Abstract
Purpose:
The objective of the study is to compare the frequency of Demodex on the eyelash follicle of patients with rosacea and referents without rosacea or ophthalmological disorders.
Methods:
This is a comparative, open, observational, and cross-sectional study that included 41 patients diagnosed with rosacea and 41 referents without rosacea diagnosis or ophthalmic alterations. The individuals underwent a slit-lamp examination in which two eyelashes per eyelid were removed with fine forceps. The presence of Demodex was sought by direct visualization under a light microscope. The results were expressed as “positive” when at least one mite on one lash was found and “negative” when no mite was identified. Chi-square test was used to compare the presence of mites in both groups.
Results:
Eighty-two study individuals (45 females and 37 males) were included, of which 41 patients were diagnosed with rosacea and 41 were without rosacea or ophthalmic alterations. The average mean age was 37 years with a minimum of 19 and a maximum of 87 years. Of the 41 patients with rosacea, 31 had erythematotelangiectatic rosacea and 10 had papulopustular rosacea. There were no patients with phymatous or ocular rosacea. The presence of Demodex was found in 32 patients: 24 patients with rosacea diagnosis (16 of the erythematotelangiectatic subtype and 8 of papulopustular subtype) and 8 patients without rosacea or ophthalmic alterations (P ≤ 0.001).
Conclusion:
Rosacea was found to be a statistically significant risk factor for Demodex infestation in eyelashes, irrespective of age and sex, with a higher prevalence in papulopustular variety.
Keywords: Blepharitis, Demodex, frequency, rosacea
According to dermatology literature, Demodex is found to colonize normal human skin everywhere; on an average, the Demodex population is approximately 5/cm2 of skin in the adult population.[1] They usually do not result in any dermatological problems, but when the parasites penetrate the dermis, they can cause acne, rosacea, and folliculitis. The symptoms aggravate with an increase in their population.[2] Rosacea is a disease of multifactorial origin, and the individual characteristics of the patient can modify the severity of the inflammatory response to Demodex.[3] Finding large quantities of Demodex may play an important role in the pathogenesis of rosacea in addition to other trigger factors.[4]
In ophthalmology, Demodex is thought to be an etiological factor in chronic blepharitis, conjunctival inflammation, and meibomian gland dysfunction. Furthermore, Demodex has also been reported to cause unusual ocular manifestations, such as superficial corneal neovascularization, marginal corneal infiltration, phlyctenule-like lesions, superficial corneal opacity, and nodular corneal scars, especially in patients with ocular rosacea.[5]
The objective of the present study is to compare the frequency of Demodex in eyelash follicles in patients with or without a clinical diagnosis of rosacea.
Methods
A comparative, open, observational, transversal, and cross-sectional study was carried out in which 82 patients were included in the study. The first group consisted of 41 patients diagnosed with rosacea by the dermatology service, and the second group consisted of 41 referents without diagnosis of rosacea or ophthalmological complaints.
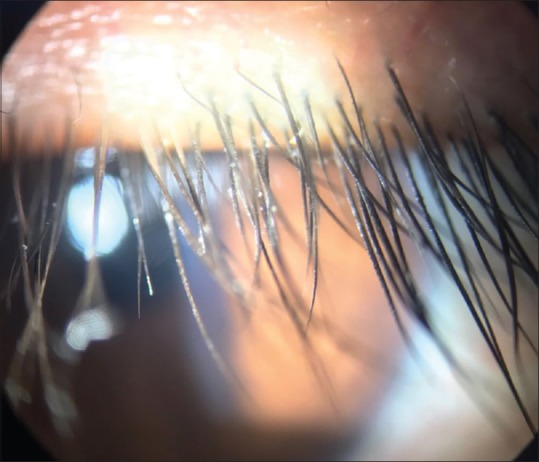
Both study groups were asked to fill the informed consent to participate in this protocol, which was followed by an interrogation carried out to capture information and slit-lamp evaluation with a magnification of ×25. A total of eight eyelashes per eye were excised per patient, four eyelashes per eye. They were extracted with fine forceps and placed separately on each end of a slide. A coverslip was placed on the top of the eyelashes after coating them with immersion oil. The presence and counting of Demodex were performed in the samples by light microscopy with a magnification of × 40 and × 100 [Figs. 1 and 2]. Results were reported as positive (presence of at least one Demodex in a tab) or negative (nonidentifiable). Patients with Demodex were treated with selenium sulfide lotion mixed with water on a concentration 1:7 applied directly to the face and eyelashes for 1 month once at night. It was found that shorter treatments had an increased risk of failure.
