Abstract
Background
Dairy product consumption may affect the risk of hip fracture, but previous studies have reported inconsistent findings. The primary aim of our meta-analysis was to examine and quantify the potential association of dairy product consumption with risk of hip fracture.
Methods
We searched the databases of PubMed and EMBASE for relevant articles from their inception through April 17, 2017. The final analysis included 10 cohort studies and 8 case-control studies. Random-effects models were used to estimate the pooled risk. Subgroup and dose-response analyses were conducted to explore the relationships between the consumption of milk and the risk of hip fracture.
Results
After pooling the data from the included studies, the summary relative risk (RR) for hip fracture for highest versus lowest consumption were 0.91 (95% CI: 0.74–1.12), 0.75 (95% CI: 0.66–0.86), 0.68 (95% CI: 0.61–0. 77), 1.02 (95% CI: 0.93–1.12) for milk, yogurt, cheese, and total dairy products in cohort studies, respectively. Higher milk consumption [Odds ratio (OR), 0.71, 95% CI: 0.55–0. 91] was associated with lower risk of hip fracture for highest versus lowest consumption in case-control studies. After quantifying the specific dose of milk, the summary RR/OR for an increased milk consumption of 200 g/day was 1.00 (95% CI: 0.94–1.07), and 0.89 (95%CI: 0.64–1.24) with significant heterogeneity for cohort and case-control studies, respectively; There was a nonlinear association between milk consumption and hip fracture risk in cohort, and case-control studies.
Conclusions
Our findings indicate that consumption of yogurt and cheese was associated with lower risk of hip fracture in cohort studies. However, the consumption of total dairy products and cream was not significantly associated with the risk of hip fracture. There was insufficient evidence to deduce the association between milk consumption and risk of hip fracture. A lower threshold of 200 g/day milk intake may have beneficial effects, whereas the effects of a higher threshold of milk intake are unclear.
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5041-5) contains supplementary material, which is available to authorized users.
Keywords: Hip fracture, Diet, Dairy products, Milk consumption, Meta-analysis, Case-control study, Cohort study
Background
Hip fracture is the most serious type of osteoporotic fracture. Hip fractures can lead to other comorbidities, increased mortality risk, and enormous social and economic costs [1]. According to recent reports, approximately 1.66 million patients are diagnosed with hip fracture occur each year worldwide [2, 3]. World population surveys have shown that the number of adults older than 60 years old was 841 million in 2013, which is approximately four times as high as that in 1950 (202 million) [4]. The incidence of hip fracture increases linearly with age [5]. The pathogenesis of hip fracture is multifactorial. The main factors contributing to the development of hip fracture are bone mineral density, falls, and lifestyle habits. Lifestyle habits include calcium intake, general nutrition, and exposure to sunlight, physical activity, smoking, and alcohol intake [6–10]. It is known that nutrition, especially dairy product consumption, has an important effect on maintaining bone health.
Dairy products have been hypothesized to help prevent hip fracture because they are a significant source of calcium, proteins, and other bioactive nutrients beneficial for bone health [11]. However, the effects of dairy products on hip fractures have not been established. The benefit of milk, as a main dietary source of calcium in reducing hip fracture risk has yet to be debated. More recently, a study by Sahni et al., [12] indicated that there was a nonsignificant 42% reduction in hip fracture risk in elderly adults who consumed more than 7 milk servings per week, compared with those who consumed less than one serving per week in the Framingham Original Cohort. Michaëlsson et al., [13] found that for every glass of milk consumed per day, women had a significant 9% increase in hip fracture risk, although no association was observed in men. Meanwhile, the data suggested that higher cheese or yogurt intake may reduce hip fracture risk in both men and women [7].
Two previous meta-analyses have been published with results focused only on milk consumption [14, 15]. However, some studies assessed the association between hip fracture and consumption of different types of dairy products, since different types of products contain varying nutrient contents (e.g., milk is rich in lactose, cheese and yogurt can provide lactic acid bacteria). Choosing dairy products like milk, cheese, or yogurt instead of cream can decrease fat, and cholesterol. Therefore, it is important to evaluate the influence of the consumption of different types of dairy products (total dairy products, milk, yogurt, cheese, and cream) on hip fracture risk.
Methods
Search strategy
The primary aim of our meta-analysis was to examine and quantify the potential association of dairy product consumption with risk of hip fracture. Searches were performed on PubMed and EMBASE databases from their inception to April 17, 2017. The search terms used were as follows: “hip fracture” (or “subtrochanteric fracture” or “trochanteric fracture” or “intertrochanteric fracture” or “femoral neck fracture”) and “dairy products” (or “milk” or “cheese” or “yogurt” or “cream”). No language restrictions were applied in the search strategy. An additional article [16] was identified through the bibliographies of relevant reviews. Figure 1 and Additional file 1 provides detailed search terms and search strategies for both databases.
Fig. 1.
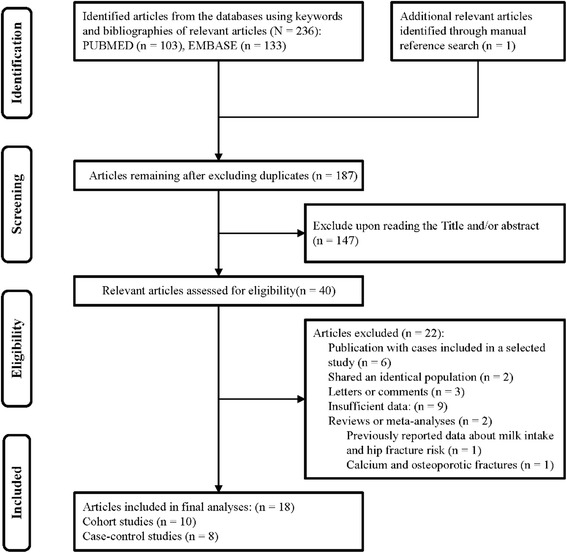
Search strategy and selection of studies for this meta-analysis
Eligibility criteria
To identify eligible studies, two independent investigators (S.B.and J.H.) performed an initial screening of all titles and abstracts, and then assessed the full text of all relevant studies in detail. Articles were included in this meta-analysis if they met the following criteria: (1) cohort or case-control study design; (2) studies that evaluated and clearly defined exposure to total dairy products, milk, cheese, yogurt, or cream; (3) studies with the risk of hip fracture as the outcome of interest; and (4) studies reporting odds ratio (OR) or relative risk (RR) with 95% confidence intervals (CI) for the association between dairy product exposure and risk of hip fracture. Studies had to define hip fracture using the criteria based on the International Classification of Diseases, 10th revision (ICD-10) or medical records. If there were multiple publications from the same study, we selected the most recent study for the meta-analysis. Studies were excluded if they provided insufficient data, such as letters, reviews, comments, or animal studies. Two previous meta-analyses had been published with results focused only on milk consumption. The meta-analysis conducted by Bischoff-Ferrari et al., [14] was excluded, because the report contained duplicated data. The meta-analysis conducted by Kanis et al., [15] was included in our meta-analysis. The flow diagrams of the selection process and results are shown in Fig. 1.
