Abstract
Background
Observational studies suggest a survival advantage with bilateral single internal thoracic artery (BITA) versus single internal thoracic artery grafting for coronary surgery, whereas this conclusion is not supported by randomized trials. We hypothesized that this inconsistency is attributed to unmeasured confounders intrinsic to observational studies. To test our hypothesis, we performed a meta‐analysis of the observational literature comparing BITA and single internal thoracic artery, deriving incident rate ratio for mortality at end of follow‐up and at 1 year. We postulated that BITA would not affect 1‐year survival based on the natural history of coronary artery bypass occlusion, so that a difference between groups at 1 year could not be attributed to the intervention.
Methods and Results
We searched MEDLINE and Pubmed to identify all observational studies comparing the outcome of BITA versus single internal thoracic artery. One‐year and long‐term mortality for BITA and single internal thoracic artery were compared in the propensity‐score–matched (PSM) series, that is, the form of observational evidence less prone to confounders. Thirty‐eight observational studies (174 205 total patients) were selected for final comparison. In the 12 propensity‐score–matched series (34 019 patients), the mortality reduction for BITA was similar at 1 year and at the end of follow‐up (incident rate ratio, 0.70; 95% confidence interval, 0.60–0.82 versus 0.77; 95% confidence interval, 0.70–0.85; P for subgroup difference=0.43).
Conclusions
Unmeasured confounders, rather than biological superiority, may explain the survival advantage of BITA in observational series.
Keywords: bypass graft, myocardial revascularization, surgery
Subject Categories: Cardiovascular Surgery
Clinical Perspective
What Is New?
Our findings suggest that factors not related to the conduit patency, such as the patients’ general status or quality of the target vessels, play a role in determining the outcome of observational studies and that a selection bias is present even in propensity‐score–matched analyses.
What Are the Clinical Implications?
Our findings elicit concerns regarding the ability of the propensity‐matching process to overcome selection bias and assure comparability between groups.
The long‐term clinical outcomes data from the ART (Arterial Revascularization Trial) trial and new randomized studies are needed to clarify the effect of bilateral internal thoracic artery grafting in patients undergoing coronary bypass surgery.
A clear contradiction between observational and randomized studies exists in the literature on the effect of multiple internal thoracic artery grafts in patients undergoing coronary artery bypass surgery.
In the 1980s, it was recognized that in coronary artery bypass surgery patients long‐term survival was enhanced when the left anterior descending (LAD) was grafted with a left internal thoracic artery, rather than a saphenous vein graft (SVG).1 By extension, the use of bilateral internal thoracic arteries (BITAs) should further increase postoperative survival, compared with the use of a single internal thoracic artery (SITA).2 This difference is generally attributed to greater and more‐durable patency of the internal thoracic artery compared with the SVG, as well as increased late SVG atherosclerosis.3
In the past 25 years, a very large amount of observational data, including 6 meta‐analyses,4, 5, 6, 7, 8, 9 have supported this concept. On this basis, the use of BITA is a class IIA recommendation in patients with a long anticipated life expectancy by current guidelines and professional society position papers.10, 11, 12
The randomized studies, however, reported different results. To date, there have been 4 randomized controlled trials (RCTs) comparing BITA and SITA.13, 14, 15, 16 In these studies, survival has been similar following BITA and SITA grafting. In the largest of the RCTs, the ART (Arterial Revascularization Trial), mortality was 8.7% after BITA grafting and 8.4% following SITA at 5 years.16
There are several possible explanations for the discrepant findings between observational and RCT evidence. The RCTs may not have sufficient sample size or follow‐up to detect a mortality difference compared with observational series. In the ART trial, a relatively higher proportion of crossovers in the patients randomized to BITA, as well as the allowed use of a radial artery in the SITA group, may have diluted the treatment effect.
The other possible explanation, however, is that the benefit observed in the observational studies for BITA grafting is largely related to unmeasured confounders.
The objective of this study is to perform a meta‐analysis of the observational literature comparing survival following BITA and SITA grafting. To evaluate whether unmeasured confounders rather than biological superiority explained the BITA effect, we chose to compare both 1‐year as well as late survival in the BITA and SITA cohorts. We postulated that BITA would not affect 1‐year survival based on the natural history of SVG occlusion. The latter analysis was restricted to propensity‐score–matched studies, because PSM is considered the best method to minimize confounding in observational series.
Methods
The data, analytical methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Search Strategy and Study Selection
This systematic review was conducted in accord to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines.17
Pubmed and OVID's version of MEDLINE was searched from January 1972 to August 2017 for publications comparing BITA versus SITA grafting on all‐cause mortality. The following keywords were combined with the Boolean operator “or”: “bilateral internal mammary,” “bilateral internal thoracic,” “total arterial revascularization,” and “multiple arterial revascularization.” The full search strategy can be found in Data S1. All citations were screened for study inclusion independently by 2 investigators (A.D.F. and M.G.). Any disagreements were discussed and resolved by consensus. In addition, the bibliography of all studies and meta‐analyses was searched to identify further publications.
Inclusion criteria for analysis were:
Observational study (unadjusted and adjusted studies were eligible).
Sample size of at least 100 patients in each group.
Follow‐up duration longer than 30 days.
Written in English language.
We excluded studies that were: RCTs, not performed in humans, review articles, case reports, editorials, and expert opinions. To ensure that the analysis was strictly limited to a comparison of BITA versus SITA, we excluded studies where an additional arterial graft was used in 1 of the 2 groups and it was not possible to abstract the exact information for the isolated BITA and SITA series. In case of overlapping between studies or multiple publications from the same center, only the publication with the largest sample size was considered.
The quality of included studies was assessed using the Newcastle–Ottawa Scale for observational studies by 2 investigators independently (A.D.F. and M.G.).18 The highest possible score is 9 stars; <6 stars was considered low quality whereas ≥6 stars was considered high quality.
Data Abstraction
Two investigators (A.D.F. and M.G.) independently abstracted the following: study demographics (study period, country, and centers involved, sample size), study design methods, completeness of follow‐up, and follow‐up duration. In addition, the following patient characteristics in the unmatched and matched groups were also obtained: age, female sex, diabetes mellitus, left ventricular ejection fraction, and chronic obstructive pulmonary disease. Continuous variables were expressed as median (25th, 75th percentile) or as mean±SD. Categorical variables are reported as frequency (%).
For all‐cause mortality, crude event rates, unadjusted and adjusted hazard ratios (HRs) for BITA versus SITA grafting, and their respective 95% confidence intervals (CIs) and log P‐rank values were abstracted.
Outcome Analyses
The primary outcome was all‐cause mortality. Long‐term all‐cause mortality for BITA and SITA patients was compared in all the studies.
Subgroup analyses for the primary outcome were performed as follows:
Studies in the general population versus studies in specific subgroups of patients (ie, diabetics, elderly patients as defined by the individual studies, patients with renal failure, urgent/emergent cases, and patients with low ejection fraction).
Unadjusted versus adjusted studies (including regression‐adjusted and PSM) in the general population.
Regression‐adjusted versus PSM studies in the general population.
To assess for possible treatment allocation bias in the observational studies, we chose to compare 1‐year mortality between matched treatment groups. The 1‐year interval was chosen because the patency rate of SVGs at 1 year remains high and a survival difference related to difference in patency between arterial and venous conduits is unlikely.19 PSM is a robust method used to balance against confounding by indication in observational studies20; for this reason, we compared all‐cause mortality for BITA and SITA at 1 year in the PSM studies only.
Analytical Plan
Long‐term all‐cause mortality between BITA and SITA patients was compared in all studies initially. Comparisons were then performed in the general population studies after exclusion of studies restricted to specific patient subgroups (diabetes mellitus, elderly as defined in the individual studies, renal failure, urgent/emergent, and reduced left ventricular ejection fraction) and in the individual specific patient subgroups. Next, separate comparisons were made between BITA and SITA in the unadjusted and adjusted series (covariate adjusted and PSM combined). Last, comparisons were performed in the covariate adjusted and PSM series separately.
One‐year mortality between BITA and SITA patients was compared in PSM studies only.
