Abstract
Background
Physicians' gender bias may contribute to gender disparities in cardiovascular testing. We used the Implicit Association Test to examine the association of implicit gender biases with decisions to use cardiovascular tests.
Methods and Results
In 2014, cardiologists completed Implicit Association Tests and a clinical vignette with patient gender randomly assigned. The Implicit Association Tests measured implicit gender bias for the characteristics of strength and risk taking. The vignette represented an intermediate likelihood of coronary artery disease regardless of patient gender: chest pain (part 1) followed by an abnormal exercise treadmill test (part 2). Cardiologists rated the likelihood of coronary artery disease and the usefulness of stress testing and angiography for the assigned patient. Of the 503 respondents (9.3% of eligible; 87% male, median age of 45 years, 58% in private practice), the majority associated strength or risk taking implicitly with male more than female patients. The estimated likelihood of coronary artery disease for both parts of the vignette was similar by patient gender. The utility of secondary stress testing after an abnormal exercise treadmill test was rated as “high” more often for female than male patients (32.8% versus 24.3%, P=0.04); this difference did not vary with implicit bias. Angiography was more consistently rated as having “high” utility for male versus female patients (part 1: 19.7% versus 9.8%; part 2: 73.7% versus 64.3%; P<0.05 for both); this difference was larger for cardiologists with higher implicit gender bias on risk taking (P=0.01).
Conclusions
Cardiologists have varying degrees of implicit gender bias. This bias explained some, but not all, of the gender variability in simulated clinical decision‐making for suspected coronary artery disease.
Keywords: angiography, gender disparities, implicit bias, stress testing
Subject Categories: Cardiovascular Disease, Women, Diagnostic Testing, Quality and Outcomes
Clinical Perspective
What Is New?
In a survey of cardiologists practicing in the United States, we detected implicit gender bias suggesting these cardiologists are more likely to view men as being strong and more likely to take risks than women.
Despite similar estimates of coronary artery disease likelihood, cardiology physicians rated the usefulness of angiography higher for a standardized male than female patient.
The gender difference in angiography ratings was related to cardiologists' implicit gender bias, suggesting that the perception of men being more risk tolerant may influence decisions about angiography with regard to female versus male patients with chest pain.
What Are the Clinical Implications?
Implicit gender bias explained some, but not all, gender differences in simulated clinical decision making, suggesting that factors beyond clinical appropriateness alone play a role.
Gender bias may be more likely in clinical scenarios that involve more subjectivity or higher risk procedures, and bias may be less likely when explicit gender‐specific recommendations exist.
Efforts to ensure equity in care for women and men should include improving the evidence base, particularly for women, who are historically underrepresented in trials and for whom there is greater clinician uncertainty about how best to manage their conditions.
Introduction
Gender differences in the use of cardiac tests in patients with suspected or confirmed coronary artery disease (CAD) have been known for decades.1, 2, 3, 4, 5, 6, 7, 8 After an abnormal cardiac stress test, women are less likely to undergo any subsequent diagnostic testing, including secondary stress testing or angiography.6, 7, 8 These gender differences persist even after considering patient factors that may explain variation in care such as differences in comorbidities, presentation, appropriateness of treatment, and patient preferences—suggesting that these differences represent disparities, as defined by the Institute of Medicine.7, 8, 9, 10, 11, 12 Despite studies documenting gender disparities in the use of cardiovascular tests, few have examined the underlying reasons for these disparities in management.
A potential reason for gender disparities in cardiovascular testing is providers' gender stereotyping and bias.11, 13, 14, 15, 16 Gender stereotyping is the process by which people make assumptions about others' characteristics based on their gender, along specific trait dimensions.17 Gender stereotypes have remained remarkably consistent over time, with men traditionally perceived to be stronger (both physically and mentally) and more likely to take risks compared with women and with women perceived to be more emotional and focused on caring for others than men.18, 19, 20, 21, 22 These gender stereotypes are referred to as bias because they create unjust assumptions or decisions about a person.17, 23 Bias has been inferred in prior studies when gender differences in care persist after adjusting for many patient, physician, and health system characteristics.24, 25, 26, 27 A recent systematic review found 14 studies that examined the presence of gender bias using controlled, randomly assigned vignettes to examine the influence of patient gender on healthcare professionals' attitudes, diagnoses, and treatment decisions.12 However, no study has directly measured physician gender bias using a validated measure.12
The Implicit Association Test (IAT) is a reliable and validated measure for determining implicit (unconscious) bias.17, 23, 28, 29, 30, 31, 32, 33 The IAT measures bias through speed of response (reaction time), operating on the principle that it is easier to pair concepts that are more strongly associated in one's minds than to pair concepts less strongly associated, regardless of one's conscious beliefs or values.31 The IAT has been used to measure race/ethnicity bias and has predicts behavior including physicians' treatment recommendations for hypothetical patients.28, 34 Although the IAT has been used to measure implicit gender bias in career and educational roles,35, 36 no study has examined the association between implicit gender bias and decision‐making in health care.12
Accordingly, we conducted a survey of cardiology physicians to measure implicit gender bias using the IAT and to determine the extent to which it is associated with making judgments about cardiac testing for hypothetical male and female patients with similar likelihoods of obstructive CAD. We hypothesized little or no effect of physician gender bias on treatment decisions for the male patient and lower use of cardiovascular tests among gender‐biased physicians for the female patient.
Methods
Study Design
This between‐subjects randomized experimental study was performed in a cohort of practicing US cardiologists. Eligible cardiologists were invited by e‐mail with a link to a secure, web‐based survey. Privately, and at their own pace, the participating cardiologists completed informed consent, read the case vignette and answered the case questions, completed 2 measures of implicit gender bias (IATs) in random order, and answered sociodemographic questions (age, race, gender, practice type, specialty).
Participants were told that the purpose of the study was to better understand provider approaches to clinical decision‐making. The focus on gender was not immediately disclosed to avoid sensitizing participants to guard against bias. After the case questions were completed, participants were fully informed about the purpose of the study but were not allowed to change their prior answers. Next, participants completed the IATs and demographic questions. Participants were e‐mailed a $25 gift card on survey completion. The survey instrument was administered by Project Implicit, a nonprofit research collaboration at Harvard University (https://implicit.harvard.edu/implicit/). The Colorado Multiple Institutional Review Board at the University of Colorado School of Medicine approved the study.
