Abstract
Rationale and Objectives
To evaluate the comparative performance of high-fidelity liquid crystal display (LCD) and cathode ray tube (CRT) devices for mammography applications, and to assess the impact of LCD viewing angle on detection accuracy.
Materials and Methods
Ninety 1k × 1k images were selected from a database of digital mammograms: 30 without any abnormality present, 30 with subtle masses, and 30 with subtle microcalcifications. The images were used with waived informed consent, HIPAA compliance, and IRB approval. With post-processing presentation identical to those of the commercial mammography system used, 1k × 1k sections of images were viewed on a monochrome CRT and a color LCD in native grayscale, and with a grayscale representative of images viewed from a 30° or 50° off-normal viewing angle. Randomized images were independently scored by four experienced breast radiologists for the presence of lesions using a 0–100 grading scale. To compare diagnostic performance of the display modes, observer scores were analyzed using Receiver Operating Characteristic (ROC) and Analysis of Variance (ANOVA).
Results
For masses and microcalcifications, the detection rate in terms of the area under the ROC curve (Az) showed a 2% increase and a 4% decrease from CRT to LCD, respectively. However, differences were not statistically significant (p > 0.05). The viewing angle data showed better microcalcification detection but lower mass detection at 30° viewing orientation. The overall results varied notably from observer to observer yielding no statistically discernable trends across all observers, suggesting that within the 0–50° viewing angle range and in a controlled observer experiment, the variation in the contrast response of the LCD has little or no impact on the detection of mammographic lesions.
Conclusions
While CRTs and LCDs differ in terms of angular response, resolution, noise, and color, these characteristics seem to have little influence on the detection of mammographic lesions. The results suggest comparable performance in clinical applications of the two devices.
Keywords: Diagnostic accuracy, Digital mammography, Liquid Crystal Display, Cathode Ray Tube, Medical Display
Introduction
The image technology for screening mammography is currently in a transition, with conventional analog screen-film mammography systems being gradually replaced by digital mammography systems. The transition is expected to accelerate because of a recent large-scale trial that found an essential equivalence of the two modalities for the majority of women but a notable advantage of digital for women with dense breasts (1).
Softcopy display is an integral element of digital mammography without which many advantages of digital mammography such as efficiency and optimized image quality would not be fully realized. Currently, softcopy display of digital mammograms may be achieved via two types of display devices: liquid crystal display (LCD) and cathode ray tube (CRT). These displays present distinctly differing resolution and noise characteristics. LCDs offer higher resolution but poorer noise performance than CRTs (2). LCD technology has also enabled incorporation of color without an undue effect on display contrast, a common problem with color CRT displays. Color CRTS have notably lower contrast ratios than their monochrome counterpart; that is not the case for LCDs. This improvement suggests the possibility of using LCDs for diagnosis. However, LCDs exhibit a non-Lambertian angular response characteristic by which the luminance and contrast of the displayed image changes as a function of viewing angle. Display specifications often characterize the angular response in terms of angular cones within which the luminance ratio exceeds 10, a threshold applicable to text applications. Using this metric, angular response specifications of 160–170 degrees are common. However, within those ranges, the contrast of the medical images can change significantly, potentially impacting the diagnostic utility of LCDs.
The differing characteristics of LCDs and CRTs have led radiologists to prefer one display type or another. However, except for a few isolated investigations (3–6), this preference has not been related to diagnostic performance. Consequently, there is a clinical urgency to substantiate the relative performance of CRT and LCD displays. The purpose of this study was to assess the comparative performance of a conventional monochrome CRT and a newer color LCD of similar pixel size for use in digital mammography. Furthermore, the study examined the impact of LCD viewing angle response on detection accuracy in screening mammography. Distinct from some prior studies, this study was based on native digital mammograms with native lesions interpreted in clinical-like viewing conditions.
Materials and Methods
Images
Ninety digital mammograms were acquired with a full-field digital mammography system (Fischer Imaging Corporation, Denver, CO). The data were used with waived informed consent, compliance with Health Insurance Portability and Accountability Act (HIPAA), and approval from the Institutional Review Board (IRB). All images were acquired with a detector pixel size of 50 micrometers, and were photo-timed at a dose level corresponding to the clinical use of that particular imaging device, as approved by the Food and Drug Administration (FDA). Thus, images represented dose (and consequently, image noise) values reflective of clinical mammography operations. All images were post-processed according to their clinical protocol without any additional post-processing applied. The images consisted of 30 Craniocaudal (CC)-view mammograms with confirmed subtle masses, 30 with confirmed microcalcification clusters, and 30 normal images without any lesion present. All lesions were confirmed with biopsy. The normal cases were also confirmed with a one-year follow up. A 1024 pixel × 1024 pixel image was extracted from each mammogram, with each lesion (if present) at approximate center of the image.