Statistical Analysis
The generic inverse variance method21 was used to pool the natural logarithm of the incident rate ratio (IRR) across studies to account for potentially different follow‐up durations between the groups. We estimated the IRR through several means depending on the available study data. When HRs were provided, we took the natural logarithm of the HR; the SE was derived from the 95% CI or log rank P value.22 When Kaplan–Meier curves were present, we estimated the number of events from the curves to calculate the IRR, as previously described.23 The SE was estimated from the number of events in each arm.22 When event rates were not readily available, they were extracted from Kaplan–Meier curves using GetData Graph Digitizer software (version 2.26; http://getdata-graph-digitizer.com/) according to a previously described method.24
A random‐effects model was used for statistical survival pooling, computing risk estimates with 95% CIs. Funnel plots were used to assess publication bias by graphical inspection.25 Hypothesis testing for equivalence was set at the 2‐tailed 0.01 level. Hypothesis testing for statistical heterogeneity was set at the 2‐tailed 0.10 level and was based on the Cochran Q test, with I2 values of 0% to 25%, 26% to 50%, and 51% to 100% representing low, moderate, and high heterogeneity, respectively.26
Metaregression analysis examining the following variables—age, sex, diabetes mellitus, and left ventricular ejection fraction—was performed. In addition, a “leave‐one‐out” analysis and a cumulative meta‐analysis were performed in all studies ordered by year of publication.
All analyses were performed using CMA software (version 3; Biostat, Englewood, NJ).
Results
Selected Studies
From 2921 titles, 149 pertinent studies were included for full‐text review. We excluded 111 studies that did not meet inclusion criteria. Further details of the study flow are shown in Figure S1. A total of 38 observational studies were selected for the quantitative analysis. Eight nonadjusted, 9 covariate‐adjusted, and 21 PSM studies were included (see Table 1).27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64 Twenty‐eight studies (162 989 patients) were performed in the general population, whereas 10 (11 216 patients) were performed in specific subgroups of patients (diabetics: 3 studies [1533 patients]; elderly: 4 studies [6033 patients]; renal failure patients: 1 study [1203 patients]; urgent/emergent cases: 1 study [652 patients]; and patients with low ejection fraction: 1 study [1795 patients]). An overview of the studies is summarized in Tables 1 and 2, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64 (variables included for PSM are summarized in Table S1).
Table 1.
Characteristics of the Studies Included in the Primary Analysis
| Study | Year | Center | Study Period | Setting | Type of Study | Adjustment Performed |
|---|---|---|---|---|---|---|
| Ashraf27 | 1994 | Manchester Royal Infirmary, Manchester, UK | 1989–1992 | Isolated primary CABG | Retrospective | NS |
| Benedetto28 | 2014 | Harefield Hospital, London, UK | 2001–2013 | Isolated primary CABG | Retrospective | PSM |
| Berreklouw29 | 2001 | Catharina Hospital, Eindhoven, The Netherlands | 1985–1990 | Isolated primary CABG | Retrospective | MCPHR |
| Bonacchi30 | 2006 | University of Florence, Italy | 1997–2003 | Non‐elective CABG in unstable angina patients | Retrospective | MCPHR |
| Buxton31 | 1998 | Austin and Repatriation Medical Center, University of Melbourne, Victoria, Australia | 1985–1995 | Isolated primary CABG | Retrospective | MCPHR |
| Calafiore32 | 2004 | University Hospital, Torino, Italy and “G D'Annunzio” University, Chieti, Italy | 1986–1999 | Isolated primary CABG in patients <75 years old | Retrospective | PSM |
| Carrier33 | 2009 | Montreal Heart Institute, Montreal, Quebec, Canada | 1995–2007 | Isolated primary CABG | Retrospective | MCPHR |
| Dalén34 | 2014 | Nationwide population‐based cohort study (Sweden) | 1997–2008 | Isolated primary CABG | Retrospective | PSM |
| Danzer35 | 2001 | University Hospital, Geneva, Switzerland | 1983–1989 | Isolated primary CABG | Retrospective | NA |
| Dewar36 | 1995 | Vancouver Hospital and Health Sciences Centre, University of British Columbia, Vancouver, Canada | 1984–1992 | Isolated primary CABG | Retrospective | Univariate regression |
| Endo37 | 2001 | Tokyo Women's Medical University, Tokyo, Japan | 1985–1998 | Isolated primary CABG | Retrospective | MCPHR |
| Gansera 200438 | 2004 | Klinikum Bogenhausen, Munich, Germany | 1997–1999 | Isolated primary CABG | Retrospective | NA |
| Gansera 201739 | 2017 | Klinikum Bogenhausen, Munich, Germany | 2000–2011 | Isolated CABG in diabetic patients, <65 years old | Retrospective | PSM |
| Grau40 | 2015 | The Valley Columbia Heart Center, Columbia University College of Physicians and Surgeons, Ridgewood, NJ, USA | 1994–2013 | Isolated CABG | Retrospective | PSM |
| Hirotani41 | 2003 | Tokyo Saiseikai Central Hospital, Minato‐Ku, Tokyo, Japan | 1991–2003 | Isolated primary CABG in diabetic patients | Retrospective | NA |
| Itoh42 | 2016 | Saitama Medical Center, Jichi Medical University, Saitama, Japan | 1990–2014 | Isolated CABG in patients ≥75 years old | Retrospective | PSM |
| Johnson43 | 1989 | Milwaukee Heart Surgery Associates, S.C., and St. Mary's Hospital, Milwaukee, WI, USA | 1972–1986 | Isolated CABG | Retrospective | NA (patients matched with the general US population) |
| Jones44 | 2000 | Baylor College of Medicine and Veterans Affairs Medical center, Houston, TX, USA | 1986–1996 | Isolated primary CABG in patients >65 years old | Retrospective | NA |
| Joo45 | 2012 | Yonsei Cardiovascular Hospital, Seoul, Republic of Korea | 2000–2009 | Isolated OPCAB | Retrospective | PSM |
| Kelly46 | 2012 | Queen Elizabeth II Health Sciences Center, Halifax, Nova Scotia, Canada | 1995–2007 | Isolated primary CABG | Retrospective | Non‐parsimonious MCPHR including PS quintiles |
| Kieser47 | 2011 | The Province of Alberta, Canada | 1995–2008 | Isolated primary CABG | Retrospective | MCPHR |
| Kinoshita48 | 2015 | Shiga University of Medical Science, Otsu, Japan | 2002–2014 | Isolated CABG‐patients stratified by GFR | Retrospective | PSM |
| Kurlansky49 | 2010 | Florida Heart Research Institute, Miami, FL, USA | 1972–1994 | Isolated CABG | Retrospective | PSM |
| Locker50 | 2012 | Mayo Clinic, Rochester, MN, USA | 1993–2009 | Isolated primary CABG | Retrospective | PSM and MCPHR |
| Lytle51 | 2004 | The Cleveland Clinic Foundation, Cleveland, OH, USA | 1971–1989 | Isolated primary CABG | Retrospective | PSM |
| Medalion52 | 2015 | Tel Aviv Sourasky Medical Center, Tel Aviv, Israel | 1996–2008 | isolated CABG in patients ≥70 years old | Retrospective | PSM |
| Mohammadi53 | 2014 | Quebec Heart and Lung Institute, Quebec City, Canada | 1991–2011 | Isolated primary CABG in patients with EF ≤40% | Retrospective | PSM |
| Nasso54 | 2012 | Multicenter | 2003–2008 | Isolated primary CABG | Retrospective | PSM |
| Naunheim55 | 1992 | St. Louis University Medical Center, St. Louis, MS, USA | 1972–1975 | Isolated CABG | Retrospective | NA |
| Navia56 | 2016 | Instituto Cardiovascular de Buenos Aires, Buenos Aires, Argentina | 1996–2014 | Isolated CABG | Retrospective | PSM |
| Parsa57 | 2013 | Duke University Medical Center, Durham, NC, USA | 1984–2009 | Isolated CABG | Prospective | MCPHR |
| Pettinari58 | 2015 | Ziekenhuis Oost Limburg, Genk, Belgium and University Hospitals Leuven, Leuven, Belgium | 1972–2006 | Isolated CABG in patients ≥70 years old | Retrospective | PSM |
| Pick59 | 1997 | Mayo Clinic, Rochester, MN, USA | 1983–1986 | Isolated CABG | Retrospective | MCPHR |
| Rosenblum60 | 2016 | Emory University School of Medicine, Atlanta, GA, USA | 2003–2013 | Isolated primary CABG | Retrospective | PSM |
| Schwann61 | 2016 | Multicenter | 1987–2011 | Isolated CABG | Retrospective | PSM |
| Stevens62 | 2004 | Montreal Heart Institute, Montreal, Quebec, Canada | 1985–1995 | Isolated primary CABG | Retrospective | MCPHR including PS |
| Tarelli63 | 2001 | Varese Hospital, Varese, Italy | 1988–1990 | Isolated CABG | Retrospective | NA |
| Toumpoulis64 | 2006 | St. Luke's–Roosevelt Hospital Center at Columbia University, NY, USA | 1992–2002 | Isolated CABG in diabetic patients | Retrospective | MCPHR in PS‐matched patients |
CABG indicates coronary artery bypass grafting; MCPHR, multivariable Cox proportional hazards regression; NA, not applicable; NR, not reported; NS, not specified; OPCAB, off‐pump coronary artery bypass; PS, propensity score; PSM, propensity‐score matching.
