Abstract
Deep vein thrombosis (DVT) is a serious medical condition that needs prompt diagnosis and treatment. The invasive gold standard contrast venography has largely been replaced by venous ultrasonography which is currently the imaging modality of choice for DVT diagnosis. Radionuclide venography (RNV) is an alternative test for DVT, but a few studies have directly compared RNV with venous ultrasonography. This study aims to determine the agreement between RNV and venous ultrasonography for diagnosis of DVT and to determine the predictive value of different RNV findings for the prediction of DVT as detected by venous ultrasonography. Imaging results from patients who underwent both RNV and venous ultrasonography for suspected DVT no more than 1 week apart were reviewed. Results from both modalities were compared to determine inter-modality agreement. A total of 121 venous segments from 102 lower limbs of 75 patients could be compared. The prevalence of DVT as detected by venous ultrasonography was 39%. RNV and venous ultrasonography had moderate agreement (73.6% agreement, κ =0.48, P < 0.0001). The absence of radiotracer activity from a deep venous segment had a positive predictive value (PPV) of 100% for DVT. Other findings such as isolated great saphenous vein activity had a lower PPV. The negative predictive value of RNV is 97.5% with only one patient out of forty with normal RNV found to have DVT by venous ultrasonography, which suggests that DVT can virtually be excluded in patients with normal RNV.
Keywords: Deep vein thrombosis, Doppler ultrasonography, radionuclide imaging, radionuclide venography, venous thrombosis
Introduction
Deep vein thrombosis (DVT) is a clinical condition, in which blood clots form in the lumen of the deep vein most commonly in the lower extremity and to a lesser extent the upper extremity. Predisposing risk factors of DVT include advancing age, pregnancy, active cancer, immobilization, recent surgery, obesity, smoking, medication such as oral contraceptives, and hypercoagulability states.[1] The overall incidence of DVT is approximately 100 cases per 100,000 persons.[2] Pulmonary embolism occurs when clots dislodge from the deep vein and obstruct the pulmonary arteries, which can have a mortality rate exceeding 15% in the first 3 months of diagnosis.[3] Approximately half of the patients with PE have concomitant DVT;[4] thus, prompt and accurate diagnosis of DVT is crucial to permit timely treatment and prevent its complications. Diagnosis of DVT begins with clinical examination. Several clinical scores have been developed to gauge the pretest probability of DVT.[5] However, the mortality rate of patients with asymptomatic DVT may be as high as 14%.[6] Laboratory testing with D-dimer has sensitivity exceeding 90% but specificity of approximately 50%, so it is used for exclusion but not for confirmation of DVT.[7] The imaging gold standard for diagnosis of DVT is contrast venography,[8,9] which due to its invasive nature is currently less frequently performed. The current imaging modality of choice for the detection of DVT is venous ultrasonography which is a noninvasive method that does not involve ionizing radiation or administration of radiographic contrast media.[10] The sensitivity and specificity of venous ultrasonography for diagnosis of DVT varies between studies, but overall, the modality has an acceptably high discrimination power, especially for DVT of the proximal veins.[11] The current guidelines recommend performing venous ultrasonography in patients with a high pretest probability of DVT as determined by clinical scoring.[12] However, technical difficulties and false negative venous ultrasonography results are possible in obese patients or patients with markedly edematous limbs.[13] Ultrasound probe placement may be difficult in patients with orthopedic casts, with instrumentation, or having extensive skin wounds.[10] Radionuclide venography (RNV) is a nuclear medicine imaging technique that has been used for the diagnosis of DVT. The radiotracer technetium-99m macroaggregated albumin (Tc-99m MAA) is intravenously injected simultaneously with imaging of the extremities with a gamma camera. Disruption of radiotracer flow in the deep vein or the presence of collateral veins suggests that DVT is present.[14] The accuracy of RNV has been found to exceed 90% when using contrast venography as the gold standard.[14,15] Although not commonly performed, RNV should be considered as an alternative test when venous ultrasonography cannot be performed or is limited. However, there have been no recent studies that compared between these two imaging modalities; therefore, the objective of this study is to determine the agreement between RNV and venous ultrasonography in the detection of DVT of the lower limb.