Display Systems
Two display devices were employed in this investigation: A monochrome cathode ray tube (CRT) (MGD 521; Barco, Duluth, Georgia) and a color liquid crystal display (LCD) (T-221; IBM, White Plains, NY). Both devices were set up according to their native specifications. The CRT display employed a 0.148 mm pixel size, a 2048 pixel × 2560 pixel matrix size, 19.1″ diagonal display dimension, and luminance values ranging between 0.5 and 308 cd/m2. The LCD employed a 0.125 mm pixel size, a 3840 pixel × 2400 pixel matrix size, 22.1″ diagonal display dimension, and luminance values ranging between 0.83 and 235 cd/m2. Both displays were used in the portrait mode, were calibrated to the Grayscale Standard Display Function (GSDF) within their applicable luminance range (7), and complied with the AAPM requirements (8).
A purpose of the study was to assess the impact of variation on LCD image contrast as a function of viewing angle. Instead of mandating a particular viewing orientation, which could restrict observers’ freedom of movement and ease of participation, observers viewed all images in a normal (ie, perpendicular) viewing orientation. However, the contrast of the images was modified using custom look-up tables (LUTs) so that the grayscale of the images would appear as if they were being viewed from an oblique orientation. The two LUTs used were based on the measured contrast response of the LCD display at 30- and 50-degree viewing orientations, reported earlier for these two viewing orientations (9). Figure 1a presents a schematic representation of this procedure. Most of the pixel values of breast anatomy images correspond to pixel value ranges that darken the image when the LUT for an oblique viewing orientation is applied. This behavior is exactly as expected and can be appreciated by the relatively high ranges of image pixel values, illustrated in Figure 1b for a typical image.
Figure 1.
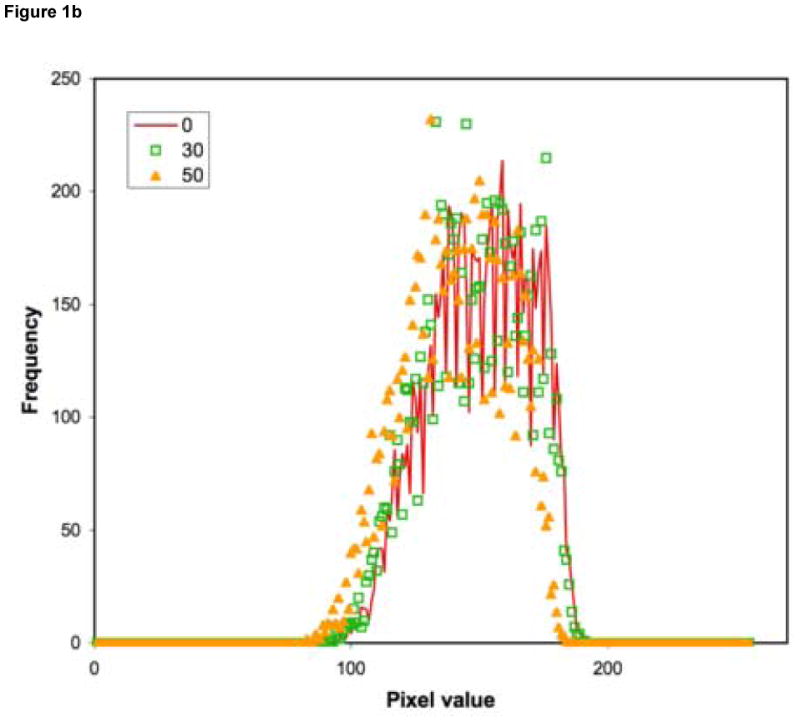
(a) An 8-bit representation of the LUT for the formation of the oblique viewing grayscale. The figure illustrates the measured luminance response of the LCD display (IBM T221) at the normal, 30-degree, and 50-degree oblique viewing orientations (19). The oblique responses are the averages of the display performance in the 45-degree and 135-degree azimuthal directions. The arrows note two examples. The LUT was formed as a transformation of the images in the 12-bit pixel value space such that the image pixel in the normal viewing orientation would render a grayscale value consistent with the desired 30-degree and 50-degree orientations. (b) Histogram of a typical image displayed with grayscale corresponding with 0-, 30-, and 50-degree viewing angles.
The display devices were thus compared in four modes: 1) CRT in its native performance, 2) LCD in its native performance, 3) LCD with modified images representing a 30-degree viewing orientation, and 4) LCD with modified images representing a 50-degree viewing orientation. Figure 2 illustrates a few examples of the images without and with modified contrast.
Figure 2.