Table 2.
Overview of the Studies Included in the Primary Analysis
| Study | Overall Population, n | UNM BITA, n | UNM SITA, n | PSM BITA, n | PSM SITA, n | Mean/Median Follow‐up (Y) | Completeness of Follow‐up |
|---|---|---|---|---|---|---|---|
| Ashraf27 | 300 | 150 | 150 | NA | NA |
Median (IQR) BITA: 1.9 (1.3–2.6) Median (IQR) SITA: 2.3 (1.7–3) |
NR |
| Benedetto28 | 4195 | 750 | 3445 | 750 | 750 | 4.8±3.2 (PSM sample) | 100% |
| Berreklouw29 | 482 | NA | NA | 249 | 233 |
BITA: 9.7±2.7 SITA: 10.1±2.4 |
94% |
| Bonacchi30 | 652 | NA | NA | 320 | 332 | 5.6±1.4 | 99.7% |
| Buxton31 | 2853 | 1296 | 1557 | NA | NA | 4.3 | 95.9% |
| Calafiore32 | 1602 | 1026 | 576 | 570 | 570 |
Overall: 7.3±4.8 BITA: 7.1±5.0 SITA: 7.5±4.7 |
100% |
| Carrier33 | 6655 |
Statin+: 1166 Statin−: 69 |
Statin+: 4835 Statin−: 585 |
NA | NA | 10 | 99% |
| Dalén34 | 49 702 | 559 | 49 143 | 558 | 558 | 7.5 | 100% |
| Danzer35 | 521 | 382 | 139 | NA | NA | 10 | 97.5% |
| Dewar36 | 1142 | 377 | 765 | NA | NA | 4 | NR |
| Endo37 | 1131 | 443 | 688 | NA | NA | 6.2 | 99.3% |
| Gansera 200438 | 1378 | 716 | 662 | NA | NA | 5.3 | NR |
| Gansera 201739 | 250 | NA | NA | 125 | 125 | 9.3±3.5 | 100% |
| Grau40 | 6666 | 1544 | 5122 | 1006 | 1006 |
Overall: 10.5±5 BITA: 10.9±5 SITA: 10.1±5 |
100% |
| Hirotani41 | 303 | 179 | 124 | NA | NA | NR | 95% |
| Itoh42 | 400 | 107 | 293 | 98 | 196 | 9.0±5.8 | 95.6% |
| Johnson43 | 2014 | 576 | 1438 | NA | NA | NR | 100% |
| Jones44 | 510 | 172 | 338 | NA | NA | 5.0±3.1 | 100% |
| Joo45 | 1749 | 392 | 1357 | 366 | 366 |
Overall: 7.0±2.0 BITA: 6.9±2.1 SITA: 7.1±2.7 |
98.1% |
| Kelly46 | 7633 | 1079 | 6554 | NA | NA |
BITA: 5.4 SITA: 4.6 |
NR |
| Kieser47 | 5067 | 1038 | 4029 | NA | NA |
Overall: 7 BITA: 6.4±3.2 SITA: 7.1±3.4 |
NR |
| Kinoshita48 | 1203 | 750 | 453 | 412 | 412 |
PSM BITA: 5.6±3.3 PSM SITA: 4.9±3.2 |
99% |
| Kurlansky49 | 4584 | 2215 | 2369 | Quintiles | Quintiles |
Overall: 11.5 BITA: 12.7 SITA: 11.1 |
BITA=96.7% SITA=98.3% |
| Locker50 | 8295 |
BITA only: 271 BITA/SVG: 589 |
7435 | NR | NR | 7.6±4.6 | 100% |
| Lytle51 | 10 124 | 2001 | 8123 | 1152 | 1152 |
BITA: 16.2±2.4 SITA: 16.3±2.5 |
100% |
| Medalion52 | 1627 | 1045 | 582 | NA | NA | 8.2±4.5 | 98% |
| Mohammadi53 | 1795 | 129 | 1666 | 111 | 111 |
Overall PSM: 8.0±5.3 PSM BITA: 8.6±5.1 PSM SITA: 7.7±5.5 |
92.7% |
| Nasso54 | 8054 | 4088 | 3966 | 3584 | 3584 | 3.1 | 98% |
| Naunheim55 | 365 | 100 | 265 | 100 | 100 | NR | 96.5% |
| Navia56 | 2486 | 2098 | 388 | 485 | NR | Median: 5.5 (IQR: 2.6–8.8) | 95% |
| Parsa57 | 17 609 | 728 | 16 881 | NA | NA | NR | 100% |
| Pettinari58 | 3496 | 1328 | 2168 | 892 | 892 | 3.1 | 100% |
| Pick59 | 321 | NA | NA | 160 | 161 | 9.8±2.8 | 100% |
| Rosenblum60 | 8254 | 873 | 7381 | 306 | 306 | Median: 2.8 (IQR: 1.1–4.9) | 100% |
| Schwann61 | 5125 | 641 | 4484 | 551 | 551 | NR | 100% |
| Stevens62 | 4382 | 1835 | 2547 | NA | NA |
Overall: 11±3 BITA: 8±2 SITA: 12±3 |
98% |
| Tarelli63 | 300 | 150 | 150 | NA | NA |
Overall: 9.2 BITA: 9.2±2.8 SITA: 9.1±2.5 |
100% |
| Toumpoulis64 | 980 | NA | NA | 490 | 490 | 4.7±3.0 | 99.1% |
BITA indicates bilateral internal thoracic arteries; IQR, interquartile range; NA, not applicable; NR, not reported; PSM, propensity‐score matched; SITA, single internal thoracic artery; SVG, saphenous vein graft.
The selected studies reported on 174 205 patients (BITA: 32 206; SITA: 141 999) for final comparisons.
Overall, the BITA and SITA groups presented different preoperative risk‐factor distribution (mean age, BITA versus SITA: 60 versus 64.1 years; female sex, BITA versus SITA: 16% versus 20.8%; diabetes mellitus, BITA versus SITA: 32.2% versus 40.5%; chronic obstructive pulmonary disease, BITA versus SITA: 9.6% versus 11.8%; Table S2).
Long‐Term All‐Cause Mortality
Mean follow‐up time across the 38 studies was 7.25 years (range, 2.1–16.3). The overall mortality rate at the end of follow‐up was 28.03±18.4% in the BITA versus 39.96±23.5% in the SITA series.
Use of BITA was associated with a statistically significant reduction of mortality at the end of follow‐up when compared with SITA (IRR, 0.74; 95% CI, 0.69–0.80; P<0.001; I2=71%; Figure 1A27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64 and Figure S2). This finding was consistent across the general population and all the specific patient subgroups and all the study designs (Figures S3 through S5) and was not influenced by age, sex, diabetes mellitus, and ejection fraction (Figure 2).
