Abstract
Background
We evaluated depression and social isolation assessed at time of waitlisting as predictors of survival in heart transplant (HTx) recipients.
Methods and Results
Between 2005 and 2006, 318 adult HTx candidates were enrolled in the Waiting for a New Heart Study, and 164 received transplantation. Patients were followed until February 2013. Psychosocial characteristics were assessed by questionnaires. Eurotransplant provided medical data at waitlisting, transplantation dates, and donor characteristics; hospitals reported medical data at HTx and date of death after HTx. During a median follow‐up of 70 months (<1–93 months post‐HTx), 56 (38%) of 148 transplanted patients with complete data died. Depression scores were unrelated to social isolation, and neither correlated with disease severity. Higher depression scores increased the risk of dying (hazard ratio=1.07, 95% confidence interval, 1.01, 1.15, P=0.032), which was moderated by social isolation scores (significant interaction term; hazard ratio = 0.985, 95% confidence interval, 0.973, 0.998; P=0.022). These findings were maintained in multivariate models controlling for covariates (P values 0.020–0.039). Actuarial 1‐year/5‐year survival was best for patients with low depression who were not socially isolated at waitlisting (86% after 1 year, 79% after 5 years). Survival of those who were either depressed, or socially isolated or both, was lower, especially 5 years posttransplant (56%, 60%, and 62%, respectively).
Conclusions
Low depression in conjunction with social integration at time of waitlisting is related to enhanced chances for survival after HTx. Both factors should be considered for inclusion in standardized assessments and interventions for HTx candidates.
Keywords: depression; heart failure; psychology and behavior; social isolation, social contacts; survival analysis; transplantation
Subject Categories: Epidemiology, Transplantation, Risk Factors, Mortality/Survival
Clinical Perspective
What Is New?
Depression and social isolation assessed at time of waitlisting were associated with reduced survival over 8 years after heart transplantation.
Patients without depressive symptoms who were not socially isolated at time of listing had the best survival rates after transplantation compared with groups with either 1 of these 2 factors or both.
The association of depression and social isolation with survival was independent of known demographic and medical covariates.
What Are the Clinical Implications?
Evaluation of patients for heart transplantation may benefit from including systematic assessments of depression and social contacts.
Psychosocial interventions to accompany medical efforts to stabilize patients at risk for health decline may be warranted early in the course of transplantation.
Survival after adult heart transplantation (HTx) has increased during the past decades.1 According to the registry of the International Society for Heart and Lung Transplantation (ISHLT), 1‐year survival amounted to 84.5%, and 5‐year survival to 72.5% in 2014,2 with about 10% lower survival rates reported in Europe.3 Several models have been developed to predict survival after HTx based on pretransplant assessments, taking into account up to 43 demographic and medical recipient and donor variables,4, 5, 6 yet excluding psychosocial patient characteristics. The importance of the latter variables has been acknowledged by the ISHLT listing criteria for HTx, which focus primarily on screening for lack of social support in an effort to reduce the risk of adverse outcomes (Class I recommendation, Level of Evidence C).7
There is some empirical evidence that depression and social isolation (ie, limited number of social contacts, being unmarried and/or living alone) are indeed linked to reduced survival in studies of patients with heart failure.8, 9 Studies in the field of HTx also suggest that psychosocial attributes contribute to both pre‐ and posttransplant outcomes. In the multisite prospective Waiting for a New Heart Study that enrolled 318 patients newly registered for HTx, we have shown that depressive symptoms and social isolation were not only prevalent among HTx candidates at time of waitlisting,10, 11 but also contributed to pre‐transplant outcomes such as reduced chances for delisting because of clinical improvement, reduced event‐free survival, higher probabilities of mechanical circulatory support device implantation, and HTx in high‐urgency status.11, 12, 13, 14 Most importantly, of several psychosocial variables that were evaluated including anxiety, only depression and social isolation were consistently associated with the abovementioned waiting list outcomes at follow‐ups of varying length. Depression and social factors also appear to play a role in post‐HTx mortality.15, 16, 17 However, in these studies of transplant recipients15, 16, 17 it is unclear whether these characteristics were already present before surgery, as their assessment took place post‐HTx. Therefore, these studies cannot provide any evidence whether depression and social factors present at time of waitlisting impact transplant outcomes and whether systematic assessment of these patient characteristics should already be part of the pretransplant evaluation. A recent meta‐analysis of heart, liver, kidney, lung, and other solid organ transplant patients found depression in general to be related to adverse posttransplant outcomes.18 However, this meta‐analysis included only 4 (smaller single‐center) studies of HTx patients with a pretransplant assessment of depression, which have reported conflicting findings.19, 20, 21, 22 Social isolation was not evaluated in these studies. Thus, the prospective role of depressive symptoms and social isolation assessed at time of waitlisting for long‐term survival of HTx recipients remains elusive.
Using data from the extended follow‐up of patients in the Waiting for a New Heart Study covering the post‐HTx period until February 2013 (an observation period of almost 8 years) allows for a test of the hypothesis that higher scores of depressive symptoms and social isolation at time of waitlisting contribute to reduced survival rates after HTx regardless of diagnosis. The large number of HTx recipients also allows for statistical control of other factors known to influence post‐HTx survival.
Methods
Procedure and Participants
The Waiting for a New Heart Study is a multisite prospective cohort study of patients newly listed for HTx in 17 hospitals (16 in Germany, 1 in Austria) between April 2005 and December 2006, carried out in collaboration with Eurotransplant International Foundation. It aims at identifying psychosocial and behavioral predictors (assessed at time of waitlisting) of pre‐ and posttransplant outcomes.
Analyses at varying follow‐ups during the waiting period found that depression and social isolation played a consistent role for reduced chances of delisting because of clinical improvement, and for increased risks for implantation of a mechanical assist device, transplantation in high‐urgency status, and for event‐free survival during waiting time.11, 12, 13, 14, 23 The present report is the first to examine these 2 patient characteristics (depression and social isolation) as predictors of post‐HTx survival in participants who received a transplant between study start and February 2013. Study procedures have been described previously.10, 11 Exclusion criteria were aged <18 years, being listed for combined heart–lung transplantation, retransplantation, not being fluent in German, and too severely ill to participate. Of 318 participants,10 164 patients had received a transplant by the end of follow‐up. Sixteen patients were lost to follow‐up because of discontinuation of participation by 1 hospital. Data from 148 recipients were analyzed (Figure 1). All participants gave written informed consent. The study was approved by the ethics committee of the Landesärztekammer Rheinland‐Pfalz and by local ethics committees, and carried out in accordance with the Declaration of Helsinki.