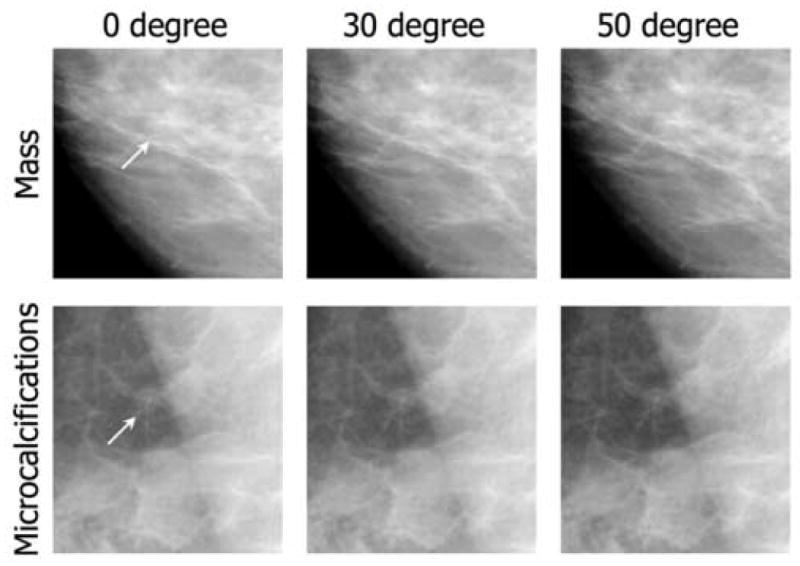
Examples of images with altered LUT to render contrast and luminance values consistent with the 30 degree and 50 degree oblique viewing orientations. Lesions are located at the center of the example images.
Observer Experiment
For the observer performance experiment, all images were viewed on all four display modes as noted above. All images had the standard clinical image post-processing of the mammography system manufacturer, and were displayed on the CRT and LCD devices with comparable sizes corresponding to the pixel sizes of the two display devices; no image interpolation was applied. A custom graphical user interface displayed one image at the time at the center of the display with a medium gray background surrounding for optimum adaptation. Four experienced breast radiologists participated in the experiment (15 ± 1 years’ average experience). After an initial training, each image was scored by each observer for the presence of a lesion (either mass or microcalcification) using a 100-point grading scale from a lesion definitely not present (0%) to a lesion definitely present (100%) (10). While each lesion, if present, was located at the approximate center of an image, that information was not disclosed to the observer. For each display, the images were viewed in a random order. The order of the display modes was also randomized for different observers to average out any potential memory effects. All interpretations took place in a zero ambient lighting condition. The observers were allowed to window and level the images to allow viewing utilities similar to clinical conditions. However, the observers were satisfied with the default settings and did not make any changes. The observers were given the freedom to take as much time needed for their reading and view the images from any distance. However, to reduce the required reading time, the magnification was fixed.
Statistical Analysis
The data were analyzed using the Receiver Operating Characteristic (ROC) methodology, which was based on the established multi-reader multi-case (MRMC) analysis developed by Dorfman, Berbaum, and Metz (LABMRMC, April 1997, University of Chicago) (11). Observer scores were processed to calculate the ROC curves and the estimated areas under the curves (Az) for each observer, lesion type, and display modes. Results from different observers were averaged to obtain the overall performance for each display mode (12). In order to deduce the statistical significance of the differences, an analysis of variance (ANOVA) was performed on the scores using commercial software (Excel 2000; Microsoft Corporation, Redmond, WA), assuming Gaussian behaviors for underlying probability distributions. A P values smaller than 0.05 was considered statistically significant.
Results
Detection of Microcalcifications
The impact of display mode on the detection of microcalcification distributions appeared to be highly observer-dependent, indicated by a notable variability in the ROC curves across observers as a function of display mode. For Observer A, the CRT yielded higher sensitivity at the lower specificity portion of the ROC curve, but that advantage disappeared at the higher specificity portion, where oblique viewing showed some advantage. A somewhat similar trend was evident for Observer C. For Observers B and D, display mode had minimal impact on the detection of microcalcifications.
Averaging ROCs for the detection of microcalcification distributions across all observers, the CRT display performed better than the LCD (Table 1), except for the LCD in the 30° viewing orientation in the higher sensitivity regions (Figure 3a). For areas under the ROC curves (Figure 3b), the CRT and the LCD at 30° viewing orientation yielded better performance than the other two display modes. Overall, the CRT yielded 4% higher performance than the LCD at normal viewing orientation. However, given the size of the error bars, neither of these trends can be considered of statistical significance.
Table 1.
