Abstract
Context
Information on health-care utilization and the economic burden of disease are essential to understanding service demands, service accessibility, and practice patterns. This information may also be used to enhance the quality of care through altered resource allocation. Thus, a systematic review of literature on the economic impact of caring for SCI/D veterans would be of great value.
Objective
To systematically review and critically appraise the literature on the economics of the management of veterans with SCI/D.
Methods
Medline, EMBASE and PsycINFO databases were searched for articles on economic impact of management of SCI/D veterans, published from 1946 to September/2016. The STROBE statement was used to determine publication quality.
Results
The search identified 1,573 publications of which 13 articles fulfilled the inclusion/exclusion criteria with 12 articles focused on costs of management of SCI/D veterans; and, one cost-effectiveness analysis. Overall, the health care costs for the management of SCI/D veterans are substantial ($30,770 to $62,563 in 2016 USD per year) and, generally, greater than the costs of caring for patients with other chronic diseases. The most significant determinants of the higher total health-care costs are cervical level injury, complete injury, time period (i.e. first year post-injury and end-of-life year), and presence of pressure ulcers.
Conclusions
There is growing evidence for the economic burden of SCI/D and its determinants among veterans, whereas there is a paucity of comparative studies on interventions including cost-effectiveness analyses. Further investigations are needed to fulfill significant knowledge gaps on the economics of caring for veterans with SCI/D.
Keywords: Spinal cord injury, Neurotrauma, Military, veterans, War, Health economics
Introduction
The incidence rates of traumatic spinal cord injury (SCI) vary from 6.2 to 174 per million inhabitants annually. The prevalence of traumatic SCI is estimated to be 50 to 906 per million inhabitants in the general population around the world.1 Although traumatic SCI has a relatively low incidence when compared with other chronic diseases, its economic impact is considerable. In the United States, the economic burden based on the total national hospital charges related to SCI was estimated at 1.69 billion in 2009 USD (or 2.09 billion in 2016 USD).2 In Canada, the total direct hospital costs associated with SCI was estimated at 40.6 million CAD in 2001 (or 44.55 million in 2016 USD).3 There is a paucity of data on the incidence, prevalence and costs of non-traumatic SCI. In a recent study in Spain, the incidence rate of non-traumatic SCI was estimated at 12.1 per million inhabitants yearly with neoplasm as the most common etiology (34.8%) followed by mechanical diseases (17.6%), vascular diseases (15.5%), infections (9.1%) and multiple sclerosis (7.8%).4 In an Australian study, individuals with non-traumatic SCI had lower rates of hospitalizations and lower mean costs per admission for treatment of secondary complications than individuals with traumatic SCI.5
Today, clinicians are commonly confronted by the escalating healthcare costs and scarce financial sources in their quest to provide proper patient care.6,7 While ethical thinking trumps cost-benefit analysis when young patients with neurotrauma require a life-saving or rescue procedure, clinicians are still reminded to provide cost-effective care, particularly, when equivalent alternatives are available.8 This underscores the need for practitioners and administrators to understand the costs and benefits of available treatments. These same dilemmas regarding quality of care and optimal resource allocation are also relevant in military healthcare settings.
The monetary costs of a war include expenses incurred before, during, and after the war. Using the United States as a case study, the overall incurred and committed costs of the wars in Iraq, Afghanistan, Pakistan and Syria, and on Homeland Security from 2001 to 2016 totalized $3.6 trillion USD as of August 2016.9 Future costs to the Department of Defense and State Department for overseas contingency operations (including wars in Iraq, Afghanistan, and Syria), Homeland Security for prevention and response to terrorism, and projected spending with veterans (including future obligations for veterans medical and disability) will add up to at least 1.2 trillion USD until 2053.9 The US Department of Veterans Affairs estimated $64.65 billion USD for medical care costs including $848 million USD for the rehabilitation care program such as Blind Rehabilitation Service and Spinal Cord Injury and Disorders Services for the year 2016.10 “The mission of Spinal Cord Injury and Disorders Services is to promote the health, independence, quality of life and productivity of individuals with spinal cord injuries and disorders through efficient delivery of acute rehabilitation, psychological, social, vocational, medical and surgical care, professional training, as well as patient and family education”.10 Based on data from the US Department of Veterans Affairs, veterans eligible for medical care and other benefits in 2009 represented approximately 17% of the 250,000 Americans with spinal cord injury or disease (SCI/D) including veterans with non-traumatic SCI, veterans with traumatic SCI that was not related to a war act, and veterans with war-related SCI.11 Moreover, the results of a recent systematic review revealed that the demographics and injury characteristic of the war-related SCIs among military personnel are different from the traumatic SCI among civilians.12 In brief, military personnel with war-related SCI are mostly comprised of young, white, men, predominantly sustaining thoracic (followed by cervical level), severe (complete or AIS A) SCI caused by gunshot or explosion and often associated with at least another bodily injury.12
Given the importance of Health Economics and the uniqueness of the group of veterans with SCI/D, this systematic review was undertaken to synthesize and critically appraise the literature on the economic impact of SCI/D, and potential cost-effective strategies.
Methods
Search strategy
The literature search was carried out using Medline, Excerpta Medica dataBASE (EMBASE), and PsycINFO in order to obtain articles on the health economics in the acute treatment and rehabilitation of veterans with SCI/D that were published from 1946 to September 2016. The search criteria included subject headings (“spinal cord injury” OR “spinal cord injuries”) AND (“trauma” OR “wounds and injuries”) AND (“military” OR “military personnel” OR “war” OR “veterans” OR “combatants” OR “soldiers”). The search was limited to “humans”. Abstracts and, if needed for clarification, actual articles were screened to find original papers that studied the economic impact of management of veterans with SCI/D or cost-effective analyses. Case reports, conference abstracts only, and editorials were excluded.
Selection process, data abstraction and publication appraisal
All titles and abstracts captured in the literature search were reviewed by two reviewers (JCF and SG). Articles considered relevant based on the title and abstract search were included. Discrepancies between the reviewers were resolved by consensus. All articles that fulfilled the inclusion and exclusion criteria were appraised by the same two reviewers (JCF and SG) using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.13 This is a widely accepted instrument among researchers and endorsed by the editorial boards of several scientific journals (e.g. Lancet, British Medical Journal and Neurology) as a checklist “to guide reporting of observational research”.14 While the STROBE group did not primarily intend to use this checklist to assess the quality of publications, compliance to the STROBE checklist has been accepted as an alternative for quality assessment of the publications on observational studies since there is no validated instrument for this purpose.14,15 The items contained within the STROBE statement were scored as 0 or 1, with a score of 1 provided for each checklist item that was properly completed or, when the item had multiple sub-items (i.e. items 12, 13, 14 and 16), 1 point was added if most of the sub-items of that specific item were appropriately completed. Using this scoring system, a maximum score of 22 would indicate the paper fulfilled all requirements for a high-quality publication. Cost-effectiveness studies were appraised according to methodological recommendations from the Panel on Cost-Effectiveness in Health and Medicine.16–18 Consensus was sought if there was any initial discordance between both reviewers with regards to the scoring of the articles, the costing information or the appraisal on the cost-effectiveness analysis. Finally, relevant data was abstracted from the selected articles following screening and prior to data synthesis.
Definitions
According to the US Department of Veterans Affairs, a veteran is defined as “a person who served in the active military service and who was discharged or released under conditions other than dishonorable”.19
Severity of SCI was classified according to the American Spinal Injury Association [ASIA] Impairment Scale (AIS) contained within the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) as follows: (i) patients with motor and sensory complete SCI (AIS A); (ii) patients with motor complete but sensory incomplete SCI (AIS B); (iii) patients with motor incomplete SCI where the majority of the key muscles below the neurological level have a muscle grade less than 3 (AIS C); and (iv) patients with motor incomplete SCI where the majority of the key muscles below the neurological level have a muscle grade greater than or equal to 3 (AIS D).20
Converted costing data
All published costs were revised to 2016 US dollars (USD) using medical-cost inflation rates as reported by the US Bureau of Labor Statistics.21 These medical-cost rates are part of the overall US government's Consumer Price Index for All Urban Consumers (CPI-U) that measures price inflation in the United States using December-to-December data instead of the annual average data. Of note, these data use the inflation of actual medical costs, which is much more reliable than the inflation of health-insurance premiums that usually rises faster than the direct medical costs.