Figure 1.
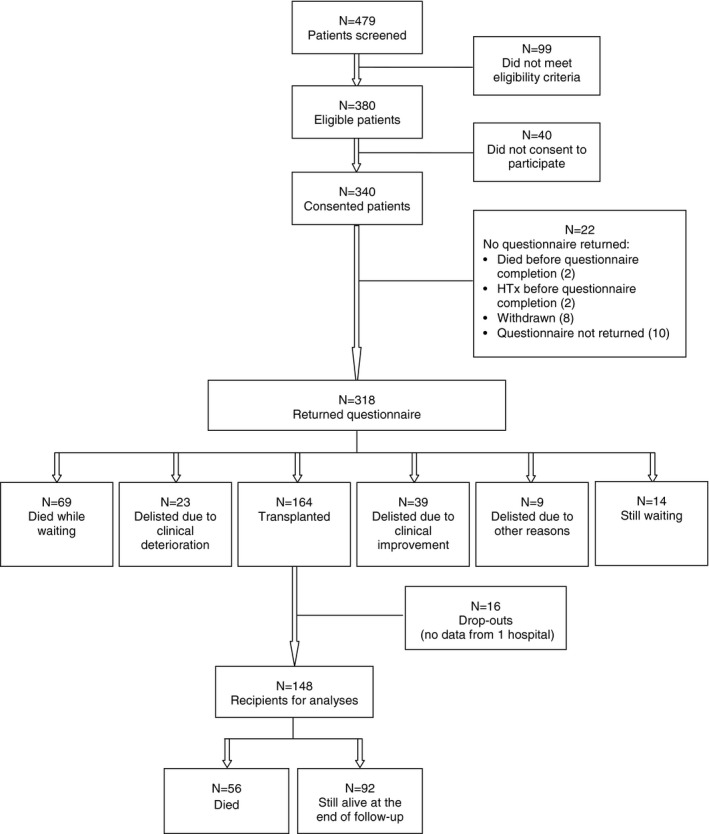
Flow chart illustrating participants and their outcomes during the course of the prospective Waiting for a New Heart Study. HTx indicates heart transplantation.
Measures
Outcome was time until death after HTx in months since transplantation with date of the event provided by hospitals. Transplantation status (high‐urgency versus elective) was documented, as was waiting time in days, rescaled that a 1‐unit increase refers to 100 days.
Nonmedical patient characteristics were self‐reported at time of listing. Depression was measured via the Hospital Anxiety and Depression Scale,24 with higher scores (possible range 0–21) indicating more depressive symptoms. Because Hospital Anxiety and Depression Scale anxiety correlated significantly with depression (r[148]=0.58) and was unrelated to waiting‐list outcomes23, it is not evaluated here. The number of social contacts was assessed asking for “the number of relatives and close friends you have contact with during 1 month.”25 For survival analyses, this score was reversed by multiplication with −1, so that a higher score reflected more social isolation. In order to increase statistical power in this reduced sample of patients who actually received a transplant, depression and social isolation were used as continuous scores. Other self‐reported items reflective of social isolation were marital status and whether patients lived alone (yes/no). The full psychosocial assessment at time of listing is described elsewhere.10
Medical parameters at time of listing were provided by Eurotransplant (for details see Table 1). These included parameters to compute the Heart Failure Survival Score, 26 cardiac index, creatinine, dates of HTx, and donor characteristics (age, sex, weight, and height). Hospitals provided recipient data at time of transplantation, including weight, height, diabetes mellitus, creatinine, pulmonary vascular resistance, panel reactive antibody level, devices before HTx, intensive care unit (yes/no), cold ischemic time, and immunosuppressive medication. Body mass index (BMI) was calculated (kg/m2).
Table 1.
Demographic, Medical, and Psychosocial Characteristics in 148 Heart Transplant Recipients
| Mean (SD) or n (%) | MD | IQR | |
|---|---|---|---|
| Demographic and anthropometric characteristics at time of listing | |||
| Age, y | 52.2 (11.7) | 54 | 45 to 62 |
| Male sex | 121 (81.8%) | ||
| Unmarried | 58 (39.2%) | ||
| Living alone | 28 (18.9%) | ||
| Currently working | 10 (6.8%) | ||
| Education ≥9 y | 66 (44.6%) | ||
| Inpatient | 65 (43.9%) | ||
| BMI, kg/m2 | 25.2 (3.9) | ||
| Medical characteristics at time of listing | |||
| Ischemic diagnosis | 45 (30.4%) | ||
| HFSS | 7.8 (1.0) | 7.7 | 7.2 to 8.3 |
| Cardiac index ([L/min] per m²) | 2 (0.5) | 1.9 | 1.6 to 2.3 |
| PCWP, mm Hg | 20.9 (8.1) | 20 | 15 to 25.8 |
| Creatinine, mg/dL | 1.4 (0.5) | 1.3 | 1.1 to 1.6 |
| Pulmonary vascular resistance (n=93) (dyn×s×cm−5) | 215.2 (147.8) | 180 | 117.5 to 255.5 |
| Smoking history | |||
| Current/former smoker | 104 (70.0%) | ||
| Never smoker | 44 (29.7%) | ||
| Comorbidities | |||
| Previous heart surgery (n=126) | 40 (27.0%) | ||
| Atrial fibrillation (n=109) | 21 (14.2%) | ||
| ICD (n=118) | 81 (54.7%) | ||
| Psychosocial characteristics at time of listing | |||
| HADS Depression score (0–21) | 7.5 (4.0) | 8 | 5 to 10 |
| HADS Depression score ≥9 | 59 (39.9%) | ||
| Number of social contacts | 8.9 (7.1) | 6.5 | 4 to 10 |
| Psychological counseling | 62 (41.9%) | ||
| Characteristics at time of HTx | |||
| Recipient age | 53 (11.8) | 55 | 46 to 63 |
| Recipient BMI (kg/m2) (n=146) | 24.9 (3.8) | ||
| Donor age (y) | 40.9 (13.0) | 43 | 32 to 48 |
| Donor male sex | 89 (60.1%) | ||
| Donor BMI, kg/m2 | 25.0 (3.7) | ||
| Creatinine (mg/dL) (n=146) | 1.6 (1.3) | 1.4 | 1.1 to 1.7 |
| Panel reactive antibody level (0) (n=132) | 132 (100.0%) | ||
| Central venous pressure (mm Hg) (n=30) | 14.9 (5.6) | 13 | 10 to 19.3 |
| Pulmonary vascular resistance (n=132) (dyn×s×cm−5) | 200.8 (90.9) | 184 | 139 to 257 |
| Diabetes mellitus | 34 (23.0%) | ||
| VAD | 11 (7.4%) | ||
| IABP | 4 (2.7%) | ||
| Intensive care unit (n=144) | 70 (47.3%) | ||
| Ventilation (n=146) | 8 (5.4%) | ||
| Cold ischemic time (min), mean (SD) (n=140) | 190.4 (60.1) | ||
| Waiting time (d) | 339 (461.5) | 142 | 57.5 to 482 |
N=148, if not indicated otherwise. BMI indicates body mass index; HADS, Hospital Anxiety and Depression Scale; HFSS, Heart Failure Survival Score; Higher scores denote a lower mortality risk; HTx, heart transplantation; IABP, intraaortic balloon pump; ICD, intracardiac cardioverter‐defibrillator; IQR, interquartile range in case of no normal distribution; MD, median; PCWP, pulmonary capillary wedge pressure; VAD, ventricular assist device.