Data processing and quality assessment
Two authors (Y.W. and K.Z.) independently extracted the following information from each included study: author name, research region, publication year, study design, study name, subjects (number of cases), sex, mean/median age of the study individuals, duration of follow-up for cohort studies, exposure and quantity of intake, dietary assessment method, the maximally adjusted risk estimates with 95% CI for the highest versus the lowest category of consumption, and adjustment for confounders in analyses.
In the dose-response meta-analysis of the relationship between dairy products and hip fracture risk, the number of cases and participants or person-years, the mean or median dairy product consumption for each exposure category, and the RR/OR and its variance estimate for three or more quantitative exposure categories were compiled from the included studies. The median level of milk consumption (g/day) for each exposure category was presented with the relevant RR/OR and corresponding 95% CI. We used standard conversions from the Food Standards Agency to convert glasses/d to g/d (1 glass = 200 mL) for relevant studies [17, 18]. Assumptions were used to convert ml/d to approximate g/d [19]. If dairy products were reported as servings, drinks, or times per day/week/month instead of quantity, the following average amounts were used to represent a serving: 177 g for total dairy products, 244 g for milk and yogurt, and 43 g for cheese consumption [20, 21].
Two investigators (M.Y. and K.Z.) independently assessed the quality of the 17 included studies (Excluding the meta-analysis [15] as previously mentioned) using the Newcastle-Ottawa scale (NOS) [22]. This scale scores studies on three categories (selection, comparability of study groups, and the outcome of interest). A study can be awarded a maximal score of 9, which represents the highest quality study.
Statistical analysis
Effect sizes were estimated with RR in cohort studies and OR in case-control studies. Cohort and case-control studies were pooled separately in our meta-analysis. We quantified the association of dairy product consumption with hip fracture risk using random-effects models [23].
Subgroup and meta-regression analyses were performed to assess potential sources of heterogeneity stratified by some of the baseline characteristics, such as study quality, region, sex, number of cases, duration of follow-up for cohort studies, age, and adjustment for potential confounders. We also investigated the influence of different types of dairy product consumption, including total dairy products, yogurt, cheese, and cream.
In the dose-response meta-analysis, we used the method proposed by Greenland and Longnecker [24] to estimate the dose-response trend of the relationship between dairy product consumption and hip fracture risk. We applied random effects models [25] to estimate the summary RR or OR within each study.
Between-study heterogeneity was evaluated using both the Q and I2 statistics. A Q statistic with P < 0.10 indicated heterogeneity, whereas I2 values of 0%, 25%, 50%, and 75% represented no, low, moderate, and high heterogeneity, respectively [25]. Publication bias was considered by visual inspection of the contour-enhanced funnel plot symmetry as well as by Egger’s test [26] and Begg’s test [27]. Furthermore, Duval’s non-parametric trim-and-fill procedure was performed to adjust for the number of missing studies and estimate possible publication bias [28]. Meta-analyses were conducted with R version 3.1.2 (The R Foundation for Statistical Computing, Vienna, Austria), using the following packages: meta, foreign, dosresmeta, Hmisc, survival, SparseM, and rms. All statistical tests were two-sided, and P values <0.05 indicated statistical significance.
Results
Literature search
Figure 1 shows the search strategy and selection of studies for our meta-analysis on dairy product consumption and the risk of hip fracture. We identified one additional article by manually searching the reference lists from the included studies [16]. A total of 18 articles [12, 13, 15, 16, 29–42] were included in the present meta-analysis (Additional file 2).
Characteristics of included studies
Table 1 shows the detailed baseline characteristics of the included studies. A total of 18 observational studies (10 cohort studies [12, 13, 15, 16, 33–37, 42] and 8 case-control studies [29–32, 38–41]) involving 381,987 participants were included in the final analysis. The 10 cohort studies were published between 1997 and 2014, with a total of 8613 hip fracture events, and 363,557 participants. The length of follow-up ranged from 3 to 22 years. Eight cohort studies included both sexes. One cohort study included only male individuals and the remaining cohort study recruited only females. Four cohort studies were conducted in the USA, 4 were conducted in Europe, 1 was conducted in Asia, and 1 was a meta-analysis of a multicenter study including participants from Europe, Australia, and Canada. The 8 case-control studies were published between 1992 and 2010, and included 3815 hip fracture cases and 6415 controls. Geographic regions of the case-control studies included Europe (n = 3), Australia (n = 1), USA (n = 1), and Asia (n = 3).
Table 1.
Baseline characteristics of studies included in the meta-analysis
| First author | Publication year | Region | Study design | Study name | Subjects (cases) | Sex | Mean/median age (years) | Follow up period (years) | Diet assessment | Exposure | Quantity | OR/RR (95% CI) | Ascertainment method of hip fracture | Adjustment for confounders |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feskanich | 2014 | USA | cohort study | The Nurses’ Health Study (NHS); the Health Professionals Follow-up Study (HPFS) | 96,927 (1716) | M/F | F (30–55) M (40–75) | 22 | FFQ | Milk | ≥ 4 vs. 1 glass/day | Males 1.21(0.86–1.64) Females 1.01(0.78–1.31) | Self -reporting | Age, questionnaire cycle, adult milk consumption, calcium supplements, vitamin D supplements, retinol from supplements, total protein, alcohol and caffeine intakes, total energy intake, physical activity, BMI, smoking, use of thiazide diuretics, use of furosemide diuretics and oral steroids (men only], use of hormone replacement therapy, incident diagnoses of osteoporosis and cancer, teenage measures |
| Michaëlsson | 2014 | Sweden | cohort study | The Swedish Mammography Cohort; the Cohort of Swedish Men | 106,772 (5425) | M/F | 56.5 (39–79) | F: 20.1 M:11.2 | FFQ | Milk | ≥ 600 vs. < 200 g/day | Males: 1.01 (0.85–1.20) Females: 1.60(1.39–1.84) |
Registers | Age, BMI, height, total energy intake, total alcohol intake, healthy dietary pattern, calcium and vitamin D supplementation, ever use of cortisone, educational level, living alone, physical activity level estimated as metabolic equivalents, smoking status, and Charlson comorbidity index; for women only, use of estrogen replacement therapy and nulliparity |
| Yogurt | ≥ 400 vs. < 1 g/day | Males: 0.75 (0.63–0.90) Females: 0.70 (0.57–0.86) |
||||||||||||
