Abstract
Background
Hispanic persons represent a heterogeneous and growing population of any race with origins in Mexico, the Caribbean, Central America, South America, or other Spanish‐speaking countries. Previous studies have documented variation in cardiovascular risk and outcomes among Hispanic subgroups. Few studies have investigated whether these patterns vary by nativity status among Hispanic subgroups.
Methods and Results
We used the National Center for Health Statistics mortality file to compare deaths of Hispanic (n=1 258 229) and non‐Hispanic white (n=18 149 774) adults (aged ≥25 years) from 2003 to 2012. We identified all deaths related to cardiovascular disease (CVD) and categorized them by subtype (all CVD, ischemic, or cerebrovascular) using the underlying cause of death (International Classification of Diseases, 10th Revision codes I00–I78, I20–I25, and I60–I69, respectively). Population estimates were calculated using linear interpolation from the 2000 and 2010 US censuses. CVD accounted for 31% of all deaths among Hispanic adults. Race/ethnicity and nativity status were recorded on death certificates by the funeral director using state guidelines. Nativity status was defined as foreign versus US born; 58% of Hispanic decedents were foreign born. Overall, Hispanic adults had lower age‐adjusted CVD mortality rates than non‐Hispanic white adults (296 versus 385 per 100 000). Foreign‐born Cubans, Mexicans, and Puerto Ricans had higher CVD mortality than their US‐born counterparts (rate ratio: 2.64 [95% confidence interval, 2.46–2.81], 1.17 [95% confidence interval, 1.15–1.21], and 1.91 [95% confidence interval, 1.83–1.99], respectively).
Conclusions
Mortality rates for total cardiovascular, ischemic, and cerebrovascular disease are higher among foreign‐ than US‐born Hispanic adults. These findings suggest the importance of disaggregating CVD mortality by disease subtype, Hispanic subgroup, and nativity status.
Keywords: acculturation, epidemiology, ethnicity, health disparities, Hispanic, mortality
Subject Categories: Race and Ethnicity, Epidemiology, Mortality/Survival
Clinical Perspective
What Is New?
Using national mortality data, we found that foreign‐born Hispanic adults have higher cardiovascular disease mortality rates than their US‐born counterparts, challenging the previously held notion of an “immigrant advantage.”
What Are the Clinical Implications?
Cardiologists and medical practitioners should be sensitive to the finding that foreign‐born Hispanic patients face higher cardiovascular disease mortality.
The term Hispanic refers to a heterogeneous group of individuals of any race who have origins in Mexico, the Caribbean, Central America, South America, or other Spanish‐speaking countries.1 Although Hispanic persons share the same Spanish language, their histories of migration into the United States differ, affecting patterns of settlement, social profiles, and health factors.2, 3, 4, 5, 6 Hispanic persons currently compose the largest ethnic minority group in the United States, and according to the US Census Bureau, that population is expected to increase from 55 million in 2014 to 119 million by 2060 (29% of total US population).7, 8 In 2014, ≈34% of all Hispanic persons in the United States were foreign born, down from a peak of ≈40% in the early 2000s.9 Although cardiovascular disease (CVD) is the leading cause of death for this group, when studied in aggregate, Hispanic persons experience lower age‐adjusted CVD mortality rates than non‐Hispanic white (NHW) persons.10 This lower than expected mortality, despite greater adverse CVD risk profiles and lower levels of income and education than NHWs, has been coined the “Hispanic paradox.”11, 12, 13, 14 It has been speculated that Hispanic cultural orientation results in healthier behaviors (eg, lower smoking rates) that result in better health outcomes, protecting Hispanic patients against the effects of lower socioeconomic status compared with other race/ethnic groups in the United States.15 The “healthy immigrant effect,” whereby there is selective migration among healthier immigrants to a host country, has also been cited as a possible explanation for the Hispanic mortality advantage.16
Acculturation is defined as a multidimensional process through which foreigners adapt to the customs, values, and traditions of a host country.17, 18 Of the limited available studies of diverse racial/ethnic groups, data suggest that increased acculturation is associated with greater risk of CVD.8, 19 Higher acculturation has been associated with increased psychosocial stress and deleterious health behaviors such as an unhealthy diet and less physical activity, leading to a greater prevalence of obesity, metabolic syndrome, inflammation, and subsequent CVD.20
Nativity status (foreign versus US born) is a frequently used proxy for acculturation.21 Compared with foreign‐born Hispanic persons, US‐born Hispanic persons generally have a higher prevalence of the major CVD risk factors of obesity, smoking, and hypertension,8 and increased acculturation has also been linked with a greater prevalence of subclinical CVD.22 Recent data from HCHS/SOL (Hispanic Community Health Study/Study of Latinos) showed that foreign‐born Hispanic women had more favorable cardiovascular risk profiles than US‐born Hispanic women.23 However, the majority of studies exploring the association between acculturation and CVD have been limited to studying only 1 Hispanic subgroup (mostly Mexican populations), with results then extrapolated to the broader Hispanic population, and most studies have focused on risk factor prevalence data instead of mortality.