The values for the areas under the ROC curve (Az) associated with the detection of microcalcifications and masses for each display (CRT and LCD at different viewing angles) and for each of the four observers.
| Observer | CRT_0 | LCD_0 | LCD_30 | LCD_50 |
|---|---|---|---|---|
| Microcalcification detection | ||||
| A | 0.84 ± 0.05 | 0.83 ± 0.05 | 0.88 ± 0.04 | 0.87 ± 0.05 |
| B | 0.90 ± 0.05 | 0.87 ± 0.06 | 0.89 ± 0.05 | 0.88 ± 0.05 |
| C | 0.91 ± 0.04 | 0.82 ± 0.06 | 0.92 ± 0.03 | 0.84 ± 0.05 |
| D | 0.89 ± 0.04 | 0.87 ± 0.04 | 0.89 ± 0.04 | 0.87 ± 0.05 |
| All | 0.89 ± 0.04 | 0.85 ± 0.05 | 0.90 ± 0.04 | 0.86 ± 0.05 |
| Mass detection | ||||
| A | 0.76 ± 0.07 | 0.83 ± 0.05 | 0.79 ± 0.06 | 0.81 ± 0.06 |
| B | 0.85 ± 0.07 | 0.82 ± 0.06 | 0.85 ± 0.06 | 0.88 ± 0.05 |
| C | 0.89 ± 0.04 | 0.84 ± 0.05 | 0.83 ± 0.05 | 0.83 ± 0.05 |
| D | 0.80 ± 0.06 | 0.85 ± 0.05 | 0.76 ± 0.06 | 0.81 ± 0.06 |
| All | 0.82 ± 0.06 | 0.84 ± 0.05 | 0.81 ± 0.06 | 0.83 ± 0.05 |
Figure 3.
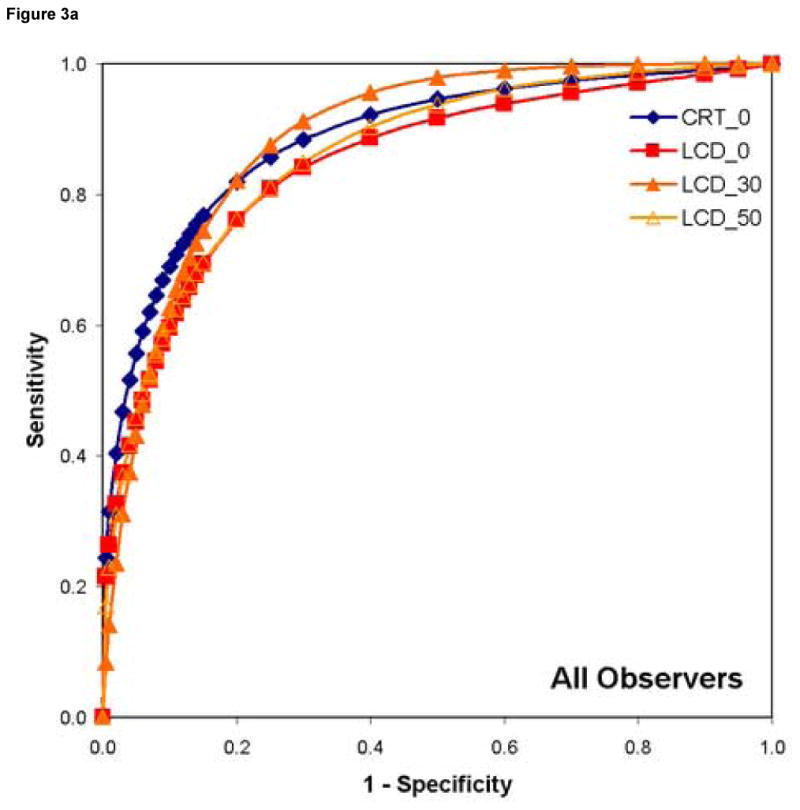
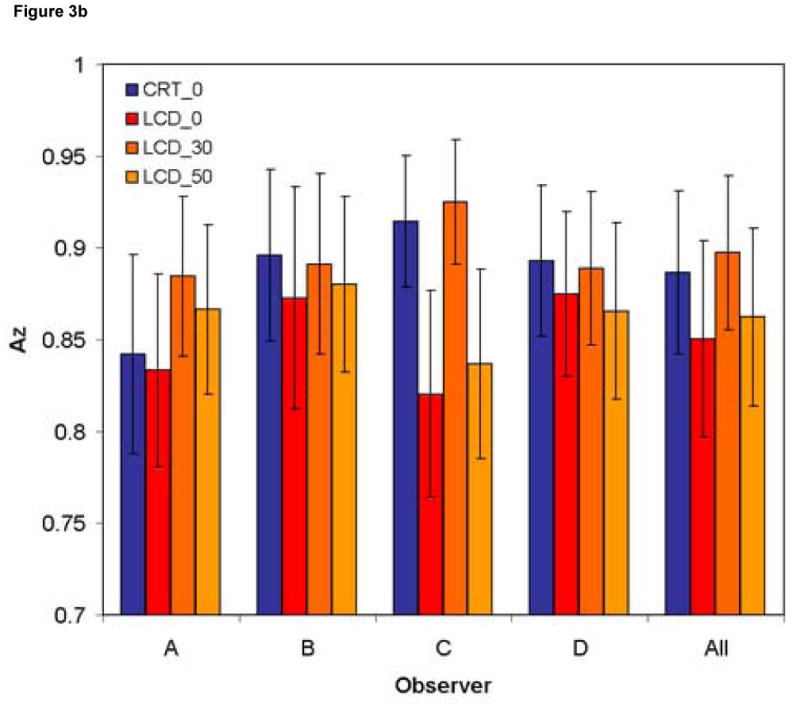
The observer-averaged ROC curves for (a) the detection of microcalcifications and (b) the associated area under the curves for each of the display modes.