Study Population
Participants were located through state cardiology foundations or, for states without this option, Research Now, a marketing company that maintains an “opt‐in” survey panel of cardiology physicians.37 Recruitment for the national survey took place from March to November 2014. All cardiology physicians identified by either method were e‐mailed up to 4 invitations to participate. Participants who saw only pediatric patients were excluded from the analysis because the study vingettes portrayed adult patients.
An invitation to participate was e‐mailed to 5413 cardiology physicians throughout the United States with valid e‐mail addresses; of these, 269 (5.0%) opted out and 568 (10.5% of those eligible) completed the entire survey. Of completed surveys, 12 were excluded for being pediatric cardiologists, and 53 were excluded for having an invalid IAT score (based on high errors rates).29 The characteristics of those included versus excluded for IAT errors were not statistically different (Table S1). The final sample for analysis included 503 (9.3% of eligible) cardiology physicians (Figure 1).
Figure 1.
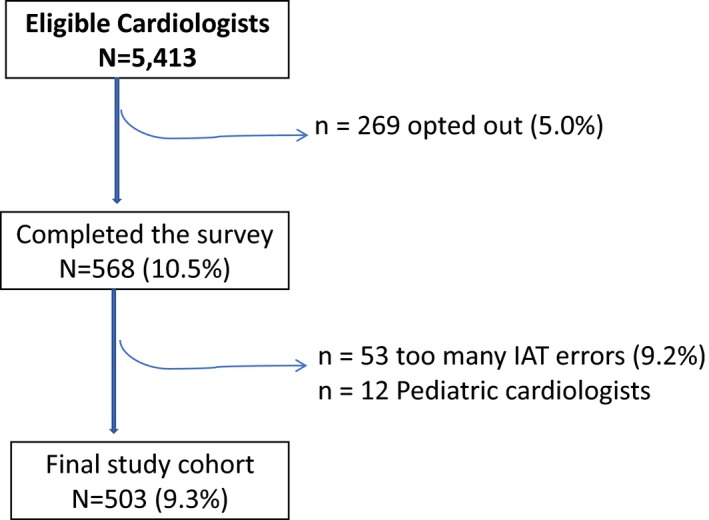
Flowchart of the study population. IAT indicates Implicit Association Test.
Participants were mostly male (87%), white (62%), in private practice (58%), and noninvasive cardiologists (52%). The median age was 45 years (range: 28–89 years), and the median number of years in practice was 12 (range: 1–55 years). The characteristics of the participants who were randomly assigned a male or female case patient did not differ significantly (Table 1). The demographics of the study population are similar to members of large cardiology organizations.38 The American College of Cardiology, for example, reports that 12% of physician members are, compared with 13% of our study sample.39, 40, 41
Table 1.
Cardiology Physician Participant Characteristics by Vignette Patient Gender
| All Participants (N=503) | Male Patient (n=259) | Female Patient (n=244) | P Valuea | |
|---|---|---|---|---|
| Age, y | ||||
| Median (range) | 45 (28–89) | 45 (29–71) | 45 (28–89) | 0.65 |
| Male, n (%) | 436 (86.9) | 225 (51.6) | 211 (48.4) | 0.99 |
| Race/ethnicity, n (%) | ||||
| White | 310 (62.3) | 154 (49.7) | 156 (50.3) | 0.57 |
| Asian | 132 (26.5) | 71 (53.8) | 61 (46.2) | |
| Otherb | 61 (12.1) | 34 (55.7) | 27 (44.3) | |
| Specialty, n (%) | ||||
| General/noninvasive | 264 (52.5) | 140 (53.0) | 124 (47.0) | 0.85 |
| Interventional | 165 (32.8) | 84 (50.9) | 81 (49.1) | |
| Electrophysiology | 40 (8.0) | 19 (47.5) | 21 (52.5) | |
| Otherc | 34 (6.8) | 16 (47.1) | 18 (52.9) | |
| Years in practice | ||||
| Median (range) | 12 (1–55) | 12 (1–45) | 12 (1–55) | 0.40 |
| Practice setting, n (%) | ||||
| Academic/university | 207 (41.2) | 101 (48.8) | 106 (51.2) | 0.31 |
| Private practice | 291 (57.9) | 158 (53.4) | 138 (56.5) | |
Wilcoxon or χ2 test.
Includes black or African American, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, Hispanic, those who picked multiple race/ethnicities, and those who declined to answer.
Includes heart failure/transplant, adult congenital cardiology, cardiothoracic surgery, and those who declined to answer.
Case Vignette
The vignette had 2 parts for the same patient (Table S2). Part 1 described a patient presenting with chest pain who, according to the information provided, would have an intermediate pretest likelihood of obstructive CAD for a male or female patient.42 Part 2 described the same patient returning with continued episodes of chest pain and an abnormal exercise treadmill test (ETT; Duke Treadmill Score 5), again suggesting an intermediate likelihood of obstructive CAD regardless of gender. For accuracy and clinical validity, the case scenarios were reviewed by a panel of 10 cardiologists with both clinical and research experience.
At the end of each part of the case description, participants rated the likelihood (low, intermediate, or high) that the patient's symptoms were related to obstructive CAD and their certainty (low, intermediate, or high) of this estimate. Finally, participants were asked to rate the usefulness (1 indicates “option has no use for this case,” 10 indicates “option is of utmost importance for this patient”) of stress testing and coronary angiography for that patient.