All published costs were initially converted to 2015 USD using a publicly available inflation calculator.22 This program was created by Mr. Tom R. Halfhill using inflation data from 1935 to 2015 according to reporting data from the US Bureau of Labor Statistics.21,22 In keeping with most recent available data from the US Bureau of Labor Statistics, a medical-cost inflation rate of 3.8% was used to convert all published costs to 2016 USD.21
Results
Selected publications
The literature search identified 1,573 publications of which 13 fulfilled the inclusion and exclusion criteria (Table 1). Of those, 12 articles reported costs of management of veterans with SCI/D 23–34; and, only 1 article reported a cost-effectiveness analysis using data from veterans with SCI/D.35
Table 1.
Included references as classified by study type, data sources, and quality of the publications based on the STROBE statement
| Reference | Study type | Data sources | STROBE |
|---|---|---|---|
| 23 | Retrospective cohort study | Health Economics Resource Center (HERC) Average Cost Database; Financial Management System (FMS) database, and Cost Distribution Report (CDR) data. | 15 |
| 24 | Retrospective cohort study | VA Health Economics Resource Center database. | 15 |
| 25 | Retrospective cohort study | 22 VA Integrated Service Networks (VISNs); geographic information system (GIS); Quality Enhancement Research Initiative (QUERI). | 17 |
| 26 | Retrospective cohort study | VA Spinal Cord Dysfunction Registry; VA National Prosthetic Patient Database (NPPD); Disability Resources and Educational Services (DRES) Student Database at the University of Illinois at Urbana-Champaign; self-reported costs by civilians. | 17 |
| 27 | Retrospective cohort study | 3 Veteran Health Administration (VHA) sites that are participating in a multisite SCI research program (Tampa, Augusta, and Boston); Decision Support System (DSS) National Data Extracts (NDE). | 19 |
| 28 | Retrospective cohort study | Veterans Health Administration databases. | 19 |
| 29 | Retrospective cohort study | VA SCI Quality Enhancement Research Initiative, Medicare, VA Health Care Systems. | 20 |
| 30 | Retrospective cohort study | VA Allocation Resource Center; VA Medical SAS Inpatient and Outpatient Datasets, Fee Basis Files paid by the VA; Decision Support System (DSS); Pharmacy NDE, and SCD Registry. | 20 |
| 31 | Retrospective cohort study | VA Allocation Resource Center; VA Medical SAS Inpatient and Outpatient Datasets, Fee Basis Files paid by the VA; Decision Support System (DSS); Pharmacy NDE, and SCD Registry. | 21 |
| 32 | Retrospective case series | DSS for the VA Centers in Ohio, United states. | 17 |
| 33 | Retrospective cohort study | VA DSS NDE; VA Fee Basis program files; Federal Supply Schedule; VA staff in the Acquisition and Material Management Service; Health Services Research and Development. | 12 |
| 34 | Retrospective cohort study | VA Medical Database, and Decision Support System Pharmacy Database. | 16 |
| 35 | Cost-effectiveness analysis | 5 Veterans Affairs medical centers. | 22 |
STROBE: Strengthening the Reporting of Observational Studies in Epidemiology; SCD: spinal cord disease; VA: Veterans Affairs
Most of the 1,573 publications were excluded because they were focused on secondary complications, management, or epidemiology of SCI, or they were case reports, conference abstracts, or editorials (Fig. 1).
Figure 1.
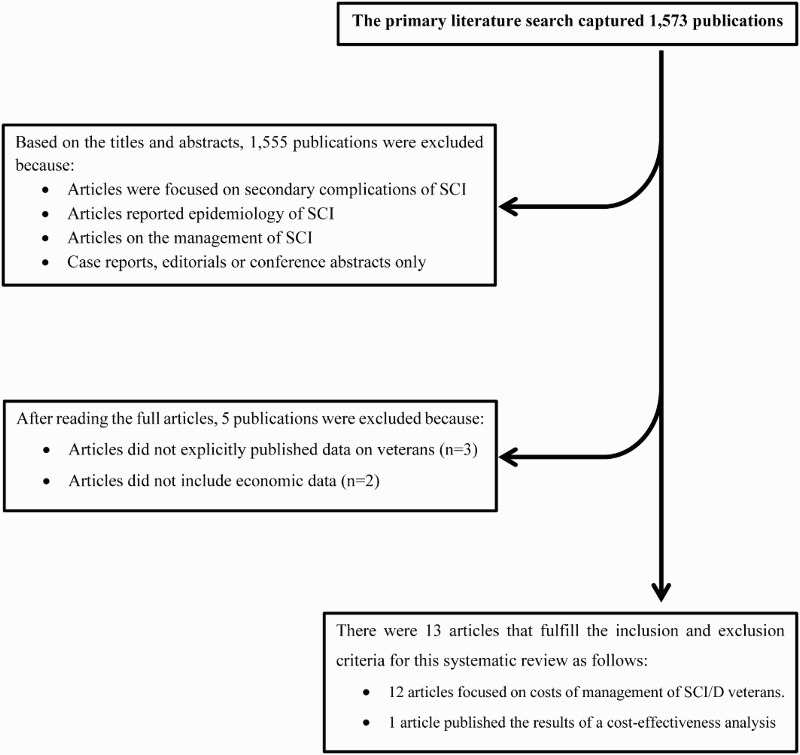
Flow diagram showing the steps of the literature search and selection of the articles included in this systematic review.
All selected articles were classified as either retrospective cohort studies or cost-effectiveness analysis published between 2003 and 2014. Their scores based on the STROBE statement varied from 15 to 22 with a trend towards higher scores in the more recent publications (Table 1). The only cost-effectiveness analysis was carried out following many recommendations from the Panel on Cost-Effectiveness in Health and Medicine.16–18,35 However, there are a few methodological concerns in the study by Sinnott et al. as follows: (i) the numerator of the cost-effectiveness analysis did not comprise some of the costs from a societal perspective (e.g. economic costs endured by employers, other employees, and the rest of society, including friction costs related to absenteeism and employee turnover); (ii) the effectiveness was measured in quality adjusted-life years (QALYs) that were generated using Veterans Rand 6 Dimension derivate from Veterans RAND 36-Item Health Survey, which does not consider the full range of impact on an individual’s health status change, including loss of income and leisure activities; (iii) no discount rate was applied; and (iv) only limited sensitivity analysis was reported.16–18,35
Costs of caring for veterans with SCI/D
The published costing data on the management of veterans with SCI/D were exclusively acquired from the VA health care administrative databases from the United States. All costing information was collected from the fiscal years 1998 to 2010. The average annual costs of caring for veterans with SCI/D varied from $30,770 to $62,563 in 2016 USD among the studies (Table 2). The inpatient rehabilitation per diem mean costs of veterans with SCI/D varied from $765 to $830 USD between 1998 and 2000 (mean per diem costs was estimated at $808 in 2000 USD or $1,436 in 2016 USD), which were more costly than the “rehabilitation program” and “blind rehabilitation program” at the VA Health Care Systems.23
Table 2.