Figure 1.
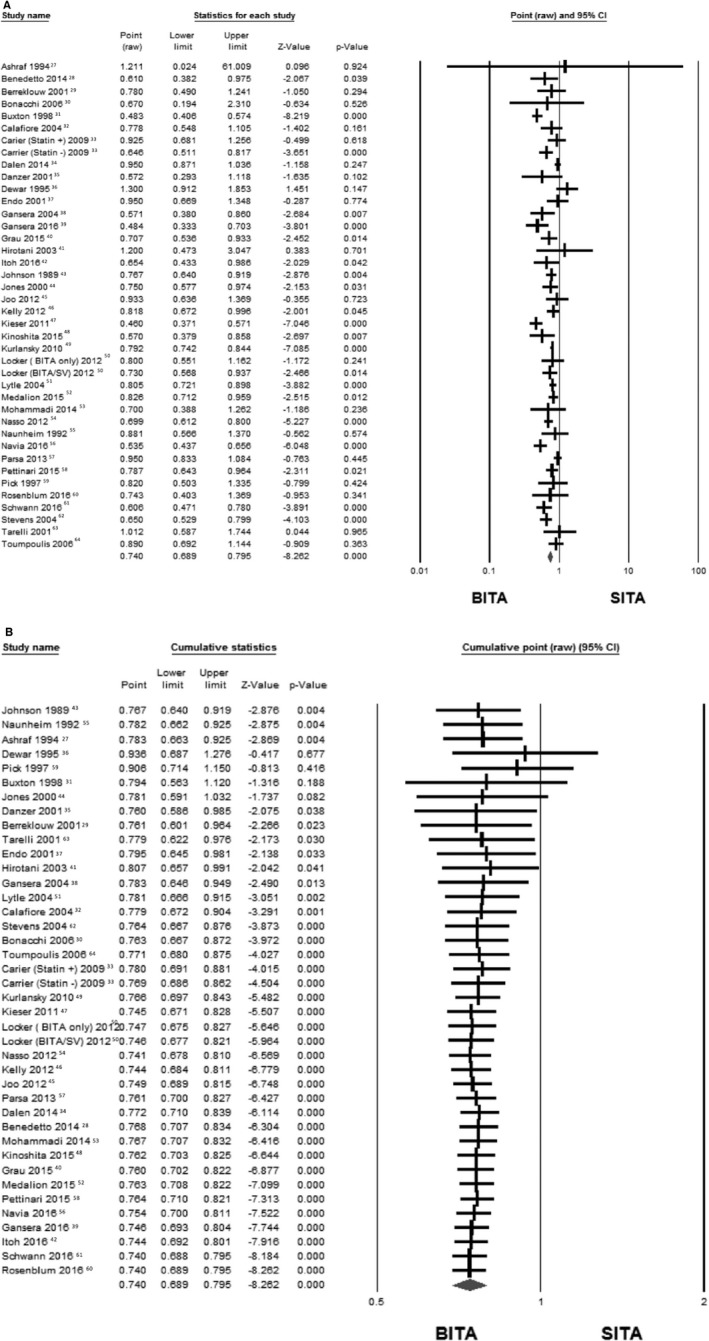
A, Forest plot comparing the effect of the use of BITA vs SITA on end of follow‐up mortality across all the included studies (38 studies; 174 205 patients). B, Cumulative analysis of all the included studies using random‐effect model (38 studies; 174 205 patients). BITA indicates bilateral internal thoracic artery; CI, confidence interval; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure 2.
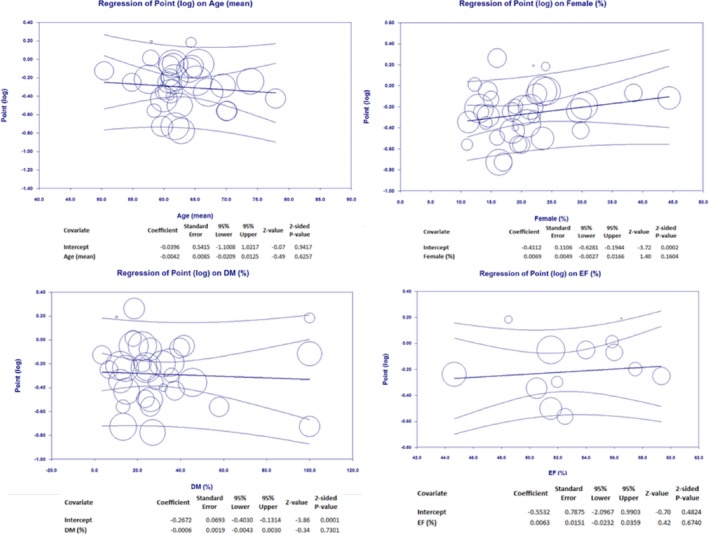
Results of the metaregression analyses. Univariate metaregression analysis showed that the effect of BITA was not influenced by age (slope P value=0.625; intercept P value=0.941), sex (slope P value=0.160; intercept P value=0.0002), diabetes mellitus (slope P value=0.730; intercept P value=0.0001), and ejection fraction (slope P value=0.674; intercept P value=0.482). Similarly, multivariate metaregression analysis showed that the effect of BITA was not influenced by age (slope P value=0.270), sex (slope P value=0.412), diabetes mellitus (slope P value=0.848), and ejection fraction (slope P value=0.644) with intercept P value=0.487 (plot not shown). BITA indicates bilateral internal thoracic artery; DM, diabetes mellitus; EF, ejection fraction.
One‐Year All‐Cause Mortality in the PSM Populations
Mean follow‐up time of the 12 PSM studies was 7.41±4.4 years, and the number of patients included was 34 019. Use of BITA was associated with a similar reduction of mortality at 1‐year and at the end of follow‐up (IRR, 0.70; 95% CI, 0.60–0.82 at 1 year versus IRR, 0.77; 95% CI, 0.70–0.85 at the end of follow‐up; P for subgroup differences=0.43; Figure 3)1 (details of the statistical analysis for the PSM studies included in this analysis are summarized in Table S3). These findings were robust in a leave‐one‐out analysis (Figure 4).2
Figure 3.
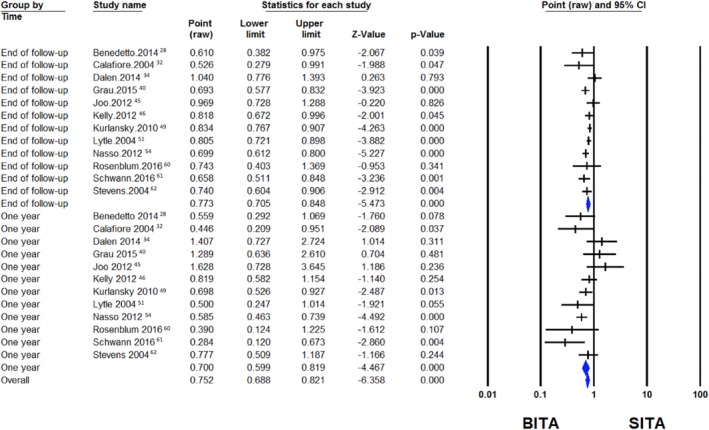
Forest plot comparing the effect of the use of BITA vs SITA on end of follow‐up (top) and 1‐year (bottom) mortality in PSM studies in the general population (12 studies; 34 019 patients). BITA indicates bilateral internal thoracic artery; CI, confidence interval; PSM, propensity‐score matched; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure 4.