The survey instrument randomly assigned participants to review the exact same case with either a male or female patient. Patient gender was identified by an accompanying picture and the usage of appropriate pronouns. The patient photos were matched between genders for perceived age, attractiveness, likeability, and representativeness of gender.43
Measures of Gender Bias
We developed 2 web‐based IATs to measure implicit gender bias on strength and risk taking. These 2 dimensions are known gender stereotypes (both more strongly associated with men than women) that our research team and consulting panel of cardiologists believed to be most likely to influence decisions to use cardiac procedures.18, 19, 20, 21, 22
The IAT measures implicit bias through the speed with which an individual accurately sorts concepts and is based on the assumption that concepts will be sorted more quickly when they are more tightly associated.31 The strength IAT, for example, asked each participant to sort images and words under 2 conditions. Condition 1, comprising pictures of men and words synonymous with strength (eg, “robust” or “powerful”), required one response, whereas pictures of women and words synonymous with weakness (eg, “delicate” or “mild”) required a different response. Condition 2, comprising pictures of women and strong words, required one response, whereas pictures of men and weak words required a different response. Participants were told to respond as quickly as possible, without sacrificing accuracy. Differences in the speed of correct responses in each condition serve as a proxy for how tightly the concepts are associated in the participant's mind.31 Faster responses in condition 1 than condition 2 indicate a stereotypical association of men with strength and women with weakness—the greater the time differences between the 2 conditions, the stronger the implicit association.44 The risk‐taking IAT was procedurally the same, except that it measured implicit gender bias on “takes risk versus avoids risk.”
We identified words that had been rated as the best synonyms for the target concepts (Table S3). We chose 6 pictures of men and women from a facial stimuli database that were rated by a panel of 10 physicians to be similar in age, attractiveness, likability, and representative of their gender category.43 The ordering of the concept pairings in the 2 sorting conditions was randomized across participants.
IAT Scoring
Implicit gender bias was assessed using standard IAT D scores, which account for variations in respondents' average speed.29 IAT D scores are computed as the mean difference in response latency of trial blocks divided by the overall standard deviation. The IAT‐D score has a possible range of −2 to +2. The higher the D score, the higher the implicit gender bias of associating strength or risk taking with men more than women, with negative numbers indicating a reversal in bias. For descriptive purposes, IAT D scores were categorized into standard classifications (no, slight, medium, or high bias).29 Break points for slight (D=0.15), medium (D=0.35), and high (D=0.65) were selected conservatively according to psychological conventions for effect size. Because the IAT is a performance‐based measure, a high error rate (>30% of responses) indicates intentional inattention (eg, random responding) or misunderstanding task instructions. Based on standard practices in IAT research, participants with error rates >30% were excluded.29 Participants were informed before each IAT that if they made too many errors, the test would not provide results.
Pretesting, Pilot Testing, and Validation of Survey Measures
Using guidelines for pretesting questionnaires, we conducted interviews with 10 cardiologists to determine their reaction to and understanding of the web‐based survey.45 We asked half of the respondents to think aloud while they were completing the case scenario questionnaire and IAT measures. The interviewer probed the respondents about how they were interpreting each question and whether their responses were adequately covered by the response options provided. The survey was modified based on these initial interviews. For the other half of the interviews, participants completed the modified web‐based survey under usual conditions. On completion of the survey, the interviewer probed participants about specific questions and response sets. We ended the pretesting with more general questions about general content of the survey, ease of completion, comfort with instructions, and any other concerns. These interviews informed final revisions of the survey.
We piloted the survey among 53 cardiologists who were not part of the pretesting or the national study. Pilot survey participants had characteristics (82% men, 63% noninvasive cardiologists), case responses, and mean IAT scores (risk‐taking IAT score: 0.45 [SD: 0.54]; strength IAT score: 0.60 [SD: 0.42]) similar to those of the larger national sample. Among this pilot sample, internal consistency of the IATs using Pearson correlation coefficients was adequate (strong IAT: r=0.65, P<0.01, Cronbach α=0.79; risk‐taking IAT: r=0.68, P<0.01, Cronbach α=0.81) and comparable to other commonly used IATs.46 Eleven of the pilot participants repeated the IATs ≈30 days after the initial survey; test–retest reliability using Pearson correlation coefficients was high (strong IAT: r=0.68, P=0.02; risk‐taking IAT: r=0.78, P<0.01). Survey responses from the pilot participants were not included in the final study cohort reported in this article.
Statistical Analyses
Demographic characteristics of the participating cardiologists were described. Based on the distribution of responses, the case management ratings were categorized as low/intermediate (1–7) or high (8–10) agreement. Case management responses were compared for the female and male patients. Physician factors associated with patient gender differences in case responses were explored. The association of cardiologists' demographic factors, including age, gender, race, years in practice and specialty, and IAT scores, were also assessed.
Next, we examined the relationship between patient gender and the participants' ratings (high versus low/intermediate) for either stress testing or angiography using logistic regression analysis. To test the extent to which implicit gender bias influenced differences in management of male and female patients, we included an interaction term for patient gender and physician IAT D score (modeled as a continuous variable). Multivariable models examining this interaction included the physicians' specialty and estimated likelihood of CAD. The analysis was conducted using SAS 9.4 software (SAS Institute).
Results
Implicit Gender Bias
Among the 503 participants, the mean risk‐taking IAT score was 0.42 (SD: 0.41), and mean strength IAT score was 0.66 (SD: 0.40), consistent with gender bias that males take more risks and are stronger than females (Figure 2). When categorized by extent of bias, 74.7% and 89.9% of the physicians had some implicit gender bias on risk taking and strength, respectively; 32.4% and 57.6% had high implicit bias on risk taking and strength, respectively (Figure 2).
Figure 2.
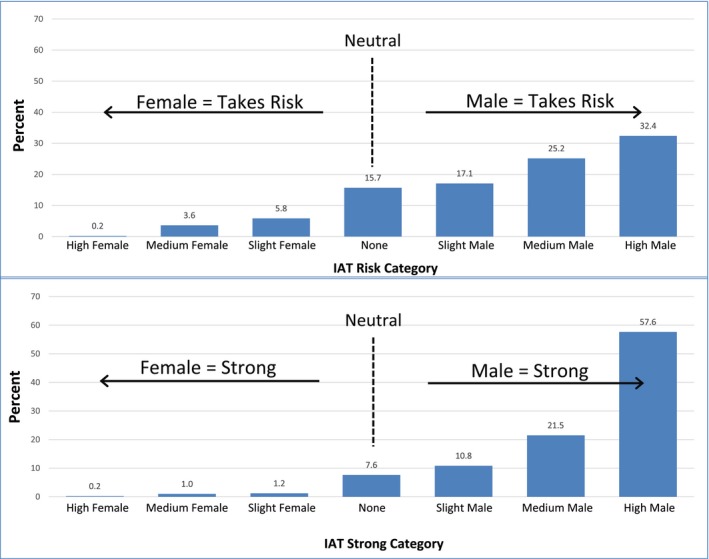
Cardiology physicians' gender bias regarding risk taking and strength. IAT indicates Implicit Association Test.