Demographic variables including age, sex, currently working (yes/no), and education (>9 years of education [yes/no]), together with smoking status (for details see 27) and receiving any psychological counseling (yes/no) were assessed at time of listing. Age at HTx was computed for survival analyses.
Data Analyses
Analyses were conducted using SPSS 22.0 (SPSS Inc, Chicago, IL). For continuous medical variables with <30% missing, sample medians were used, according to Eurotransplant procedures.11 Otherwise, observations were considered missing (Table 1). Descriptive statistics are presented in absolute numbers and percentages for categorical variables, means, and SD for normally distributed continuous variables, and medians and interquartile ranges for not normally distributed variables, respectively. Pearson correlations of depression scores and number of social contacts (reverse scored) with indicators of disease severity at time of listing were computed.
To identify relevant demographic and medical predictors for post‐HTx mortality (time until death in months), univariate Cox proportional hazards analyses were conducted. P values derived from reductions in the −2 Log Likelihood expressed as change of χ2 are reported.28 Associations of these variables with the exposure variables “depression” and “social isolation” were examined. In addition, relationships among variables associated with time until death were examined to identify redundant predictors. Interrelationships among number of social contacts, marital status, and living alone were also inspected. To evaluate depressive symptoms and social isolation as predictors for post‐HTx survival, Cox proportional hazards regression was applied to test univariate and multivariate associations with time until death. Continuous scores were used to avoid loss of power associated with dichotomization. Four multivariate models were built. First, centered depression and social isolation scores were entered, followed by their interaction term. This procedure was repeated, controlling for age and sex of recipient and donor. Additional medical covariates significantly associated with death in univariate analyses were also entered. Finally, to ensure that the results were not affected by overfitting, a model including only statistically significant predictors was run.
To further explore a significant interaction term of depression and social isolation scores, the associations of depression scores with time until death in patients at the lower and at the upper 10th percentile of social isolation were examined. To do this, social isolation was first rescaled such that the value 0 represented very low social isolation (ie, 20 social contacts per month), and secondly, that the value 0 represented high social isolation (ie, 3 social contacts per month). In addition, findings were illustrated by using dichotomous variables (Hospital Anxiety and Depression Scale‐D ≥9 and median split of social isolation) to plot Kaplan–Meier survival curves for patients not depressed/not socially isolated, not depressed/isolated, depressed/not isolated, and depressed/isolated. All statistical tests were 2‐tailed with the significance level at P<0.05.
Results
Baseline Findings
Characteristics of study participants are shown in Table 1. The 16 patients lost to follow‐up did not differ from the 148 recipients included in the analyses in terms of demographic and psychosocial characteristics, BMI, or medical parameters assessed at time of listing, except for being more likely to be outpatients (87.5% versus 56.1%, P=0.016). Fifteen patients (10.1%) out of 129 patients, for whom these data had been documented, had received antidepressants at baseline. Depressive symptoms and social isolation scores were not significantly correlated with indicators of disease severity at time of listing (Table 2), except for 2 small associations of social isolation scores with the Heart Failure Survival Score (r=−0.16) and with the cardiac index (r=0.17). Depressive symptoms and social isolation were uncorrelated, r(148)=0.06, P=0.44. Married and unmarried patients reported comparable numbers of social contacts (M=9.4, SD=8.8, versus M=8.6, SD=5.9, t[146]=0.70, P=0.48). The same was observed for patients living alone compared with those living with others (M=7.2, SD=6.6, versus M=9.3, SD=7.2, t[146]=−1.4, P=0.17).
Table 2.
Correlations of Depressive Symptoms and Social Isolation Assessed at Time of Listing With Indicators of Disease Severity at Time of Listing
| Variable | HADS Depression Score | Social Isolation |
|---|---|---|
| Ischemic diagnosisa , b | 0.04 | 0.08 |
| HFSS | −0.004 | −0.16c |
| Cardiac index, L/min per m2 | −0.03 | 0.17c |
| PCWP, mm Hg | 0.13 | −0.03 |
| Creatinine, mg/dL | 0.04 | 0.03 |
| PVR, dyn×s×cm−5 | 0.00 | −0.07 |
N=148. HADS indicates Hospital Anxiety and Depression Scale; HFSS, Heart Failure Survival Score; higher scores denote a reduced risk; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance.
Included in the Heart Failure Survival Score.
P value of Pearson correlation identical to P value derived from t test (t[146]=−0.54 and −0.94, respectively].
P<0.05.
Outcomes After Transplantation
Of the 148 HTx recipients, 107 patients (72%) had received HTx while listed in Eurotransplant high‐urgency status. Patients transplanted in high‐urgency status and those transplanted electively did not differ in their baseline depressive symptom (t[146]=−0.83, P=0.41) or social isolation scores (t[146]=1.38, P=0.17).
During a median follow‐up of 70 months after HTx (range <1–93 months), 56 (38%) recipients died. One‐year actuarial survival for this sample was 75% and 5‐year survival was 66%. In univariate analyses, a higher recipient BMI at time of listing, former or current smoking, ischemic diagnosis, longer waiting time, higher donor age, higher pulmonary vascular resistance, and stay in intensive care unit at time of transplant were each significantly associated with an increased risk of death (Table 3). None of the medications assessed at baseline was associated with survival (data not shown; all P values >0.12). Higher depression scores at time of listing predicted death (Table 3; hazard ratio [HR]=1.07, 95% confidence interval [CI] 1.01–1.15; P=0.032), but social isolation by itself did not (Table 3; HR=1.03, 95% CI, 0.98–1.07; P=0.19). Neither being unmarried nor living alone was associated with death (both P values >0.71).