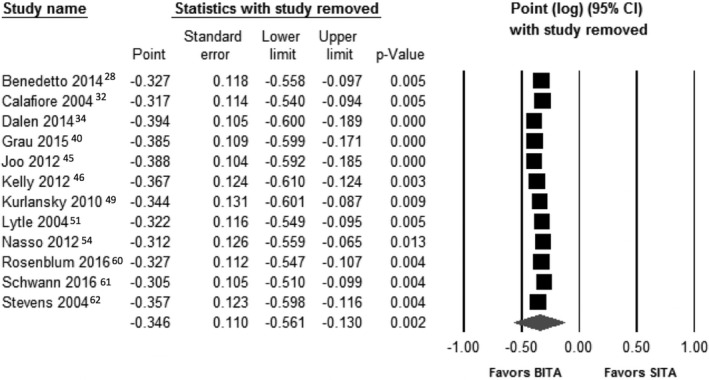
Leave‐one‐out analyisis for 1‐year mortality among PSM studies (12 studies). BITA indicates bilateral internal thoracic artery; CI, confidence interval; PSM, propensity‐score matched; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Publication Bias and Internal Validity Appraisal
Study quality was high across all studies included in the primary analysis (Table S4). Overall heterogeneity was high both at 1‐year analysis in the PSM studies (I2=51%) and at end of follow‐up in the overall studies analysis (I2=71%). Publication bias was low, as assessed by funnel plots, for all‐cause mortality in the primary analysis (Figure 5).
Figure 5.
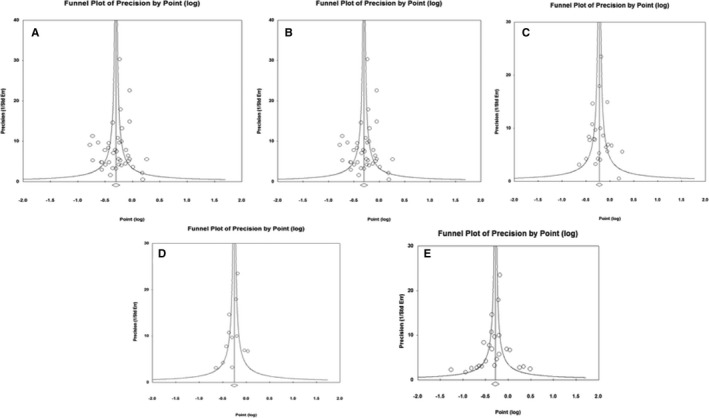
Publication bias as assessed by funnel plots for all‐cause mortality in the primary analysis. A, All included studies. B, Studies performed in the general population vs studies performed in specific subpopulations. C, Unadjusted studies vs adjusted studies. D, PSM studies vs adjusted non‐PSM studies. E, PSM studies at 1‐year follow‐up vs PSM studies at end of follow‐up. PSM indicates propensity‐score matched.
An overview of the results of all the analyses is provided in Table S5.
Discussion
For almost 25 years, the concept that the use of BITA is associated with improved survival after coronary artery bypass surgery has been accepted in the cardiovascular community. This concept is almost completely based on observational studies.
To date, at least 60 English‐language observational studies comparing the clinical outcome of BITA and SITA patients have been published (Figure S1). The overwhelming majority of these have shown better outcomes in the BITA treatment group. Several reports have also suggested that the advantages of BITA grafting could be extended to females,65 diabetics,66 and patients with chronic renal insufficiency.48 Over time, this evidence has been summarized in 6 meta‐analyses.4, 5, 6, 7, 8, 9 All of them showed a significant and similar survival advantage, as measured by the HR, for the use of BITA (see Table 3).4, 5, 6, 7, 8, 9
Table 3.
Published Meta‐Analyses of the Observational Evidence on the BITA vs SITA Comparison
| First Author, Year | Studies Included in Survival Analysis, n | Patients Included in Survival Analysis, n | Type of Observational Studies Included | Patient Populations Excluded by Inclusion Criteria | HR in Favor of BITA |
|---|---|---|---|---|---|
| Taggart, 20015 | 7 | 15 962 | All | None | 0.81 [95% CI 0.70–0.94] |
| Rizzoli, 20024 | 7 | 15 299 | All | High‐risk patients, emergencies, diabetics | 0.79 [95% CI 0.66–0.91] |
| Weiss, 20137 | 27 | 79 063 | All | None | 0.78 [95% CI 0.72–0.84] |
| Takagi, 20146 | 20 | 70 897 | Adjusted | None | 0.80 [95% CI 0.77–0.84] |
| Yi, 20148 | 9 | 15 583 | Adjusted | None | 0.79 [95% CI 0.75–0.84] |
| Buttar, 20179 | 29 | 89 399 | All | None | 0.78 [95% CI 0.72–0.84] |
BITA indicates bilateral internal thoracic artery; HR, hazard ratio; PSM, propensity‐score matched; UNM, unmatched.
Our analysis pools data from 38 of these studies and 174 205 patients and confirms the previous findings (Table 3).4, 5, 6, 7, 8, 9 We used IRRs instead of HR or relative risk ratio to account for potential differences in follow‐up duration within studies and between studies. We confirmed better long‐term survival for BITA compared with SITA (IRR, 0.74; 95% CI, 0.69–0.80; P<0.001; Figure 1A).27–64 This difference was evident independently from the patient population included and the methodology used (Figures S3 through S5). The benefit was uncertain from 1989 to 2000, was consistently significant at the 0.05 level starting in 2001, and crossed the 0.01 and 0.001 levels in 2004 (Figure 1B).27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64
Basing on these data, the current US10 and European11 Guidelines encourage the use of a second arterial graft in patients with a long life expectancy, and last year the Society of Thoracic Surgeons published a position paper strongly encouraging a wider use of arterial grafts.12
It must, however, be noted that the results of the observational studies have not been confirmed in the randomized comparisons. The 4 RCTs that have compared BITA and SITA to date have all failed to show a survival difference between the 2 revascularization strategies.13, 14, 15, 16 Two of the RCTs were small, with less than 100 patients in each arm, and had limited follow‐up, so that they were probably underpowered to detect moderate differences.13, 14 Another study was moderate in size (Stand‐in‐Y,15 800 patients) and the most recent, the ART trial,16 included more than 3000 patients.
The Stand‐in‐Y Mammary study compared the outcomes of 800 patients randomized to receive BITA using 2 different configurations: SITA and radial artery or SITA and saphenous vein.15 At a mean follow‐up of 24.1±9.8 months, no difference in survival was found between the BITA and SITA groups (P=0.62; odds ratio, 0.63; 95% CI, 0.27–1.47), although patients with arterial grafts had better cardiac event–free survival (Wilcoxon test, P<0.0001).
The ART trial randomized 3102 patients to receive 1 or 2 internal thoracic arteries.16 The primary end point is overall survival, and the study was designed to be able to detect a 20% reduction in the primary end point at 10 years. At a planned 5‐year interim analysis, no difference in survival (91.3% in the BITA group and 91.6% in the SITA group; HR, 1.04; CI, 0.81–1.32) or in the composite of mortality, myocardial infarction, and/or stroke (12.2% BITA versus 12.7% SITA; HR, 0.96; CI, 0.79–1.17) was found between groups.
Several methodological flaws in the design of the RCTs can partially explain the variance between the results of the randomized and observational studies. All the RCTs were limited to mid‐term follow‐up, and it is known the attrition rate of saphenous grafts remains low at 5 years19; it is possible that a difference between the groups would have become apparent with further follow‐up. There are additional considerations specifically regarding the ART study that may explain a negative result. A sizeable proportion (23%) of patients randomized to SITA also received a radial artery as an additional arterial graft. There was a high rate of crossover in the group allocated to BITA (16.4%). There was very high compliance with optimal medical therapy in both groups (90% of patients on aspirin, beta‐blockers, and statins). Finally, there was a treatment age interaction that approached statistical significance, favoring BITA in patients aged <70 years whereas BITA appeared harmful in patients aged >70.
There are, however, biological reasons in support of the results of the RCTs. A second arterial conduit to a non‐LAD target has less potential to impact on overall survival than the single left internal thoracic artery to the LAD. Solid evidence suggests, in fact, that in coronary artery bypass surgery, patient survival is mainly determined by the status of the LAD and that grafts to non‐LAD vessels are more likely to affect other cardiac end points (myocardial infarction, angina recurrence, and need for revascularization), but not overall survival.27, 28, 29 The LAD also can provide collaterals to other coronaries (commonly the right coronary); a persistently patent internal thoracic artery graft to the LAD can therefore supply not only the anterior wall, but, through collaterals, viable myocardium in other territories. Last, patency of grafts to the LAD generally exceed the patency of grafts to non‐LAD vessels.3
Our hypothesis, however, is that the difference in results between the RCTs and the observational evidence is attributed to unmeasured confounders and not to the difference in revascularization strategy.