Summary of the studies on costs of veterans with spinal cord injury/disease (SCI/D) according to this systematic review
| Reference | Participants | Costing data | Original costs for SCI/D | Current costs for SCI/D | Notes | Results |
|---|---|---|---|---|---|---|
| 23 | Veterans with SCI/D who underwent inpatient rehabilitation (number of cases is not available) | Direct VA inpatient rehabilitation budgetary costs | (Mean costs per year in 2000 USD): Per diem costs for SCI/D: 1998: $765 1999: $830 2000: $829 Average: $808 Overall costs for SCI/D: 1998: $263,374,200 1999: $295,264,200 2000: $248,113,897 Mean: $268,917,432 Inpatient rehabilitation categories: SCI: $268,917,432 Rehab: $200,057,995 Blind rehab: $111,694,191 |
(Mean costs per year in 2016 USD): Per diem costs for SCI/D: 1998: $1,360 1999: $1,475 2000: $1,473 Average: $1,436 Overall costs for SCI/D: 1998: $468,112,783 1999: $524,793,037 2000: $440,989,614 Mean: $477,965,144 Inpatient rehabilitation categories: SCI: $477,965,144 Rehab: $207,660,199 Blind rehab: $115,938,570 |
The Health Economics Resource Center (HERC) Average Cost Database is based on allocated budgets and, hence, it may not precisely reflect the true costs of production services. Also, the cost data included spending with facility and physician but not the cost of capital financing or malpractice. |
The mean per diem costs of inpatient rehabilitation of veterans with SCI/D was estimated in $808 in 2000 USD (or $1,436 in 2016 USD). The inpatient rehabilitation of veterans with SCI/D was the most expensive among the categories of inpatient rehabilitation in the study. |
| 24 | Veterans with SCI/D aged 65 to 79 years (n=5,401); and Veterans with SCI/D aged 80 or older (n=993) |
Direct VA inpatient and outpatient costs |
(Mean costs per case in 2000 USD): Aged 65 to 79 years: Total costs: $31,306 Costs without long-term care: $25,193* Aged 80 years or older: Total costs: $31,714 Costs without long-term care: $22,290 * Top 3 most costly chronic conditions after SCI: Aged 65 to 79 years: Renal failure: $20,967 Lung cancer: $17,145 All dementias: $16,795 Aged 80 years or older: Renal failure: $ $19,302 Lung cancer: $15,252 All dementias: $ $17,056 |
(Mean costs per case in 2016 USD): Aged 65 to 79 years: Total costs: $55,642 Costs without long-term care: $44,777 * Aged 80 years or older: Total costs: $56,367 Costs without long-term care: $39,618 * Top 3 most costly chronic conditions after SCI: Aged 65 to 79 years: Renal failure: $37,266 Lung cancer: $30,473 All dementias: $29,850 Aged 80 years or older: Renal failure: $34,307 Lung cancer: $27,108 All dementias: $30,315 |
The proportion of users of long-term care varied as follows: Aged 65 to 79 years: SCI (15.6%), renal failure (11.6%), lung cancer (16%), and all dementias (19.4%) Aged 80 years or older: (SCI 20.4%), renal failure (15.5%), lung cancer (19.5%), and all dementias (22.8%) |
The total costs to care for elderly veterans with SCI/D did not significantly differ between the age-related groups. However, the oldest veterans with SCI/D had significantly lower health care costs after excluding the long-term care costs when compared with SCI/D veterans who aged 65 to 79 years. The most expensive chronic condition among elderly veterans was SCI/D followed by renal failure, lung cancer and all dementias. |
| 25 | 19,234 veterans with SCI/D | Direct VA inpatient and outpatient costs identified using Quality Enhancement Research Initiative (QUERI) system |
(Mean costs per case in 2000 USD): Inpatient medical/surgical services: $5,690 Other inpatient services: $15,115 Outpatient: $3,512 Pharmacy: $2,777 Overall costs: $27,094 Top 3 most common QUERI conditions: Psychiatric diseases ($9,704), diabetes ($7,709), and substance abuse ($9,489) Top 3 most costly QUERI conditions after SCI: Chronic heart failure ($14,959); stroke ($14,679); colorectal cancer ($14,422) |
(Mean costs per case in 2016 USD): Inpatient medical/surgical services: $10,113 Other inpatient services: $26,865 Outpatient: $6,242 Pharmacy: $4,936 Overall costs: $48,156 Top 3 most common QUERI conditions: Psychiatric diseases ($17,248), diabetes ($13,702), and substance abuse ($16,865) Top 3 most costly QUERI conditions after SCI: Chronic heart failure ($26,588); stroke ($26,090); colorectal cancer ($25,633) |
The top 3 most common QUERI conditions were psychiatric disorders (23.3%), diabetes (18.5%), and substance abuse (13.5%). The least common QUERI conditions were colorectal cancer, SCI, and HIV/AIDS, accounting for less than 1% of QUERI patients. Of note, the QUERI groups are not mutually exclusive since patients may have multiple conditions. |
The inpatient care costs represented 76.8% of the total direct health care costs for veterans with SCI/D, whereas outpatient costs (13%) and outpatient pharmacy (10.2%) had less impact on their total direct health care costs. The costs to care for veterans with SCI/D were the highest among the QUERI chronic conditions in the study, even though it represents less than 1% of them. |
| 26 | 98 working-age veterans with SCI/D (aged 18 to 64 years); and 93 college-educated civilians of working age with SCI/D (aged 18 to 64 years) |
Costs of the assistive technology (AT) devices self-reported by civilians and veterans with SCI/D. The VA costs reported by the veterans were also verified using the National Prosthetic Patient Database (NPPD). | (Costs in 1998-2002 USD) Mean cost per device per person across all categories was $2,032 for veterans vs. $2,155 for civilians. Mean cost per Manual Mobility and Independent Living (MMIL) device was $859 for veterans vs. $859 Mean cost per Powered Mobility and Independent Living (PMIL) device was $ 9,472 for veterans vs. $ 7,947 for civilians. Mean cost per prosthetics & orthotics device was $ 178 for veterans vs. $47* |
Costing data could not be properly converted to 2016 USD due to the lack of original data by year. Using the extremes of all original costs in 1998 USD and all original costs in 2002 USD, the mean cost per device per person across all device categories could vary from $3,298 to $3,892 in 2016 USD among veterans, and from $3,498 to $4,127 in 2016 USD among civilians. |
SCI/D veterans were significantly older, more likely to be male, non-white than the SCI/D civilians. While both groups had similar degree of disability, the proportion of paraplegics was greater among civilians (57%) when comparted to veterans (47%). Of note, the veterans usually underreported the AT costs in comparison with the NPPD information | Self-reported costing data were underestimated among veterans with SCI/D when compared with NPPD data. The two most frequently owned assistive technology device categories were also the most expensive (i.e. MMIL devices and PMIL devices). The mean costs of the Prosthetics & Orthotics devices were significantly higher for the veterans than for the civilians. |
| 27 | 675 veterans with SCI for at least 2 years who use wheelchair as a primary means of mobility. | Direct VA inpatient and outpatient costs | (Mean costs per case in 2005 USD): Cervical complete SCI: $28,334 incomplete SCI: $22,134 Thoracic complete SCI: $20,925 incomplete SCI: $16,792 Lumbar complete SCI: $23,158 incomplete SCI: $17,561 Overall: $21,450 Inpatient costs (n=233): $30,866 Outpatient costs: $10,795 |
(Mean costs per case in 2016 USD): Cervical complete SCI: $40,644 incomplete SCI: $31,751 Thoracic complete SCI: $30,017 incomplete SCI: $24,088 Lumbar complete SCI: $33,220 incomplete SCI: $25,191 Overall costs: $30,770 Inpatient costs: $44,277 Outpatient costs: $15,485 |
Proportion of inpatient costs (by service): nursing (53.1%); pharmacy (6.5%); surgery (5.7%); laboratory (2%); Radiology (3.8%); other costs (28.9%) Proportion of outpatient costs (by service): SCI clinic (25.8%); Prosthetic (17.9%); VA-paid home care (15.5%); SCI home (3.6%); laboratory (3.3%); Radiology (3%); contract nursing homes (2.6%); dental (2.2%); phone/ancillary medicine (1.9%); primary care (1.5%); other costs (22.9%) |
The total inpatient care costs ($7,191,725 in 2005 USD) were close to the total outpatient costs ($7,286,719 in 2005 USD). The overall costs to care for veterans with chronic SCI were higher for cervical complete SCI and lower for thoracic incomplete SCI. Among the inpatient costs, nursing services (53.1%) were the most expensive followed by other costs (28.9%), pharmacy (6.5%) and surgery (5.7%). Among the outpatient costs, SCI clinic services (25.8%) were the most expensive followed by prosthetic services (17.9%) and VA-paid home care (15.5%). |
