 1.
Figure 1.
The DCE survey can help illuminate which characteristics of potential screening programs would be most important in increasing screening. Using the literature and prior research, four key attributes of CRC screening programs were identified and used in the DCE survey: testing options, travel time, money paid for screening, and the portion of the cost of follow-up care paid out of pocket. A plausible range of levels was selected for each attribute. The testing options attribute included four levels: two options with a choice (choice of stool test or colonoscopy; choice of stool test, colonoscopy, or CT colonography) and two without a choice (stool test only; colonoscopy only). For the attribute travel time, the levels ranged from “no travel” to “1 hour+”. The attribute money paid for screening included both rewards and costs (copayments) within the same attribute. The levels ranged from a $100 reward to a $1000 cost, with the highest amount selected to simulate the cost of colonoscopy screening without insurance coverage. Percent follow-up cost paid ranged from 0 % to paying 100 % of the costs. Participants were given an opt-out option, “Given these options, I would not get screened”, for each choice task. Sawtooth Software Version 8 was used to design a balanced and efficient set of 16 DCE choice tasks for the English version of the survey; this number of questions has been shown in our past work to be feasible for English-speaking participants to complete [1, 19].
The results from the English DCE revealed valuable information about screening preferences of vulnerable populations. Cost variables, such as follow-up costs and screening test cost, were more important than travel time or choice of test. Findings also indicated that individuals would be more likely to be screened if given a large reward and more likely to avoid screening if screening tests or follow-up care required individuals to incur large costs [20].
DCE Analysis
We performed descriptive analyses with means and proportions using Stata version 11. The primary outcomes of interest were the mean utility levels for the four attributes and the mean DCE-calculated most important attribute. The DCE survey responses from focus groups and the individually administered surveys were analyzed together using CBC Hierarchical Bayesian (HB) component of Sawtooth Software to obtain preliminary individual-level preferences. We analyzed the data using Sawtooth Software’s CBC/HB module, as we did with the English version of the survey [20]. The module uses data from the DCE in a mixed effects multivariate, multinomial logit model to estimate the value or “utility” each participant assigns to the varying levels of the four attributes. The value associated with the opt-out choice is expressed as a constant [24].
Sawtooth Software uses a two-step HB process to determine individual-level utilities. First, average utilities are calculated for the full sample of participants, followed by the difference of each individual’s from the average. Individual utilities are then adjusted to an optimal mix of average sample utilities and individual utilities, based on the variance in the sample average and information provided by participants (Markov Chain Monte Carlo). These individual-level utility estimates are then averaged to give the population mean utilities [16, 24]. Utilities represent the relative desirability of the levels within each attribute in numerical form and are arbitrarily-scaled, zero-centered values. The higher the number, the more desirable a level is to participants, and the lower the number, the less desirable to participants [16]. Each participant’s utilities are used to calculate individual-level attribute importance scores, representing the relative importance of the four attributes, given the range of levels employed [16]. Attribute importance scores were calculated for each individual separately and then averaged for mean importance scores. The attribute that has the highest importance score from the DCE survey is considered to be “most important”.
Results
Of the 84 individuals who expressed interest in being in a focus group or taking the survey, 46 were eligible. Of these, eight participants declined participation, 18 participated in a focus group and pre-tested the survey, and 20 completed the final survey. Participant characteristics from both the focus groups and the survey are shown in Table 1 (n=38). Themean age of participants was 58 years, half were female, and most had a high school education/GED or less. The majority of participants had low household incomes (less than $30,000 per year), more than half were uninsured, and the majority had never been screened for CRC.
Table 1.