Materials and Methods
Patients
This retrospective, analytical, observational study has been approved by Khon Kaen University Institutional Review Board (reference number: HE591286). Patient imaging records were searched from the imaging database of the Department of Radiology, Faculty of Medicine, Khon Kaen University. Inclusion criteria are (1) patients 18 years of age and older, (2) both RNV and venous ultrasonography were performed for diagnosis of lower limb DVT, and (3) RNV and venous ultrasonography were done no more than 1 week apart. Sample size was calculated per the methods previously described,[16] with estimation of the prevalence of DVT being 20% in the cohort and that RNV and venous ultrasonography have a similar detection rate. The lowest kappa value that would be acceptable was designated at 0.5 and the expected value was estimated to be 0.8. Type I error rate was set at 0.05 while the power was set at 80%. This yielded a minimum sample size of 66 comparisons.
Radionuclide venography
RNV was performed using the radiotracer Tc-99m MAA. Imaging was done using either Vertex V60 EPIC HP dual-headed gamma camera (ADAC, CA, USA) or Genesys single-headed gamma camera (ADAC, CA, USA) equipped with low-energy general purpose collimator with a 64 × 64 imaging matrix with an energy peak set at 140 keV ± 10%. First, the patient was placed supine on the gamma camera bed. Elastic tourniquets were tied around both ankles; then, 3–5 mCi of Tc-99m MAA in a volume of 10 mL was injected into the superficial veins of each foot simultaneously. Planar scintigraphic images were acquired at the same time of injection of the radiotracer starting from the feet and gradually moving up to the lung base. Images were acquired in the anterior and posterior projections when the dual-headed gamma camera was used and in the anterior projection when the single-headed gamma camera was used. Careful coordination between the technologist controlling the gamma camera and the nurse injecting the radiotracer was maintained to assure that the radiotracer injection finished at the same time the gamma camera reached the lung base. The planar images obtained were examined for the evidence of DVT. Abnormal findings noted include absence or reduced radiotracer in the deep venous drainage track of the lower extremity and presence of radiotracer activity in the superficial collateral veins of the lower extremity, pelvic region, or abdominal wall.
Venous ultrasonography
Ultrasonography of the lower extremities was carried out using one of the three ultrasound systems including Xario XG (Toshiba Medical Systems, Tokyo, Japan), Prosound F75 (Hitachi Aloka, Tokyo, Japan), or LOGIQ 9 (GE Healthcare, IL, USA). Both B-mode and Doppler mode were performed. Findings indicative of DVT on B-mode ultrasonography examinations include the presence of intraluminal filling defect, noncompressible venous segment. In color Doppler mode, absent color flow, loss of phasic waveform, absence of increased flow in response to augmentation, and increased flow in superficial veins are indicative of DVT. When possible, chronicity of DVT was specified. Acute DVT typically presents with loosely attached intraluminal hypoechoic clot in distended venous segments with generally the absence of collateralization. Subacute DVT presents as isoechoic clots firmly attached to the venous wall which has started to retract to normal size with possible collateralization. However, chronic DVT has hyperechoic clots that are firmly attached to the venous wall with venous lumen smaller than the usual size and possible recanalization and collateralization. Ultrasonography images and reports in the picture archiving and communication system were reviewed, and the abnormal findings and sonographic diagnosis of the presence or absence of DVT were noted.
Statistical analysis
Patient characteristics are represented as mean, standard deviation, and percentage. Correlation between RNV and venous ultrasonography was determined using percent agreement and Cohen's kappa. The power of various abnormalities seen on RNV to predict positive venous ultrasonography was determined. Statistical analysis was carried out using Stata version 10 (StataCorp LLC, TX, USA). A P < 0.05 designates statistical significance.