| Cheese | ≥ 60 vs. < 20 g/day | Males: 0.75 (0.62–0.92) Females: 0.64 (0.55–0.74) |
||||||||||||
| Sahni | 2014 | USA | cohort study | The Framingham Original Cohort | 764 (97) | M/F | 76.9 (68–96) | 11.6 | Validated FFQ | Milk | ≥ 7 vs. ≤ 1 servings/week | 0.58 (0.31–1.06) | Self-reporting confirmed by review of medical records and radiographic and operative reports | Age, sex, weight, height, total energy intake, current cigarette smoking, calcium supplement use, vitamin D supplement use |
| Yogurt | > 0 vs. 0 servings/week | 1.09 (0.65–1.81) | ||||||||||||
| Cheese | > 1 vs. ≤ 1 servings/week | 0.72 (0.48–1.08) | ||||||||||||
| Cream | ≥ 3 vs. < 1 servings/week | 1.04 (0.59–1.86) | ||||||||||||
| Benetou | 2011 | European | cohort study | The Cancer and nutrition (EPIC) study | 29,122 (275) | M/F | 64.3 (60–86) | 8 | Validated FFQ | Total dairy products | Yes vs. no | 1.02 (0.93–1.12) | Both registers and self-reporting | Sex, age, BMI, height, educational level, smoking status, physical activity at leisure, supplement use, history of diabetes at enrolment, total energy intake |
| Feart | 2013 | France | cohort study | The Three-City (3C) study | 1482 (57) | M/F | 75.9 (67.7–94.9) | 8 | FFQ and a 24-h dietary recall | Dairy products | Highest vs. lowest category | 1.05 (0.60–1.85) | Self-reporting | Each individual food group component of the Mediterranean diet score, age, gender, physical activity, total energy intake, educational level, marital status, BMI, osteoporosis treatment, calcium and/or vitamin D treatment |
| Milk | Highest vs. lowest category | 0.86 (0.50–1.49) | ||||||||||||
| Yogurt | Highest vs. lowest category | 0.90 (0.50–1.61) | ||||||||||||
| Cheese | Highest vs. lowest category | 0.78 (0.44–1.39) | ||||||||||||
| Cumming | 1997 | USA | cohort study | Study of Osteoporotic Fractures (SOF Study) | 9704 (306) | F | 71 (65+) | 6.6 | Validated FFQ | Milk | ≥ 3 vs. rarely/never glasses/day | 0.90 (0.50–1.70) | Self-reporting | Age, clinic, weight, history of osteoporosis, history of fractures since age 50, fall in past 12 months, protein intake, caffeine intake, recreational physical activity, take walks for exercise, impaired low frequency contrast sensitivity, estrogen replacement therapy, thiazide use, use of calcium and Vitamin D supplements, use of Turns antacid tablets |
| Fujiwara | 1997 | Japan | cohort study | the Adult Health Study (AHS) | 4573 (55) | M/F | 58.5 | 14 | Standardized questionnaire | Milk | ≥ 5 vs. ≤ 1 times/week | 0.54 (0.25–1.07) | Registers | Age, alcohol, BMI, prevalent vertebral fracture, number of children, age at menarche |
| Meyer | 1997 | Norway | cohort study | the National Health Screening study | 39,787 (213) | M/F | 47.1 (42.9–65.9) | 11.4 | FFQ | Milk | ≥ 5 vs. < 1 glasses/day | Males: 0.46 (0.22–0.98) Females: 0.83 (0.44–1.56) |
Self-reporting confirmed by review of medical records and radiographic and operative reports | Age, body height, BMI, self-reported physical activity at work and during leisure time, diabetes mellitus, disability pension, marital status, smoking |
| Owusu | 1997 | USA | cohort study | The Health Professionals Follow-up Study | 43,063 (56) | M | 54 (40–75) | 8 | Validated FFQ | Milk | 2.5 vs. ≤1 glass/week | 0.97 (0.39–2.42) | Self-reporting | Age, alcohol consumption, smoking, BMI, physical activity, total energy intake |
| Kanis | 2004 | Europe, Australia, and Canada |
Meta-analysis of cohort study | The European Vertebral Osteoporosis Study (EVOS);The Canadian Multicentre Osteoporosis Study (CaMos);The Dubbo Osteoporosis Epidemiology Study (DOES);The Rotterdam Study;The Sheffield Study;The Gothenburg study | 39,563 (413) | M/F | 66.7(58.9–80.0) | 3–8 | NR | Milk | 'Highest vs. lowest category of consumption | Males:0.66 (0.39–1.12) Females: 0.92 (0.69–1.22) |
Both registers and self-reporting | NR |
| Jha | 2010 | India | case-control study | NR | 200 (100) |
M/F | 65.2 | NR | Standardized questionnaire | Milk, | > 1 vs. ≤ 1 glass/day | 0.30 (0.13–0.72) | Self-reporting | NR |
| Cheese | > 1 vs. ≤ 1 servings/week | 0.48 (0.24–0.93) | ||||||||||||
| Yogurt | > 2 vs. ≤ 2 cups/week | 0.77 (0.39–1.51) | ||||||||||||
| Lan | 2010 | Taiwan | case-control study | NR | 725 (228) | M/F | (60+) | NR | Standardized questionnaire | Milk | ≥ 6 vs. none or <1 drink/week | 0.58 (0.37–0.91) | Self-reporting | Socio-demographic, disease history, self-assessed health, anthropometry and health habits, diet habits, injury-related experience, physical functioning, cognitive and other functioning, physical performance, female reproductive history, bone mineral density |
| Jitapunkul | 2001 | Thai Chinese | case-control study | NR | 120 (60) | F | 71.4 | NR | Structured questionnaire | Milk | Yes vs. no | 0.26 (0.09–0.76) | Self-reporting | No regular intake of milk, low number of pregnancies, thin body appearance, low serum calcium |
| Kanis | 1999 | Southern Europe | case-control study | The MEDOS study | 1862 (730) | M | 74 | NR | Standardized questionnaire | Milk | Highest vs. lowest category of consumption | 0.82 (0.61–1.11) | Registers | BMI, recreational physical activity, consumption of tea, alcohol consumption, coffee consumption, smoking, sunlight exposure |
| Cheese | Yes vs. no | 0.75 (0.49–1.14) | ||||||||||||
| Johnell | 1995 | Southern Europe | case-control study | The MEDOS Study | 5618 (2086) |
F | 77.8 | NR | Standardized questionnaire | Milk | Highest vs. lowest category | 0.71 (0.58–0.87) | Registers | Mental score, BMI, menarche, menopause, sunlight exposure, tea consumption |
| Tavani | 1995 | Italy | case–control study | NR | 960 (241) | F | 63.3 (45–74) | NR | Standardized questionnaire | Milk | > 7 vs. < 7 drinks/week | 1.00 (0.60–1.60) | Registers | Age, education, BMI, estrogen replacement therapy |
| Cheese | > 6 vs. < 4 portions/week | 1.00 (0.70–1.50) | ||||||||||||
| Cumming | 1994 | Australia | case-control study | NR | 416 (209) | M/F | (65–100) | NR | Standardized questionnaire | Dairy product | Highest vs. lowest category | 1.70 (0.50–5.40) | Registers | Age, sex, country of birth, mental state score, psychotropic drug use, smoker status, work in the house and garden, weight |
| Nieves | 1992 | USA | case-control study | NR | 329 (161) | F | (50–103) | NR | Validated FFQ | Milk | ≥ 7 vs. no glasses/week | 1.10 (0.63–1.94) | Registers | Hospital site, age and BMI, smoking status, alcohol consumption |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); F, Female; M, male; FFQ, food frequency questionnaire; NR, not reported
Milk consumption and risk of hip fracture
Nine cohort studies [12, 13, 15, 16, 33, 34, 36, 37, 42] and 7 case-control studies [29–32, 38, 39, 41] reported the association between milk consumption and risk of hip fracture.
Meta-analysis of cohort studies
For cohort studies, the pooled RR for highest versus lowest category of milk consumption and hip fracture risk was 0.91 (95% CI: 0.74–1.12, I2 = 75.0%, Pheterogeneity < 0.01) (Fig. 2a), indicating that milk consumption had no association with hip fracture risk. The analyses producing the pooled estimates indicated heterogeneity.