Participant Demographics (focus groups + surveys, n=38)
| Mean age (SD) | 57.8 (6.79) |
| Gender | No. (%) |
| Female | 18 (51) |
| Education | |
| Less than high school graduate | 14 (40) |
| High school graduate/GED | 8 (23) |
| Some College OR 2-year college Graduate | 11 (31) |
| 4 Year College graduate or more | 2 (6) |
| Need Help with Written Materials | |
| Always | 7 (21) |
| Sometimes | 5 (15) |
| Rarely | 7 (21) |
| Never | 14 (42) |
| Income | |
| <$30,000 | 24 (83) |
| $30,000–59,999 | 5 (17) |
| Employment | |
| Employed | 21 (64) |
| Retired | 6 (18) |
| Unemployed | 4 (12) |
| Disabled | 1 (3) |
| Other | 1 (3) |
| CRC screening status | |
| Unscreened | 22 (58) |
| Up to Date | 11 (29) |
| Insurance Statusa | |
| Uninsured | 21 (55) |
| Private Insurance | 6 (18) |
| Medicaid | 4 (11) |
| Medicare | 6 (18) |
| Medicare Supplement | 2 (6) |
Insurance status categories may overlap, as some individuals are insured by multiple policies or programs
Focus Group Results
The analysis of the focus group data revealed 24 descriptive codes, the most prevalent of which were: lack of awareness, social ties, screening cost, self-care, travel/time for test, and risk perception. Two primary emergent themes were identified during the interpretive analyses: Culture and Access. Both of these emergent themes appeared throughout the 24 codes, and neither was unique to any single code.
Culture
Culture was the most prominent emergent theme, identified as perspectives that are inherently tied to this population’s experiences as Spanish-speakers living in North Carolina. Many focus group participants expressed that their Hispanic or Latino identity influenced their access to CRC information, relationships with providers, self-care, and stigma around CRC screening. Some participants recognized that they did not have sufficient CRC knowledge but had a desire for more information tailored to their community and culture. As non-natives to the United States, some participants felt that migration led to a lack of awareness of their family health history, resulting in a lack of personal health knowledge that could potentially inform their decision to be screened.
Participants’ lack of awareness, as influenced by their Hispanic/Latino background and culture, often resulted in fear-based avoidance. One participant stated: “At least the Latinos I know, they prefer not knowing because they don’t have the means to address these problems so well.” Some participants associated this avoidant behavior with their Hispanic cultural norms. As phrased by one participant: “…we Hispanics don’t like going to the doctor.” Some male participants discussed a cultural stigma that CRC screening was embarrassing, noting that they still avoid screening even with a doctor’s recommendation, due to this stigma. This avoidance seemed to manifest itself as a means of coping due to a lack of resources, and many participants said that they self-medicate with alternative medicinal and healing therapies from their home countries. Other participants discussed lack of access and self-care challenges due to their acculturation experience in the United States.
Access
The overarching theme of access was the second emergent theme found in the data, broadly discussed as access to insurance, resources, information, and transportation. Participants expressed challenges with accessing information about health and CRC screening. One participant described feeling unsure of how to access screening information and resources: “No, I haven’t done it [screening] because I didn’t know where to go, or how much it costs, I don’t have a car, I don’t know how to drive and I was not working at that point.” Access to healthcare resources and insurance, as well as the prohibitively high costs of screening, were also widely discussed barriers across all focus groups. Many participants felt that, whether it was access to insurance or money, they were unable to gain the healthcare resources needed to take care of their health and get screened. Having insurance did not guarantee that a participant would be screened. Even with insurance, the high cost of co-pays and additional procedures, as well as cost uncertainty, prevented some participants from getting screened, which some attributed to the lifestyle and economic hardships related to living in the United States. As expressed by one participant: “Because here you live hand to mouth. If you get paid every week, the next day you already owe that…what’s the point of going to a doctor to leave–for the consultation when you won’t be able to buy the medication?” Unsure of the cost of continued primary and follow-up care, participants felt deterred from getting screened.
DCE Results
Mean utility levels from the DCE survey are shown in Table 2. The negative constant associated with “Given these options, I would not get screened” suggests a strong overall preference for participation in CRC screening programs. Individuals expressed a preference for having choice in their testing options; being given an option of two or three tests was preferred over either colonoscopy or the stool test alone. Additionally, participants preferred travel times of 30 or 45 min. Utility levels for money paid for screening showed an inconsistent pattern. Individuals exhibited preferences for the small ($10) reward for screening and for the $25 and $100 co-payments. Additionally, $1000 cost and $100 reward was not preferred by individuals. Mean attribute importance scores, which reflect the relative importance of the four attributes compared to one another, given the levels of the attributes employed, suggested that the cost variables were more important than testing options or travel time: follow-up care cost had a 42 % importance score, followed by money paid for screening (reward or copayment) at 28 %. The other attributes, testing options and travel time (both 15 %), were significantly less important given the ranges of levels tested.