Results
Patients characteristics
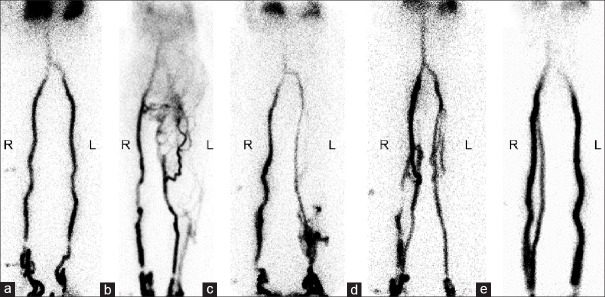
From January 1, 2012, to May 31, 2016, there were 75 patients who underwent both RNV and venous ultrasonography for suspected lower extremity DVT. Characteristics of patients included in the study are described in Table 1. The cohort has a slight female predilection, with an average age of 57.8 ± 17.1 years. Approximately 41.3% of the patients had underlying cancer, 9.3% had systemic lupus erythematosus, while 8.0% had previous thrombotic disease. Of the 75 patients, RNV was technically adequate to evaluate 75 right lower extremities from iliac vein down to the calf but could evaluate 72 left lower extremities due to inability to cannulate the veins at the left foot in three cases. This makes a total of 147 extremities that are evaluable by RNV. The inferior vena cava (IVC) was evaluable in 71 RNV studies with four studies having poor IVC radiotracer activity due to technical errors. On the other hand, of the 75 patients, venous ultrasonography was performed in both extremities in 27 patients, only the right extremity in 25, and only the left extremity in 23 patients, which makes a total of 102 limbs being examined by venous ultrasonography. When dividing the venous segments into veins of the iliac region, thigh region, and calf region, all 102 extremities had ultrasonography examination of the thigh veins, while the iliac veins and calf veins were examined in only 14 and 5 limbs, respectively. This results in a total of 121 venous segments that underwent scrutiny by both RNV and venous ultrasonography, which could be compared. Table 2 describes RNV and venous ultrasonography performed in this cohort.
Table 1.
Characteristics of 75 patients who underwent both radionuclide venography and venous ultrasonography for suspected deep vein thrombosis
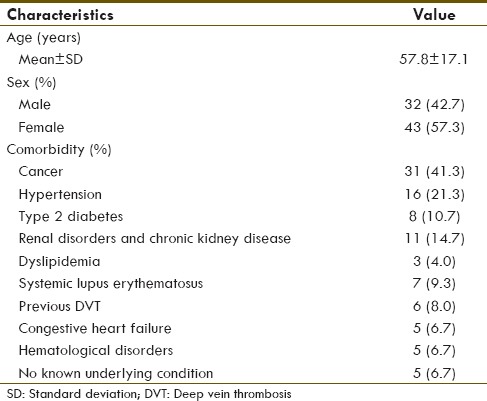
Table 2.
Description of radionuclide venography and venous ultrasonography performed in 75 patients
Venous ultrasonography findings
As described in Table 2, of the 102 extremities on which venous ultrasonography was performed, some form of DVT was found in 40 extremities resulting in the prevalence of DVT of 39% as detected by venous ultrasonography. Among the types of DVT found, acute DVT and chronic DVT each accounted for approximately one-third, while the remaining third are cases which DVT was detected, but chronicity of the clot was not able to be determined. Subacute DVT accounted for only three cases.
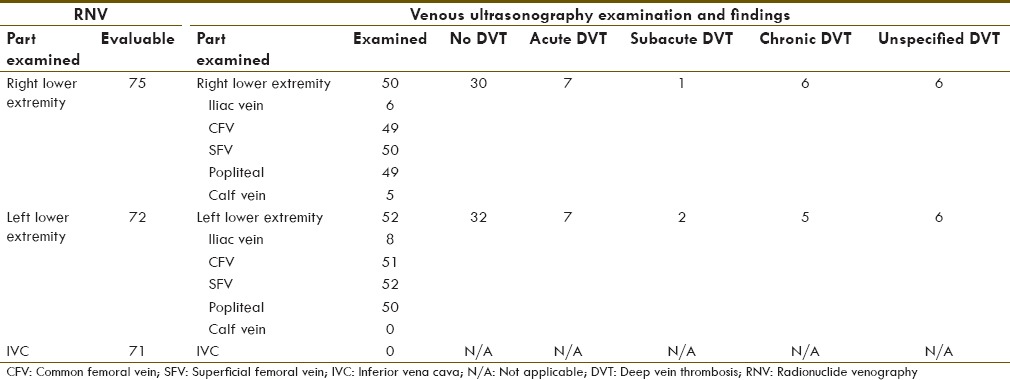
Radionuclide venography findings
There are several abnormal findings that can be encountered on RNV. A normal lower extremity RNV should demonstrate intense symmetrical radiotracer activity in the deep venous system of bilateral lower extremities from the calves up to the thighs, iliac veins, and IVC without interruption or reduction of radiotracer activity or the presence of radiotracer activity in any collateral veins at any level. Details of abnormal findings are described in Table 3. Of the 121 venous segments included in the analysis, 56 segments (46.3%) were completely normal whereas 65 segments (53.7%) had one or more abnormal findings. The most common abnormal finding is the presence of radiotracer activity in collateral draining veins which was found in approximately half of the evaluated extremities. Absent or reduced radiotracer activity which is considered a finding specific to deep venous obstruction was found in two-thirds of the iliac vein level and about a quarter of thigh vein level. Figure 1 illustrates some examples of normal and abnormal findings that can be found on RNV studies.
