Abstract
Adenoviral conjunctivitis may lead to subepithelial corneal infiltrates as a late complication. Herein, we aim to present a 19-year-old healthy female, who developed bilateral disciform keratitis three weeks after suffering adenoviral conjunctivitis. She presented with widespread subepithelial corneal infiltrates in addition to central corneal edema with white distinct border resembling immune stromal ring, as well as Descemet's folds and keratic precipitates in the central area. Following topical corticosteroid and ganciclovir for 10 days, her condition improved. After 1 month, she had another episode. Short-term topical corticosteroids in addition to long-term topical cyclosporine and nonpreserved artificial tears were able to prevent further recurrences.
Keywords: Adenoviridae, corneal edema, infectious keratoconjunctivitis, keratitis, viral conjunctivitis
Adenoviral keratoconjunctivitis presents at the very early stage as a pink eye and is usually nonspecific.[1] It can lead to severe red eye with edema, hyperemia, and pseudomembrane formation[2] and be complicated by symblepharon formation and subepithelial corneal infiltrates. An immune process is suspected in the etiology of subepithelial corneal infiltrates, and in some cases, these might lead to a decrease in visual acuity that might last a few months or a few years.
The treatment protocol is not definite.[3] There is still a debate on antibiotic coverage, as well as corticosteroid use. Topical virustatic agents are only mildly effective against adenoviral keratoconjunctivitis, but some reports suggested the use of ganciclovir to decrease the virus load experimentally.[4,5]
Herein, we aimed to present the case of a woman who developed disciform keratitis following presumed adenoviral conjunctivitis.
Case Report
A 19-year-old healthy female presented to another clinic with bilateral conjunctivitis following upper respiratory tract infection. According to the clinical signs of conjunctival hyperemia, chemosis, pseudomembrane formation as well as preauricular lymphadenopathy, she was diagnosed with adenoviral conjunctivitis and given topical antibiotics. Three weeks later, she developed a decrease in vision and was referred to our clinic. On examination, her visual acuity was 20/125 bilaterally. Slit lamp showed normal conjunctiva, bilateral widespread subepithelial corneal infiltrates, in addition to central corneal edema with white distinct border resembling immune stromal ring, as well as Descemet's folds and keratic precipitates in the central area [Fig. 1]. Anterior chamber was normal without any flare. Anterior segment optical coherence tomography showed corneal edema with keratic precipitates [Fig. 2]. Central corneal thickness (CCT) was 969 and 956 μm in the right and left eyes, respectively.
Figure 1.
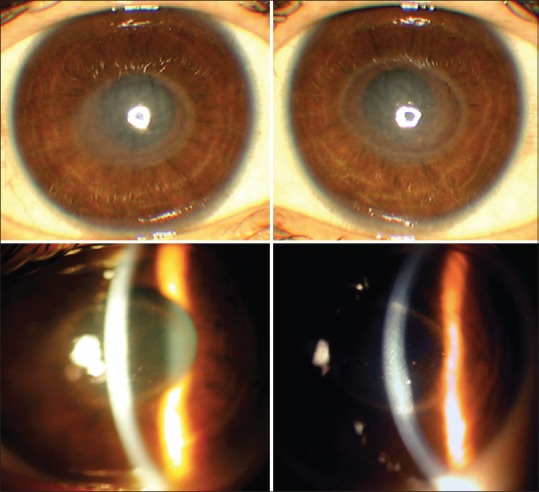
At presentation: Bilateral widespread mild subepithelial corneal infiltrates in addition to disciform keratitis with white distinct border resembling immune stromal ring, as well as central corneal edema, Descemet's folds, and keratic precipitates in the central area (upper and lower left – right eye, upper and lower right – left eye)
Figure 2.