| 28 | 5,518 veterans with paraplegia after SCI/D; and 4,521 veterans with tetraplegia after SCI/D included in the Veterans Equitable Resource Allocation (VERA) system |
Direct VA inpatient and outpatient costs | (Median costs per case in USD in different years) Paraplegia: 1998: $18,894 1999: $21,553 2000: $22,408 2001: $19,661 2002: $19,838 Tetraplegia: 1998: $20,237 1999: $24,917 2000: $24,967 2001: $26,018 2002: $21,762 |
(Median costs per case in 2016 USD) Paraplegia: 1998: $36,182 1999: $39,878 2000: $39,827 2001: $33,408 2002: $32,196 Tetraplegia: 1998: $38,754 1999: $46,102 2000: $44,376 2001: $44,210 2002: $35,318 |
Based on the available data, the overall median costs per case were estimated in $22,402 (in 2002 USD) or $36,357 (in 2016 USD) for paraplegics, and $25,799 (in 2002 USD) or $41,869 (in 2016 USD) for tetraplegics |
The median costs for VERA complex class of veterans with paraplegia were estimated in $22,402 USD (2002) or $36,357 USD (2016). The median costs for VERA complex class of veterans with tetraplegia were estimated in $25,799 USD (2002) or $41,869 USD (2016). |
| 29 | 2,008 veterans with SCI/D during their last 24 months of life | Direct VA medical and surgical costs based on Medicare, other inpatient costs (e.g. home care, long-term hospital care) and outpatient costs based on national costs per diem. | (Mean costs per case in 2016 USD) Overall costs: Final year: $61,900 Previous year: $24,900 Overall costs: $86,800 Traumatic SCI: $98,400 Non-traumatic: $97,600 Paraplegia: $100,400 Tetraplegia: $95,700 Major conditions: Nephritis: $120,200 Septicemia: $99,500 Other: $97,300 COPD: $93,100 Blood vessel disease: $91,700 Pneumonia: $90,400 Diabetes: $84,400 Hernia: $80,900 Heart disease: $79,800 Stroke: $73,200 Cancer: $71,300 |
(Mean costs per case in 2001 USD) Overall costs: Final year: $105,181 Previous year: $42,310 Overall costs: $147,491 Traumatic SCI: $167,202 Non-traumatic: $165,842 Paraplegia: $170,600 Tetraplegia: $162,614 Major conditions: Nephritis: $204,244 Septicemia: $169,071 Other: $165,333 COPD: $158,196 Blood vessel disease: $155,817 Pneumonia: $153,608 Diabetes: $143,413 Hernia: $137,466 Heart disease: $135,596 Stroke: $124,382 Cancer: $121,153 |
The most common “major causes of death” and their 2-year costs (in 2016 USD) were: cancer (20.9%; $49 million), influenza/ pneumonia (15.1%; $44.9 million), heart disease (13.5%; 35.4 million), septicemia (5.9%; $19.3 million), stroke (5.1%; $12.3 million), COPD (4.5%; $13.8 million), diabetes (5.3%; $14.7 million), nephritis (4%; $15.8 million), hernia (2.8%; $7.4 million), blood vessel disorders (1.4%; 4.2 million), and other causes (21.5%; $68.8 million) | The costs of caring for SCI/D veterans near their end of life (24 month) are substantially higher than the costs of caring for VA veterans without SCI/D. Most the costs of caring for veterans with SCI/D near their end of life incur in the final year (71.3%), that significantly escalate in the last 6 months before death. Although nephritis was the top major condition with the highest costs for the end of life among veterans with SCI/D, the most expensive major condition for the VA to care for veterans with SCI/D in their near end of life was cancer, followed by influenza/ pneumonia, and heart disease. |
| 30 | Veterans with SCI/D and pressure ulcer (n=1,220); and veterans with SCI/D without pressure ulcer (n=9,757) | Direct VA expenditures for patient care either provided at VA facilities or provided in non-VA facilities but paid for by VA. | (Mean annual costs in 2008 USD) SCI/D veterans with pressure ulcer: Outpatient costs: $19,844 Pharmacy costs: $2,394 Inpatient costs: $91,341 Total costs: $100,935 SCI/D veterans without pressure ulcer: Outpatient costs: $11,829 Pharmacy costs: $1,613 Inpatient costs: $13,754 Total costs: $27,195 |
(Mean annual costs in 2016 USD) SCI/D veterans with pressure ulcer: Outpatient costs: $20,598 Pharmacy costs: $3,050 Inpatient costs: $116,373 Total costs: $128,596 SCI/D veterans without pressure ulcer: Outpatient costs: $15,071 Pharmacy costs: $2,055 Inpatient costs: $17,523 Total costs: $35,564 |
Both groups were statistically similar with regards to their age, sex distribution, ethnic subgroups, and most of the co-morbidities; however, veterans with pressure ulcer were more likely to have a traumatic SCI, diabetes mellitus, prior hospitalization, and higher mean household income. | SCI/D veterans with pressure ulcers were more costly and had longer length of hospital stay than SCI/D veterans without ulcers. After adjustments, the total annual costs per patient were $73,021 USD (or $75,796 in 2016 USD) higher among veterans with pressure ulcer and their annual hospital admissions were about 52 days longer than SCI/D veterans without ulcer. |
| 31 | 8,645 veterans with traumatic SCI; and 2,795 veterans with non-traumatic SCI/D |
Direct VA expenditures for patient care either provided at VA facilities or provided in non-VA facilities but paid for by VA. | (Mean costs per year in 2008 USD) Traumatic SCI: Outpatient costs: $16,655 Pharmacy costs: $1,938 Inpatient costs: $30,513 Total costs: $49,106 Non-traumatic SCI/D: Outpatient costs: $15,860 Pharmacy costs: $2,030 Inpatient costs: $27,581 Total costs: $45,470 |
(Mean costs per year in 2016 USD) Traumatic SCI: Outpatient costs: $21,219 Pharmacy costs: $2,469 Inpatient costs: $38,875 Total costs: $62,563 Non-traumatic SCI/D: Outpatient costs: $20,206 Pharmacy costs: $2,586 Inpatient costs: $35,139 Total costs: $57,931 |
The group of veterans with traumatic SCI were significantly younger and predominantly white men with less co-morbidities, more pressure ulcers, and greater median household income than their counterparts with non-traumatic SCI/D. | Veterans with non-traumatic SCI/D had greater overall outpatient utilization; however, there were no significant differences between the group of veterans with traumatic SCI and the group of veterans with non-traumatic SCI/D with regards to their total health care costs. |
| 32 | 76 veterans with SCI/D received traditional care; and 20 veterans with SCI/D received teleconsultation for wound care | Direct inpatient and outpatient costs from the VA Decision Support System (DSS) for the VA Centers in Ohio | (Median costs during 30 months in 2007 USD) Outpatient encounters: Teleconsultation: $3,956* Traditional care: $474 Inpatient admissions: Teleconsultation: $139,473 Traditional care: $70,666 |
(Median costs during 30 months in 2016 USD) Outpatient encounters: Teleconsultation: $5,227 * Traditional care: $626 Inpatient admissions: Teleconsultation: $184,270 Traditional care: $93,363 |
This retrospective economic analysis used a convenience sample | There were no significant differences in inpatient cost between the two strategies. However, teleconsultation group had a significantly higher median cost per outpatient encounter than the traditional care group. |
| 33 | Standard of care versus telehealth care for treatment of pressure ulcers after SCI using low-, medium- and high-cost technology (Base estimate for the model: 20,000 veterans with SCI) |
Direct costs primarily gathered from US Department of VA administrative records. | (Medium costs per year in 2007 USD) Prevention care: Standard of care (with homecare): $23,673 Standard of care (without homecare): $9,242 High-cost tech: $21,349 Medium-cost technology: $8,066 Treatment: Standard of care (with homecare): $11,234 Standard of care (without homecare): $8,408 Low-cost tech: $6,325 |
(Medium costs in 2016 USD) Prevention care: Standard of care (with homecare): $31,276 Standard of care (without homecare): $12,210 High-cost tech: $28,206 Medium-cost technology: $10,657 Treatment: Standard of care (with homecare): $14,842 Standard of care (without homecare): $11,109 Low-cost tech: $8,356 |
Low-cost technology: digital cameras and e-mail. Medium-cost technology: interactive videoconferencing machine plus station-to-station (hub and spoke) teleconferencing. High-cost technology: interactive videoconferencing machine that was installed in the patient’s home. |
Telehealth care was less expensive than standard care when patients and facilities used low-cost technology (e.g. digital cameras and e-mail). Telehealth care using low- and medium-cost technology may reduce the costs of prevention and treatment of SCI-related pressure ulcers. |