In unadjusted analysis, female cardiologists had less implicit gender bias on both risk taking and strength; younger age and nonwhite race of the physician were also associated with less implicit gender bias on strength. After adjustment, female cardiologists still showed significantly less implicit gender bias on risk taking or strength than male cardiologists (risk‐taking bias: D=−0.17, P<0.01; strength bias: D=−0.21, P<0.01). Nonwhite race and age were no longer significant after adjustment (Table 2).
Table 2.
Physician Factors Associated With Implicit Gender Bias
| Measure | Risk‐Taking IATa | Strength IATa | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjustedb | Unadjusted | Adjustedb | |||||
| Estimate | P Value | Estimate | P Value | Estimate | P Value | Estimate | P Value | |
| Intercept | ··· | ··· | 0.45 | <0.01 | ··· | ··· | 0.79 | <0.01 |
| Age, y | 0.01 | 0.27 | ··· | 0.65 | 0.01 | <0.01 | ··· | 0.07 |
| <35 | −0.05 | 0.43 | −0.02 | 0.75 | −0.13 | 0.04 | −0.08 | 0.24 |
| 35–45 | −0.03 | 0.55 | −0.02 | 0.79 | −0.13 | 0.02 | −0.09 | 0.11 |
| 46–60 | 0.04 | 0.50 | 0.06 | 0.54 | 0.01 | 0.93 | 0.02 | 0.78 |
| >60 | Ref. | ··· | Ref. | ··· | ··· | ··· | ||
| Gender | ||||||||
| Female | −0.18 | <0.01 | −0.17b | <0.01 | −0.24 | <0.01 | −0.21 | <0.01 |
| Male | Ref. | ··· | Ref. | ··· | Ref. | ··· | Ref. | ··· |
| Race/ethnicity | 0.19 | 0.67 | <0.01 | 0.06 | ||||
| Asian | −0.05 | 0.25 | −0.05 | 0.42 | −0.10 | 0.01 | −0.07 | 0.11 |
| Other | −0.10 | 0.12 | −0.02 | 0.58 | −0.17 | <0.01 | −0.13 | 0.04 |
| White | Ref. | ··· | ··· | ··· | Ref. | ··· | Ref. | ··· |
| Years in practicec | 0.29 | ··· | <0.01 | |||||
| 0–5 | −0.07 | 0.19 | −0.02 | ··· | −0.19 | <0.01 | ··· | ··· |
| 6–15 | −0.04 | 0.43 | 0.003 | ··· | −0.13 | <0.01 | ··· | ··· |
| 16–24 | 0.03 | 0.59 | 0.04 | ··· | −0.08 | 0.18 | ··· | ··· |
| ≥25 | Ref. | ··· | ··· | ··· | Ref. | ··· | Ref. | ··· |
| Cardiology specialty | ||||||||
| Invasive | 0.05 | 0.21 | 0.02 | 0.56 | −0.01 | 0.96 | −0.03 | 0.38 |
| Noninvasive | Ref. | ··· | ··· | ··· | Ref. | ··· | ··· | ··· |
IAT indicates Implicit Association Test; Ref., reference value.
A positive IAT score is associated with a higher implicit association with males and risk taking or strength, and a negative score is associated with higher implicit association with females and risk taking or strength.
Adjusted models include age, gender, race/ethnicity, and specialty.
Age and years in practice are highly correlated (P<0.0001); only age was retained in the multivariable linear regression model.
Case Responses
For a patient with symptoms suggesting CAD (part 1), the majority of cardiologists estimated the likelihood of obstructive CAD as intermediate or low in equal proportions for the male and female patients; however, respondents were less certain of their CAD estimates for the female patient (Table 3). More than 90% agreed that stress testing would be highly useful for the patient with symptoms suggestive of CAD regardless of patient gender, although a larger percentage rated angiography as highly appropriate for the male versus the female patient (19.7% versus 9.8%, P<0.01).
Table 3.
Responses to the Management Questions According to Patient Gender in Vignette
| Male Patient (n=259), % | Female Patient (n=244), % | P Value | |
|---|---|---|---|
| Part 1: patient with symptoms suggestive of CAD | |||
| Likelihood of CAD | |||
| High | 41.3 | 38.5 | 0.52 |
| Intermediate/low | 58.7 | 61.5 | |
| Certainty of estimate | |||
| High | 53.7 | 44.3 | 0.04 |
| Intermediate/low | 46.4 | 55.7 | |
| Stress test rating | |||
| High | 90.1 | 90.6 | 0.82 |
| Intermediate/low | 10.0 | 9.4 | |
| Angiography rating | |||
| High | 19.7 | 9.8 | <0.01 |
| Intermediate/low | 80.3 | 90.2 | |
| Part 2: patient with abnormal stress test | |||
| Likelihood of CAD | |||
| High | 83.0 | 79.5 | 0.31 |
| Intermediate/low | 17.0 | 20.5 | |
| Certainty of estimate | |||
| High | 86.1 | 79.1 | 0.04 |
| Intermediate/low | 13.9 | 20.9 | |
| Secondary stress test rating | |||
| High | 24.3 | 32.8 | 0.04 |
| Intermediate/low | 75.7 | 67.2 | |
| Angiography rating | |||
| High | 73.7 | 64.3 | 0.03 |
| Intermediate/low | 26.3 | 35.6 | |
CAD indicates coronary artery disease.