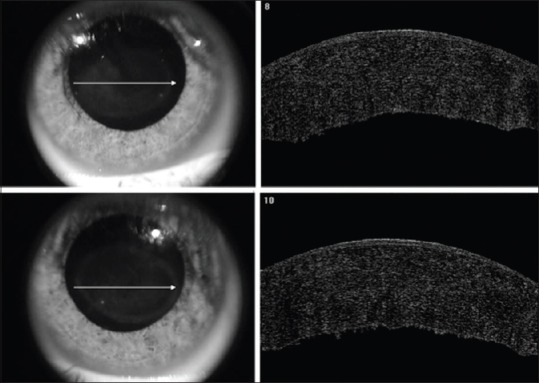
Anterior segment optical coherence tomography showed corneal edema with keratic precipitates in the right and left eyes (upper and lower, respectively)
Her systemic evaluation revealed no immunosuppression; she had neither any systemic disease nor any history of varicella vaccination. Conjunctival scrapings, staining, and cultures of both eyes for viral and bacterial etiologies were performed. In addition, a polymerase chain reaction (PCR) of anterior chamber fluid of the left eye for adenovirus and herpes simplex virus was performed. She was started on valacyclovir 500 mg 2 times a day, topical ganciclovir 5 times a day, and topical prednisolone acetate 6 times a day. There was no growth in conjunctival cultures, and PCR came negative for adenovirus and herpes simplex virus. Therefore, oral valacyclovir was stopped after 5 days. She observed significant improvement in visual acuity starting in the 1st day. Ten days after the onset of treatment, visual acuity improved to 20/40 and 20/50 in the right and left eyes, respectively. The keratic precipitates and stromal ring faded, the density of subepithelial corneal infiltrates decreased, and corneal edema resolved. The CCT decreased to 521 μm in the right and 519 μm in the left eyes at day 15. Her topical steroids were decreased gradually. One month following cessation of treatment, her visual acuity decreased in both eyes, subepithelial corneal infiltrates increased in density, and mild increase in CCT was observed [Fig. 3]. She was given topical prednisolone acetate, topical cyclosporine (0.05%), and nonpreserved artificial tears. Immediate improvement was observed, topical steroid was gradually decreased, and topical cyclosporine and nonpreserved artificial tears were continued for 6 months. No other recurrence was observed in the 6-month follow-up period.
Figure 3.
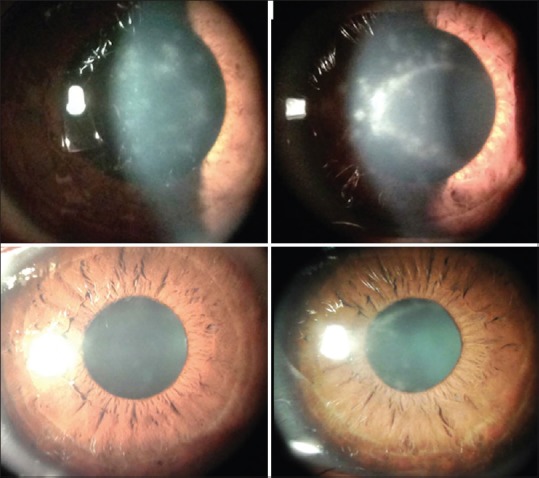
One month following cessation of treatment: Disciform keratitis with subepithelial corneal infiltrates recurred (upper left – right eye and upper right – left eye). The opacities decreased in intensity shortly after treatment (lower left – right eye and lower right – left eye)
Discussion
Adenoviral conjunctivitis usually occurs in the nature of an epidemic. Over the last year, the number of cases with adenoviral conjunctivitis increased significantly in our area (unpublished personal data). The diagnosis is usually clinical, and adenoviral kits are not commonly used in every case.
Almost one-third to 50% of adenoviral conjunctivitis cases develop subepithelial corneal infiltrates.[2] These lesions are possibly due to cellular immune reaction against viral antigens deposited in the corneal stroma. In the present case, we reported an otherwise healthy woman who had a clinical appearance resembling immune stromal keratitis. In literature, Descemet's folds were reported in adenoviral infections; however, bilateral simultaneous disciform edema was not reported very often.[6] To the best of our knowledge, this might be the first case with bilateral disciform keratitis presumably related to adenoviral keratoconjunctivitis.
In differential diagnosis, we considered herpetic and cytomegalovirus keratitis. Although herpetic infections usually occur unilaterally, bilateral cases were also reported.[7] At the initial appearance of disciform keratitis, we added short-term systemic and topical antivirals to topical steroids, due to the possible etiology of herpetic stromal keratitis. Following negative PCR results, we were able to stop antivirals. In the present case, we did not perform PCR for cytomegalovirus since the clinical findings did not resemble cytomegalovirus keratitis, in that keratic precipitates were not linear or coin shaped,[8] and short-term antiviral treatment in addition to topical steroids was able to resolve the disciform keratitis.