Table 3.
Description of abnormal findings on radionuclide venography of the evaluable iliac, thigh, and calf deep venous segments
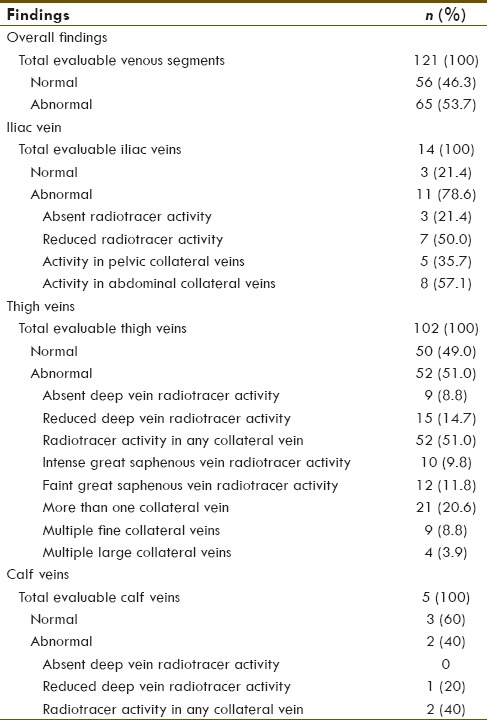
Figure 1.
(a) Normal radionuclide venography study showing radiotracer passage through deep veins bilaterally; (b) left deep vein thrombosis with reduced activity in the deep vein with activity in the great saphenous vein and multiple small collaterals; (c) left deep vein thrombosis with the absence of radiotracer from the deep vein and shunting through the great saphenous vein; (d) bilateral deep vein thrombosis with reduced deep vein activity and activity in multiple bilateral collateral veins; (e) normal radiotracer passage through deep veins bilaterally with activity in the right great saphenous vein but venous ultrasonography reveals no deep vein thrombosis
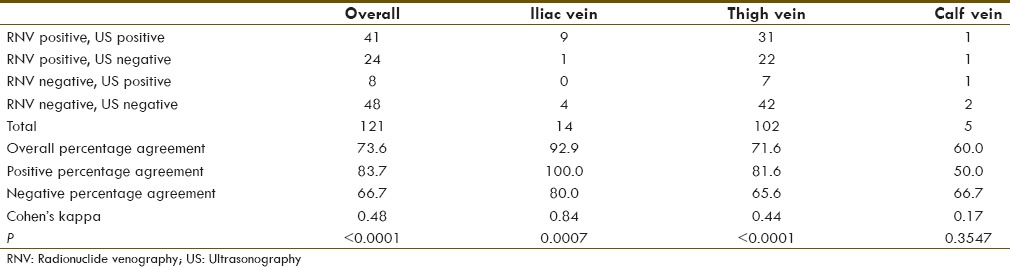
Agreement between radionuclide venography and venous ultrasonography
The overall agreement between venous ultrasonography and RNV was moderate with a percent agreement of 73.6% and kappa of 0.48 (P < 0.0001) as shown in Table 4. When analyzed by venous levels, the two modalities were in highest agreement for the diagnosis of iliac vein thrombosis with a kappa of 0.84 and a significant P value (P = 0.0007) despite the small number of venous segments compared. Agreement was poorest for calf veins although only five segments could be compared. Moderate agreement was found for thigh veins which are the majority of venous segments compared in this study.
Table 4.