For the patient with an abnormal ETT and continued symptoms of chest pain despite medications (part 2), respondents rated the likelihood of CAD as high at similar rates for the male and female patients (83.0% versus 79.5%, P=0.31) but again were less certain of this estimate for the female patient (Table 3). Respondents were more likely to rate the usefulness of a secondary stress test as intermediate to low (75.7% versus 67.2%, P=0.04) and angiography as high (73.7% versus 64.3%, P=0.03) for the male versus the female patient (Table 3).
For both parts of the case, factors independently associated with a higher angiography rating included male patient gender, higher estimated likelihood of CAD, and higher certainty of this estimate (all P<0.05). Physician factors independently associated with higher angiography ratings included having a procedural specialty (interventional, cardiothoracic surgery, or electrophysiology) and fewer years in practice (all P<0.05).
Implicit Gender Bias and Case Responses
In unadjusted analysis, gender differences in angiography ratings for parts 1 and 2 of the case varied significantly by physician implicit bias (an interaction effect of patient gender and physician IAT scores). Physicians with more gender bias on risk taking (Figure 3A) or strength (Figure 3B) rated angiography as more useful for men than for women (P<0.05 for both unadjusted interactions). After adjustment for perceived likelihood of CAD and physician specialty, physicians' gender bias on risk taking remained a significant predictor of gender differences in angiography ratings in patients with symptoms suggestive of CAD (adjusted P=0.01 for interaction); however, gender bias on strength was no longer significant in patients with an abnormal stress test (adjusted P=0.12). Implicit gender bias did not significantly relate to gender differences in stress test ratings in either part of the case (all P>0.05 for interactions; data not shown).
Figure 3.
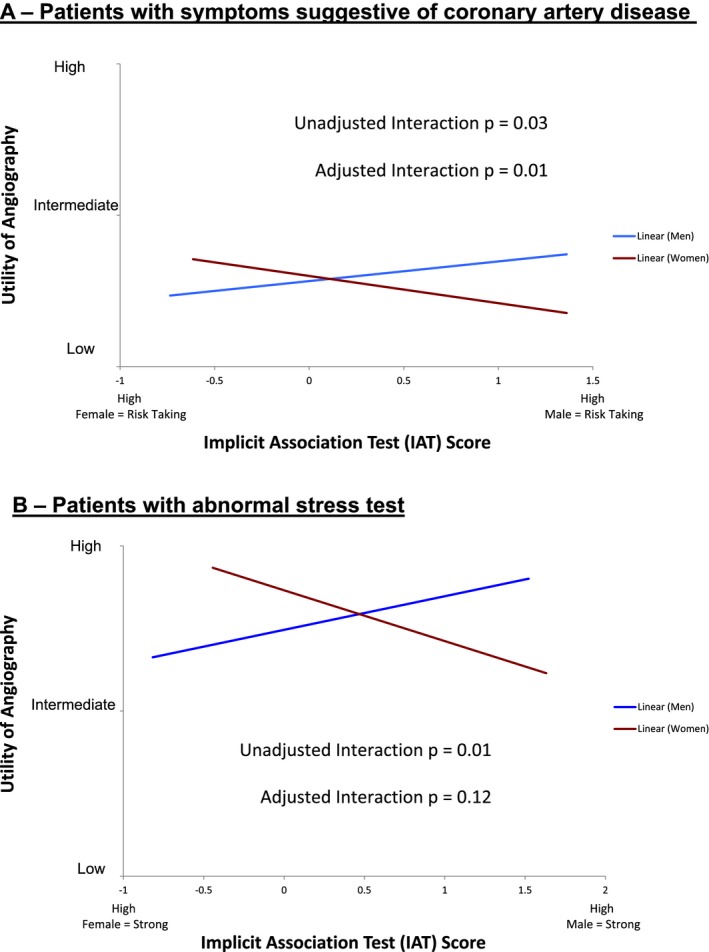
The strength of angiography rating varied according to case patient gender and physician implicit gender bias. The x‐axis represents physician gender bias based on Implicit Association Test scores, and the y‐axis represents the extent to which angiography was rated as useful for the case vignette by the physician. The relationship between gender bias and angiography rating is indicated when the case patient was male (blue line) and female (red line). In unadjusted analysis, significant interactions were seen between gender bias and case gender; those with higher implicit gender bias on risk taking (A) or strength (B) rated angiography as less useful in women than men (unadjusted P<0.05 for interaction for both). After adjustment for perceived likelihood of coronary artery disease and physician specialty, the interaction between risk‐taking bias and patient gender on angiography usefulness remained significant (adjusted P=0.01 for interaction in panel A); however, the interaction with strength bias was no longer significant (adjusted P=0.12 in panel B).
Discussion
In this survey of cardiology physicians practicing throughout the United States, most participants exhibited implicit gender bias suggesting they viewed men as stronger or more likely to take risks than women. Hypothetical female and male patients were also evaluated differently; in an identical case presentation with symptoms and a stress test suggestive of CAD, participating cardiologists were less likely to rate angiography as highly useful for a female patient compared with a male patient. Importantly, this gender difference in case management was associated with implicit gender bias: cardiologists who associated risk taking more with men than with women were more likely to view angiography as highly useful for male versus female patients. Implicit gender bias was not significantly associated with differences in angiography recommendations among patients with an abnormal ETT or in the use of stress testing. Consequently, implicit gender bias—as measured in this study—may influence some clinical decisions but not others.
To our knowledge, this study is the first to directly measure implicit gender bias among physicians and the first to relate such bias with clinical decision‐making.12 Research shows that people commonly use a person's social identify (eg, gender) as a mechanism to organize, simplify, or supplement the torrent of information that must be dealt with in everyday situations.47, 48 Implicit biases are common and operate in a relatively unintentional, automatic manner.49, 50 Our study is the first to demonstrate that >70% of the participating cardiologists associated strength and risk taking with men more than women. Prior studies have shown that the majority of physicians have implicit race/ethnicity bias at rates similar to community samples.12, 46, 51, 52, 53 Physicians may be especially vulnerable to the use of implicit biases in clinical settings characterized by time pressure, brief encounters, and the need to manage very complex situations—the type of situations in which implicit bias is more likely to be applied.17, 50 Demonstrating the presence of bias among physicians and other healthcare professionals is an important step in understanding the potential role of bias in clinical decision‐making.