| 34 | 5,233,994 veterans with SCI and/or other chronic diseases received care within the VA system in the Fiscal Year 2010. |
The overall cost of VA care for each patient was estimated by aggregating costs for inpatient care, outpatient care, prescription drugs, and contract care from several sources. |
(Mean costs per year in 2016 USD) Triad of diabetes, hypertension, SCI: $77,546 among veterans younger than 65 years old; and $65,905 among veterans aged 65 years or older |
(Mean costs per year in 2010 USD) Triad of diabetes, hypertension, SCI: $92,586 among veterans younger than 65 years old; and $78,687 among veterans aged 65 years or older |
The authors did not report the cost for each condition separately. | Among younger veterans, the triad “chronic heart failure, chronic renal failure, chronic obstructive pulmonary disease” was the most expensive for the year 2010; the triad “diabetes, hypertension, SCI” was the fourth most expense. Among older veterans, the triad “diabetes, hypertension, SCI” was the most expensive for the year 2010. |
SCI: spinal cord injury; SCI/D: spinal cord injury or disease; COPD: chronic obstructive pulmonary disease; AIDS: Acquired Immunodeficiency Syndrome; * indicates statistically significant differences
Other investigations compared the costs of caring for SCI/D veterans with the costs of management of other more common diseases among veterans without SCI/D.24,25,34 In all prior studies, the mean annual health care costs of caring for veterans with SCI/D exceeded the costs of management of other chronic diseases (Table 2). Among elderly veterans (age 65 years or older), Yu, Ravelo et al. reported that SCI was the most expensive disease among the 29 most costly chronic conditions followed by renal failure, lung cancer, all dementias, and others.24 While the veterans more commonly developed psychiatric disorders (23.3%), diabetes (18.5%), and substance abuse (13.5%), SCI accounted for less than 1% of the VA database.24 In another study using VA Health Care System data, Yu, Cowper et al. documented that SCI was the most expensive disease (mean annual cost of $27,094 in 2000 USD) among 29 of the most common chronic conditions among veterans, followed by chronic heart failure, stroke and colorectal cancer.25 Studying the most costly triads among VA patients with at least 3 out of 28 chronic conditions, Yoon et al. reported “diabetes, hypertension, SCI” as the most expensive triad among elderly veterans with mean annual costs of $65,905 in 2010 USD, and the fourth most costly among veterans younger than 65 years of age with mean annual costs of $77,546 in 2010 USD.34
Hendrick et al. reported that the mean costs per device across all categories of assistive technologies were similar between a group of working-age veterans with SCI/D and another group of working-age civilians with SCI/D ($2,032 and $2,155 in 2008 USD, respectively), even though the mean costs of the prosthetics & orthotics devices were significantly higher for the veterans than for the civilians ($178 and $47 in 2008 USD, respectively).26 Of note, the two most commonly owned assistive technology device categories by veterans and civilians with SCI/D were the Manual Mobility and Independent Living (MMIL; including wheelchair, ambulatory support device, seating, cushion, bed, exercise equipment) and Powered Mobility and Independent Living (PMIL; including automated wheelchair, motor vehicle devices, residential devices), which were also the most expensive.26
Components and determinants of the health care costs of the veterans with SCI/D
The costing information on the components of the health care of veterans with SCI/D was detailed in four articles.25,27,30,31 Based on these published data, the proportion of inpatient care costs varied from 50.6% to 80.4% of the overall health care costs, whereas the proportion of the outpatient care costs varied from 13% to 43.5%, and the proportion of outpatient pharmacy costs varied from 2.1% to 10.3% (Table 2). French et al. also reported that the inpatient care costs ($30,866 in 2005 USD) were higher than the outpatient care costs ($10,795 USD).27 The authors also described that nursing services comprised the highest proportion of the inpatient costs, followed by other costs, pharmacy, surgery, radiology and laboratory costs (Table 2). The costs associated with outpatient SCI clinic services comprised the highest proportion of the outpatient care costs, followed by other costs, prosthetic services, VA-paid home care services, SCI home services, laboratory, Radiology, contract nursing home services, dental services, phone/ancillary medicine services, and primary care services (Table 2).
Other investigators have previously reported potential determinants of the health care costs among veterans with SCI/D, which included admission into a long-term care facility, presence of pressure ulcers, level and severity of injuries, and nature of the SCI/D (traumatic versus nontraumatic SCI/D). Analyzing costing data from elderly veterans with SCI/D, Yu, Ravelo et al. found that veterans aged 65 to 79 years had similar mean health care costs to veterans aged 80 years or older ($31,306 versus $31,714 in 2005 USD, respectively).24 However, the mean health care costs with long-term care expenses were significantly higher among veterans aged 65 to 79 years when compared with older veterans ($25,193 versus $22,290 in 2005 USD, respectively).24 In another retrospective cohort study, Stroup et al. documented that the mean annual health care costs for veterans with pressure ulcers were substantially higher than the mean annual costs for veterans without pressure ulcers ($128,596 versus $34,648 in 2016 USD, respectively).30
The effects of the level and severity of SCI on health care costs were reported in three previous studies (Table 2). While the results of two studies suggested that veterans with tetraplegia showed a trend towards higher annual health care costs than veterans with paraplegia, another investigation reported no substantial effects of the level of SCI on the near end-of-life costs among veterans with SCI/D.27–29 In a subsequent study, Yu et al. showed that the majority of the costs of caring for veterans with SCI/D near end of their life (i.e. during the last 24 months) incurred in the final year (71.3%), which considerably escalated in the last 6 months before death.29 The mean annual costs of caring for veterans with tetraplegia varied from $31,751 to a mean annual cost during their last 24 months of life of $162,614 in 2016 USD, whereas the average annual costs of caring for veterans with paraplegia varied from $24,088 to a mean annual cost during their last 24 months of life of $170,600 in 2016 USD.27,29 The median health care costs for a veteran with tetraplegia were $41,869 in 2016 USD, whereas a veteran with paraplegia had median health care costs of $36,357 in 2016 USD. French et al. also documented that veterans with incomplete SCI have a trend towards lower health care costs than their counterparts with complete SCI.27
The potential influence of the nature of the SCI/D on the health care costs was reported in two prior studies. St. Andre et al. documented that the mean annual costs of caring for veterans with non-traumatic SCI/D were statistically similar to their counterparts with traumatic SCI ($57,931 and $62,563 in 2016 USD, respectively), even though veterans with non-traumatic SCI/D were significantly older, had greater number of comorbidities and required more often outpatient services than veterans with traumatic SCI.31 Similarly, Yu et al. showed that the mean annual health care costs of caring for veterans with traumatic SCI were statistically comparable to the mean annual health care costs among veterans with non-traumatic SCI/D ($167,202 and $147,491 in 2016 USD, respectively).29
Intervention-based studies and health care costs of caring for veterans with SCI/D
This literature search captured three intervention-based studies with potential cost-saving benefits in the care of veterans with SCI/D (Tables 2 and 3). Young-Hughes and Simbartl compared traditional wound care with expert wound care provided using teleconsultation for veterans with SCI/D.32 While there were no significant differences between the two treatment groups with regards to their median inpatient care costs, the teleconsultation group had a significantly higher median cost per outpatient encounter than the traditional care group.32
Table 3.