Fig. 2.
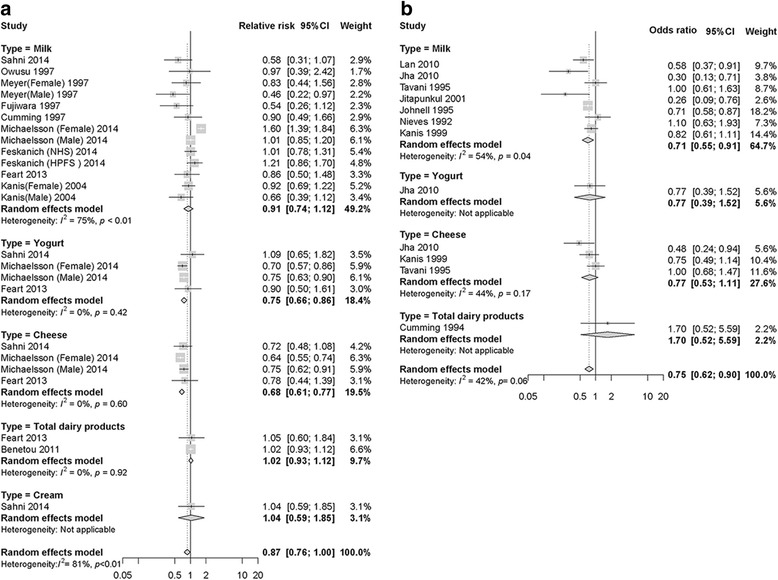
Relative risks of hip fracture for the highest compared with the lowest categories of dairy product consumption. a Collection of pooled data from cohort studies; b Collection of pooled data from case-control studies. The gray box indicates the 95% confidence intervals (CIs). The size of the square around each effect estimate indicates the weight of the individual study
The contour-enhanced funnel plot demonstrated asymmetry (Fig. 3a). However, Egger’s test (P = 0.81) and Begg’s test (P = 0.30) indicated no publication bias with regard to milk intake and hip fracture risk. We used the trim-and-fill method to confirm robustness of the results. There were no significant changes to the results after using the trim-and-fill method when including four missing articles (adjusted random effects summary RR: 1.06, 95% CI: 0.91–1.23).
Fig. 3.
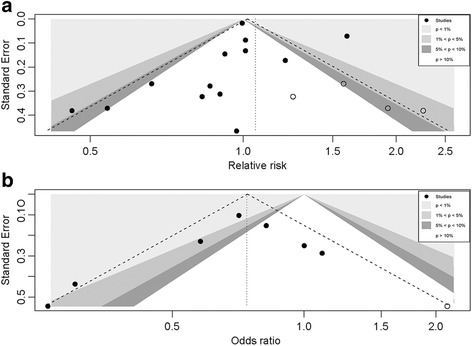
Contour-enhanced funnel plot of Milk consumption and hip fracture risk. a Data are collected from cohort studies; b Collection of data from case-control studies. Each dot indicates a different study
Meta-analysis of case-control studies
The case-control studies indicated that participants in the highest categories of milk consumption had a 29% reduction in the risk of hip fracture (OR = 0.71, 95%CI: 0.55–0.91, I2 = 54%, Pheterogeneity = 0.04) (Fig. 2b). Pooled estimate analyses indicated heterogeneity.
For case-control studies, the contour-enhanced funnel plot showed asymmetry (Fig. 3b). There were no significant changes to the results after using the trim-and-fill method when including one missing article (adjusted random effects summary OR: 0.74, 95% CI: 0.57–0.97). The trim-and-fill estimates should be interpreted with great caution due to the limitations inherent to the methods used.
Quality study, subgroup, and meta-regression analyses
The quality of the 17 included studies (Excluding the meta-analysis study [15] as discussed previously) using the Newcastle-Ottawa scale (NOS) [22] is shown in Tables 2, and 3.
Table 2.
Quality assessment of the included cohort studies
| Newcastle-Ottawa Scale for assessing the quality of cohort studies in meta-analysis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | |||||||||
| Study | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that the current outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow up of cohorts | Quality score | ||
| 1 | Feskanich | 2014 | ★ | ★ | ★ | ★★ | ★ | ★ | 7 | ||
| 2 | Michaëlsson | 2014 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| 3 | Sahni | 2014 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| 4 | Feart | 2013 | ★ | ★ | ★ | ★★ | ★ | ★ | 7 | ||
| 5 | Benetou | 2011 | ★ | ★ | ★ | ★★ | ★ | ★ | 7 | ||
| 6 | Cumming | 1997 | ★ | ★ | ★ | ★★ | ★ | ★ | 7 | ||
| 7 | Fujiwara | 1997 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| 8 | Meyer | 1997 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| 9 | Owusu | 1997 | ★ | ★ | ★ | ★★ | ★ | ★ | 7 | ||
A study can be awarded a maximum of one star for each numbered item within the Selection and Outcome categories. A maximum of two stars can be given for Comparability
Table 3.
Quality assessment of the included case-control studies
| Newcastle-Ottawa Scale for assessing the quality of case control studies in meta-analysis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | |||||||||
| Study | Is the case definition adequate | Representativeness of the cases | Selection of controls | Definition of controls | Comparability of cases and controls on the basis of the design or analysis | Ascertainment of exposure | Same method of ascertainment for cases and controls | Non-Response rate | Quality score | ||
| 1 | Jha | 2010 | ★ | ★★ | ★ | ★ | 5 | ||||
| 2 | Lan | 2010 | ★ | ★★ | ★ | 4 | |||||
| 3 | Jitapunkul | 2001 | ★ | ★ | ★★ | ★ | 5 | ||||
| 4 | Kanis | 1999 | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8 | |
| 5 | Johnell | 1995 | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8 | |
| 6 | Tavani | 1995 | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8 | |
| 7 | Cumming | 1994 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | 8 | |
| 8 | Nieves | 1992 | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 8 | |
A study can be awarded a maximum of one star for each numbered item within the Selection and Outcome categories. A maximum of two stars can be given for Comparability
In subgroup and meta-regression analyses, the null association between milk consumption and hip fracture risk was consistently observed in the subgroup analysis of 9 cohort studies [12, 13, 15, 16, 33, 34, 36, 37, 42] stratified by different factors (Table 4), except for studies that did not adjust for total energy intake. In addition, there was an inverse association between calcium and vitamin D supplements and hip fracture risk in cohort studies. An inverse association between milk consumption and hip fracture risk was consistently observed in case-control studies (Fig. 2b); subgroup analysis showed that milk consumption had no association with hip fracture risk in studies from the USA.
Table 4.