The ANOVA results did not indicate a statistically significant difference for the detection of microcalcifications (Table 2). The only statistically significant impact (P < 0.05) was, as expected, due to case variability, given the variation in the observer scores for a given image.
Table 2.
The results of the ANOVA analysis indicating that only the case variability exhibited a statistically significant impact.
| Source of variability | Mass detection p-value |
uCa detection p-value |
|---|---|---|
| Display | 0.5284 | 0.1316 |
| Case | < 0.05* | < 0.05* |
| Reader | 0.5094 | 0.5517 |
| Display-Case | 0.8405 | 0.0766 |
| Display-Reader | 0.5875 | 0.8975 |
| Reader-Case | < 0.05* |
5% significance level
Detection of Masses
Compared to the microcalcification detection cases, the ROC results for the detection of masses across observers showed more observer variability. Observer C showed higher performance with the CRT, with degrading performance at increased viewing angles. However, the other three observers exhibited different trends with respect to the impact of display mode, with some showing a reduced performance with increased viewing angle and others the opposite.
Averaging ROCs across observers for each of the display modes (Table 1 and Figure 4a), the CRT and the LCD display performed similarly in the low specificity region except for the LCD in the 30° viewing orientation, exhibiting lower performance. In the high-sensitivity/high-specificity region, however, the LCD performed better regardless of the viewing orientation. Considering the fact that most breast radiologists usually operate in this region of the ROC curve, this superiority may translate into superior clinical performance for LCDs. Given the variation as a function of specificity level, while the total areas under the ROC curves showed different trends for different observers (Figure 4b), they did not demonstrate a notable trend when averaged across observers. Averaged across all observers, the CRT yielded 2% lower performance than the LCD at normal viewing orientation (p > 0.05). Similar to the analysis of microcalcification detection, the ANOVA results for the detection of masses did not indicate a statistically significant difference (Table 2). As also noted earlier, the only statistically significant impact was due to case variability, as expected, given the variation in the observer scores for a given image.
Figure 4.

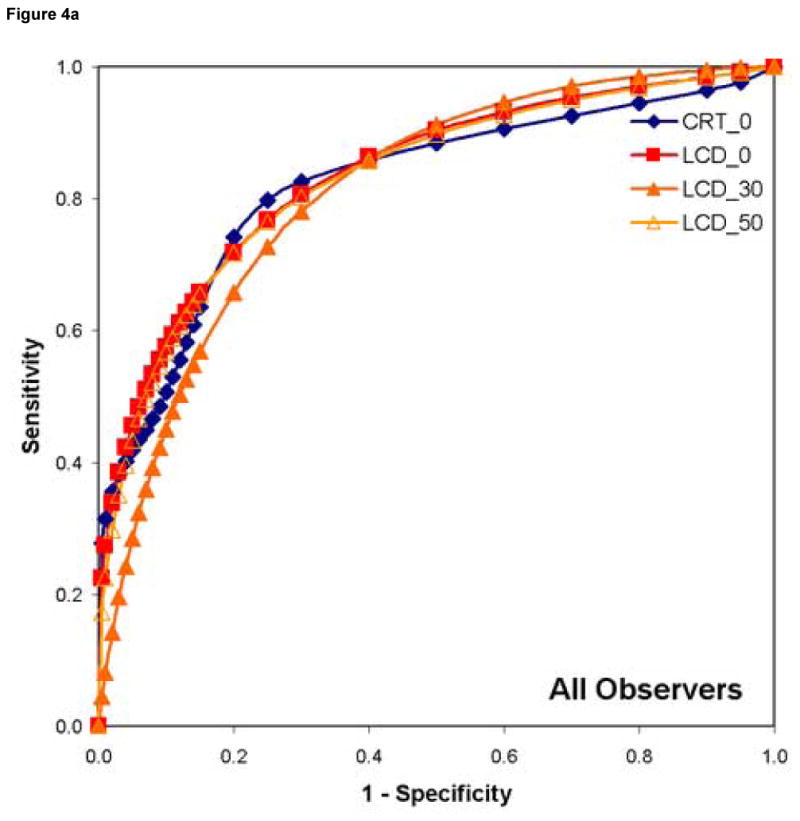
The observer-averaged ROC curves for (a) the detection of masses and (b) the associated area under the curves for each of the display modes.