Summary on cost-effectiveness analyses on management of veterans with spinal cord injury (SCI) according to this systematic review
| Reference | Comparison groups | Number of cases | Age (years) | Perspective | Original costs | Current costs | Effectiveness | Results |
|---|---|---|---|---|---|---|---|---|
| 35 | Spinal Cord Injury Vocational Integration Program | 81 | 48.7±9.8 | Societal perspective | $26,611 USD (2009) | $32,852 USD (2016) | 0.60±0.09 QALYs | ICER: $575,500 USD (2009) per QALY ICER: $710,478USD (2016) per QALY |
| Usual care for the acquisition of competitive employment in veterans with SCI. | 76 | 49.8±9.8 | Societal perspective | $32,366 USD (2009) | $39,957 USD (2016) | 0.61±0.08 QALYs | The intervention was more effective for veterans with SCI to achieve competitive employment, but the intervention was not cost-effective after 1 year of follow-up when compared to the usual strategy. |
ICER: incremental cost-effectiveness ratio; QALY: quality adjusted life years
Using a model built with data from 20,000 spinal cord injured veterans, Smith et al. compared standard of care versus telehealth care for prevention and treatment of pressure ulcers using low-cost technology, medium-cost technology, and high-cost technology.33 The authors found that the strategy using telehealth care was less expensive than standard care when patients and facilities used low-cost technology (e.g. digital cameras and e-mail).33 Furthermore, Smith et al. reported that telehealth care using low-cost and medium-cost technology might reduce the costs of prevention and treatment of pressure ulcers in spinal cord injured individuals.33
Sinnott et al. carried out a cost-effectiveness analysis comparing supported employment intervention (i.e. Spinal Cord Injury Vocational Integration Program) with the usual strategy for the acquisition of competitive employment in a group of veterans with SCI.35 The intervention was more effective for veterans with SCI to achieve competitive employment within a time period of 1 year, but the intervention was not considered cost-effective (incremental cost-effectiveness ratio of $575,500 USD [2009] per QALY) when compared with the usual strategies (Table 3).
Discussion
The results of this review suggest the estimated average annual costs of caring for veterans with SCI/D varied from $30,770 to $62,563 in 2016 USD in prior published studies. The costs of caring for veterans with SCI/D always exceeded the costs of managing veterans with other more common chronic diseases. The proportion of inpatient care costs over the total health care costs (range: 50.6% to 80.4%) was greater than the proportion of the outpatient care costs (range: 13% to 43.5%), and the proportion of outpatient pharmacy costs (range: 2.1% to 10.3%). The most relevant determinants of higher health care costs among veterans with SCI/D were the presence of pressure ulcer, cervical level of injury, and more severe SCI. Among the few intervention-based studies, the only potentially cost-saving intervention was the usage of telehealth care associated with low-cost and medium-cost technology in the prevention and treatment of pressure ulcers following SCI. Finally, there is a paucity of cost-effectiveness analyses focused on the management of veterans with SCI/D.
Costs of caring for veterans with SCI/D
The studies included in this review solely included costing information from the VA health care administrative databases in the United States that were collected from the fiscal years 1998 to 2010. According to those prior studies, the average annual costs of caring for veterans with SCI/D were estimated to be between $30,770 and $62,563 in 2016 USD.24,25,27,31 Furthermore, the costs of caring for veterans with SCI/D exceeded the costs of management of other chronic diseases in all published comparative studies.24,25,34 Using data from general population in the United States, DeVivo et al. reported that the mean charges for individuals during the first year after SCI were $523,089 in 2009 USD (or $606,349 in 2016 USD), and the mean annual charges of caring for individuals with SCI were estimated at $79,759 in 2009 USD (or $92,454 in 2016 USD).36 Of note, those authors combined clinical and costing data from the National SCI Statistical Center that include people treated at federally designated SCI Model Care systems.36 Using data from the publicly funded health care database in Canada, Munce et al. reported the average total direct health care costs from the time of initial hospitalization to 1 year after initial acute discharge were $109,017 in 2005 CAD (or $122,298 in 2016 USD, using an exchange rate of 1.28 for 2005 CAD/USD from Bank of Canada) among individuals with traumatic SCI.37 Of note, the total direct health care costs in the study by Munce et al. incorporated the costs of acute inpatient care, emergency department, inpatient rehabilitation, complex continuing care, home care services, and physician visits in the year after index hospitalization.
The observed discrepancies between the group of veterans and the general population with regards to their costs for management of SCI/D could be, at least partially, attributed to key methodological differences and shortcomings as follow: (i) most of the data from VA Health Care System represent actual costs, whereas the data from the general population in the study by DeVivo et al. are expectedly higher because they are charges instead of costs; (ii) data from veterans might have missed indirect costs such as out-of-pocket costs due to constraints in service access; (iii) an increased occurrence of SCI among veterans during the Afghanistan war (starting in October 2001) and the Iraq war (starting in March 2003), which would have a greater impact on health-utilization and costs in the costing data from VA Health Care Systems included in fiscal years 1998 to 2010; whereas, data from general population includes the first-year charges of all new cases of SCI with estimated incidence rates from 23.9 to 77 cases per million per year 38; and, (iv) the epidemiological profile of the veterans with war-related SCI is distinct from the spinal cord injured civilians. In a systematic review on the epidemiology of SCIs among military personnel, war-related SCIs were more common among young, white men in the military service who typically sustained thoracic, severe (complete or AIS A) SCIs secondary to gunshot or explosion.12 Unlike SCI in civilians, war-related SCI is commonly associated with other bodily injuries including head and neck injuries, traumatic brain injury, injuries to the chest, abdomen or pelvis, and limb injuries, alone or in combination. Other potential reasons for the discrepancies in the costs of caring for veterans and civilians with SCI could include differences in terms of the healthcare coverage and access, and healthcare system efficiency.
Therefore, care for veterans with SCI/D is essential but unarguably costly and more expensive than several other common chronic diseases. There are substantial economic differences in the management of veterans with SCI/D and spinal cord injured individuals in the general population that need to be considered when making decisions regarding provision of health care services for veterans.