Subgroup analyses comparing milk intake and hip fracture risk for case-control and cohort studies
| Cohort studies (n = 9) | Case-control studies (n = 7) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | RR | 95% CI | I2 (%) | P a | P b | n | OR | 95% CI | I2 (%) | P a | P b | |
| Study quality | ||||||||||||
| Score ≥ 8 | 4 | 0.98 | 0.75–1.27 | 90.0 | <0.01 | 0.90 | 4 | 0.80 | 0.67–0.95 | 10.0 | 0.34 | 0.05 |
| Score < 8 | 4 | 1.03 | 0.86–1.24 | 0.0 | 0.82 | 3 | 0.42 | 0.25–0.71 | 35.0 | 0.21 | ||
| Region | ||||||||||||
| USA | 4 | 1.00 | 0.96–1.03 | 0.0 | 0.84 | 0.44 | 1 | 1.10 | 0.63–1.94 | NA | NA | 0.04 |
| Europe | 3 | 0.98 | 0.68–1.41 | 86.0 | <0.01 | 3 | 0.77 | 0.65–0.90 | 0.0 | 0.39 | ||
| Asia | 1 | 0.54 | 0.26–1.12 | 3 | 0.42 | 0.25–0.71 | 35.0 | 0.21 | ||||
| Sex | ||||||||||||
| Male | 5 | 0.91 | 0.70–1.19 | 48.0 | 0.10 | 0.68 | 1 | 0.82 | 0.61–1.11 | NA | NA | 0.28 |
| Female | 6 | 1.07 | 0.78–1.47 | 81.0 | <0.01 | 4 | 0.78 | 0.53–1.14 | 58.0 | 0.07 | ||
| Both | 3 | 0.91 | 0.70–1.18 | 23.8 | 0.23 | 2 | 0.46 | 0.25–0.85 | 44.0 | 0.18 | ||
| No. of cases | ||||||||||||
| ≥ 1000 | 2 | 1.19 | 0.85–1.66 | 90.0 | <0.01 | 0.16 | 1 | 0.71 | 0.58–0.87 | NA | NA | 0.21 |
| 100–1000 | 4 | 1.00 | 0.82–1.21 | 0.0 | 0.57 | 4 | 0.83 | 0.65–1.06 | 24.0 | 0.27 | ||
| ≤ 100 | 6 | 0.79 | 0.60–1.04 | 46.0 | 0.10 | 2 | 0.28 | 0.15–0.55 | 0.0 | 0.84 | ||
| Duration of follow-up years | ||||||||||||
| ≥ 10 years | 5 | 1.02 | 0.84–1.25 | 86.0 | <0.01 | 0.63 | NA | NA | NA | NA | NA | NA |
| < 10 years | 3 | 0.89 | 0.62–1.29 | 0.0 | 0.98 | NA | NA | NA | NA | NA | NA | |
| Age | ||||||||||||
| ≥ 70 | 4 | 1.00 | 0.96–1.03 | 0.0 | 0.80 | 0.45 | 3 | 0.61 | 0.34–1.09 | 68.0 | 0.04 | 0.66 |
| < 70 | 5 | 0.89 | 0.66–1.02 | 83.0 | <0.01 | 4 | 0.76 | 0.57–1.01 | 52.0 | 0.10 | ||
| Adjustment for confounders | ||||||||||||
| Smoking | ||||||||||||
| Yes | 5 | 1.06 | 0.87–1.29 | 85.0 | <0.01 | 0.21 | 2 | 0.87 | 0.67–1.12 | 0.0 | 0.50 | 0.32 |
| No | 3 | 0.78 | 0.55–1.11 | 0.0 | 0.52 | 5 | 0.60 | 0.42–0.88 | 60.0 | 0.04 | ||
| Alcohol | ||||||||||||
| Yes | 4 | 1.10 | 0.84–1.43 | 81.0 | <0.01 | 0.18 | 2 | 0.87 | 0.67–1.12 | 0.0 | 0.50 | 0.32 |
| No | 4 | 0.93 | 0.79–1.10 | 16.0 | 0.31 | 5 | 0.60 | 0.42–0.88 | 60.0 | 0.04 | ||
| BMI | ||||||||||||
| Yes | 5 | 1.00 | 0.77–1.29 | 79.0 | <0.01 | 0.71 | 4 | 0.80 | 0.67–0.95 | 10.0 | 0.34 | 0.05 |
| No | 3 | 0.99 | 0.96–1.03 | 0.0 | 0.83 | 3 | 0.42 | 0.25–0.71 | 35.0 | 0.21 | ||
| Physical activity | ||||||||||||
| Yes | 6 | 1.03 | 0.82–1.29 | 75.0 | <0.01 | 0.47 | 2 | 0.72 | 0.52–1.00 | 37.0 | 0.21 | 0.93 |
| No | 2 | 0.82 | 0.47–1.43 | 63.0 | 0.10 | 5 | 0.67 | 0.45–1.01 | 65.0 | 0.02 | ||
| Sunlight exposure | ||||||||||||
| Yes | 0 | NA | NA | NA | NA | NA | 2 | 0.74 | 0.63–0.88 | 0.0 | 0.43 | 0.67 |
| No | 8 | 1.01 | 0.84–1.20 | 80.0 | <0.01 | 5 | 0.62 | 0.38–1.01 | 67.0 | 0.02 | ||
| Total energy intake | ||||||||||||
| Yes | 5 | 1.11 | 0.91–1.35 | 86.0 | <0.01 | 0.05 | 0 | NA | NA | NA | NA | NA |
| No | 3 | 0.69 | 0.49–0.96 | 0.0 | 0.45 | 7 | 0.71 | 0.55–0.91 | 54.0 | 0.04 | ||
| Calcium and vitamin D supplementation | ||||||||||||
| Yes | 5 | 1.12 | 0.92–1.36 | 86.0 | <0.01 | 0.04 | 0 | NA | NA | NA | NA | NA |
| No | 3 | 0.69 | 0.50–0.95 | 0.0 | 0.47 | 7 | 0.71 | 0.55–0.91 | 54.0 | 0.04 | ||
Abbreviations: N, the number of studies; CI, confidence interval; OR, odds ratio; RR, relative risk; NA, not applicable; BMI, body mass index. Pa, heterogeneity within each subgroup; Pb, heterogeneity between subgroups with meta-regression analysis
Dose-response analysis
The relationship between milk consumption and hip fracture risk was further quantified via dose-response analysis for milk consumption. The summary RR for an increased milk consumption of 200 g/day was 1.00 (95% CI: 0.94–1.07), with significant heterogeneity among cohort studies (I2 = 87%, Pheterogeneity < 0.01, Fig. 4). The dose-response associations between milk consumption and risk of hip fracture in the cohort studies (n = 7) [12, 13, 16, 33, 34, 37, 42] are shown in Fig. 5a. There was a nonlinear positive association between milk consumption and hip fracture risk (Pnonlinerity < 0.01), with a rapid increase in risk when milk consumption increased from 0 to 600 g/d; there was no further increase in risk with milk consumption between 600 and 1200 g/d.
Fig. 4.
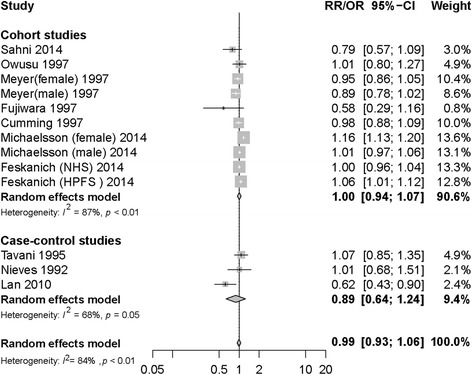
Milk consumption and risk of hip fracture. The summary relative risk per 200 g/d by using random-effects models
Fig. 5.