Women with angina have a lower prevalence of obstructive CAD at angiography compared with men, and lower angiography referral in women may not necessarily be inappropriate.54 Similarly, it is not surprising that men were perceived as stronger or more likely to take risks than women because these perceptions align with societal stereotypes.18, 19, 20 What is unique about our findings is the demonstration that implicit gender stereotypes (bias) were related to some clinical decisions; those with the most bias that women are less likely to take risks than men were the least likely to rate angiography as useful in women. Our findings suggest that factors beyond clinical appropriateness alone play a role. The inappropriate application of prior knowledge or assumptions about differences between populations can result in “knowledge‐mediated bias.”27, 48, 55 In other words, an assumption that all women with symptoms of angina or an abnormal stress test do not have obstructive CAD or are more risk avoidant, resulting in lower angiography rates in women, could result in significant health disparities.
Our study demonstrated that implicit gender bias was associated with differences in some simulated clinical decisions but not others. Gender‐based variation in recommendations for angiography among patients with chest pain was related to implicit gender bias on risk taking. This same bias was not significantly associated with observed differences in rated usefulness of secondary stress testing or angiography after an abnormal ETT. Explanations for this heterogeneity include the possibility that gender bias may be more relevant in clinical scenarios that involve more subjectivity or higher risk procedures. In a patient with chest pain, the clinician must subjectively interpret the patient's symptoms to determine risk, whereas an ETT provides a more objective assessment of risk. It is also possible that physicians viewed proceeding directly to angiography in a patient with symptoms of CAD as a higher risk first step, rendering gender biases about the patient's risk acceptance more relevant. Nevertheless, once presented with an abnormal stress test, angiography was felt to be useful regardless of a patient's assumed risk acceptance. Gender bias may be less relevant when gender‐specific recommendations exist. A consensus statement on women and diagnostic cardiovascular testing recommends a secondary stress test after an abnormal ETT, which may explain the higher rating of secondary stress testing for women than men in our study.56 Finally, it is possible that other gender biases, beyond risk taking and strength, may contribute to disparities in care. Taken together, our findings suggest that although implicit gender bias exists, it does not explain all gender differences in the use of cardiac testing among patients being evaluated for CAD.
Another important contribution to the literature is our inclusion of cardiologists' estimated likelihood of CAD and their certainty of this estimate. Others have appropriately criticized claims of gender disparities in care when physicians' estimates of risk were not included.57 Our participants estimated the likelihood of obstructive CAD in hypothetical male and female patients similarly but felt less certain of these estimates for the female patient. Other studies have similarly shown that physician certainty of cardiac diagnoses varied by patient gender and influenced clinical decisions.58, 59 Consequently, efforts to reduce gender disparities in management may need to focus on increasing physician certainty of evaluating suspected CAD in female patients.
Our study provides evidence of the presence of physician gender bias, raising the question of whether implicit bias is modifiable.34 The first step in minimizing any potential negative effects of implicit bias is increasing awareness. Awareness of unwanted implicit stereotypes and being motivated to counteract them—or creating structures that minimize their effects—may help ensure that implicit bias does not overtly influence behavior.34, 60 Implicit bias is modifiable in experimental settings using counterstereotyping exercises; however, these methods have not been applied in a clinical setting.61 Furthermore, changing bias among all healthcare professionals is an ambitious task. Efforts to ensure equity in care for women and men may be better spent by improving the evidence base, particularly for women, who are historically underrepresented in trials and for whom there is greater clinician uncertainty about management. Finally, using decision support to guide management based on evidence appropriate to a patient's objective clinical data rather than clinicians' implicit stereotypes may reduce some disparities in care related to bias.
Certain limitations should be considered in the interpretation of our findings. First, we used case scenarios and not real patient encounters to measure gender differences in clinical decisions. Although decision‐making in clinical vignettes may not match in‐person encounters, vignettes have the benefit of eliminating the influence of variation in patient behavior, preferences, and patient–provider interaction.25 Furthermore, our study is the first to directly measure physician gender bias instead of inferring it based on observed gender differences in care, as has been done in prior work. Future studies should evaluate whether measured gender bias is associated with clinical decisions in actual patient encounters. Another limitation of our study is the low response rate and our convenience‐sampling approach. Our respondents may not reflect the rates of gender bias among a larger population of practicing cardiologists in the United States or internationally; however, response bias would not be expected to influence the interaction between physician gender bias and patient gender in predicting decision‐making. In other words, we have no a priori reason to suspect that factors related to nonresponse would differentially affect this relationship (ie, those less likely to respond would be more or less likely to be influenced by gender bias). Furthermore, our respondents represent >500 cardiologists practicing throughout the United States, and their demographics are similar to those of members of large cardiology organizations.38, 39, 40, 41 Finally, compared with surveys among the general population, physician surveys have lower average response rates, and response bias has been shown to be minimal.62, 63, 64
Conclusions
In summary, we conducted the first study to demonstrate the existence of implicit gender bias among cardiology physicians. Our findings also suggest that hypothetical women and men with suspected CAD are managed differently and that implicit gender bias is associated with some of these differences. Consequently, although implicit gender bias exists, it does not appear to explain all gender differences in the use of cardiac tests among patients being evaluated for CAD. Additional research is needed to better understand why women and men may receive different care when they have similar clinical characteristics.
Sources of Funding
This study was supported by award number K08 HL103776 from the National Heart, Lung, and Blood Institute. Drs Daugherty, Blair and Havranek are currently supported by R01 HL133343 from the National Heart, Lung, and Blood Institute and 15SFDRN24470027 from the American Heart Association. The views expressed in this article represent those of the authors, and do not necessarily represent the official views of the National Heart, Lung and Blood Institute or the American Heart Association. Dr Daugherty and Ms Furniss had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures
Dr Masoudi is the Chief Science Officer for the NCDR. All other authors report no conflicts in relation to this article.