Table 3.
Univariate Associations of Patient, Donor, and Transplantation Characteristics With Time Until Death in 148 Heart Transplant Recipients
| Variable | HR | 95% CI | P Value |
|---|---|---|---|
| Demographic characteristics | |||
| Age at HTx, y | 1.02 | 0.99–1.04 | 0.199 |
| Male sex | 1.47 | 0.70–3.11 | 0.292 |
| Unmarried | 0.90 | 0.53–1.55 | 0.711 |
| Living alone | 0.90 | 0.46–1.79 | 0.767 |
| Education ≤9 y | 0.97 | 0.57–1.63 | 0.893 |
| Former or current smoking | 1.91 | 0.99–3.69 | 0.041 |
| Donor characteristics | |||
| Donor age, y | 1.04 | 1.01–1.06 | 0.002 |
| Donor male sex | 0.76 | 0.45–1.28 | 0.302 |
| Donor BMI, kg/m2 | 1.04 | 0.97–1.11 | 0.282 |
| Medical recipient characteristics at time of listing | |||
| BMI, kg/m2 | 1.09 | 1.02–1.17 | 0.015 |
| Ischemic diagnosis | 2.00 | 1.18–3.39 | 0.012 |
| HFSS | 0.93 | 0.71–1.23 | 0.623 |
| Creatinine, mg/dL | 1.49 | 0.93–2.39 | 0.114 |
| PCWP, mm Hg | 1.00 | 0.96–1.03 | 0.833 |
| Cardiac index, L/min per m2 | 1.11 | 0.66–1.85 | 0.705 |
| ICD (n=118) | 0.72 | 0.39–1.31 | 0.286 |
| Previous heart surgery (n=126) | 1.56 | 0.88–2.75 | 0.135 |
| Medical recipient characteristics at time of HTx | |||
| BMI at HTx (kg/m2) (n=146) | 1.08 | 1.00–1.16 | 0.045 |
| Creatinine at HTx (mg/dL) (n=146) | 0.97 | 0.79–1.20 | 0.773 |
| PVRa (dyn×s×cm−5) (n=132) | 1.03 | 1.00–1.06 | 0.088 |
| VAD support | 2.02 | 0.86–4.73 | 0.139 |
| ICU (n=144) | 2.01 | 1.15–3.51 | 0.012 |
| Intra‐aortic balloon pump | 1.28 | 0.31–5.23 | 0.745 |
| Diabetes mellitus | 1.38 | 0.77–2.46 | 0.289 |
| Ventilation (n=146) | 1.81 | 0.72–4.55 | 0.241 |
| Inotropes (n=143) | 1.38 | 0.79–2.39 | 0.251 |
| High‐urgency status | 1.26 | 0.69–2.31 | 0.447 |
| Cold ischemic time (min; n=140) | 1.00 | 0.99–1.00 | 0.752 |
| Waiting time (100 d) | 1.06 | 1.01–1.11 | 0.049 |
| Psychosocial characteristics at time of listing | |||
| Depressive symptoms (HADS‐D ≥9) | 1.62 | 0.96–2.73 | 0.075 |
| Depressive symptoms (HADS‐D; 0–21) | 1.07 | 1.01–1.15 | 0.032 |
| Social isolation | 1.03 | 0.98–1.07 | 0.187 |
| Psychological counseling | 0.86 | 0.50–1.47 | 0.570 |
BMI indicates body mass index; CI, confidence interval; HADS‐D, Hospital Anxiety and Depression Scale; HFSS, Heart Failure Survival Score; HR, hazard ratio derived from univariate Cox proportional hazards regression; HTx, heart transplantation; ICD, implanted cardioverter defibrillator; ICU, intensive care unit; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; VAD, ventricular assist device.
Representing a 10‐unit increase in PVR.
None of the above‐identified univariate predictors was significantly associated with the exposure variables depression and social isolation. However, to evaluate whether depression and social isolation and their interaction term were associated with time until death over and above known predictors of posttransplant mortality such as donor age, ischemic diagnosis, and BMI,29, 30, 31 recipient and donor age and sex, BMI at HTx, diagnosis, and waiting time were retained as covariates. Stay in intensive care unit, pulmonary vascular resistance, and smoking history were not retained in the multivariate models, as they were significantly correlated with the other major covariates in the model.
The first model tested the interaction of depressive symptoms and social isolation, controlling for their main effects (Table 4). In the second and third multivariate models controlling for demographic characteristics (model 2), and also BMI at HTx, ischemic diagnosis and waiting time (model 3), the interaction term remained significantly associated with time until death (Table 4). This association proved robust both in a model that also adjusted for transplantation status (P=0.027; data not shown) and in a model restricted to significant predictors only (df=5; Table 4). In all of these models, depression (centered at the mean) was significantly associated with time until death, with social isolation (also centered) held constant at its mean. To further explore the interaction of both variables, we examined the association of depression with survival in patients at the lower 10th percentile and at the upper 10th percentile of social isolation. Social isolation was first rescaled such that the value 0 represented very low social isolation (ie, 20 social contacts per month). Among those with low social isolation, higher depression scores remained associated with a significantly increased risk of death, even when controlling for covariates (HR=1.29, 95% CI, 1.06–1.56, P=0.011). If social isolation was high (ie, the value 0 represented only 3 social contacts per month), higher depression scores did not increase the risk (HR=0.99, 95% CI, 0.91–1.09, P=0.86), but high social isolation was associated with death (HR=1.06, 95% CI, 1.00–1.12, P=0.049).
Table 4.