In order to test this hypothesis, we repeated the BITA versus SITA comparison at 1 year, when the attrition rate of the SVGs is still low and a survival difference attributable to a difference in graft patency is unlikely.
Because PSM studies are considered the observational studies less prone to confounders, we decided to limit the 1‐year analysis to PSM studies only.
In fact, PSM series constitute a large amount of the current evidence in the surgical fields.20 The PSM process is thought to be able to minimize differences in the preoperative risk profile of the patients, and PSM studies are often quoted as the best level of evidence after RCTs.20
We found that the relative survival advantage attributed to the BITA group at 1 year was similar to that observed at late follow‐up (Figure 3).3
This finding suggests that factors not related to the conduit patency, such as the patients’ general status or quality of the target vessels, played a role in determining the outcome and that unmatched biases are present even in PSM studies.
The use of the BITA increases the complexity and invasiveness of the procedure. It is likely that surgeons tend to reserve this operation for the patients perceived as healthier and with longer life expectancy from a cardiac and a general health perspective. A bias may also exist in terms of the graftability and location of the target vessels. This type of “eye‐balling” or clinical acumen based on the individual surgeon's experience is very difficult to quantify; the statistics can only be adjusted for the measured, and not for the unmeasured, confounders. Our findings elicit concerns on the ability of the propensity‐matching process to overcome treatment allocation biases in observational studies and assure comparability between groups.
Limitations
This analysis shares the common limitations of meta‐analysis of observational data, although the funnel plots do not indicate important publication bias.
In addition, the different studies included different surgical techniques (on‐ versus off‐pump) and grafting strategies (single versus composite grafts) as well as different definitions and matching algorithms, so that the homogeneity of the included population cannot be regarded as optimal.
In most of the series, the 1‐year IRR was not specified in the original study and had to be derived using the described statistical methods.
Upon careful review of the methods of the PSM studies, we could not confer that the original studies adjusted the variance estimates appropriately for the matched nature of the data in the original studies (Table S3). That said, the HRs would still be correct, and the leave‐one‐out analysis was consistent with the overall findings.
Finally, given that we included only articles in English, a language bias cannot be excluded, although there are no plausible biological reasons to support it.
Conclusions
In conclusion, the present meta‐analysis challenges the benefit traditionally attributed to BITA grafting. The fact that, even in the PSM series, BITA patients exhibit a significant survival advantage at 1‐year follow‐up suggests that unmeasured confounders may account for the reported survival benefit of BITA in the observational series.
In addition, our results suggest that even our best statistical methods to minimize baseline demographic differences in observational studies have major limitations.
Later reporting of the clinical outcomes of ART and new randomized studies are needed to clarify the effect of BITA grafting in patients undergoing CABG.
Sources of Funding
Prof Fremes is partially supported by the Bernard S. Goldman Chair in Cardiovascular Surgery.
Disclosures
Prof Fremes is supported, in part, by the Bernard S. Goldman Chair in Cardiovascular Surgery. The remaining authors have no disclosures to report.
Supporting information
Data S1. Full search strategy.
Table S1. Pretreatment Variables Included for Propensity‐Score Matching
Table S2. Risk Factor Distribution in the Populations of the Studies Included in the Primary Analysis
Table S3. Details of Statistical Analysis for the Propensity‐Score–Matched Studies Included in the 1‐Year Analysis
Table S4. Newcastle–Ottawa Scale for the Studies Included in the Primary Analysis
Table S5. Overview of the Results
Figure S1. Flow chart for study selection.
Figure S2. Leave‐one‐out analysis for the end of follow‐up mortality among all the studies included in the primary analyisis (38 studies). Incident rate ratio (IRR) is used.
Figure S3. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality after the exclusion of studies performed in specific subpopulations (28 studies; 162 989 patients, top) and in those studies performed in specific subpopulations (10 studies; 11 216 patients, bottom). BITA indicates bilateral internal thoracic artery; CI, confidence interval; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure S4. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality in adjusted (22 studies; 155, 925 patients, top) and unadjusted (6 studies; 7064 patients, bottom) studies in the general population. BITA indicates bilateral internal thoracic artery; CI, confidence interval; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure S5. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality in adjusted non‐PSM studies (10 studies; 43 855 patients, top) and PSM studies (12 studies; 34 019 patients, bottom) in the general population. BITA indicates bilateral internal thoracic artery; CI, confidence interval; PSM, propensity‐score matched; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
(J Am Heart Assoc. 2018;7:e008010 DOI: 10.1161/JAHA.117.008010.)29306899
Notes
References
- 1. Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC. Influence of the internal‐mammary‐artery graft on 10‐year survival and other cardiac events. N Engl J Med. 1986;314:1–6. [DOI] [PubMed] [Google Scholar]
- 2. Lytle BW, Blackstone EH, Loop FD, Houghtaling PL, Arnold JH, Akhrass R, McCarthy PM, Cosgrove DM. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 1999;117:855–872. [DOI] [PubMed] [Google Scholar]
- 3. Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years. Ann Thorac Surg. 2004;77:93–101. [DOI] [PubMed] [Google Scholar]
- 4. Rizzoli G, Schiavon L, Bellini P. Does the use of bilateral internal mammary artery (IMA) grafts provide incremental benefit relative to the use of a single IMA graft? A meta‐analysis approach. Eur J Cardiothorac Surg. 2002;22:781–786. [DOI] [PubMed] [Google Scholar]
- 5. Taggart DP, D'Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet. 2001;358:870–875. [DOI] [PubMed] [Google Scholar]
- 6. Takagi H, Goto S, Watanabe T, Mizuno Y, Kawai N, Umemoto T. A meta‐analysis of adjusted hazard ratios from 20 observational studies of bilateral versus single internal thoracic artery coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2014;148:1282–1290. [DOI] [PubMed] [Google Scholar]
- 7. Weiss AJ, Zhao S, Tian DH, Taggart DP, Yan TD. A meta‐analysis comparing bilateral internal mammary artery with left internal mammary artery for coronary artery bypass grafting. Ann Cardiothorac Surg. 2013;2:390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yi G, Shine B, Rehman SM, Altman DG, Taggart DP. Effect of bilateral internal mammary artery grafts on long‐term survival: a meta‐analysis approach. Circulation. 2014;130:539–545. [DOI] [PubMed] [Google Scholar]
- 9. Buttar SN, Yan TD, Taggart DP, Tian DH. Long‐term and short‐term outcomes of using bilateral internal mammary artery grafting versus left internal mammary artery grafting: a meta‐analysis. Heart. 2017;103:1419–1426. [DOI] [PubMed] [Google Scholar]
- 10. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e652–e735. [DOI] [PubMed] [Google Scholar]
- 11. Authors/Task Force members , Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio‐Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 12. Aldea GS, Bakaeen FG, Pal J, Fremes S, Head SJ, Sabik J, Rosengart T, Kappetein AP, Thourani VH, Firestone S, Mitchell JD; Society of Thoracic Surgeons . The Society of Thoracic Surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg. 2016;101:801–809. [DOI] [PubMed] [Google Scholar]
- 13. Myers WO, Berg R, Ray JF, Douglas‐Jones JW, Maki HS, Ulmer RH, Chaitman BR, Reinhart RA. All‐artery multigraft coronary artery bypass grafting with only internal thoracic arteries possible and safe: a randomized trial. Surgery. 2000;128:650–659. [DOI] [PubMed] [Google Scholar]
- 14. Gaudino M, Cellini C, Pragliola C, Trani C, Burzotta F, Schiavoni G, Nasso G, Possati G. Arterial versus venous bypass grafts in patients with in‐stent restenosis. Circulation. 2005;112:I265–I269. [DOI] [PubMed] [Google Scholar]
- 15. Nasso G, Coppola R, Bonifazi R, Piancone F, Bozzetti G, Speziale G. Arterial revascularization in primary coronary artery bypass grafting: direct comparison of 4 strategies—results of the Stand‐in‐Y Mammary Study. J Thorac Cardiovasc Surg. 2009;137:1093–1100. [DOI] [PubMed] [Google Scholar]
- 16. Taggart DP, Altman DG, Gray AM, Lees B, Gerry S, Benedetto U, Flather M. Randomized trial of bilateral versus single internal‐thoracic‐artery grafts. N Engl J Med. 2016;375:2540–2549. [DOI] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wells G, Shea B, O'Connel D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. [Internet]. 2011. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed September 15, 2017.