Our previous work has documented marked heterogeneity in CVD mortality in the 3 largest Hispanic subgroups; Puerto Ricans had the highest rates of ischemic and hypertensive heart disease deaths compared with other Hispanic subgroups, whereas Mexicans had the highest rates of stroke deaths.24 Given the importance of acculturation to Hispanic cardiovascular health, our current study aims to explore CVD mortality outcomes by nativity status (US versus foreign born) among Hispanic subgroups.
Methods
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure because our data set is restricted; however, these data are publicly available through the US Census Bureau should other investigators choose to obtain them.
Study Population
The study population was comprised of comprised Hispanic and US‐born NHW (NHW) decedents aged ≥25 years in the US population from 2003 to 2012. Race/ethnicity was recorded on death certificates by the funeral director using state guidelines. Hispanic ethnic groups are classified as one of the following categories on US mortality records: Mexican, Puerto Rican, Cuban, Central or South American, and other or unknown Hispanic. Because of limited sampling for the last 2 categories, analyses were restricted to the 3 largest Hispanic subgroups that are consistently documented on the national death certificates throughout our study period, which together make up ≈80% of the Hispanic group.
We identified total decedents from the Mortality Multiple Cause‐of‐Death files of National Center for Health Statistics. We analyzed deaths specifically as all–cause mortality or as all CVD, ischemic heart disease (IHD), and cerebrovascular disease using the underlying cause of death (International Classification of Diseases, 10th Revision codes I00–I78, I20–I25, and I60–I69, respectively) from mortality records. Population data were obtained from the 2000 and 2010 US Census data, and midyear estimates were calculated using linear interpolation and extrapolation out to 2012 to generate denominator data for age‐adjusted mortality rates (AMRs). Methods for linear interpolation have been described previously.24, 25 Educational attainment was categorized as no formal education, high school or GED (General Equivalency Diploma), some college, bachelor's degree or higher, and unknown, using both 2003 and 1989 revisions because different states adopted different revisions.
Nativity Status
Several steps were taken to maintain consistent classification of nativity status across the databases. On the death certificates, decedents were classified as foreign born if they were born in any of the US territories (eg, Puerto Rico, Guam, Virgin Islands) or other foreign countries listed, as has been done in previous literature exploring nativity status and mortality.26, 27, 28 In the 2000 and 2010 censuses, however, individuals self‐identified as US born if they were born within the 50 states or the District of Columbia or “outside the United States” including Puerto Rico, the US Island Areas, or abroad of American parents. Individuals self‐identified as foreign born if they were a “naturalized US citizen” or “not a US citizen.” Consequently, we reclassified Puerto Ricans who indicated they were born in Puerto Rico/US Island Areas as foreign born, using the 2005–2009 ACS (American Community Survey) Public Use Microdata Sample (PUMS) files, for the purpose of this analysis. Sex‐specific proportions were calculated by stratifying each 5‐year age category from ages 25 to 29 through ≥85 years for both US‐ and foreign‐born Puerto Ricans, using 2005–2009 ACS PUMS data. We then used the proportion calculated in PUMS to multiply by the total death counts from the 2000 and 2010 censuses to obtain population estimates for Puerto Ricans by nativity status.
Statistical Analyses
Directly standardized, AMRs with 95% confidence intervals (CIs) by nativity status were calculated for all‐cause mortality, all CVD, IHD, and cerebrovascular disease by 5‐year age categories, adjusting to the 2000 US standard population. We analyzed the ratios of foreign‐born AMRs for causes of death of interest with respective US‐born AMRs, as the referent population. Relative rate ratios of foreign‐ versus US‐born AMRs for CVD and subtypes were calculated for Hispanic subgroups.