Models Displaying Multivariate Associations of Psychosocial Patient Characteristics Assessed at Time of Listing With Time Until Death Post‐HTx in 148 Heart Transplant Recipients
| Variable | HR | 95% CI | χ2 (df) | P Value |
|---|---|---|---|---|
| 1. Model including psychosocial variables only | ||||
| Depressive symptoms | 1.097 | 1.024–1.175a | ||
| Social isolation | 1.048 | 0.996–1.103b | ||
| Depression×social isolation | 0.985 | 0.973–0.998a | 5.23 (1) | 0.022 |
| 2. Model controlling for demographic characteristics | ||||
| Recipient age | 1.000 | 0.974–1.026 | ||
| Recipient female sex | 0.641 | 0.286–1.440 | ||
| Donor age | 1.031 | 1.006–1.057a | ||
| Donor female sex | 1.377 | 0.765–2.478 | ||
| Depressive symptoms | 1.077 | 1.003–1.157a | ||
| Social isolation | 1.044 | 0.993–1.099b | ||
| Depression×social isolation | 0.985 | 0.973–0.998a | 5.45 (1) | 0.020 |
| 3. Model controlling for additional covariates (N = 146) | ||||
| Recipient age | 0.983 | 0.954–1.013 | ||
| Recipient female sex | 0.695 | 0.305–1.585 | ||
| Donor age | 1.033 | 1.007–1.060a | ||
| Donor female sex | 1.890 | 0.992–3.599b | ||
| Ischemic diagnosis | 1.900 | 1.044–3.460a | ||
| BMI at HTx | 1.071 | 0.989–1.160b | ||
| Waiting time (100 d) | 1.024 | 0.966–1.086 | ||
| Depressive symptoms | 1.085 | 1.007–1.169a | ||
| Social isolation | 1.056 | 1.000–1.115a | ||
| Depression×social isolation | 0.985 | 0.971–0.999a | 4.64 (1) | 0.031 |
| 4. Reduced model including only significant terms plus the main effects and the interaction term of depression and social isolation | ||||
| Donor age | 1.032 | 1.008–1.057a | ||
| Ischemic diagnosis | 1.790 | 1.052–3.046a | ||
| Depressive symptoms | 1.077 | 1.003–1.156a | ||
| Social isolation | 1.039 | 0.987–1.093 | ||
| Depression×social isolation | 0.987 | 0.974–0.9995a | 4.25 (1) | 0.039 |
Displayed are values based on centered variables of depression and social isolation. BMI indicates body mass index; CI, confidence interval; df, degrees of freedom; HR, hazard ratio; HTx, heart transplantation.
Wald test P value <0.05.
Wald test P value <0.10.
Thus, higher depression scores were associated with an increased risk of death when social isolation scores were low to average, but the combination of both factors did not augment the risk further. To further illustrate this interaction, dichotomized variables of depression (Hospital Anxiety and Depression Scale‐D cutoff) and social isolation (median split, median=−6.5) were used in a Kaplan–Meier analysis and survival curves were plotted and compared via the log rank test (Figure 2). The relative absence of both depression and social isolation provided the best survival chances, with 1‐year actuarial survival (5‐year survival) of 86% (79%), compared with only 65% (60%) in patients who were not depressed, but socially isolated, 68% (56%) in patients who were depressed and not socially isolated, and 77% (62%) in patients who were both depressed and socially isolated. Each of the latter 3 survival curves differed significantly from the curve depicting survival in patients who were not depressed and not socially isolated at time of listing (all P values <0.05).
Figure 2.
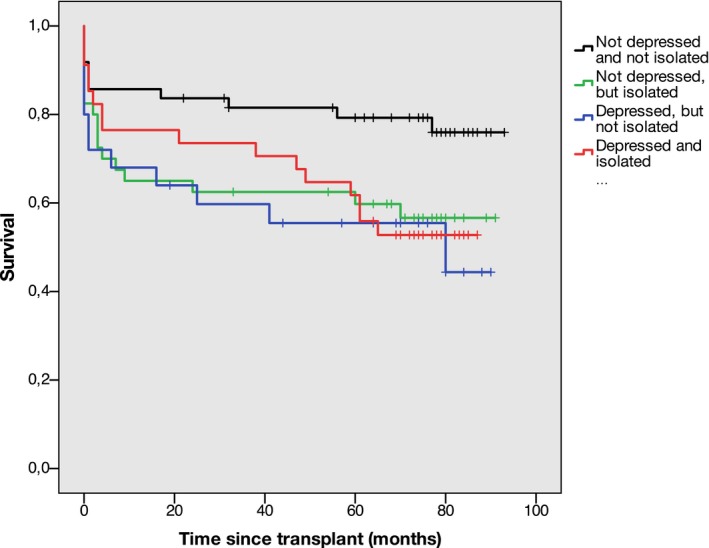
Kaplan–Meier survival plot comparing 4 groups with either low or high scores in depressive symptoms (HADS‐D <9 vs HADS‐D ≥9) and in social isolation (median split of social isolation, median=−6.5). Patients with low depression and low social isolation constitute the reference group against which each other group is compared applying the log rank test. (Overall log rank test χ2(3)=7.3, P=0.066.) HADS‐D indicates Hospital Anxiety and Depression Scale‐D.
Discussion
Our analyses of survival post‐HTx extended our findings observed for the pre‐HTx phase: depressive symptoms and social isolation present at time of waitlisting impacted not only the prognosis of patients on the HTx waiting list, but were also important for post‐HTx survival. Patients without depressive symptoms who were also not socially isolated at time of listing had the best survival rates up to 8 years after transplantation compared with groups with either 1 of these 2 factors or both. This was significant, even after adjusting for donor and recipient age and sex, and patient primary diagnosis. One‐year survival in our entire sample was 75%, which is comparable to 76% reported for Germany previously.32 Thus, a 1‐year survival of 86% in patients without depressive symptoms who were well socially integrated is considerably higher than the average 1‐year survival in Germany.
Importantly, there was no indication that patients with increased psychosocial risk had already been sicker than patients without these risk factors at time of listing. Moreover, both depressive symptoms and social isolation were unrelated to factors assessed at time of HTx that predicted posttransplant survival in this sample.
This finding suggests that survival of HTx recipients may not only be affected when depression and social isolation occur after HTx,15, 16, 17 but also when they are already present at time of waitlisting, indicating the opportunity for addressing these factors early in the course of transplantation.
As we have already shown, patients who reported depressive symptoms (in the clinically relevant range) and few social contacts at time of listing also reported more emotional stressors and stressors related to the domain of family and social contacts than patients without these psychosocial risk factors.13 These patients also had diminished chances to get delisted because of clinical improvement.11, 13 Moreover, high psychosocial risk reduced event‐free survival in the pre‐HTx phase14 and contributed independently to a declining health status, indicated by an increased probability of receiving a mechanical assist device, or to receive HTx in high‐urgency status.13 Thus, taken together, our findings from the Waiting for a New Heart Study strongly suggest that psychosocial problems present at waitlisting affect the entire course of transplantation.