Table 2.
Discrete choice experiment results of Spanish focus groups + surveys
| Attribute | Level | Meana raw utilities | Lower CI | Upper CI | Mean attributeb importance scores (CI) |
|---|---|---|---|---|---|
| Testing options | Stool test only | −0.72 | −1.30 | −0.14 | 0.15 (0.12–0.18) |
| Colonoscopy only | −1.16 | −1.70 | −0.61 | ||
| Choice: stool test OR Colonoscopy | 0.74 | 0.40 | 1.08 | ||
| Choice: stool test, Colonoscopy OR CT Colonography | 1.14 | 0.53 | 1.74 | ||
| Travel time | No Travel | −0.52 | −1.14 | 0.07 | 0.15 (0.14 – 0.17) |
| 15 min | −1.55 | −2.06 | −1.05 | ||
| 30 min | 1.51 | 1.09 | 1.93 | ||
| 45 min | 0.73 | 0.37 | 1.09 | ||
| 1 h + | −0.16 | −0.50 | 0.18 | ||
| Money paid for screening | $100 Reward | −0.17 | −0.51 | 0.16 | 0.28 (0.25 – 0.30) |
| $10 Reward | 2.09 | 1.51 | 2.68 | ||
| $0 | 0.82 | 0.32 | 1.32 | ||
| $25 Cost | 1.15 | 0.42 | 1.88 | ||
| $100 Cost | 0.96 | 0.31 | 1.61 | ||
| $1000 Cost | −4.85 | −5.37 | −4.34 | ||
| % Follow-up care cost you pay | 0% | 5.70 | 4.71 | 6.69 | 0.42 (0.38 – 0.46) |
| 5% | 3.83 | 3.27 | 4.38 | ||
| 20% | 0.26 | −0.25 | 0.77 | ||
| 50% | −2.64 | −3.21 | −2.08 | ||
| 100% | −7.14 | −8.23 | −6.06 | ||
| None | Given these options, I would not get screened | −11.62 | −13.14 | −10.10 | n/a |
Mean raw utilities indicate the relative desirability of each level within an attribute; the higher the number, the more desirable; the lower the number (the more negative), the less desirable.
The relative importance of each attribute, when the stated levels included are employed. The importance scores sum to 1.0 and can be interpreted as proportions.
Discussion
Our study explored knowledge, barriers, facilitators, and preferences around CRC screening programs in Spanish-speakers living in North Carolina using focus groups and a DCE survey. To our knowledge, this is the first DCE survey conducted among Spanish-speakers with a focus on CRC screening. Findings from the DCE coupled with the findings from the focus groups support the current literature and provide a more comprehensive understanding of preferences around CRC screening programs. Although focus group participants voiced barriers and felt deterred from CRC screening, the DCE survey indicates that CRC screening was preferred to no screening. Additionally, focus group participant expressed some awareness about certain elements related to CRC screening, such as the importance of family history, but acknowledged specific barriers, such as culturally influenced attitudes or lack of access, that continued to prevent screening. Supported by the literature [14], the DCE and focus group data taken together demonstrate basic awareness and even preference for CRC screening but highlight important barriers to screening, such as fear, lack of information about how to get screened, culturally influenced attitudes, lack of insurance, poor access to healthcare providers, and high costs of care that result in continued avoidance. These findings reveal that respondents were aware of the importance of screening but experienced multiple barriers preventing them from actually being screened. We encourage future research to explore effective facilitators to screening to help overcome screening barriers and bridge screening intention with action.
The focus groups offered rich insight into barriers and facilitators to CRC screening for this population that were not fully captured by the DCE survey. Experiences surrounding culture, migration, and acculturation were widely discussed among participants. Consistent with other studies of CRC screening barriers in this population [7, 8, 14], results showed that background, language, and culturally related attitudes affected respondents’ perspective of CRC screening, experiences with CRC-related stigma, avoidance of screening, and relationships with providers. The migration process of adjusting to the cost of living in the United States also may contribute to cost uncertainty around screening and follow-up care, creating a unique experience compared to nonimmigrant populations.