Supporting information
Table S1. Cardiology Physician Participant Characteristics of Those Included Versus Excluded for Erroneous Implicit Association Test Responses
Table S2. Terms for Gender Bias Implicit Association Tests
Table S3. Case Vignettes
(J Am Heart Assoc. 2017;6:e006872 DOI: 10.1161/JAHA.117.006872.)29187391
An earlier version of this article was presented as a poster at the American Heart Association Quality of Care and Outcomes Research Conference, June 2—4, 2014, in Baltimore, MD and at the American Heart Association Scientific Sessions, November 7—11, 2015, in Orlando, FL.
References
- 1. Tobin JN, Wasserthiel‐Smoller S, Wexler JP, Steingart RM, Budner N, Lense L. Sex bias in considering coronary bypass surgery. Ann Intern Med. 1987;107:19–25. [DOI] [PubMed] [Google Scholar]
- 2. Steingart R, Packer M, Hamm P, Coglianese M, Gersh B, Geltman E, Sollano J, Katz S, Moye L, Basta L, Lewis S, Gottlieb S, Bernstein V, McEwan P, Jacobson K, Brown E, Kukin M, Kantrowitz N, Pfeffer MA. Sex differences in the management of coronary artery disease. Survival and Ventricular Enlargement Investigators. N Engl J Med. 1991;325:226–230. [DOI] [PubMed] [Google Scholar]
- 3. Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–225. [DOI] [PubMed] [Google Scholar]
- 4. Shaw LJ, Miller DD, Romeis JC, Kargl D, Younis LT, Chaitman BR. Gender differences in the noninvasive evaluation and management of patients with suspected coronary artery disease. Ann Intern Med. 1994;120:559–566. [DOI] [PubMed] [Google Scholar]
- 5. Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, Brogan JGX, Boden WE, Roe MT. Gender disparities in the diagnosis and treatment of non‐ST‐segment elevation acute coronary syndromes: large‐scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. [DOI] [PubMed] [Google Scholar]
- 6. Miller TD, Roger VL, Hodge DO, Hopfenspirger MR, Bailey KR, Gibbons RJ. Gender differences and temporal trends in clinical characteristics, stress test results and use of invasive procedures in patients undergoing evaluation for coronary artery disease. J Am Coll Cardiol. 2001;38:690–697. [DOI] [PubMed] [Google Scholar]
- 7. Daugherty SL, Peterson PN, Magid DJ, Ho PM, Bondy J, Hokanson JE, Ross CA, Rumsfeld JS, Masoudi FA. The relationship between gender and clinical management after exercise stress testing. Am Heart J. 2008;156:301–307. [DOI] [PubMed] [Google Scholar]
- 8. Chang AM, Mumma B, Sease KL, Robey JL, Shofer FS, Hollander JE. Gender bias in cardiovascular testing persists after adjustment for presenting characteristics and cardiac risk. Acad Emerg Med. 2007;14:599–605. [DOI] [PubMed] [Google Scholar]
- 9. Daugherty SL, Magid DJ. Do sex differences exist in patient preferences for cardiovascular testing? Ann Emerg Med. 2011;57:561–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heidenreich PA, Shlipak MG, Geppert J, McClellan M. Racial and sex differences in refusal of coronary angiography. Am J Med. 2002;113:200–207. [DOI] [PubMed] [Google Scholar]
- 11. Smedley BD, Stith AY, Nelson AR. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Board on Health Sciences Policy, and Institute of Medicine, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 12. FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rathore SS, Krumholz HM. Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med. 2004;141:635–638. [DOI] [PubMed] [Google Scholar]
- 14. Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Aff (Millwood). 2008;27:374–382. [DOI] [PubMed] [Google Scholar]
- 15. Kilbourne AM, Switzer G, Hyman K, Crowley‐Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96:2113–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. J Health Econ. 2003;22:89–116. [DOI] [PubMed] [Google Scholar]
- 17. Blair I. Implicit stereotypes and prejudice In: Moskowitz GB, ed. Cognitive Social Psychology: The Princeton Symposium on the Legacy and Future of Social Cognition. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2001:359–374. [Google Scholar]
- 18. Lopez‐Saez M, Morales JF, Lisbona A. Evolution of gender stereotypes in Spain: traits and roles. Span J Psychol. 2008;11:609–617. [DOI] [PubMed] [Google Scholar]
- 19. Eagly AH, Steffen VJ. Gender stereotypes stem from the distribution of women and men into social roles. J Pers Soc Psychol. 1984;46:735–754. [Google Scholar]
- 20. Rudman LA, Glick P. Prescriptive gender stereotypes and backlash toward agentic women. J Soc Issues. 2001;57:743. [Google Scholar]
- 21. Eagly AH, Mladinic A. Gender stereotypes and attitudes toward women and men. Pers Soc Psychol Bull. 1989;15:543–558. [Google Scholar]
- 22. Andersson J, Salander P, Hamberg K. Using patients' narratives to reveal gender stereotypes among medical students. Acad Med. 2013;88:1015–1021. [DOI] [PubMed] [Google Scholar]
- 23. Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self‐esteem, and stereotypes. Psychol Rev. 1995;102:4–27. [DOI] [PubMed] [Google Scholar]
- 24. Abuful A, Gidron Y, Henkin Y. Physicians’ attitudes toward preventive therapy for coronary artery disease: is there a gender bias? Clin Cardiol. 2005;28:389–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ, Ayers W. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. [DOI] [PubMed] [Google Scholar]
- 26. Hamberg K, Risberg G, Johansson EE, Westman G. Gender bias in physicians' management of neck pain: a study of the answers in a Swedish national examination. J Womens Health Gend Based Med. 2002;11:653–666. [DOI] [PubMed] [Google Scholar]
- 27. Hamberg K. Gender bias in medicine. Womens Health (Lond). 2008;4:237–243. [DOI] [PubMed] [Google Scholar]
- 28. Green A, Carney D, Pallin D, Ngo L, Raymond K, Iezzoni L, Banaji M. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85:197–216. [DOI] [PubMed] [Google Scholar]
- 30. Nosek BA, Greenwald AG, Banaji MR. Understanding and using the implicit association test: II. Method variables and construct validity. Pers Soc Psychol Bull. 2005;31:166–180. [DOI] [PubMed] [Google Scholar]
- 31. Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74:1464–1480. [DOI] [PubMed] [Google Scholar]
- 32. Lane K, Banaji M, Nosek B, Greenwald A. Understanding and using the implicit association test: IV: what we know (so far) about the method In: Schwarz N, Wittenbrink B, ed. Implicit Measures of Attitudes. New York, NY: Guilford Press; 2007:59–102. [Google Scholar]
- 33. Cunningham WA, Preacher KJ, Banaji MR. Implicit attitude measures: consistency, stability, and convergent validity. Psychol Sci. 2001;12:163–170. [DOI] [PubMed] [Google Scholar]
- 34. Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: a narrative review. Group Process Intergroup Relat. 2016;19:528–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nosek BA, Banaji MR, Greenwald AG. Harvesting implicit group attitudes and beliefs from a demonstration web site. Group Dyn. 2002;6:101–115. [Google Scholar]
- 36. Smyth FL, Nosek BA. On the gender‐science stereotypes held by scientists: explicit accord with gender‐ratios, implicit accord with scientific identity. Front Psychol. 2015;6:415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Research Now . 2014. Available at: https://www.researchnow.com/. Accessed January 8, 2014.