While depression and social isolation are clearly related to poor prognosis in this patient population, the mechanisms linking these characteristics to poor outcomes are unclear. It has been suggested that biological and behavioral pathways appear to be involved in this relationship. For example, depression and heart failure share the dysregulation of the hypothalamus–pituitary–adrenal axis, inflammation, and oxidative stress.33 Similar mechanisms have been described for social isolation.34 Although sympathetic and parasympathetic innervation of the heart is no longer possible after transplantation, cardiac function can still be influenced by circulating catecholamine levels via activation/suppression of adrenergic receptors.35 Moreover, there is evidence for sympathetic reinnervation of the heart, at least in the long run.35, 36 From a behavioral perspective, depression and lacking social contacts have been linked to impaired self‐care and adherence to the complex regimen associated with advanced heart failure and transplantation, such as medication taking, adequate diet, physical activity, and symptom monitoring.37, 38 Future studies need to assess additional variables (eg, medication adherence and behavioral and psychological distress markers) in order to explore the mechanisms underlying the observed association of depression and social isolation with poorer outcomes.
Our findings that depressive symptoms and social isolation impair the prognosis of patients with advanced heart failure pre and post HTx underscore the need for routine screening of psychosocial problems even as early as at evaluation for waitlisting.38 Screenings should include reliable and well‐established instruments39 and, in the case of social isolation, not only rely on assessing marital status or living situation. Neither marital status nor living alone were related to survival in the present study.
Because depression and lacking social integration are modifiable behavioral risk factors, psychosocial interventions to accompany medical efforts to stabilize patients at risk for health decline are warranted early in the course of the disease and during the entire clinical course of transplantation. Treatment options such as cognitive behavior therapy have shown promise for patients with heart failure,40 but more studies are needed in this population with more advanced disease, particularly regarding means to promote social integration.
Our study has several limitations. First, it relied on self‐reports of depressive symptoms instead of a clinical diagnosis, and depressive symptoms and social contacts were assessed only at time of waitlisting. Thus, we cannot know in how many patients depression and social isolation remained stable until time of transplant. It is conceivable that depression and social isolation are particularly detrimental when present until time of transplant, as has been shown for depressive symptoms in lung transplantation.41 However, because depression tends to increase during the waiting period42 and has been shown to remain stable when present after HTx,43 the associations observed in the present study may actually be underestimated. Second, we had to exclude patients who were considered too ill to participate at waitlisting. Thus, depression of the entire population might have been even higher and might have had an even greater impact if critically ill patients had been permitted to participate. Third, social isolation was only based on self‐reports on the number of contacts with close friends/relatives during 1 month. In spite of this, this measure proved to be more important for survival than the assessment of marital status and/or living alone. Being unmarried has also been criticized as a measure of social isolation by others,44 which is supported by the fact that in our sample married and unmarried patients reported comparable numbers of social contacts. The same was true for patients living alone and those living with others. Future studies might use a more comprehensive assessment of social isolation. Fourth, our focus on depression should not preclude the role of other negative emotions (eg, anxiety) that have been shown to correlate significantly with depression.45 Also, future studies might assess additional variables, (eg, medication adherence), in order to explore the mechanisms for the observed association of depression and social isolation with poorer outcomes.
Finally, to more fully understand the relevance of depression and social relationships for pre‐ and post‐HTx survival, larger data sets, allowing for a more comprehensive evaluation of recipient and donor characteristics as well as potential mechanisms, are needed. These could also allow for investigating 3 additional issues: first, whether socioeconomic deprivation is related to these associations;46 second, whether these findings generalize to non‐European heart transplant populations; and third, whether ethnicity and sex play a role in these associations. This was not feasible in our European sample that included only 27 transplanted women. Yet, sex‐specific associations of depression, social support, and social network characteristics with outcomes have been reported previously.47, 48 Therefore, we strongly recommend adding standardized measures of psychosocial patient characteristics to the evaluation of HTx candidates and relevant databases, in order to provide sufficient data to address these questions in the future.
To conclude, this first report of the Waiting for a New Heart Study to evaluate associations between pretransplant psychosocial risk factors and post‐transplant survival corroborates the clinical relevance of depression and social contacts for clinical outcomes in heart transplant patients. The relative absence of depression in combination with social integration in patients newly listed for HTx benefits survival after transplantation, and both factors impact the entire clinical course of transplantation. Therefore, screening and early intervention for patients at risk is warranted.
Sources of Funding
This work was supported by the International Society for Heart and Lung Transplantation (Spaderna, Weidner); Alexander von Humboldt‐Foundation (Weidner); Eurotransplant International Foundation; German Academic Exchange Service (Weidner); Deutsche Forschungsgemeinschaft (DFG, grant numbers SP 945/1‐1, SP 945/1‐3, SP 945/1‐4 to Spaderna, MA 155/75‐1 to Weidner); Johannes Gutenberg‐University Mainz (Spaderna, Weidner).
Disclosures
None.
Acknowledgments
We are indebted to Lisa Grewe, Richard Mays, and Lena Rausch for their assistance in post‐HTx data acquisition and preparation of data and article. We also thank the patients of the following participating hospitals: Med. Klinik I/Kardiologie, Pneumologie, Angiologie Universitätsklinikum Aachen. Herz‐Zentrum Bad Krozingen. Herz‐ und Diabeteszentrum Nordrhein‐Westfalen Bad Oeynhausen. Herzzentrum Dresden. Med. Klinik III/Kardiologie Klinikum der Universität Frankfurt. Klinik für Thorax‐, Herz‐, und Gefäßchirurgie des Klinikums Fulda. Abteilung Kardiologie, Universitätsklinikum Gießen und Marburg, Standort Gießen. Klinik für Chirurgie der Medizinischen Universität Graz, Austria. Universitätsklinik und Poliklinik für Herz‐ und Thoraxchirurgie Halle‐Wittenberg. Universitäres Herzzentrum Hamburg GmbH. Klinik für Herz‐, Thorax‐ und Gefäßchirurgie des Universitätsklinikums Jena. Klinik und Poliklinik für Herz‐ und Thoraxchirurgie der Universität zu Köln. Klinik für Herzchirurgie des Herzzentrums Leipzig GmbH. II. Medizinische Klinik und Poliklinik Universitätsmedizin Mainz. Herzchirurgische Klinik der Universität München. Klinik und Poliklinik für Herz‐, Thorax‐ und herznahe Gefäßchirurgie der Universität Regensburg.
(J Am Heart Assoc. 2017;6:e007016 DOI: 10.1161/JAHA.117.007016.)29187384
This article was presented in part at the Annual Meeting of the International Society for Heart and Lung Transplantation (ISHLT), April 10 — 13, 2014, in San Diego, CA.
Contributor Information
Heike Spaderna, Email: spaderna@uni-trier.de.
Gerdi Weidner, Email: gweidner@sfsu.edu.