Figure 1.

Demodex attached to an eyelash
Figure 2.

Demodex mites
For the statistical calculations, the IBM SPSS Statistics 22.0 (IBM Corp. Released 2013. IBM SPSS Statistics for Mac, Version 22.0. Armonk, NY: IBM Corp.) for Mac program was used. Chi-square test was carried out, reporting a contingency table to analyze if a difference existed between the presence of Demodex and having rosacea or not.
Results
A total of 82 individuals were studied, of which 45 were women (54.9%) and 37 were men (45.1%) with a minimum age of 19 years and a maximum of 87 years. They were divided into two groups: 41 patients with rosacea diagnosis and 41 patients without rosacea diagnosis or ophthalmological alterations. In the group of patients with rosacea, 31 patients (37.8%) had erythematotelangiectatic rosacea, 10 patients (12.2%) had papulopustular rosacea, and no patient presented with either ocular or phymatous rosacea.
Of the total number of patients, the presence of Demodex was found in 32 (39%). Demodex was present in 8 patients (19.5%) with no diagnosis of rosacea or ophthalmologic alterations, whereas the same mite was found in 24 patients (58.5%) with a diagnosis of rosacea (16 of them with erythematotelangiectatic rosacea and 8 with papulopustular rosacea) (P < 0.001).
All patients underwent slit-lamp examination. The findings for the first group (rosacea) were the following: seven patients had thick meibomian secretion, eight had collarettes and/or scales on eyelashes [Fig. 3], one had madarosis, five had red eye, four had eyelid margin telangiectasia, two had conjunctival papillae, and one had thick eyelid margin. For the second group (no rosacea), three patients had thick meibomian secretion and two patients had scales on eyelashes and with telangiectasia.
Figure 3.
Scales on eyelashes
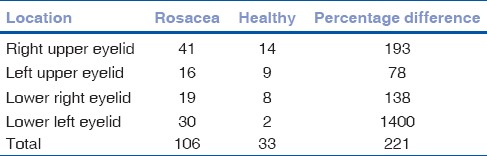
A total of 139 Demodex mites could be located on patients’ eyelashes (106 with rosacea vs 33 healthy). The distribution was as follows: 55 (40%) on the right upper eyelid, 25 (18%) on the upper left eyelid, 27 (19%) on the lower right eyelid, and 32 (23%) on the lower left eyelid [Table 1]. The average number of Demodex mites per patient was similar between groups (4 per patient).
Table 1.
Distribution of Demodex
Discussion
There is a statistically significant association between Demodex density and rosacea. Forton and Seys in 1993, through a study of 49 patients with rosacea, evaluated biopsies of 1 cm2 of skin showing an average mite density of 10.8/cm2 compared to 0.7/cm2 in control patients (P < 0.001). The presence of Demodex was also demonstrated with facial pruritus with or without erythema.[6]
There is currently no information linking rosacea and Demodex to eyelash follicles. Among our results, we obtained a frank predominance of this mite in patients with rosacea, which opens new doors on the intimate relationship that may exist between an external agent and the immune reaction in the pathophysiology of rosacea. Likewise, in our study, 80% of patients with papulopustular rosacea presented Demodex infestation, as opposed to 51% in patients with erythematotelangiectatic rosacea. This finding supports the theory that this distribution is due to the fact that sebum acts as an energy source for Demodex.[7]
In 1998, Erbaǧci and Ozgöztaşi studied 38 patients with rosacea and 38 healthy patients as a control group. They performed skin surface biopsies in search of this mite. Their findings were similar to our study, and the average number of mites in the rosacea group was significantly higher. The cheek was the area that showed the most infestation of the mite.[4]
Divani et al. carried out skin scrapings from the base of the eyelashes in 69 patients with therapy-resistant chronic blepharitis and compared them with 30 healthy individuals. They found that 66% of individuals in the affected group had Demodex mites compared to 33% in the control group.[8] In this study, diagnosis of rosacea was not mentioned in the patients with chronic blepharitis, and 69 patients presented with ocular symptoms such as redness, pruritus, foreign body sensation, conjunctival inflammation, and madarosis.[8]
In the study by Rodríguez et al. in 2005, the incidence of infestation of this mite was investigated in 20 patients with chronic blepharitis and 105 patients as a control group. Ten eyelashes per eye were extracted in both the groups, which were observed under a microscope. They found that the density of Demodex was greater in patients with chronic blepharitis than in controls (0.69 mites/eyelash vs 0.08 mite/eyelash P = 0.006).[9] However, it was not directly studied if patients had concomitant rosacea.