Discussion
While the interpretation of medical images was historically performed with transilluminated films, the transition to digital imaging has brought about a corresponding transition to softcopy displays (13). In the early years of digital transition, the CRT was the only technology for softcopy display of medical images (14). More recent advances in the fabrication of large-area, thin-film transistors have enabled the manufacturing of LCDs with the quality and large size suitable for medical applications. Fueled by their size and energy efficiencies, and improved durability and stability, LCDs are gradually replacing CRTs in many medical settings (13). The possibility of using a color display for reading medical images, non-existent with the CRT due to the degrading impact of the CRT color apparatus on image contrast, has been a further incentive in the move from the CRT to the LCD. Even so, the legacy of color CRTs, as devices inherently inferior to monochrome CRTs, has prevented a rapid adoption of color LCDs in radiology.
Mammography is perhaps the last of the radiological applications to transition to digital (15). Earlier systems were approved for clinical use with CRT displays only. While forces similar to those impacting other medical applications will likely steer digital mammography towards LCD deployment, a number of potential disadvantages have not yet been fully addressed. Among those, LCDs, compared to CRTs, exhibit notable structure noise due to their inherent pixel architecture, reduced contrast with changes in viewing orientation, and higher levels of minimum luminance. While advancements in LCD technology will continue to lessen these deficiencies, it is important to ascertain their impact on diagnostic performance, which is of significant importance in digital mammography.
In this study, we compared a conventional monochrome CRT and a color LCD, of comparable pixel size, in terms of their diagnostic utility for the detection of subtle mammographic lesions. The study included the impact of contrast degradation due to changes in LCD viewing orientation. The particular color LCD display tested in this study (IBM T221) has been the highest resolution color LCD available in the market, though recently became unavailable. With its basic physical and psychophysical performance reported previously (5, 6, 16–18), its performance on medical images had not yet been reported. The observer experiments were conducted with the displays as installed for clinical use, and with as many display functionalities as possible to emulate their clinical use. Notwithstanding a few trends noted in Results, the findings indicated no statistically significant impact of either the display type or the viewing orientation on diagnostic performance. While failing to demonstrate a difference cannot be the basis to claim that there is no difference, nonetheless, if there were to be a notable impact, we would have expected to see some evidence to that effect. We thus conclude that the display modes under investigation were either equivalent, or their differences were close enough that they could be easily masked by normal variations in the diagnostic performance of experienced breast radiologists.
While indicating null results, the findings of our study have notable clinical implications. First and foremost, the overall similarity in the performance of the CRT and LCD displays suggests that either type of display may be used for digital mammography with less hesitation over quality. While LCDs appear to have adequate quality and are thus suitable for clinical use, they are not so significantly better to justify replacing existing CRTs with LCDs. Thus, the question of technology replacement should be answered more on the basis of cost and utilization than quality. Secondly, the findings of this study did not indicate any particular advantage or disadvantage of a color LCD. Color LCDs often have lower maximum luminance values than their monochrome versions due to the light absorption of their added color filters. From that standpoint, a monochrome LCD, compared to its color version, enables operation at brighter ambient lighting conditions while staying in compliance with AAPM guidelines (8). However, provided that a color LCD has other favorable hi-fidelity attributes, such as a high luminance ratio, and is being used in proper ambient lighting conditions, its color features may offer additional functionalities and ease of use not available on monochrome LCDs.
The findings of our study are in general concert with prior work aiming to compare LCDs and CRTs. Prior research has also noted no statistically significant differences between CRTs and LCDs in the detection of nodules in chest radiography (19), and the detection and classification of breast lesions in mammograms (3, 4). However, Krupinski et al found oblique viewing orientations for LCDs to be inferior to normal, perpendicular viewing (6). That study was based on a larger number of images than ours and thus had more statistical power to demonstrate a measurable influence of the viewing orientation, if present. However, that study was limited to masses only, included lesions inserted electronically, and used a grayscale LCD with a matrix size identical to that of the employed CRT. These differences could potentially lead to different conclusions by the two studies. Nonetheless, putting the findings of the prior studies in perspective, one may conclude that the impact of display modality on diagnostic accuracy is so small that it is easily masked by the normal statistics associated with reading digital mammograms.