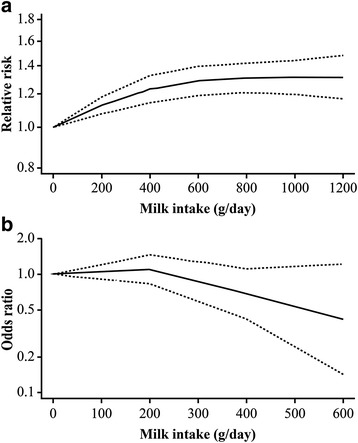
Dose-response relationship between milk consumption and risk of hip fracture
The summary OR for increasing milk consumption by 200 g/day was 0.89 (95% CI: 0.64–1.24), with significant heterogeneity among case-control studies (I2 = 68%, Pheterogeneity = 0.05, Fig. 4). Dose-response meta-analysis of the association between milk consumption and hip fracture risk in case-control studies (n = 3) [30, 39, 41] suggested a nonlinear association between milk consumption and hip fracture risk (Pnonlinerity = 0.28), with a reduction in risk with milk consumption of 200–600 g/d. However, the confidence intervals were wide for all outcomes (Fig. 5b).
Other dairy product intake and hip fracture risk
Consumption of yogurt (n = 3) and cheese (n = 3) reduced hip fracture risk, total dairy products (n = 2) and cream (n = 1) showed no association with hip fracture risk in cohort studies for the highest versus lowest category (Fig. 2a). Consumption of total dairy products (n = 1), yogurt (n = 1), and cheese (n = 3) in case-control studies showed no association with hip fracture risk (Fig. 2b). No additional contour-enhanced funnel plots, subgroup, or dose-response analyses for total dairy products, yogurt, cheese, and cream could be performed because of the limited results reported in the included studies.
Discussion
In this meta-analysis, a higher intake of yogurt and cheese was associated with a significant reduction in hip fracture risk as compared to low intake in cohort studies, and there was no overall association reported in case-control studies. Cohort and case-control studies reported no overall associations between total dairy products and cream, and hip fracture risk. Milk consumption was associated with a non-significant 9% lower hip fracture risk for highest versus lowest consumption in cohort studies. Nevertheless, the results of the case-control studies showed a significant 29% reduction in hip fracture risk for highest versus lowest consumption. The association between milk consumption and hip fracture risk remained unchanged when stratified by multiple study characteristics. Our finding for highest versus lowest milk consumption is consistent with the results from previous meta-analyses [14, 15]. Highest versus lowest analysis is limited, owing to differences in both the level, and range of milk consumption between the included studies, which may contribute to heterogeneity in the results. However, we further refined the precision of the risk estimates by applying the dose-response analysis for milk consumption, which may be important to guide recommendations for milk consumption with regard to risk reduction. Meanwhile, it is important to define and evaluate the potential threshold effects between milk consumption and hip fracture risk. In the nonlinear dose-response analysis, a low threshold of 200 g/day may have beneficial effects, whereas there is a degree of uncertainty with higher milk consumption.
Dairy products have a complicated influence on human health, and evidence on the impact of dairy products on hip fracture development remains inconsistent. Some previous studies indicated that dairy products might be beneficial for the prevention of hip fracture, as they contain calcium and vitamin D. Dairy products are often fortified with vitamin D in the United States, which is essential for the absorption of calcium and bone health [43]. A previous study has shown that vitamin D supplementation, with or without calcium, may have only minor effects on fracture risk among community-dwelling individuals [44]. Nonetheless, Chapuy et al., [45] showed that hip fracture risk was reduced with vitamin D and calcium supplementation among elderly women (mean age 84 years) who had very low vitamin D levels, with concurrent low dietary intake of calcium. Supplementation with vitamin D and calcium is a health-seeking behavior, which could be an important confounder.
Other studies argue that D-galactose in milk might promote oxidative stress and inflammation, which in turn influences the risk of fracture and mortality [13]. D-galactose is known to cause oxidative stress, aging, and inflammation. Milk contains high levels of lactose and galactose, while cheese and yogurt contain lower or non-existent levels. Previous cohort studies observed that milk consumption had a positive relationship with concentrations of marks for oxidative stress and inflammation.
These data suggest that higher milk, yogurt, and cheese consumption may contribute to a lower hip fracture risk, although the results with respect to milk consumption were not statistically significant in cohort studies. In contrast to high milk consumption, high yogurt and cheese consumption was associated with a significant 25%–32% lower risk of hip fracture, for the highest versus lowest consumption in cohort studies. Unlike milk, yogurt and cheese contain probiotics, which can improve bone formation, increase bone mass density and prevent bone loss. A study by Lei. et al., used probiotics to treat elderly patients with hip fracture on functional recovery [46].
This meta-analysis involved a larger number of cases to enhance the statistical power. Subgroup and dose-response analyses were performed to explore the heterogeneity of sources, used contour-enhanced funnel plots to display publication bias, and performed sensitivity analyses to test the robustness of the risk estimates. This meta-analysis is the first meta-analysis to evaluate the relationship between different types of dairy product consumption and hip fracture risk.
Our meta-analysis was subject to some limitations that may have affected the results. First, it is possible that the link between dairy product consumption and hip fracture risk could be interpreted within measurement errors in the dietary assessment. Food frequency questionnaires can be limited by errors in reporting and by incomplete assessment of all sources of dairy product consumption, which can lead to misclassification of exposure and weaken the association towards the null. Second, compared to cohort studies, case-control studies may have recall and selection bias. Dairy products and their possible role in bone health were widely discussed. The public debate might produce a bias in collecting dietary data among patients. Due to recall error, or dietary changes after hip fracture, participants are likely to have provided the current dietary data as a proxy for the previous diet. Cases reported a significant decrease in the frequency of dairy product consumption after the hip fracture, and it was even more obvious when the cases that provided a deliberate change in their dietary date were excluded. However, this was not evident with the control participants [47]. Indeed, inconsistent results between cohort and case-control studies were found, which might be explained by publication bias that was detected in the case-control studies. Publication bias refers to the idea that studies with positive results are more likely to be submitted for publication than those with negative results, which leads to misleading conclusions in meta-analyses. Third, differential loss to follow-up is a well-known source of bias in cohort studies, and the direction of that bias is hard to predict. Identification of fracture events may be an additional reason in cohort studies. Furthermore, the included studies may be limited by their use of differing means of assessing and measuring exposure and outcome, thereby impacting study quality scores. Ascertainment of hip fractures was partly or completely assumed by self-report in the included studies, which is also a source of bias. Mortality after hip fracture is high and a large proportion of persons who suffer a hip fracture are discharged to nursing facilities. Loss to follow-up and self-report are two important factors that increase the probability of a hip fracture not being reported, which could have affected the results. Fourth, high heterogeneity across studies was observed in this meta-analysis and baseline characteristics and adjustment for confounders also affected the results. Analyses of high versus low consumption were limited because of the different units (glasses/day, times/week, gram/day, servings/week) of dairy product consumption reported between studies, which may explain some heterogeneity in the results. Meta-regression analyses were used to explore potential sources of heterogeneity in our meta-analysis results, such as whether the studies adjusted for calcium and vitamin D supplementation, BMI, total energy intake, region, and study quality. Energy intake may increase when dairy product consumption increases, and BMI increases as total energy intake increases [48]. Several previous meta-analyses have suggested that BMI is inversely associated with hip fracture risk [49–51]. Meanwhile, a recent large, prospective, population-based study indicated that participants with BMI ≥ 25 kg/m2 had a reduced risk of hip fracture and patients with BMI < 22 kg/m2 had an increased risk compared with those with BMI between 22 and 24.9 kg/m2 [52], these sources of heterogeneity may have substantially influenced the results. Finally, only a small number of studies were available for the effects of total dairy products, cheese, yogurt, and cream consumption on hip fracture risk. Therefore, there was limited statistical power in the subgroup and dose-response analyses for our meta-analysis.