In the treatment of subepithelial corneal infiltrates, topical use of corticosteroids was reported to accelerate the visual recovery although they were claimed not to affect the final outcome.[9] Our case, who presented with disciform keratitis, responded favorably to topical steroids, most probably because the disciform lesions were an immunological response of corneal stroma. At the recurrence of disciform keratitis following cessation of treatment, topical corticosteroids could be used only in the short term with the addition of long-term topical cyclosporine. Topical 0.05% to 2% cyclosporine was reported to reduce the formation of subepithelial corneal infiltrates.[10] However, the result of decrease of subepithelial corneal infiltrates in adenoviral keratitis was probably more related to the use of steroids than cyclosporine.[11]
Conclusion
We believe that in cases with adenoviral keratoconjunctivitis, immune response could be so intense that it might lead to disciform keratitis. In such cases, temporary topical steroid, followed by cyclosporine, use might be helpful, as in our case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kaufman HE. Adenovirus advances: New diagnostic and therapeutic options. Curr Opin Ophthalmol. 2011;22:290–3. doi: 10.1097/ICU.0b013e3283477cb5. [DOI] [PubMed] [Google Scholar]
- 2.Jhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB. Adenoviral keratoconjunctivitis. Surv Ophthalmol. 2015;60:435–43. doi: 10.1016/j.survophthal.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Meyer-Rüsenberg B, Loderstädt U, Richard G, Kaulfers PM, Gesser C. Epidemic keratoconjunctivitis: The current situation and recommendations for prevention and treatment. Dtsch Arztebl Int. 2011;108:475–80. doi: 10.3238/arztebl.2011.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trousdale MD, Goldschmidt PL, Nóbrega R. Activity of ganciclovir against human adenovirus type-5 infection in cell culture and cotton rat eyes. Cornea. 1994;13:435–9. doi: 10.1097/00003226-199409000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Huang J, Kadonosono K, Uchio E. Antiadenoviral effects of ganciclovir in types inducing keratoconjunctivitis by quantitative polymerase chain reaction methods. Clin Ophthalmol. 2014;8:315–20. doi: 10.2147/OPTH.S55284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsagkataki M, Trainor E, Kaye LC, Hopkins MJ, Kaye SB. Adenoviral keratoconjunctivitis associated with stromal oedema and keratic precipitates. Clin Exp Ophthalmol. 2013;41:715–6. doi: 10.1111/ceo.12076. [DOI] [PubMed] [Google Scholar]
- 7.Souza PM, Holland EJ, Huang AJ. Bilateral herpetic keratoconjunctivitis. Ophthalmology. 2003;110:493–6. doi: 10.1016/S0161-6420(02)01772-4. [DOI] [PubMed] [Google Scholar]
- 8.Koizumi N, Inatomi T, Suzuki T, Shiraishi A, Ohashi Y, Kandori M, et al. Clinical features and management of cytomegalovirus corneal endotheliitis: Analysis of 106 cases from the Japan corneal endotheliitis study. Br J Ophthalmol. 2015;99:54–8. doi: 10.1136/bjophthalmol-2013-304625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laibson PR, Dhiri S, Oconer J, Ortolan G. Corneal infiltrates in epidemic keratoconjunctivitis. Response to double-blind corticosteroid therapy. Arch Ophthalmol. 1970;84:36–40. doi: 10.1001/archopht.1970.00990040038010. [DOI] [PubMed] [Google Scholar]
- 10.Asena L, Şıngar Özdemir E, Burcu A, Ercan E, Çolak M, Altınörs DD, et al. Comparison of clinical outcome with different treatment regimens in acute adenoviral keratoconjunctivitis. Eye (Lond) 2017;31:781–7. doi: 10.1038/eye.2017.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maychuk DY, Vasil’eva OA, Russu LI, Mezentseva MV. Clinical and immunological comparisons of therapeutic regimens for corneal infiltrates secondary to adenoviral keratoconjunctivitis. Vestn Oftalmol. 2015;131:49–55. doi: 10.17116/oftalma2015131449-55. [DOI] [PubMed] [Google Scholar]