Both focus group and DCE participants expressed that out-of-pocket CRC screening costs were important, paralleling existing research [9]. In the DCE, money paid for screening and follow-up costs strongly influenced participants’ preferences. In the focus groups, costs of screening and challenges with insurance were discussed barriers, supporting the DCE findings that participants were willing to accept smaller copays ($25–100) but were not willing or able to pay larger copays ($1000). Participants may have assigned positive utility to the $25 and $100 co-payments because insured individuals often pay similar copayment amounts for medical visits, and uninsured individuals are accustomed to paying for care. Individuals also preferred to avoid paying a great deal for screening ($1000), yet did not prefer to receive moderate rewards ($100). These results may indicate that individuals do not feel it is appropriate to take a large reward for healthy behaviors, but may find it acceptable to receive a small reward ($10). Cost uncertainty was also discussed in focus groups, as participants indicated a lack of transparency of screening and follow-up care costs was a deterrent to screening. Supported by Ko et al.[13], these findings show that the costs of screening: (1) influence individual screening decisions, (2) are possibly influenced by this population’s migration experience, and (3) are confounded by individuals’ inability to understand or predict future costs.
Our findings suggest that to intervene with the Spanish-speaking population in a meaningful way, it is important to recognize this population’s needs around culture and the acculturation process. Supported by previous research [12, 15], these findings show a need to raise provider awareness for culturally and linguistically appropriate CRC communication and services for Spanish-speaking patients, a valuable step towards improving care for Spanish-speakers. As patient navigation has been deemed a successful strategy to help patients overcome CRC screening barriers [11], we recommend screening programs designed to incorporate in-person elements to target the Spanish-speakers, such as Spanish-speaking promotoras (health educators). Also, culturally and linguistically adapted multi-media CRC screening materials in the form of decision aids and education videos have been developed and shown to improve CRC-related knowledge and clinical communication [22]. Furthermore, since cost and cost uncertainty were prevalent concerns among our participants and found by Ko et al. [13], we recommend programs and providers inform patients about initial screening costs and costs that may be incurred through additional testing (e.g., surveillance colonoscopy) and treatment, as well as provide linguistically appropriate resources on interfacing with insurance providers so patients may seek information about co-payments and costs.
Additionally, insurance coverage through Medicaid or the Affordable Care Act may alleviate some of the concerns surrounding costs for some Spanish-speaking individuals. However, Hispanics make up more than 80 % of undocumented individuals who are not eligible for government assistance [17]. These populations will not benefit from governmental programs and may remain unscreened unless programs are created to aid their specific needs. Ultimately, we have an opportunity to design interventions, research, and target policies to focus more efforts in this population to better understand the needs of insured and uninsured Spanish-speaking individuals.
Further research is needed to examine the differing results between the English and Spanish screening program preferences. The Spanish DCE revealed that Spanish-speaking individuals have inconsistent opinions around travel time, whereas the English DCE participants preferred shorter or no travel times to longer travel times [20]. Regarding costs, both the English and Spanish DCE found that participants were more likely to get screened if they were given a reward. However, unlike the English DCE participants, the Spanish-speakers were deterred from both a large reward and a large copayment [20]. We see this study as an important step to provide future research with a foundation to explore transportation barriers and rewards for screening within Spanish-speakers.
Limitations
Our findings should be considered in light of several limitations. This was a preliminary study with a small sample size (n=38); a larger sample size is necessary to provide more robust results. Since the study was limited geographically and based on a convenience sample, generalizability may be limited. Also, focus group and DCE participants might be individuals who are more vested in their health, as they chose to participate and therefore might have more interest in discussing and maintaining their health than the general population. These participants also may have provided socially desirable answers as opposed to their own opinions, as Hispanics have demonstrated a higher likelihood of providing socially desirable answers when self-reporting than their White counterparts [10]. Furthermore, we did not collect information about participants’ country of origin; future research is needed to further explore the role of an individuals’ country of origin in their screening behaviors. Nevertheless, the data provide important insight into the CRC screening decision-making process among Spanish-speaking Hispanic/Latino persons and sheds light on important areas for intervention.