Components and determinants of the health care costs of the veterans with SCI/D
This literature review revealed that a greater proportion of inpatient care costs (range: 50.6% and 80.4%) from the overall total health care costs was observed when compared to the proportion of the outpatient care costs (range: 13% to 43.5%), and the proportion of outpatient pharmacy costs (range: 2.1% to 10.3%).25,27,30,31 Similarly, the estimated proportion of inpatient SCI care charges after first-year was 80.2%, followed by the proportion of outpatient SCI care charges (15%) and outpatient pharmacy charges (4.8%) in a study using data from the general population in the United States.36
According to this review, many publications were focused on potential determinants of the health care costs among veterans with SCI/D, including admission to a long-term care facility, treatment of pressure ulcers, level and severity of spinal cord impairment, and nature of the SCI/D (traumatic versus non-traumatic SCI/D). 24,27–30 The economic impact of pressure ulcers is a well-recognized worldwide issue in the general population with or without SCI.39–41 For instance, Brem et al. found that the mean inpatient care cost associated with stage IV pressure ulcers and their complications was $129,248 USD for hospital-acquired ulcers, and $124,327 USD for community-acquired ulcers (data prior to 2010).39 According to the US statistics on the hospitalizations for pressure ulcers from the Healthcare Cost and Utilization Project databases, the top 3 most frequent associated conditions were anemia (31.2%), urinary tract infections (30.5%), and paralysis (29.2%).42 When stratifying the data analysis by age groups, paralysis and SCI were more noticeable among younger patients, while fluid and electrolyte disorders, nutritional disorders, diabetes without complications, and dementia were more often seen among patients aged 65 years or older.42 The level and severity of SCI are commonly reported as determinants of health care costs among veterans with SCI/D as well as among civilians with SCI/D, particularly in the end-of-life care.27–29 Using data from the general population, prior studies reported a costing gradient from the lowest annual health care costs among individuals with incomplete paraplegia to the highest costs among individuals with complete tetraplegia. 27,36,43 The end-of-life care is a well-recognized major expenditure in the Medicare program in the United States.44 The estimated costs of hospital admissions ending in death were $17.6 billion in 2007 USD (or $23.3 billion in 2016 USD) accounting for 5.1% of total inpatient hospital costs.44 The average costs of the hospitalizations ending in death in the United States were estimated to be $23,017 in 2007 USD (or $30,410 in 2016 USD), which was 2.7 times greater than for inpatients discharged alive.44 While both prior studies from our literature review concluded that the annual health care costs of the veterans with traumatic SCI were similar to the annual costs of caring for veterans with non-traumatic SCI/D, there is apparently no previous report using costing data from the general population on the annual health care costs comparing traumatic SCI to non-traumatic SCI/D.29,31
In summary, the most prominent component of the costs of caring for veterans with SCI/D is the inpatient care cost, followed by outpatient care expenses and outpatient pharmacy spending. While the cervical level, complete injury, time period (i.e. first year after injury and last end-of-life year), and presence of pressure ulcers are well recognized determinants of higher health care costs of veterans with SCI/D, prior studies reported no important economic impact of other potential factors such as the nature of the SCI/D (i.e. traumatic SCI versus nontraumatic SCI/D) and old age (e.g. elderly veterans aged 65 to 79 years with SCI/D versus older veterans).
Intervention-based studies and health care costs of caring for veterans with SCI/D
This literature search identified three intervention-based studies with potential cost-saving benefits in the care of veterans with SCI/D32,33,35 While Young-Hughes and Simbartl found no significant differences between traditional wound care and specialty wound care provided using teleconsultation among veterans with SCI/D with regards to their median inpatient care costs, Smith et al. reported that telehealth care was less expensive than the standard care when patients and facilities used low-cost technology (e.g. digital cameras and e-mail) in the prevention and treatment of pressure ulcers among veterans with SCI after adjusting the models for outcomes.32,33 In a prior systematic review on publications focused on the use of telerehabilitation modalities, Kairy et al. identified 3 out of 28 previous studies that were exclusively focused on telehealth tools in the rehabilitation of pressure ulcers (n=2) or depression (n=1) among spinal cord injured individuals in the general population.45 Despite to common methodological shortcomings and lack of costing data, the authors reported that two articles revealed negative results when comparing standard of care to telerehabilitation, whereas one study suggested decreased hospitalizations with the utilization of a telerehabilitation tool.45 Overall, Kairy et al. concluded that the interest in telerehabilitation has been growing among patients and healthcare professionals, likely due to decreased patient travel burden, even though there is insufficient evidence in favor of telerehabilitation as a cost-saving or cost-effective solution.45
Moreover, this literature search captured only one cost-effectiveness analysis that compared supported employment intervention to the usual strategy for the acquisition of competitive employment in veterans with SCI.35 Sinnott et al. reported that the intervention was not more cost effective than the usual strategy, even though the intervention was more effective for veterans with SCI to achieve competitive employment within a time period of 1 year.35 This is a particularly important issue as an individual’s income over their lifetime has been identified as an important predictor of health and all-cause mortality. In a systematic review on cost effectiveness of acute hospital-based SCI services, Bagnall et al. highlighted the paucity of cost-effectiveness studies in the management of traumatic SCI.46 Similarly, Chan et al. stressed that the literature on comparative studies focused on interventions for patients with SCI is scarce.47 This paucity in comparative economic evaluation is common to the the literature regarding veterans with SCI/D as well as the general traumatic and non-traumatic SCI literature.
While the VA in the United States has generously funded several important economic analyses as above mentioned, there is a clear need for further comparative studies on interventions including cost effectiveness, which could assist administrators, policy makers and healthcare professionals in making better decisions regarding resource allocation based on the anticipated efficacy of an intervention and its cost effectiveness when planning for the optimal care of veterans with SCI/D.
Study limitations
This is an original systematic review that synthesized and appraised the literature on the economic burden of SCI/D among veterans. While the results of this review stress the economic burden of SCI/D and significant knowledge gaps regarding the costs of care for veterans with SCI/D, there are limitations that need to be considered before generalizing the results. Firstly, most the data included in this review were derived from retrospective cohort studies, which are vulnerable to potential bias and methodological limitations. Secondly, all publications identified in this systematic review used data from the VA Health Care Systems in the United States that were collected from the fiscal years 1998 to 2010. This limits the generalizability of the data to other settings and countries that have distinct healthcare policies and services for veterans. Finally, the composition of the costs may vary from publication to publication or site to site (e.g. charges versus costs) and, hence, caution is recommended when comparing costing data across jurisdictions and health systems.
Conclusions
This systematic review, for the first time, synthesized and evaluated data from publications on the economic burden of care for veterans with SCI/D. These results highlight that the health care costs of the management of veterans with SCI/D are substantial and, in general, lower than the costs of caring for civilians with SCI, but greater than the costs of caring for patients with other more common chronic diseases. The discrepancy between civilians and veterans with regards to the costs of caring for spinal cord individuals could be due to differences in terms of methodology, disease epidemiology, healthcare coverage and access, and healthcare system efficiency, among other potential explanations. Similar to data from non-veterans with SCI/D, the greatest expenditures are in the first year after injury and last end-of-life year, and the inpatient care costs are greater than the outpatient care costs and pharmacy costs. Higher total healthcare costs are anticipated among individuals with cervical level injury, complete injury, and pressures sores. Although there is a growing evidence for the economic burden of SCI/D and its determinants among veterans, there is a paucity of comparative studies on interventions including cost-effectiveness analyses essential to resource allocation when advancing quality of care with a fixed resource envelope.25
Disclaimer statements
Contributors None.
Funding This work was supported by Wings for Life [WFL-CA-0916].
Conflict of interest The authors report no conflicts of interest.
Ethics approval None.
Disclosure statement
Dr. Furlan receives salary support from the Wings for Life Spinal Cord Research Foundation.