References
- 1. Wilhelm MJ. Long‐term outcome following heart transplantation: current perspective. J Thorac Dis. 2015;7:549–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lund LH, Edwards LB, Kucheryavaya AY, Benden C, Christie JD, Dipchand AI, Dobbels F, Goldfarb SB, Lewey BJ, Meiser B, Yusen RD, Stehlik J. The registry of the International Society for Heart and Lung Transplantation: thirty‐first official adult heart transplant report–2014; focus theme: retransplantation. J Heart Lung Transplant. 2014;33:996–1008. [DOI] [PubMed] [Google Scholar]
- 3. International Society for Heart and Lung Transplantation . Quarterly Data Report. 2016. Available at: https://www.ishlt.org/registries/quarterlyDataReportResults.asp?organ=HR&rptType=all&continent=32017. Accessed January 10, 2017.
- 4. Hong KN, Iribarne A, Worku B, Takayama H, Gelijns AC, Naka Y, Russo MJ. Who is the high‐risk recipient? Predicting mortality after heart transplant using pre‐transplant donor and recipient risk factors. Ann Thorac Surg. 2011;92:520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Smits JM, De Pauw M, de Vries E, Rahmel A, Meiser B, Laufer G, Zuckermann A. Donor scoring system for heart transplantation and the impact on patient survival. J Heart Lung Transplant. 2012;31:387–397. [DOI] [PubMed] [Google Scholar]
- 6. Nilsson J, Ohlsson M, Hoglund P, Ekmehag B, Koul B, Andersson B. The International Heart Transplant Survival Algorithm (IHTSA): a new model to improve organ sharing and survival. PLoS One. 2015;10:e0118644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, Baran DA, Danziger‐Isakov L, Kirklin JK, Kirk R, Kushwaha SS, Lund LH, Potena L, Ross HJ, Taylor DO, Verschuuren EA, Zuckermann A; International Society for Heart Lung Transplantation (ISHLT) Infectious Diseases Council; International Society for Heart Lung Transplantation (ISHLT) Pediatric Transplantation Council; International Society for Heart Lung Transplantation (ISHLT) Heart Failure and Transplantation Council . The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10‐year update. J Heart Lung Transplant. 2016;35:1–23. [DOI] [PubMed] [Google Scholar]
- 8. Pelle AJ, Gidron YY, Szabo BM, Denollet J. Psychological predictors of prognosis in chronic heart failure. J Card Fail. 2008;14:341–350. [DOI] [PubMed] [Google Scholar]
- 9. Chung ML, Lennie TA, Dekker RL, Wu JR, Moser DK. Depressive symptoms and poor social support have a synergistic effect on event‐free survival in patients with heart failure. Heart Lung. 2011;40:492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Spaderna H, Weidner G, Zahn D, Smits JMA. Psychological characteristics and social integration of patients with ischemic and non‐ischemic heart failure newly listed for heart transplantation: the waiting for a new heart study. Appl Psychol Health Well Being. 2009;1:188–210. [Google Scholar]
- 11. Spaderna H, Mendell NR, Zahn D, Wang Y, Kahn J, Smits JM, Weidner G. Social isolation and depression predict 12‐month outcomes in the “waiting for a new heart study”. J Heart Lung Transplant. 2010;29:247–254. [DOI] [PubMed] [Google Scholar]
- 12. Zahn D, Weidner G, Beyersmann J, Smits JMA, Deng MC, Kaczmarek I, Mehlhorn U, Reichenspurner HC, Wagner FM, Meyer S, Spaderna H. Composite risk scores and depression as predictors for competing waiting‐list outcomes: the waiting for a new heart study. Transpl Int. 2010;23:1223–1232. [DOI] [PubMed] [Google Scholar]
- 13. Spaderna H, Weidner G, Koch KC, Kaczmarek I, Wagner FM, Smits JM; for the Waiting for a New Heart Study Group . Medical and psychosocial predictors of mechanical circulatory support device implantation and competing outcomes in the waiting for a new heart study. J Heart Lung Transplant. 2012;31:16–26. [DOI] [PubMed] [Google Scholar]
- 14. Weidner G, Spaderna H. The role of the Heart Failure Survival Score and psychosocial stress in predicting event‐free survival in patients referred for heart transplantation. J Heart Lung Transplant. 2012;31:436–438. [DOI] [PubMed] [Google Scholar]
- 15. Havik OE, Sivertsen B, Relbo A, Hellesvik M, Grov I, Geiran O, Andreassen AK, Simonsen S, Gullestad L. Depressive symptoms and all‐cause mortality after heart transplantation. Transplantation. 2007;84:97–103. [DOI] [PubMed] [Google Scholar]
- 16. Sirri L, Potena L, Masetti M, Tossani E, Magelli C, Grandi S. Psychological predictors of mortality in heart transplanted patients: a prospective, 6‐year follow‐up study. Transplantation. 2010;89:879–885. [DOI] [PubMed] [Google Scholar]
- 17. Tam V, Arnaoutakis GJ, George TJ, Russell SD, Merlo CA, Conte JV, Baumgartner WA, Shah AS. Marital status improves survival after orthotopic heart transplantation. J Heart Lung Transplant. 2011;30:1389–1394. [DOI] [PubMed] [Google Scholar]
- 18. Dew MA, Rosenberger EM, Myaskovsky L, DiMartini AF, DeVito Dabbs AJ, Posluszny DM, Steel J, Switzer GE, Shellmer DA, Greenhouse JB. Depression and anxiety as risk factors for morbidity and mortality after organ transplantation: a systematic review and meta‐analysis. Transplantation. 2015;100:988–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maricle RA, Hosenpud JD, Norman DJ, Pantely GA, Cobanoglu AM, Starr A. The lack of predictive value of preoperative psychologic distress for postoperative medical outcome in heart transplant recipients. J Heart Lung Transplant. 1991;10:942–947. [PubMed] [Google Scholar]
- 20. Skotzko CE, Rudis R, Kobashigawa JA, Laks H. Psychiatric disorders and outcome following cardiac transplantation. J Heart Lung Transplant. 1999;18:952–956. [DOI] [PubMed] [Google Scholar]
- 21. Zipfel S, Schneider A, Wild B, Löwe B, Jünger J, Haass M, Sack F‐U, Bergmann G, Herzog W. Effect of depressive symptoms on survival after heart transplantation. Psychosom Med. 2002;64:740–747. [DOI] [PubMed] [Google Scholar]