Agreement between radionuclide venography and venous ultrasonography
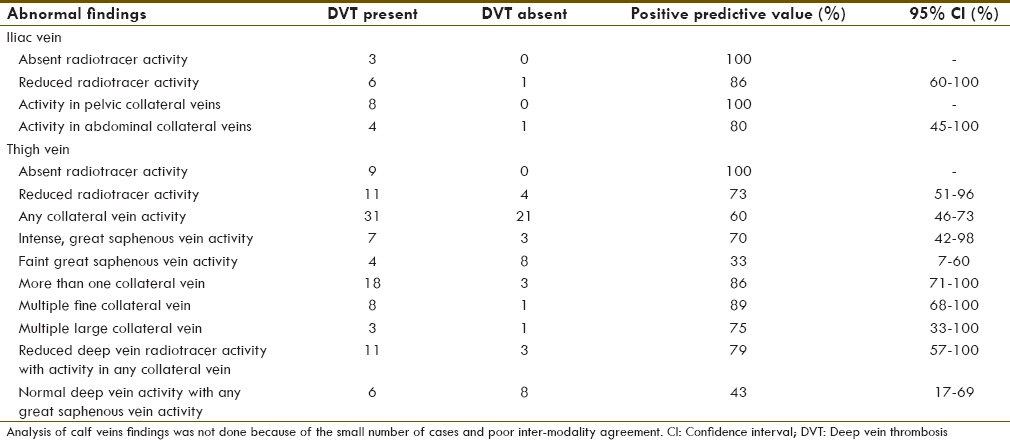
Predictive value of radionuclide venography
Since there are several abnormal findings in RNV that have been associated with the presence of DVT, cases with positive venous ultrasonography were analyzed to find the positive predictive value (PPV) of different RNV findings in predicting DVT as detected by venous ultrasonography for each venous level, as detailed in Table 5. The finding that most strongly and perfectly predicts the presence of DVT is the absence of radiotracer activity from a venous segment. Findings with also high PPV include reduction of radiotracer activity in a venous segment and presence of radiotracer activity in more than one collateral vessel, regardless of intensity and characteristics. Findings with lower PPV include radiotracer activity in the great saphenous vein but with normal radiotracer activity in the deep vein. The negative predictive value (NPV) of RNV was also assessed. Among the 102 lower limbs examined, forty were completely normal. Of the normal cases, only one case was found to have subacute DVT despite normal RNV findings, which equates to an NPV of 97.5%.
Table 5.
Predictive value of abnormal finding in radionuclide venography in predicting the presence of deep vein thrombosis as detected by venous ultrasonography
Discussion
Accurate and timely diagnosis of DVT is important to guide management decisions to reduce patient morbidity and mortality. Several diagnostic modalities are available for the detection of DVT, venous ultrasonography being the most prominent in the current clinical practice due to its good diagnostic performance, availability, and absence of use of ionizing radiation. In this study, the authors compare findings between the nuclear medicine imaging modality, RNV, to those of venous ultrasonography. The sample included in this study comprises middle-aged to elderly people with underlying cancer as the dominant underlying comorbidity which is typical for patients at risk of having venous thrombosis. DVT was detected by venous ultrasonography in about 40% of venous segments, which is within the range found in most previous studies which reported prevalence of 5%–65%.[11] This rather high prevalence could be due to the nature of patient selection, since this is a retrospective study, it is expected that patients who were sent for both imaging examinations would have a high pretest probability of having DVT. Since no gold standard test for diagnosis of DVT was performed in this study, sensitivity, specificity, and diagnostic accuracy were not analyzed; instead, the two imaging modalities, i.e., RNV and venous ultrasonography, were compared on how well they agree. As it turns out, the overall agreement between the two imaging techniques was only moderate as determined by Cohen's kappa. Since venous ultrasonography has been found to be highly specific for diagnosis of DVT, a positive venous ultrasonography should be compelling evidence of DVT, and to better aid in future clinical application and interpretation of RNV, positive RNV findings were compared with positive venous ultrasonography findings to calculate the PPV of each abnormal finding of RNV. The high PPV of RNV found in this study is in agreement with the previous studies,[14,15] with the findings of absent or reduced radiotracer activity in a deep venous segment or presence of multiple collateral vessels as strong evidence that DVT is present. However, the presence of collateral vessel activity alone particularly in the great saphenous vein when activity in the deep vein is normal carries a lower PPV of only 43%, so patients with these RNV findings should receive further investigation or follow-up studies. The NPV of RNV in this study is 97.5%, which is expected of a test that has been demonstrated to be very sensitive for DVT in previous studies.[14,15] The strength of this study is the detailed analysis of PPV for the many patterns of abnormal RNV findings which could aid in gauging of the posttest probability in clinical practice. Limitations of this study include retrospective data collection which results in limited clinical information, so pretest probability of DVT cannot be assessed. Further outcomes study which investigates the effect of RNV on clinical outcome should provide additional information on the prognostic role of RNV in patients with suspected DVT.