Conclusions
The conclusions of this meta-analysis were discordant. Milk consumption was found to be associated with an average 29% decrease in hip fracture risk in the included case-control studies. Meanwhile, recall bias or other possible bias could be a major influence on the findings in the case-control studies. The inconsistent findings for cohort studies indicate that there is no consistent evidence on the association between milk consumption and the risk of hip fracture. Therefore, we were unable to draw any conclusion from the estimates on the association between milk consumption and hip fracture risk. Consumption of other dairy products, yogurt and cheese intake was associated with lower risk of hip fracture in cohort studies, and total dairy products and cream was not significantly associated with hip fracture risk.
Additional files
Description: Search Phrases for a) PubMed, and b) EMBASE. (DOC 37 kb)
Title: Selection procedure for inclusion and exclusion of the studies. (DOC 50 kb)
Acknowledgements
We express our appreciation to all of the study participants. This study was supported by the National Natural Science Foundation of China (grant nos. 81702110).
Funding
This study was supported by the National Natural Science Foundation of China (grant nos. 81702110).
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon request.
Author contributions
SB and JH conceived the study design SB and JH wrote and applied this protocol under the guidance of JM, SB, JH, YW, KZ, and MY collected data. SB and JH drafted the manuscript; SB, JH and J.M. contributed to the interpretation of results and subsequent revisions. J.M. revised the study data for inclusion and the manuscript for intellectual content. The final version of the manuscript was approved by all of the authors.
Abbreviations
- BMI
Body mass index
- CI
Confidence interval
- FFQ
food frequency questionnaire
- OR
odds ratio
- RR
relative risk
- the ICD-10
International Classification of Diseases, 10th revision
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5041-5) contains supplementary material, which is available to authorized users.
Contributor Information
Shanshan Bian, Email: bianshanshan1986@126.com.
Jingmin Hu, Email: 13164098556@163.com.
Kai Zhang, Email: zhangkaitjykdxdeyy@126.com.
Yunguo Wang, Email: 8760715@163.com.
Miaohui Yu, Email: yumiaohui2011@126.com.
Jie Ma, Phone: +86-22-88328783, Email: majie_tjykdxdeyy@126.com.
References
- 1.Lotters FJ, Lenoir-Wijnkoop I, Fardellone P, Rizzoli R, Rocher E, Poley MJ. Dairy foods and osteoporosis: an example of assessing the health-economic impact of food products. Osteoporos Int. 2013;24:139–150. doi: 10.1007/s00198-012-1998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/PL00004148. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 4.United Nations, Department of Economic and Social Affairs, Population Division (2013). WorldPopulation Ageing 2013. [Online]. Available: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf. Accessed 1 July 2017.
- 5.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 6.Nilson F, Moniruzzaman S, Andersson RA. Comparison of hip fracture incidence rates among elderly in Sweden by latitude and sunlight exposure. Scand J Public Health. 2014;42(2):201–206. doi: 10.1177/1403494813510794. [DOI] [PubMed] [Google Scholar]
- 7.Hoidrup S, Gronbaek M, Gottschau A, Lauritzen JB, Schroll M. Alcohol intake, beverage preference, and risk of hip fracture in men and women. Copenhagen Centre for Prospective Population Studies. Am J Epidemiol. 1999;149(11):993–1001. doi: 10.1093/oxfordjournals.aje.a009760. [DOI] [PubMed] [Google Scholar]
- 8.Wu ZJ, Zhao P, Liu B, Yuan ZC. Effect of Cigarette Smoking on Risk of Hip Fracture in Men: A Meta-Analysis of 14 Prospective Cohort Studies. PLoS One. 2016;11(12):e0168990. [DOI] [PMC free article] [PubMed]
- 9.Body JJ, Bergmann P, Boonen S, Boutsen Y, Bruyere O, Devogelaer JP, et al. Non-pharmacological management of osteoporosis: a consensus of the Belgian bone Club. Osteoporos Int. 2011;22(11):2769–2788. doi: 10.1007/s00198-011-1545-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tucker KL. Osteoporosis prevention and nutrition. Curr Osteoporos Rep. 2009;7(4):111–117. doi: 10.1007/s11914-009-0020-5. [DOI] [PubMed] [Google Scholar]
- 11.Heaney RP. Calcium, dairy products and osteoporosis. J Am Coll Nutr. 2000;19(2 Suppl):83S–99S. doi: 10.1080/07315724.2000.10718088. [DOI] [PubMed] [Google Scholar]
- 12.Sahni S, Mangano KM, Tucker KL, Kiel DP, Casey VA, Hannan MT. Protective association of milk intake on the risk of hip fracture: results from the Framingham original cohort. J Bone Miner Res. 2014;29:1756–1762. doi: 10.1002/jbmr.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michaelsson K, Wolk A, Langenskiold S, Basu S, Warensjo Lemming E, Melhus H, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014;349:g6015. doi: 10.1136/bmj.g6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, Kanis JA, Orav EJ, Staehelin HB, et al. Milk intake and risk of hip fracture in men and women: a meta-analysis of prospective cohort studies. J Bone Miner Res. 2011;26(4):833–839. doi: 10.1002/jbmr.279. [DOI] [PubMed] [Google Scholar]
- 15.Kanis JA, Johansson H, Oden A, De Laet C, Johnell O, Eisman JA, et al. A meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int. 2005;16(7):799–804. doi: 10.1007/s00198-004-1755-6. [DOI] [PubMed] [Google Scholar]
- 16.Cumming RG, Cummings SR, Nevitt MC, Scott J, Ensrud KE, Vogt TM, et al. Calcium intake and fracture risk: results from the study of osteoporotic fractures. Am J Epidemiol. 1997;145(10):926–934. doi: 10.1093/oxfordjournals.aje.a009052. [DOI] [PubMed] [Google Scholar]
- 17.Food Standards Agency. Food portion sizes, third edition. London: TSO; 2003. [Online]. Available: https://www.food.gov.uk/sites/default/files/research-report-ao1020.pdf. Accessed 1 July 2017.
- 18.Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc. 2008;67(3):253–256. doi: 10.1017/S002966510800712X. [DOI] [PubMed] [Google Scholar]
- 19.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, FB H, Engberink MF, Willett WC, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93(1):158–171. doi: 10.3945/ajcn.2010.29866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aune D, Navarro Rosenblatt DA, Chan DS, Vieira AR, Vieira R, Greenwood DC, et al. Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am J Clin Nutr. 2015;101(1):87–117. doi: 10.3945/ajcn.113.067157. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Agriculture, Agricultural Research Service . USDA National Nutrient Database for Standard Reference. 2015. [Google Scholar]
- 22.Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2000. [Online]. Available: https://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 1 July 2017.