ORCID
Julio C. Furlan http://orcid.org/0000-0002-2038-0018
Malin Nygren-Bonnier http://orcid.org/0000-0001-8234-6803
References
- 1.Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV.. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci. 2013;40(4):456–64. [DOI] [PubMed] [Google Scholar]
- 2.Mahabaleshwarkar R, Khanna R.. National hospitalization burden associated with spinal cord injuries in the United States. Spinal Cord. 2014;52(2):139–44. [DOI] [PubMed] [Google Scholar]
- 3.CIHI The Burden of Neurological Diseases, Disorders and Injuries in Canada. Ottawa: Canadian Institute for Health Information, 2007. [Google Scholar]
- 4.van den Berg ME, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J.. Incidence of nontraumatic spinal cord injury: a Spanish cohort study (1972–2008). Arch Phys Med Rehabil. 2012;93(2):325–31. [DOI] [PubMed] [Google Scholar]
- 5.New PW, Jackson T.. The costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, Australia. Spine (Phila Pa 1976). 2010;35(7):796–802. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh D, Alvis W.. Efficient utilization of medical practice resources: a framework and case analysis. J Health Care Finance. 2003;30(1):41–8. [PubMed] [Google Scholar]
- 7.Roski RA, Pollock KJ.. The fundamentals of building an effective neurosurgical practice. Clin Neurosurg. 2004;51:43–7. [PubMed] [Google Scholar]
- 8.Honeybul S, Gillett GR, Ho KM, Lind CR.. Neurotrauma and the rule of rescue. J Med Ethics. 2011;37(12):707–10. [DOI] [PubMed] [Google Scholar]
- 9.Crawford NC. US Budgetary Costs of Wars through 2016: $4.79 Trillion and Counting [online]. Accessed December 31, 2016. [Google Scholar]
- 10.US-VA The 2017 Budget and 2018 Advance Appropriations requests for VA. In: Affairs UDoV , ed. Washington, DC: US Department of Veterans Affairs, 2016. [Google Scholar]
- 11.US-VA Fact sheet: VA and spinal cord injury. In: Affairs UDoV , ed. Washington, DC: US Department of Veterans Affairs, 2009: 1–5. [Google Scholar]
- 12.Furlan JC, Gulasingam S, Craven BC.. Epidemiology of war-related spinal cord injury among combatants: A systematic review. Personal Communication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.da Costa BR, Cevallos M, Altman DG, Rutjes AW, Egger M.. Uses and misuses of the STROBE statement: bibliographic study. BMJ Open. 2011;1:e000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Theobald K, Capan M, Herbold M, Schinzel S, Hundt F.. Quality assurance in non-interventional studies. GMS German Med Sci. 2009;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB.. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996;276(15):1253–8. [PubMed] [Google Scholar]
- 17.Siegel JE, Weinstein MC, Russell LB, Gold MR.. Recommendations for reporting cost-effectiveness analyses. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276(16):1339–41. [DOI] [PubMed] [Google Scholar]
- 18.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC.. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276(14):1172–7. [PubMed] [Google Scholar]
- 19.US-VA Health Benefits. In: Affairs UDoV , ed. Washington, DC: US Department of Veterans Affairs, 2016. [Google Scholar]
- 20.Furlan JC, Fehlings MG, Tator CH, Davis AM.. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA Standards. J Neurotrauma. 2008;25(11):1273–301. [DOI] [PubMed] [Google Scholar]
- 21.US-BLS Consumer Price Index - All Urban Consumers (Meidcal Care). Databases, Tables & Calculators by Subject. December 31, 2016 ed: US Bureau of Labor Statistics, 2016. [Google Scholar]
- 22.Halfhill TR. Tom's Inflation Calculator. http://www.halfhill.com/inflation_js.html. Accessed December 31, 2016. [Google Scholar]
- 23.Yu W, Wagner TH, Chen S, Barnett PG.. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003;60(3 Suppl):40S–53S. [DOI] [PubMed] [Google Scholar]
- 24.Yu W, Ravelo A, Wagner TH, Barnett PG.. The relationships among age, chronic conditions, and healthcare costs. Am J Manag Care. 2004;10(12):909–16. [PubMed] [Google Scholar]
- 25.Yu W, Cowper D, Berger M, Kuebeler M, Kubal J, Manheim L.. Using GIS to profile health-care costs of VA Quality-Enhancement Research Initiative diseases. J Med Syst. 2004;28(3):271–85. [DOI] [PubMed] [Google Scholar]
- 26.Hedrick B, Pape TL, Heinemann AW, Ruddell JL, Reis J.. Employment issues and assistive technology use for persons with spinal cord injury. J Rehab Res Dev. 2006;43(2):185–98. [DOI] [PubMed] [Google Scholar]
- 27.French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D.. Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med. 2007;30(5):477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petersen LA, Urech TH, Byrne MM, Pietz K.. Do financial incentives in a globally budgeted healthcare payment system produce changes in the way patients are categorized? A five-year study. Am J Manag Care. 2007;13(9):513–22. [PubMed] [Google Scholar]
- 29.Yu W, Smith B, Kim S, Chow A, Weaver FM.. Major medical conditions and VA healthcare costs near end of life for veterans with spinal cord injuries and disorders. J Rehab Res Dev. 2008;45(6):831–9. [DOI] [PubMed] [Google Scholar]
- 30.Stroupe KT, Manheim L, Evans CT, Guihan M, Ho C, Li K, et al. Cost of Treating Pressure Ulcers for Veterans with Spinal Cord Injury. Top Spinal Cord Inj Rehab. 2011;16(4):62–73. [Google Scholar]
- 31.St. Andre JR, Smith BM, Stroupe KT, Burns SP, Evans CT, Ripley DC, et al. A Comparison of Costs and Health Care Utilization for Veterans with Traumatic and Nontraumatic Spinal Cord Injury. Top Spinal Cord Inj Rehab. 2011;16(4):27–42. [Google Scholar]
- 32.Young-Hughes S, Simbartl LA.. Spinal cord injury/disorder teleconsultation outcome study. Rehab Nursing. 2011;36(4):153–8, 172. [DOI] [PubMed] [Google Scholar]
- 33.Smith MW, Hill ML, Hopkins KL, Kiratli BJ, Cronkite RC.. A modeled analysis of telehealth methods for treating pressure ulcers after spinal cord injury. Int J Telemed Appl. 2012;2012:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoon J, Zulman D, Scott JY, Maciejewski ML.. Costs associated with multimorbidity among VA patients. Med Care. 2014;52(Suppl 3):S31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sinnott PL, Joyce V, Su P, Ottomanelli L, Goetz LL, Wagner TH.. Cost-effectiveness of supported employment for veterans with spinal cord injuries. Arch Phys Med Rehab. 2014;95(7):1254–61. [DOI] [PubMed] [Google Scholar]
- 36.Devivo MJ, Chen Y, Mennemeyer ST, Deutsch Y.. Costs of care following spinal cord injury. Top Spinal Cord Inj Rehab. 2011;16(4):1–9. [Google Scholar]
- 37.Munce SE, Wodchis WP, Guilcher SJ, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51(1):64–9. [DOI] [PubMed] [Google Scholar]
- 38.Furlan JC, Krassioukov A, Miller WC, Trenaman LM.. Epidemiology of Traumatic Spinal cord Injury. In: Eng JJ, Teasell RW, Miller WC, et al., eds. Spinal Cord Injury Rehabilitation Evidence. Version 5.0 ed. Vancouver 2014: 1–121. [Google Scholar]
- 39.Brem H, Maggi J, Nierman D, Rolnitzky L, Bell D, Rennert R, et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200(4):473–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zakrasek EC, Creasey G, Crew JD.. Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord. 2015;53(1):7–13. [DOI] [PubMed] [Google Scholar]
- 41.Chan BC, Nanwa N, Mittmann N, Bryant D, Coyte PC, Houghton PE.. The average cost of pressure ulcer management in a community dwelling spinal cord injury population. Int Wound J. 2013;10(4):431–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Russo CA, Steiner C, Spector W.. Hospitalizations Related to Pressure Sores, 2006. HCUP Statistical Brief 2008;2017:1–9 (http://www.hcup-us.ahrq.gov/reports/statbriefs/sb64.pdf). [Google Scholar]
- 43.Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS.. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33(3):113–22. [PubMed] [Google Scholar]
- 44.Zhao Y, Encinosa W.. The Cost of End-of-Life Hospitalizations, 2007. HCUP Statistical Brief 2009. (http://www.hcup-us.ahrq.gov/reports/statbriefs/sb81.pdf). [PubMed] [Google Scholar]
- 45.Kairy D, Lehoux P, Vincent C, Visintin M.. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disab Rehab. 2009;31(6):427–47. [DOI] [PubMed] [Google Scholar]
- 46.Bagnall AM, Jones L, Richardson G, Duffy S, Riemsma R.. Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review. Health Tech Assess. 2003;7(19):iii, 1–92. [DOI] [PubMed] [Google Scholar]
- 47.Chan B, McIntyre A, Mittmann N, Teasell RW, Wolfe DL.. Economic evaluation of spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JT, et al., eds. Spinal Cord Injury Rehabilitation Evidence. Version 5.0 ed. Vancouver, BC: SCIRE, 2014:1–21. [Google Scholar]