Conclusion
RNV and venous ultrasonography have moderate agreement for detection of lower limb DVT. The key advantage of RNV is the possibility of simultaneously evaluating bilateral lower limbs from calf to IVC. The absence of or reduced radiotracer activity in a deep venous segment or the presence of radiotracer activity in multiple collateral veins is the finding highly predictive of the presence of DVT. The high NPV suggests that patients with normal RNV have a very low probability of having DVT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mackman N. New insights into the mechanisms of venous thrombosis. J Clin Invest. 2012;122:2331–6. doi: 10.1172/JCI60229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I4–8. doi: 10.1161/01.CIR.0000078468.11849.66. [DOI] [PubMed] [Google Scholar]
- 3.Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: Clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER) Lancet. 1999;353:1386–9. doi: 10.1016/s0140-6736(98)07534-5. [DOI] [PubMed] [Google Scholar]
- 4.Jimezez D, Aujesky D, Diaz G. Prognostic significance of deep vein thrombosis in patients presenting with acute symptomatic pulmonary embolism. J Vasc Surg. 2011;53:1448–9. doi: 10.1164/rccm.200908-1204OC. [DOI] [PubMed] [Google Scholar]
- 5.Kafeza M, Shalhoub J, Salooja N, Bingham L, Spagou K, Davies AH. A systematic review of clinical prediction scores for deep vein thrombosis. Phlebology. 2017;32:516–31. doi: 10.1177/0268355516678729. [DOI] [PubMed] [Google Scholar]
- 6.Vaitkus PT, Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Goldhaber SZ. PREVENT Medical Thromboprophylaxis Study Group. Mortality rates and risk factors for asymptomatic deep vein thrombosis in medical patients. Thromb Haemost. 2005;93:76–9. doi: 10.1160/TH04-05-0323. [DOI] [PubMed] [Google Scholar]
- 7.Di Nisio M, Squizzato A, Rutjes AW, Büller HR, Zwinderman AH, Bossuyt PM. Diagnostic accuracy of D-dimer test for exclusion of venous thromboembolism: A systematic review. J Thromb Haemost. 2007;5:296–304. doi: 10.1111/j.1538-7836.2007.02328.x. [DOI] [PubMed] [Google Scholar]
- 8.Rossi R, Agnelli G. Current role of venography in the diagnosis of deep-vein thrombosis. Minerva Cardioangiol. 1998;46:507–14. [PubMed] [Google Scholar]
- 9.Hull R, Hirsh J, Sackett DL, Taylor DW, Carter C, Turpie AG, et al. Clinical validity of a negative venogram in patients with clinically suspected venous thrombosis. Circulation. 1981;64:622–5. doi: 10.1161/01.cir.64.3.622. [DOI] [PubMed] [Google Scholar]
- 10.Zierler BK. Ultrasonography and diagnosis of venous thromboembolism. Circulation. 2004;109(12 Suppl 1):I9–14. doi: 10.1161/01.CIR.0000122870.22669.4a. [DOI] [PubMed] [Google Scholar]
- 11.Kassaï B, Boissel JP, Cucherat M, Sonie S, Shah NR, Leizorovicz A. A systematic review of the accuracy of ultrasound in the diagnosis of deep venous thrombosis in asymptomatic patients. Thromb Haemost. 2004;91:655–66. doi: 10.1267/THRO04040655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chong LY, Fenu E, Stansby G, Hodgkinson S, Guideline Development Group Management of venous thromboembolic diseases and the role of thrombophilia testing: Summary of NICE guidance. BMJ. 2012;344:e3979. doi: 10.1136/bmj.e3979. [DOI] [PubMed] [Google Scholar]
- 13.Divittorio R, Bluth EI, Sullivan MA. Deep vein thrombosis: Diagnosis of a comon clinical problem. Ochsner J. 2002;4:14–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Mangkharak J, Chiewvit S, Chaiyasoot W, Pusuwan P, Permpikul C, Toopmongkol C, et al. Radionuclide venography in the diagnosis of deep vein thrombosis of the lower extremities: A comparison to contrast venography. J Med Assoc Thai. 1998;81:432–41. [PubMed] [Google Scholar]
- 15.Ennis JT, Elmes RJ. Radionuclide venography in the diagnosis of deep vein thrombosis. Radiology. 1977;125:441–9. doi: 10.1148/125.2.441. [DOI] [PubMed] [Google Scholar]
- 16.Cantor AB. Sample-size calculations for Cohen's kappa. Psychol Methods. 1996;1:150–3. [Google Scholar]