The similar diagnostic performance of CRTs and LCDs that we found is somewhat surprising given the importance of resolution in digital mammography (15) and the superior resolution performance of LCDs (2, 20). For a given image, an, LCD display should provide a better representation of the higher spatial frequency content of a given image. Our results can perhaps be attributed to the structured noise of LCDs. Created by a large portion of the “real-estate” of each pixel devoted to complex electronic circuitries controlling the pixel luminance, structured noise has a notable presence in the images displayed on an LCD. While the perception of this noise can vary, depending on the pixel size, and the viewing distance and orientation, it is always present and thus distort a medical image (2). While not directly supported by the results of the study, the findings suggest that the resolution advantages of the LCD are counterbalanced by its noise disadvantages, thus yielding similar performance to that of the CRT.
The results of our study on the impact of viewing orientation on diagnostic performance were also unexpected. A number of prior investigations have noted the dramatic impact of viewing orientation on the contrast of LCDs (17, 21). A recent study reported a reduced detectability with increased viewing angle (22). However, our study found no measurable impact. This may be due to anatomical noise, or more specifically, the impact of viewing angle on the relationship between lesion contrast and background contrast. Against a uniform background, a reduction in lesion contrast would naturally reduce its likelihood of detection. However, in a non-uniform anatomical background, for the lesion to be detected, it needs to be distinguished from the contrasts associated with the normal background features surrounding it. Increased viewing angle reduces background contrast as well as lesion contrast. Thus, the detectability of the lesion is no longer determined by lesion contrast alone but also by its contrast in relationship to the contrast of the background. It is likely that the interplay of these two types of contrast may render the conspicuity of a lesion insensitive to changes in the viewing angle. Again, while this assertion cannot be directly supported by the results of this study, it can provide a likely mechanism to explain them.
While general implications can be drawn from the findings of our study with respect to the clinical utility of LCDs and CRTs, the study had several limitations. First, strictly speaking, the findings are directly applicable only to the two particular display devices tested at their particular installation settings. While conclusions can be drawn for typical displays, extrapolations of the findings should be confirmed by follow-up studies. Second, our study did not investigate other key performance characteristics of LCDs such as minimum luminance performance or structured noise. Third, our study addressed only contrast change with respect to viewing angle. Associated geometric changes in terms of distortions and changes in spatial resolution and visibility of structure noise with viewing angle were not included. Furthermore, the timing performance was not taken into consideration because the purpose of the study was to compare oblique views of LCD and CRT displays. Thus, the primary difference between the two displays would be contrast rendition as the geometrical distortions would be generally the same. Finally, our observer experiment used partial (as opposed to full) mammograms, with the lesion location (though not disclosed to the observers) at the approximate center of the images. This strategy, which may have limited the extent of the visual search applied by each observer, was implemented because the display effects would manifest themselves more substantially when other sources of variability were kept under control. Finally, we used images acquired at only one, clinically-applicable average dose/noise level. The impact of display quality might vary as a function of varying noise levels in mammographic images. Addressing these limitations may serve as worthy objectives for future investigations.
Conclusions
With digital mammography, there is an inherent need to use softcopy display devices to view the images. While LCDs and CRTs exhibit notable variations in their physical characteristics, those do not appear to translate into notable performance advantages or disadvantages. In our study, while some trends could be appreciated, such as CRT’s slight superiority to detect microcalcifications and masses in the low and high sensitivity regions, respectively, there was no statistical significance between the monochrome CRT and the color LCD evaluated. Findings may reflect the structured noise found in LCD displays. Furthermore, there was no statistically significant difference between LCD at normal and at up to 50-degree oblique viewing orientations. Those results may be explained on the basis of the overall impact of contrast change as a function of viewing angle on the conspicuity of the lesions taken into account both the lesion and the background contrasts. Notwithstanding the limitations of the study, our overall findings suggest that CRT and LCD devices have largely comparable performances for digital mammography applications, and that the angular response might not have as much of a negative impact as predicated by studies focused on uniform backgrounds.
Acknowledgments
Support:
The work was supported in part by a grant from the NIH, R44 CA099068.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ehsan Samei, Duke Advanced Imaging Laboratories, Departments of Radiology Physics and, Biomedical Engineering, and Medical Physics Graduate Program, Duke University Medical Center, Durham, NC 27705, Tel. 919-684-7852, FAX 919-684-1492.
Ananth Poolla, Fischer Imaging Corporation, Denver, CO 80241.
Michael J. Ulissey, Parkland Memorial Hospital, Dallas, TX 75390-8896.
John M. Lewin, Diversified Radiology of Colorado, Denver, CO 80205.