- 19. Benedetto U, Raja SG, Albanese A, Amrani M, Biondi‐Zoccai G, Frati G. Searching for the second best graft for coronary artery bypass surgery: a network meta‐analysis of randomized controlled trials†. Eur J Cardiothorac Surg. 2015;47:59–65; discussion, 65. [DOI] [PubMed] [Google Scholar]
- 20. Lonjon G, Boutron I, Trinquart L, Ahmad N, Aim F, Nizard R, Ravaud P. Comparison of treatment effect estimates from prospective nonrandomized studies with propensity score analysis and randomized controlled trials of surgical procedures. Ann Surg. 2014;259:18–25. [DOI] [PubMed] [Google Scholar]
- 21. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 22. Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta‐analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–2834. [DOI] [PubMed] [Google Scholar]
- 23. Yanagawa B, Verma S, Jüni P, Tam DY, Mazine A, Puskas JD, Friedrich JO. A systematic review and meta‐analysis of in situ versus composite bilateral internal thoracic artery grafting. J Thorac Cardiovasc Surg. 2017;153:1108–1116.e16. [DOI] [PubMed] [Google Scholar]
- 24. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time‐to‐event data into meta‐analysis. Trials. 2007;8:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rothstein HR, Sutton AJ, Borenstein M. Publication Bias in Meta‐Analysis: Prevention, Assessment and Adjustments. Chichester, UK: John Wiley & Sons Ltd; 2005. [Google Scholar]
- 26. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ashraf SS, Shaukat N, Akhtar K, Love H, Shaw J, Rowlands DJ, Keenan D. A comparison of early mortality and morbidity after single and bilateral internal mammary artery grafting with the free right internal mammary artery. Br Heart J. 1994;72:321–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Benedetto U, Amrani M, Gaer J, Bahrami T, de Robertis F, Simon AR, Raja SG; Harefield Cardiac Outcomes Research Group . The influence of bilateral internal mammary arteries on short‐ and long‐term outcomes: a propensity score matching in accordance with current recommendations. J Thorac Cardiovasc Surg. 2014;148:2699–2705. [DOI] [PubMed] [Google Scholar]
- 29. Berreklouw E, Rademakers PP, Koster JM, van Leur L, van der Wielen BJ, Westers P. Better ischemic event‐free survival after two internal thoracic artery grafts: 13 years of follow‐up. Ann Thorac Surg. 2001;72:1535–1541. [DOI] [PubMed] [Google Scholar]
- 30. Bonacchi M, Maiani M, Prifti E, Di Eusanio G, Di Eusanio M, Leacche M. Urgent/emergent surgical revascularization in unstable angina: influence of different type of conduits. J Cardiovasc Surg (Torino). 2006;47:201–210. [PubMed] [Google Scholar]
- 31. Buxton BF, Komeda M, Fuller JA, Gordon I. Bilateral internal thoracic artery grafting may improve outcome of coronary artery surgery. Risk‐adjusted survival. Circulation. 1998;98:II1–II6. [PubMed] [Google Scholar]
- 32. Calafiore AM, Di Giammarco G, Teodori G, Di Mauro M, Iacò AL, Bivona A, Contini M, Vitolla G. Late results of first myocardial revascularization in multiple vessel disease: single versus bilateral internal mammary artery with or without saphenous vein grafts. Eur J Cardiothorac Surg. 2004;26:542–548. [DOI] [PubMed] [Google Scholar]
- 33. Carrier M, Cossette M, Pellerin M, Hébert Y, Bouchard D, Cartier R, Demers P, Jeanmart H, Pagé P, Perrault LP. Statin treatment equalizes long‐term survival between patients with single and bilateral internal thoracic artery grafts. Ann Thorac Surg. 2009;88:789–795; discussion, 795. [DOI] [PubMed] [Google Scholar]
- 34. Dalén M, Ivert T, Holzmann MJ, Sartipy U. Bilateral versus single internal mammary coronary artery bypass grafting in Sweden from 1997‐2008. PLoS One. 2014;9:e86929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Danzer D, Christenson JT, Kalangos A, Khatchatourian G, Bednarkiewicz M, Faidutti B. Impact of double internal thoracic artery grafts on long‐term outcomes in coronary artery bypass grafting. Tex Heart Inst J. 2001;28:89–95. [PMC free article] [PubMed] [Google Scholar]
- 36. Dewar LR, Jamieson WR, Janusz MT, Adeli‐Sardo M, Germann E, MacNab JS, Tyers GF. Unilateral versus bilateral internal mammary revascularization. Survival and event‐free performance. Circulation. 1995;92:II8–II13. [DOI] [PubMed] [Google Scholar]
- 37. Endo M, Nishida H, Tomizawa Y, Kasanuki H. Benefit of bilateral over single internal mammary artery grafts for multiple coronary artery bypass grafting. Circulation. 2001;104:2164–2170. [DOI] [PubMed] [Google Scholar]
- 38. Gansera B, Loef A, Angelis I, Gillrath G, Schmidtler F, Kemkes BM. Double thoracic artery—halved mid‐term mortality? A 5‐year follow‐up of 716 patients receiving bilateral ITA versus 662 patients with single ITA. Z Kardiol. 2004;93:878–883. [DOI] [PubMed] [Google Scholar]
- 39. Gansera B, Delalic A, Eszlari E, Eichinger W. 14‐year results of bilateral versus single internal thoracic artery grafts for left‐sided myocardial revascularization in young diabetic patients. Thorac Cardiovasc Surg. 2017;65:272–277. [DOI] [PubMed] [Google Scholar]
- 40. Grau JB, Johnson CK, Kuschner CE, Ferrari G, Shaw RE, Brizzio ME, Zapolanski A. Impact of pump status and conduit choice in coronary artery bypass: a 15‐year follow‐up study in 1412 propensity‐matched patients. J Thorac Cardiovasc Surg. 2015;149:1027–1033.e2. [DOI] [PubMed] [Google Scholar]
- 41. Hirotani T, Nakamichi T, Munakata M, Takeuchi S. Risks and benefits of bilateral internal thoracic artery grafting in diabetic patients. Ann Thorac Surg. 2003;76:2017–2022. [DOI] [PubMed] [Google Scholar]
- 42. Itoh S, Kimura N, Adachi H, Yamaguchi A. Is bilateral internal mammary arterial grafting beneficial for patients aged 75 years or older? Circ J. 2016;80:1756–1763. [DOI] [PubMed] [Google Scholar]
- 43. Johnson WD, Brenowitz JB, Kayser KL. Factors influencing long‐term (10‐year to 15‐year) survival after a successful coronary artery bypass operation. Ann Thorac Surg. 1989;48:19–24; discussion, 24–25. [DOI] [PubMed] [Google Scholar]
- 44. Jones JW, Schmidt SE, Miller CC, Beall AC, Baldwin JC. Bilateral internal thoracic artery operations in the elderly. J Cardiovasc Surg (Torino). 2000;41:165–170. [PubMed] [Google Scholar]
- 45. Joo HC, Youn YN, Yi G, Chang BC, Yoo KJ. Off‐pump bilateral internal thoracic artery grafting in right internal thoracic artery to right coronary system. Ann Thorac Surg. 2012;94:717–724. [DOI] [PubMed] [Google Scholar]
- 46. Kelly R, Buth KJ, Légaré JF. Bilateral internal thoracic artery grafting is superior to other forms of multiple arterial grafting in providing survival benefit after coronary bypass surgery. J Thorac Cardiovasc Surg. 2012;144:1408–1415. [DOI] [PubMed] [Google Scholar]
- 47. Kieser TM, Lewin AM, Graham MM, Martin B‐J, Galbraith PD, Rabi DM, Norris CM, Faris PD, Knudtson ML, Ghali WA; APPROACH Investigators . Outcomes associated with bilateral internal thoracic artery grafting: the importance of age. Ann Thorac Surg. 2011;92:1269–1275; discussion, 1275–1276. [DOI] [PubMed] [Google Scholar]