Overall, we believe that findings on barriers, facilitators, and preferences around CRC screening programs in Spanish-speakers are relevant to improving care and access for this population. When constructing intervention efforts, it is important to consider this population’s unique beliefs and preferences related to their cultural and acculturation experiences. Special attention should be given to their needs surrounding access to healthcare resources and insurance, as well as associated costs. With the application of the data to broader settings, we are hopeful Spanish-speaking individuals will receive, and continue to receive, recommended CRC screening services.
Acknowledgments
Primary funding for this project was sponsored by the Centers for Disease Control and Prevention, Special Interest Project, “Behavioral economics of colorectal cancer screening in underserved populations” (CDC-SIP-11-041 3U48DP001944-03S1, Co-PIs: Pignone and Wheeler). Additional funding came from the Carolina Community Network Center to Reduce Cancer Health Disparities, a NCI-CRCHD Community Network Program Center (grant # U54CA153602). Dr. Wheeler’s time on this project was further supported by the Agency for Healthcare Research and Quality (AHRQ), 1-K-12 HS019468-01 Mentored Clinical Scientists Comparative Effectiveness Development Award (PI:Weinberger; Scholar:Wheeler). Dr. Reuland’s effort was supported by North Carolina Translational and Clinical Science’s (NC TraCS) Institute and Community Academic Resources for Engaged Scholarship (CARES) through National Institutes of Health Grant Award Number 1UL1TR001111.
The authors would like to acknowledge Connor Kane and Nacire Garcia for support with data collection through the NC TraCS Institute program on Expanding Networks for Latinos through Community Engagement (ENLaCE).
References
- 1.Brenner A, Howard K, Lewis C, Sheridan S, Crutchfield T, Hawley S, Reuland D, Kistler C, Pignone M. Comparing 3 values clarification methods for colorectal cancer screening decision-making: a randomized trial in the US and Australia. J Gen Intern Med. 2014;29:507–13. doi: 10.1007/s11606-013-2701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown A, Patten E. Statistical Portrait of Hispanics in the United States, 2012. Pew Research Center; 2014. [Accessed 10 June 2014]. http://www.pewhispanic.org/files/2014/04/FINAL_Statistical-Portrait-of-Hispanics-in-the-United-States-2012.pdf. [Google Scholar]
- 3.American Cancer Society. Cancer facts & figures for Hispanics/Latinos 2012–2014. American Cancer Society; Atlanta, GA: 2012. [Google Scholar]
- 4.American Cancer Society. Cancer prevention & early detection facts & figures 2012. American Cancer Society; Atlanta, GA: 2012. [Google Scholar]
- 5.American Cancer Society. Colorectal cancer facts & figures 2011–2013. American Cancer Society; Atlanta, GA: 2011. [Google Scholar]
- 6.Hispanic Trends Project. Pew Research Center; 2013. [Accessed 10 June 2014]. Demographic Profile of Hispanics in North Carolina, 2011. http://www.pewhispanic.org/states/state/nc/ [Google Scholar]
- 7.Diaz JA, Roberts MB, Clarke JG, Simmons EM, Goldman RE, Rakowski W. Colorectal cancer screening: language is a greater barrier for Latino men than Latino women. J Immigr Minor Health. 2013;15:472–475. doi: 10.1007/s10903-012-9667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez ME, Wippold R, Torres-Vigil I, Byrd T, Freeberg D, Bains Y, Guajardo J, Coughlin SS, Vernon SW. Colorectal cancer screening among Latinos from U.S. cities along the Texas-Mexico border. Cancer Causes Control. 2008;19:195–206. doi: 10.1007/s10552-007-9085-6. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Dominic O, Lengerich EJ, Wray LA, Parrott R, Aumiller B, Kluhsman B, Renderos C, Dignan M. Barriers to CRC screening among Latino adults in Pennsylvania: ACCN results. Am J Health Behav. 2012;36:153–167. doi: 10.5993/AJHB.36.2.2. [DOI] [PubMed] [Google Scholar]