- 22. Owen JE, Bonds CL, Wellisch DK. Psychiatric evaluations of heart transplant candidates: predicting post‐transplant hospitalizations, rejection episodes, and survival. Psychosomatics. 2006;47:213–222. [DOI] [PubMed] [Google Scholar]
- 23. Spaderna H, Vögele C, Barten MJ, Smits JM, Bunyamin V, Weidner G. Physical activity and depression predict event‐free survival in heart transplant candidates. Health Psychol. 2014;33:1328–1336. [DOI] [PubMed] [Google Scholar]
- 24. Herrmann‐Lingen C, Buss U, Snaith RP. HADS‐D Hospital Anxiety and Depression Scale—Deutsche Version. Ein Fragebogen zur Erfassung von Angst und Depressivität in der somatischen Medizin. 2nd ed Bern: Huber, Switzerland; 2005. [Google Scholar]
- 25. Frasure‐Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101:1919–1924. [DOI] [PubMed] [Google Scholar]
- 26. Aaronson KD, Schwartz JS, Chen T‐M, Wong K‐L, Goin JE, Mancini DM. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997;95:2660–2667. [DOI] [PubMed] [Google Scholar]
- 27. Gali K, Spaderna H, Smits JM, Bramstedt KA, Weidner G. Smoking status at time of listing for a heart transplant predicts mortality on the waiting list: a multicenter prospective observational study. Prog Transplant. 2016;26:117–121. [DOI] [PubMed] [Google Scholar]
- 28. Collett D. Modelling survival data in medical research, 2nd ed Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- 29. Aziz T, Burgess M, Rahman AN, Campbell CS, Yonan N. Cardiac transplantation for cardiomyopathy and ischemic heart disease: differences in outcome up to 10 years. J Heart Lung Transplant. 2001;20:525–533. [DOI] [PubMed] [Google Scholar]
- 30. Weiss ES, Allen JG, Patel ND, Russell SD, Baumgartner WA, Shah AS, Conte JV. The impact of donor‐recipient sex matching on survival after orthotopic heart transplantation: analysis of 18 000 transplants in the modern era. Circ Heart Fail. 2009;2:401–408. [DOI] [PubMed] [Google Scholar]
- 31. Kilic A, Weiss ES, George TJ, Arnaoutakis GJ, Yuh DD, Shah AS, Conte JV. What predicts long‐term survival after heart transplantation? An analysis of 9,400 ten‐year survivors. Ann Thorac Surg. 2011;93:699–704. [DOI] [PubMed] [Google Scholar]
- 32. Smits JM. Actual situation in Eurotransplant regarding high urgent heart transplantation. Eur J Cardiothorac Surg. 2012;42:609–611. [DOI] [PubMed] [Google Scholar]
- 33. Ghosh RK, Ball S, Prasad V, Gupta A. Depression in heart failure: intricate relationship, pathophysiology and most updated evidence of interventions from recent clinical studies. Int J Cardiol. 2016;224:170–177. [DOI] [PubMed] [Google Scholar]
- 34. Cacioppo JT, Hawley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46:39–52. [PubMed] [Google Scholar]
- 35. Ferretti G, Marconi C, Achilli G, Caspani E, Fiocchi R, Mamprin F, Gamba A, Ferrazzi P, Cerretelli P. The heart rate response to exercise and circulating catecholamines in heart transplant recipients. Pflugers Arch. 2002;443:370–376. [DOI] [PubMed] [Google Scholar]
- 36. Wilson RF, Johnson TH, Haidet GC, Kubo SH, Mianuelli M. Sympathetic reinnervation of the sinus node and exercise hemodynamics after cardiac transplantation. Circ J. 2000;101:2727–2733. [DOI] [PubMed] [Google Scholar]
- 37. Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self‐care of patients with heart failure. Ann Behav Med. 2008;35:70–79. [DOI] [PubMed] [Google Scholar]
- 38. Dobbels F, Vanhaecke J, Dupont L, Nevens F, Verleden G, Pirenne J, De Geest S. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497–1504. [DOI] [PubMed] [Google Scholar]
- 39. Celano CM, Huffman JC. Depression and cardiac disease: a review. Cardiol Rev. 2011;19:130–142. [DOI] [PubMed] [Google Scholar]
- 40. Freedland KE, Carney RM, Rich MW, Steinmeyer BC, Rubin EH. Cognitive behavior therapy for depression and self‐care in heart failure patients: a randomized clinical trial. JAMA Intern Med. 2015;175:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith PJ, Blumenthal JA, Carney RM, Freedland KE, O'Hayer CVF, Trulock EP, Martinu T, Schwartz TA, Hoffman BM, Koch GG, Davis RD, Palmer SM. Neurobehavioral functioning and survival following lung transplantation. Chest. 2014;145:604–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zipfel S, Löwe B, Paschke T, Immel B, Lange R, Zimmermann R, Herzog W, Bergmann G. Psychological distress in patients awaiting heart transplantation. J Psychosom Res. 1998;45:465–470. [DOI] [PubMed] [Google Scholar]
- 43. Dobbels F, De Geest S, Martin S, Van Cleemput J, Droogne W, Vanhaecke J. Prevalence and correlates of depression symptoms at 10 years after heart transplantation: continuous attention required. Transpl Int. 2004;17:424–431. [DOI] [PubMed] [Google Scholar]
- 44. Glass TA, Mendes de Leon CF, Seeman TE, Berkman LF. Beyond single indicators of social networks: a LISREL analysis of social ties among the elderly. Soc Sci Med. 1997;44:1503–1517. [DOI] [PubMed] [Google Scholar]
- 45. Weidner G, Spaderna H. Emotions and cardiovascular disease In: Goldman MB, Troisi R, Rexrode KM, eds. Women and Health, 2nd ed Amsterdam: Academic Press; 2013:991–1002. [Google Scholar]
- 46. Evans JD, Kaptoge S, Caleyachetty R, Di Angelantonio E, Lewis C, Parameshwar KJ, Pettit SJ. Socioeconomic deprivation and survival after heart transplantation in England: an analysis of the United Kingdom Transplant Registry. Circ Cardiovasc Qual Outcomes. 2016;9:695–703. [DOI] [PubMed] [Google Scholar]
- 47. Shye D, Mullooly JP, Freeborn DK, Pope CR. Gender differences in the relationship between social network support and mortality: a longitudinal study of an elderly cohort. Soc Sci Med. 1995;41:935–947. [DOI] [PubMed] [Google Scholar]
- 48. Leifheit‐Limson EC, Reid KJ, Kasl SV, Lin H, Jones PG, Buchanan DM, Parashar S, Peterson PN, Spertus JA, Lichtman JH. The role of social support in health status and depressive symptoms after acute myocardial infarction: evidence for a stronger relationship among women. Circ Cardiovasc Qual Outcomes. 2010;3:143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]