References
- 1.Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 2.Saunders RS, Jr, Samei E. Resolution and noise measurements of selected commercial medical displays. Med Phys. 2006;33:308–319. doi: 10.1118/1.2150777. [DOI] [PubMed] [Google Scholar]
- 3.Krupinski EA, Johnson J, Roehrig H, Nafziger J, Fan J, Lubin J. Use of a human visual system model to predict observer performance with CRT vs LCD display of images. J Digit Imaging. 2004;17:258–263. doi: 10.1007/s10278-004-1016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saunders RS, Jr, Samei E, Baker JA, et al. Comparison of LCD and CRT displays based on utility for mammographic tasks. Acad Radiol. 2006;13:1317–1326. doi: 10.1016/j.acra.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Averbukh AN, Channin DS, Homhual P. Comparison of human observer performance of contrast-detail detection across multiple liquid crystal displays. J Digit Imaging. 2005;18:66–77. doi: 10.1007/s10278-004-1035-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krupinski EA, Johnson J, Roehrig H, Nafziger J, Lubin J. On-axis and off-axis viewing of images on CRT displays and LCDs: observer performance and vision model predictions. Acad Radiol. 2005;12:957–964. doi: 10.1016/j.acra.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Digital Imaging and Communications in Medicine (DICOM) Part 14: Grayscale Display Standard Function. Rosslyn, VA: National Electrical Manufacturers Association; 2000. NEMA-PS3.14. [Google Scholar]
- 8.Samei E, Badano A, Chakraborty D, et al. Assessment of display performance for medical imaging systems: Executive summary of AAPM TG18 report. Med Phys. 2005;32:1205–1225. doi: 10.1118/1.1861159. [DOI] [PubMed] [Google Scholar]
- 9.Samei E, Wright SL. The effect of viewing angle response on DICOM compliance of LCD displays. Proc SPIE. 2004;5371:170–177. [Google Scholar]
- 10.Saunders RS, Jr, Samei E, Hoeschen C. Impact of resolution and noise characteristics of digital radiographic detectors on the detectability of lung nodules. Med Phys. 2004;31:1603–1613. doi: 10.1118/1.1753112. [DOI] [PubMed] [Google Scholar]
- 11.Dorfman DD, Berbaum KS, Metz CE. Receiver operating characteristic rating analysis. Generalization to the population of readers and patients with the jackknife method. Invest Radiol. 1992;27:723–731. [PubMed] [Google Scholar]
- 12.Swetz JA, Pickett RM. Evaluation of Diagnostic Systems. New York, NY: Academic Press; 1982. [Google Scholar]
- 13.Samei E. Advances in Digital Radiography. Oak Brook, IL: Radiological Society of North America (RSNA) Publication; 2003. Assessment of display quality; pp. 109–121. [Google Scholar]
- 14.Samei E. AAPM/RSNA physics tutorial for residents: technological and psychophysical considerations for digital mammographic displays. Radiographics. 2005;25:491–501. doi: 10.1148/rg.252045185. [DOI] [PubMed] [Google Scholar]
- 15.Yaffe MJ, Mainprize JG. Detectors for digital mammography. Technol Cancer Res Treat. 2004;3:309–324. doi: 10.1177/153303460400300401. [DOI] [PubMed] [Google Scholar]
- 16.Averbukh AN, Channin DS, Flynn MJ. Assessment of a novel, high-resolution, color, AMLCD for diagnostic medical image display: luminance performance and DICOM calibration. J Digit Imaging. 2003;16:270–279. doi: 10.1007/s10278-003-1718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samei E, Wright SL. Viewing angle performance of medical liquid crystal displays. Med Phys. 2006;33:645–654. doi: 10.1118/1.2168430. [DOI] [PubMed] [Google Scholar]
- 18.Fifadara DH, Averbukh AN, Channin DS, Badano A. Effect of viewing angle on luminance and contrast for a five-million-pixel monochrome display and a nine-million-pixel color liquid crystal display. J Digit Imaging. 2004;17:264–270. doi: 10.1007/s10278-004-1021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang SA, Seo JB, Choi BK, et al. Liquid-crystal display monitors and cathode-ray tube monitors: a comparison of observer performance in the detection of small solitary pulmonary nodules. Korean J Radiol. 2003;4:153–156. doi: 10.3348/kjr.2003.4.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Badano A, Hipper SJ, Jennings RJ. Luminance effects on display resolution and noise. Proc SPIE. 2002;4681:305–313. [Google Scholar]
- 21.Badano A, Fifadara DH. Goniometric and conoscopic measurements of angular display contrast for one-, three-, five-, and nine-million-pixel medical liquid crystal displays. Med Phys. 2004;31:3452–3460. doi: 10.1118/1.1824198. [DOI] [PubMed] [Google Scholar]
- 22.Badano A, Gallas BD. Detectability decreases with off-normal viewing in medical liquid crystal displays (abs) RSNA Proceedings. 2005:307. doi: 10.1016/j.acra.2005.08.015. [DOI] [PubMed] [Google Scholar]