Li et al. analyzed 59 patients with positive serum immunoreactivity for Bacillus oleronius and found a significant correlation between serum immunoreactivity and the presence of facial rosacea, eyelid edge inflammation, and Demodex infestation. The Demodex count was significantly higher with facial rosacea. A significant relationship was also found between facial rosacea and palpebral border inflammation.[10] O’Reilly et al. looked for the relationship between this bacillus and the corneal epithelium response to its presence in a patient, concluding that corneal epithelial cells with exposure to B. oleronius proteins cause an aberrant scarring response. This suggests the likely relationship between a high density of Demodex in rosettes of patients with rosacea and the development of corneal ulcers.[11] The question that arises from this protocol is whether there is a relationship between Demodex, B. oleronius, and rosacea. Perhaps, a series of factors of these two pathogens initiates an inflammatory cascade triggering the characteristic changes of rosacea. This opens the door to deeper studies as there is a symbiosis between both pathogens and exacerbates the inflammatory responses that produce chronic blepharitis.
There is a strong association between a higher concentration of the Demodex mite and the clinical diagnosis of rosacea. The role of this parasite in the pathophysiology of this disease as well as in its different subtypes has not been defined. In this protocol, the different subspecies of Demodex were not identified, which leads us to consider the possibility that there may be differences between them and their roles in the initial inflammatory reaction of rosacea. This analysis opens the possibility of other studies, such as therapeutic management for Demodex, treatment comparison at the ocular level, assessing whether treating Demodex infestation modifies rosacea disease course at both facial and ocular levels as well as its impact at the ocular level.
Conclusion
Rosacea proves to be a significant risk factor for Demodex infestation in the eyelashes. This is independent of age and sex and has a higher prevalence in the papulopustular variety. It is acceptable to search for Demodex infestation in patients diagnosed with rosacea. Similarly, patients with chronic blepharitis may be questioned for common rosacea symptoms such as flushing and facial redness as the treatment for Demodex in rosacea may improve their clinical presentation without necessarily being an ocular rosacea. Identifying a higher frequency of Demodex in hair follicles of patients with rosacea could have therapeutic implications that would lead to improvement of the symptomatology and probably modification of the course of the disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lacey N, Kavanagh K, Tseng SC. Under the lash: Demodex mites in human diseases. Biochem (Lond) 2009;31:2–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, et al. Demodicosis and rosacea: Epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52:74–87. doi: 10.1016/j.jaad.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 3.Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC, et al. Ocular surface discomfort and demodex: Effect of tea tree oil eyelid scrub in demodex blepharitis. J Korean Med Sci. 2012;27:1574–9. doi: 10.3346/jkms.2012.27.12.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erbaǧci Z, Ozgöztaşi O. The significance of demodex folliculorum density in rosacea. Int J Dermatol. 1998;37:421–5. doi: 10.1046/j.1365-4362.1998.00218.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51:2906–11. doi: 10.1167/iovs.09-4850. [DOI] [PubMed] [Google Scholar]
- 6.Forton F, Seys B. Density of demodex folliculorum in rosacea: A case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993;128:650–9. doi: 10.1111/j.1365-2133.1993.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 7.Elston DM. Demodex mites: Facts and controversies. Clin Dermatol. 2010;28:502–4. doi: 10.1016/j.clindermatol.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Divani S, Barpakis K, Kapsalas D. Chronic blepharitis caused by demodex folliculorum mites. Cytopathology. 2009;20:343–4. doi: 10.1111/j.1365-2303.2009.00639.x. [DOI] [PubMed] [Google Scholar]
- 9.Rodríguez AE, Ferrer C, Alió JL. Chronic blepharitis and demodex. Arch Soc Esp Oftalmol. 2005;80:635–42. doi: 10.4321/s0365-66912005001100004. [DOI] [PubMed] [Google Scholar]
- 10.Li J, O’Reilly N, Sheha H, Katz R, Raju VK, Kavanagh K, et al. Correlation between ocular demodex infestation and serum immunoreactivity to bacillus proteins in patients with facial rosacea. Ophthalmology. 2010;117:870–70. doi: 10.1016/j.ophtha.2009.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Reilly N, Gallagher C, Reddy Katikireddy K, Clynes M, O’Sullivan F, Kavanagh K, et al. Demodex-associated bacillus proteins induce an aberrant wound healing response in a corneal epithelial cell line: Possible implications for corneal ulcer formation in ocular rosacea. Invest Ophthalmol Vis Sci. 2012;53:3250–9. doi: 10.1167/iovs.11-9295. [DOI] [PubMed] [Google Scholar]