- 10.Hopwood CJ, Flato CG, Ambwani S, Garland BH, Morey LC. A comparison of Latino and Anglo socially desirable responding. J Clin Psychol. 2009;65:769–780. doi: 10.1002/jclp.20584. [DOI] [PubMed] [Google Scholar]
- 11.Jandorf L, Stossel LM, Cooperman JL, Graff Zivin J, Ladabaum U, Hall D, Thelemaque LD, Redd W, Itzkowitz SH. Cost analysis of a patient navigation system to increase screening colonoscopy adherence among urban minorities. Cancer. 2013;119:612–620. doi: 10.1002/cncr.27759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jibara G, Jandorf L, Fodera MB, DuHamel KN. Adherence to physician recommendation to colorectal cancer screening colonoscopy among Hispanics. J Gen Intern Med. 2011;26:1124–1130. doi: 10.1007/s11606-011-1727-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ko LK, Reuland D, Jolles M, Clay R, Pignone M. Cultural and linguistic adaptation of a multimedia colorectal cancer screening decision aid for Spanish-speaking Latinos. J Health Commun. 2014;19:192–209. doi: 10.1080/10810730.2013.811325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Natale-Pereira A, Marks J, VegaM, Mouzon D, Hudson SV, Salas-Lopez D. Barriers and facilitators for colorectal cancer screening practices in the Latino community: perspectives from community leaders. Cancer Control. 2008;15:157–165. doi: 10.1177/107327480801500208. [DOI] [PubMed] [Google Scholar]
- 15.Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med. 2012;27:1033–1046. doi: 10.1007/s11606-012-2044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orme BK. Getting started with conjoint analysis: strategies for product design and pricing research. 2. Research Publishers, LLC; Chicago: 2009. [Google Scholar]
- 17.Passel JS, Cohn D. Unauthorized Immigrants: 11.1 Million in 2011. [Accessed 10 June 2014];Hispanic Trends Project: Pew Research. 2012 http://www.pewhispanic.org/2012/12/06/unauthorized-immigrants-11-1-million-in-2011/
- 18.Philips BU, Jr, Belasco E, Markides KS, Gong G. Socioeconomic deprivation as a determinant of cancer mortality and the Hispanic paradox in Texas, USA. Int J Equity Health. 2013;12:26. doi: 10.1186/1475-9276-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pignone MP, Brenner AT, Hawley S, Sheridan SL, Lewis CL, Jonas DE, Howard K. Conjoint analysis versus rating and ranking for values elicitation and clarification in colorectal cancer screening. J Gen Intern Med. 2012;27:45–50. doi: 10.1007/s11606-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pignone MP, Crutchfield TM, Brown PM, Hawley ST, Laping JL, Lewis CL, Lich K, Richardson LC, Tangka F, Wheeler SB. Using a discrete choice experiment to inform the design of programs to promote colon cancer screening for vulnerable populations in North Carolina. BMC Health Serv Res. 2014;14:611. doi: 10.1186/s12913-014-0611-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinheiro PS, Williams M, Miller EA, Easterday S, Moonie S, Trapido EJ. Cancer survival among Latinos and the Hispanic Paradox. Cancer Causes Control. 2011;22:553–561. doi: 10.1007/s10552-011-9727-6. [DOI] [PubMed] [Google Scholar]
- 22.Reuland DS, Ko LK, Fernandez A, Braswell LC, Pignone M. Testing a Spanish-language colorectal cancer screening decision aid in Latinos with limited English proficiency: results from a pre-post trial and four month follow-up survey. BMC Med Inform Decis Mak. 2012;12:53. doi: 10.1186/1472-6947-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silberman P, Bazan-Manson A, Purves H, Odom CH, Easley MP, Weisner KK, DeFriese GH. North Carolina Latino health, 2003. A report from the Latino Health Task Force. N C Med J. 2003;64:113–121. [PubMed] [Google Scholar]
- 24.Sawtooth Software. The CBC/HB Systemfor Hierarchical Bayes Estimation Version 5.0. Sequim, WA: 2009. [Google Scholar]
- 25.Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]