- 38. American College of Cardiology . 2015. Available at: http://www.acc.org/membership/about-membership/member-profile. Accessed November 25, 2015.
- 39. Poppas A, Cummings J, Dorbala S, Douglas PS, Foster E, Limacher MC. Survey results: a decade of change in professional life in cardiology: a 2008 report of the ACC women in cardiology council. J Am Coll Cardiol. 2008;52:2215–2226. [DOI] [PubMed] [Google Scholar]
- 40. Hlatky MA, Shaw LJ. Women in cardiology: very few, different work, different pay. J Am Coll Cardiol. 2016;67:542–544. [DOI] [PubMed] [Google Scholar]
- 41. Sanghavi M. Women in cardiology: introspection into the under‐representation. Circ Cardiovasc Qual Outcomes. 2014;7:188–190. [DOI] [PubMed] [Google Scholar]
- 42. Gibbons RJ, Balady GJ, Bricker TJ, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O'Reilly MG, Winters WL Jr, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Russell RO, Smith SC Jr; American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883–1892. [DOI] [PubMed] [Google Scholar]
- 43. Minear M, Park D. A lifespan database of adult facial stimuli. Behav Res Methods Instrum Comput. 2004;36:630–633. [DOI] [PubMed] [Google Scholar]
- 44. Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta‐analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. [DOI] [PubMed] [Google Scholar]
- 45. Forsyth B, Lessler J. Cognitive laboratory methods: a taxonomy In: Biemer PP, Groves RM, Lyberg LE, Mathiowetz NA, Sudman S. eds. Measurement Errors in Surveys. New York: Wiley & Sons; 1991:393–418. [Google Scholar]
- 46. Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swoboda S, Villegas CV, Haut ER, Bonds M, Pronovost PJ, Lipsett PA, Freischlag JA, Cornwell EE. Association of unconscious race and social class bias with vignette‐based clinical assessments by medical students. JAMA. 2011;306:942–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Macrae C, Bodenhausen G. Social cognition: categorical person perceptions. Br J Soc Psychol. 2001;92:239–255. [PubMed] [Google Scholar]
- 48. van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40:I‐140–I‐151. [DOI] [PubMed] [Google Scholar]
- 49. Dovidio JF. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol. 1997;33:510–540. [Google Scholar]
- 50. Devine P. Stereotypes and prejudice: their automatic and controlled components. J Pers Soc Psychol. 1989;56:5–18. [Google Scholar]
- 51. Cooper LA. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Blair IV. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013;103:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sabin JA, Nosek BA, Greenwald AG, Rivara FP. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Shaw LJ, Bugiardini R, Merz CNB. Women and ischemic heart disease: evolving knowledge. J Am Coll Cardiol. 2009;54:1561–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Risberg G, Johansson EE, Hamberg K. A theoretical model for analysing gender bias in medicine. Int J Equity Health. 2009;8:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mieres JH, Gulati M, Merz NB, Berman DS, Gerber TC, Hayes SN, Kramer CM, Min JK, Newby LK, Nixon JV, Srichai MB, Pellikka PA, Redberg RF, Wenger NK, Shaw LJ. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. Circulation. 2014;130:e86. [DOI] [PubMed] [Google Scholar]
- 57. Paulus JK, Shah ND, Kent DM. All else being equal, men and women are still not the same: using risk models to understand gender disparities in care. Circ Cardiovasc Qual Outcomes. 2015;8:317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lutfey KE, Link CL, Marceau LD, Grant RW, Adams A, Arber S, Siegrist J, Bonte M, von dem Knesebeck O, McKinlay JB. Diagnostic certainty as a source of medical practice variation in coronary heart disease: results from a cross‐national experiment of clinical decision making. Med Decis Making. 2009;29:606–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Maserejian NN, Link CL, Lutfey KL, Marceau LD, McKinlay JB. Disparities in physicians' interpretations of heart disease symptoms by patient gender: results of a video vignette factorial experiment. J Womens Health (Larchmt). 2009;18:1661–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social‐cognitive psychology. J Gen Intern Med. 2007;22:882–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Blair IV. The malleability of automatic stereotypes and prejudice. Pers Soc Psychol Rev. 2002;6:242–261. [Google Scholar]
- 62. Flanigan TS, McFarlane E, Cook S. Conducting survey research among physicians and other medical professionals—a review of the current literature, in Section on Survey Research Methods. A.A.f.P.O. Research, Editor. 2008.
- 63. Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jette N. Exploring physician specialist response rates to web‐based surveys. BMC Med Res Methodol. 2015;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20:61–67. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Cardiology Physician Participant Characteristics of Those Included Versus Excluded for Erroneous Implicit Association Test Responses
Table S2. Terms for Gender Bias Implicit Association Tests
Table S3. Case Vignettes