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 24.Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135(11):1301–1309. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 28.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 29.Jha RM, Mithal A, Malhotra N, Brown EM. Pilot case-control investigation of risk factors for hip fractures in the urban Indian population. BMC Musculoskelet Disord. 2010;11:49. doi: 10.1186/1471-2474-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lan TY, Hou SM, Chen CY, Chang WC, Lin J, Lin CC, et al. Risk factors for hip fracture in older adults: a case-control study in Taiwan. Osteoporos Int. 2010;21(5):773–784. doi: 10.1007/s00198-009-1013-z. [DOI] [PubMed] [Google Scholar]
- 31.Jitapunkul S, Yuktananandana P, Parkpian V. Risk factors of hip fracture among Thai female patients. J Med Assoc Thail. 2001;84(11):1576–1581. [PubMed] [Google Scholar]
- 32.Johnell O, Gullberg B, Kanis JA, Allander E, Elffors L, Dequeker J, et al. Risk factors for hip fracture in european women: the MEDOS study. J Bone Miner Res. 1995;10(11):1802–1815. doi: 10.1002/jbmr.5650101125. [DOI] [PubMed] [Google Scholar]
- 33.Feskanich D, Bischoff-Ferrari HA, Frazier AL, Willett WC. Milk consumption during teenage years and risk of hip fractures in older adults. JAMA Pediatr. 2014;168(1):54–60. doi: 10.1001/jamapediatrics.2013.3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fujiwara S, Kasagi F, Yamada M, Kodama K. Risk factors for hip fracture in a Japanese cohort. J Bone Miner Res. 1997;12(7):998–1004. doi: 10.1359/jbmr.1997.12.7.998. [DOI] [PubMed] [Google Scholar]
- 35.Benetou V, Orfanos P, Zylis D, Sieri S, Contiero P, Tumino R, et al. Diet and hip fractures among elderly Europeans in the EPIC cohort. Eur J Clin Nutr. 2011;65(1):132–139. doi: 10.1038/ejcn.2010.226. [DOI] [PubMed] [Google Scholar]
- 36.Feart C, Lorrain S, Ginder Coupez V, Samieri C, Letenneur L, Paineau D, et al. Adherence to a Mediterranean diet and risk of fractures in French older persons. Osteoporos Int. 2013;24(12):3031–3041. doi: 10.1007/s00198-013-2421-7. [DOI] [PubMed] [Google Scholar]
- 37.Owusu W, Willett WC, Feskanich D, Ascherio A, Spiegelman D, Colditz GA. Calcium intake and the incidence of forearm and hip fractures among men. J Nutr. 1997;127(9):1782–1787. doi: 10.1093/jn/127.9.1782. [DOI] [PubMed] [Google Scholar]
- 38.Kanis J, Johnell O, Gullberg B, Allander E, Elffors L, Ranstam J, et al. Risk factors for hip fracture in men from southern Europe: the MEDOS study. Mediterranean osteoporosis study. Osteoporos Int. 1999;9(1):45–54. doi: 10.1007/s001980050115. [DOI] [PubMed] [Google Scholar]
- 39.Tavani A, Negri E, La Vecchia C. Calcium, dairy products, and the risk of hip fracture in women in northern Italy. Epidemiology. 1995;6(5):554–557. doi: 10.1097/00001648-199509000-00017. [DOI] [PubMed] [Google Scholar]
- 40.Cumming RG, Klineberg RJ. Case-control study of risk factors for hip fractures in the elderly. Am J Epidemiol. 1994;139(5):493–503. doi: 10.1093/oxfordjournals.aje.a117032. [DOI] [PubMed] [Google Scholar]
- 41.Nieves JW, Grisso JA, Kelsey JLA. Case-control study of hip fracture: evaluation of selected dietary variables and teenage physical activity. Osteoporos Int. 1992;2(3):122–127. doi: 10.1007/BF01623818. [DOI] [PubMed] [Google Scholar]
- 42.Meyer HE, Pedersen JI, Løken EB, Tverdal A. Dietary factors and the incidence of hip fracture in middle-aged Norwegians: a prospective study. Am J Epidemiol. 1997;145(2):117–123. doi: 10.1093/oxfordjournals.aje.a009082. [DOI] [PubMed] [Google Scholar]
- 43.Bonjour JP, Lecerf JM. Dairy micronutrients: new insights and health benefits. Introduction J Am Coll Nutr. 2011;30(5 Suppl 1):399S. doi: 10.1080/07315724.2011.10719982. [DOI] [PubMed] [Google Scholar]
- 44.Bolland MJ, Grey A. A case study of discordant overlapping meta-analyses: vitamin D supplements and fracture. PLoS One. 2014;9(12):e115934. doi: 10.1371/journal.pone.0115934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med. 1992;327(23):1637–1642. doi: 10.1056/NEJM199212033272305. [DOI] [PubMed] [Google Scholar]
- 46.Lei M, Hua LM, Wang DW. The effect of probiotic treatment on elderly patients with distal radius fracture: a prospective double-blind, placebo-controlled randomised clinical trial. Benef Microbes. 2016;7(5):631–637. doi: 10.3920/BM2016.0067. [DOI] [PubMed] [Google Scholar]
- 47.Michaelsson K, Holmberg L, Ljunghall S, Mallmin H, Persson PG, Wolk A. Effect of prefracture versus postfracture dietary assessment on hip fracture risk estimates. Int J Epidemiol. 1996;25(2):403–410. doi: 10.1093/ije/25.2.403. [DOI] [PubMed] [Google Scholar]
- 48.Yoshita K, Arai Y, Nozue M, Komatsu K, Ohnishi H, Saitoh S, et al. Total energy intake and intake of three major nutrients by body mass index in Japan: NIPPON DATA80 and NIPPON DATA90. Am J Epidemiol. 2010;20(Suppl 3):S515–S523. doi: 10.2188/jea.JE20090219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leslie WD, Orwoll ES, Nielson CM, Morin SN, Majumdar SR, Johansson H, et al. Estimated lean mass and fat mass differentially affect femoral bone density and strength index but are not FRAX independent risk factors for fracture. J Bone Miner Res. 2014;29(11):2511–2519. doi: 10.1002/jbmr.2280. [DOI] [PubMed] [Google Scholar]
- 50.De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16(11):1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 51.Tang X, Liu G, Kang J, Hou Y, Jiang F, Yuan W, et al. Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLoS One. 2013;8(4):e55077. doi: 10.1371/journal.pone.0055077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sogaard AJ, Holvik K, Omsland TK, Tell GS, Dahl C, Schei B, et al. Age and sex differences in body mass index as a predictor of hip fracture: a NOREPOS study. Am J Epidemiol. 2016;184(7):510–519. doi: 10.1093/aje/kww011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description: Search Phrases for a) PubMed, and b) EMBASE. (DOC 37 kb)
Title: Selection procedure for inclusion and exclusion of the studies. (DOC 50 kb)
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.