- 48. Kinoshita T, Asai T, Suzuki T. Off‐pump bilateral skeletonized internal thoracic artery grafting in patients with chronic kidney disease. J Thorac Cardiovasc Surg. 2015;150:315–321.e3. [DOI] [PubMed] [Google Scholar]
- 49. Kurlansky PA, Traad EA, Dorman MJ, Galbut DL, Zucker M, Ebra G. Thirty‐year follow‐up defines survival benefit for second internal mammary artery in propensity‐matched groups. Ann Thorac Surg. 2010;90:101–108. [DOI] [PubMed] [Google Scholar]
- 50. Locker C, Schaff HV, Dearani JA, Joyce LD, Park SJ, Burkhart HM, Suri RM, Greason KL, Stulak JM, Li Z, Daly RC. Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery: analysis of 8622 patients with multivessel disease. Circulation. 2012;126:1023–1030. [DOI] [PubMed] [Google Scholar]
- 51. Lytle BW, Blackstone EH, Sabik JF, Houghtaling P, Loop FD, Cosgrove DM. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg. 2004;78:2005–2012; discussion, 2012–2014. [DOI] [PubMed] [Google Scholar]
- 52. Medalion B, Mohr R, Ben‐Gal Y, Nesher N, Kramer A, Eliyahu S, Pevni D. Arterial coronary artery bypass grafting is safe and effective in elderly patients. J Thorac Cardiovasc Surg. 2015;150:607–612. [DOI] [PubMed] [Google Scholar]
- 53. Mohammadi S, Kalavrouziotis D, Cresce G, Dagenais F, Dumont E, Charbonneau E, Voisine P. Bilateral internal thoracic artery use in patients with low ejection fraction: is there any additional long‐term benefit? Eur J Cardiothorac Surg. 2014;46:425–431; discussion, 431. [DOI] [PubMed] [Google Scholar]
- 54. Nasso G, Popoff G, Lamarra M, Romano V, Coppola R, Bartolomucci F, Giglio MD, Romeo F, Tavazzi L, Speziale G. Impact of arterial revascularization in patients undergoing coronary bypass. J Card Surg. 2012;27:427–433. [DOI] [PubMed] [Google Scholar]
- 55. Naunheim KS, Barner HB, Fiore AC. 1990: results of internal thoracic artery grafting over 15 years: single versus double grafts. 1992 update. Ann Thorac Surg. 1992;53:716–718. [DOI] [PubMed] [Google Scholar]
- 56. Navia DO, Vrancic M, Piccinini F, Camporrotondo M, Dorsa A, Espinoza J, Benzadon M, Camou J. Myocardial revascularization exclusively with bilateral internal thoracic arteries in T‐graft configuration: effects on late survival. Ann Thorac Surg. 2016;101:1775–1781. [DOI] [PubMed] [Google Scholar]
- 57. Parsa CJ, Shaw LK, Rankin JS, Daneshmand MA, Gaca JG, Milano CA, Glower DD, Smith PK. Twenty‐five‐year outcomes after multiple internal thoracic artery bypass. J Thorac Cardiovasc Surg. 2013;145:970–975. [DOI] [PubMed] [Google Scholar]
- 58. Pettinari M, Sergeant P, Meuris B. Bilateral internal thoracic artery grafting increases long‐term survival in elderly patients. Eur J Cardiothorac Surg. 2015;47:703–709. [DOI] [PubMed] [Google Scholar]
- 59. Pick AW, Orszulak TA, Anderson BJ, Schaff HV. Single versus bilateral internal mammary artery grafts: 10‐year outcome analysis. Ann Thorac Surg. 1997;64:599–605. [DOI] [PubMed] [Google Scholar]
- 60. Rosenblum JM, Harskamp RE, Hoedemaker N, Walker P, Liberman HA, de Winter RJ, Vassiliades TA, Puskas JD, Halkos ME. Hybrid coronary revascularization versus coronary artery bypass surgery with bilateral or single internal mammary artery grafts. J Thorac Cardiovasc Surg. 2016;151:1081–1089. [DOI] [PubMed] [Google Scholar]
- 61. Schwann TA, Hashim SW, Badour S, Obeid M, Engoren M, Tranbaugh RF, Bonnell MR, Habib RH. Equipoise between radial artery and right internal thoracic artery as the second arterial conduit in left internal thoracic artery‐based coronary artery bypass graft surgery: a multi‐institutional study. Eur J Cardiothorac Surg. 2016;49:188–195. [DOI] [PubMed] [Google Scholar]
- 62. Stevens LM, Carrier M, Perrault LP, Hébert Y, Cartier R, Bouchard D, Fortier A, El‐Hamamsy I, Pellerin M. Single versus bilateral internal thoracic artery grafts with concomitant saphenous vein grafts for multivessel coronary artery bypass grafting: effects on mortality and event‐free survival. J Thorac Cardiovasc Surg. 2004;127:1408–1415. [DOI] [PubMed] [Google Scholar]
- 63. Tarelli G, Mantovani V, Maugeri R, Chelazzi P, Vanoli D, Grossi C, Ornaghi D, Panisi P, Sala A. Comparison between single and double internal mammary artery grafts: results over ten years. Ital Heart J. 2001;2:423–427. [PubMed] [Google Scholar]
- 64. Toumpoulis IK, Anagnostopoulos CE, Balaram S, Swistel DG, Ashton RC, DeRose JJ. Does bilateral internal thoracic artery grafting increase long‐term survival of diabetic patients? Ann Thorac Surg. 2006;81:599–606; discussion, 606–607. [DOI] [PubMed] [Google Scholar]
- 65. Gansera B, Gillrath G, Lieber M, Angelis I, Schmidtler F, Kemkes BM. Are men treated better than women? Outcome of male versus female patients after CABG using bilateral internal thoracic arteries. Thorac Cardiovasc Surg. 2004;52:261–267. [DOI] [PubMed] [Google Scholar]
- 66. Raza S, Sabik JF, Masabni K, Ainkaran P, Lytle BW, Blackstone EH. Surgical revascularization techniques that minimize surgical risk and maximize late survival after coronary artery bypass grafting in patients with diabetes mellitus. J Thorac Cardiovasc Surg. 2014;148:1257–1264; discussion, 1264–1266. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Full search strategy.
Table S1. Pretreatment Variables Included for Propensity‐Score Matching
Table S2. Risk Factor Distribution in the Populations of the Studies Included in the Primary Analysis
Table S3. Details of Statistical Analysis for the Propensity‐Score–Matched Studies Included in the 1‐Year Analysis
Table S4. Newcastle–Ottawa Scale for the Studies Included in the Primary Analysis
Table S5. Overview of the Results
Figure S1. Flow chart for study selection.
Figure S2. Leave‐one‐out analysis for the end of follow‐up mortality among all the studies included in the primary analyisis (38 studies). Incident rate ratio (IRR) is used.
Figure S3. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality after the exclusion of studies performed in specific subpopulations (28 studies; 162 989 patients, top) and in those studies performed in specific subpopulations (10 studies; 11 216 patients, bottom). BITA indicates bilateral internal thoracic artery; CI, confidence interval; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure S4. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality in adjusted (22 studies; 155, 925 patients, top) and unadjusted (6 studies; 7064 patients, bottom) studies in the general population. BITA indicates bilateral internal thoracic artery; CI, confidence interval; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.
Figure S5. Forest plots comparing the effect of the use of BITA vs SITA on end of follow‐up mortality in adjusted non‐PSM studies (10 studies; 43 855 patients, top) and PSM studies (12 studies; 34 019 patients, bottom) in the general population. BITA indicates bilateral internal thoracic artery; CI, confidence interval; PSM, propensity‐score matched; SITA, single internal thoracic artery. Incident rate ratio (IRR) is used.