All analyses were performed in R Studio (version 0.99.896) and SAS (version 9.4), and statistical tests were based on 2‐sided tests with a significance level of 0.05.
The Stanford University institutional review board provided a waiver for use of these publicly available mortality and census data.
Results
Table 1 shows the demographic characteristics of decedents by nativity status among all‐Hispanic, Cuban, Mexican, Puerto Rican, and NHW adults. Foreign‐born all‐Hispanic, Cuban, and Puerto Rican adults were considerably older at the time of death compared with US‐born all‐Hispanic, Cuban, and Puerto Rican adults. Foreign‐born Hispanic adults were more likely to have lower educational attainment, with 40.5% of Cubans, 73.6% of Mexicans, and 46.7% of Puerto Ricans having less than a high school education. IHD accounted for more than half of the CVD‐related deaths among both foreign‐ and US‐born Hispanic persons (54% and 52%, respectively).
Table 1.
Characteristics for Decedents Aged ≥25 Years for All‐Hispanic, Cuban, Mexican, Puerto Rican and NHW Adults by Nativity Status, 2003–2012
| Decedent Characteristics | All Hispanic | Cuban | Mexican | Puerto Rican | NHW | ||||
|---|---|---|---|---|---|---|---|---|---|
| Foreign‐Born | US‐Born | Foreign‐Born | US‐Born | Foreign‐Born | US‐Born | Foreign‐Born/Islander | US‐Born | US‐Born | |
| Deaths, n | 730 524 | 527 705 | 125 671 | 5092 | 318 315 | 376 266 | 134 266 | 30 815 | 18 149 774 |
| Average annual population sizea, n | 147 997 414 | 101 496 757 | 8 737 069 | 2 851 745 | 81 814 249 | 64 607 669 | 11 709 019 | 11 789 098 | 1 317 541 018 |
| Absolute no. of death by cause, n (%) | |||||||||
| All CVD | 237 125 (32.5) | 153 822 (29.1) | 47 643 (37.9) | 1504 (29.5) | 96 452 (30.3) | 112 903 (30.0) | 45 314 (33.7) | 7099 (23.0) | 6 170 859 (34.0) |
| IHD | 128 729 (17.6) | 79 292 (15.0) | 28 865 (23.0) | 804 (15.8) | 47 994 (15.1) | 58 669 (15.6) | 26 744 (19.9) | 3536 (11.5) | 3 152 576 (17.4) |
| Cerebrovascular disease | 42 515 (5.8) | 28 264 (5.4) | 6411 (5.1) | 201 (3.9) | 20 678 (6.5) | 21 201 (5.6) | 6561 (4.9) | 1033 (3.4) | 1 020 008 (5.6) |
| Age at death, median (IQR) | 73 (57–83) | 70 (53–81) | 80 (71–87) | 63 (43–83) | 69 (52–82) | 71 (55–82) | 73 (61–83) | 50 (41–62) | 79 (67–87) |
| Female; % | 46.4 | 44.3 | 48.9 | 42.0 | 43.3 | 44.3 | 47.7 | 38.2 | 51.2 |
| Educational attainment, % | |||||||||
| No formal education | 55.9 | 46.6 | 40.5 | 24.4 | 73.6 | 50.7 | 46.7 | 25.9 | 23.3 |
| High school or GED completed | 24.9 | 32.4 | 31.7 | 38.7 | 13.6 | 30.1 | 37.0 | 48.0 | 43.0 |
| Some college | 7.4 | 13.5 | 8.9 | 19.9 | 5.3 | 12.6 | 7.2 | 16.5 | 16.0 |
| Bachelor's degree or higher | 4.6 | 5.4 | 3.6 | 14.9 | 4.7 | 4.4 | 4.0 | 7.7 | 14.6 |
| Unknown | 7.2 | 2.2 | 15.3 | 2.0 | 2.8 | 2.2 | 5.1 | 2.0 | 3.1 |
CVD indicates cardiovascular disease; GED, General Equivalency Diploma; IHD, ischemic heart disease; IQR, interquartile range: NHW, non‐Hispanic white.
Over the 10‐year study period.
Figure 1 demonstrates age‐adjusted all‐cause and CVD mortality among all Hispanic adults by nativity status. Foreign‐born Hispanic adults experienced higher age‐adjusted death rates for all‐cause mortality, all CVD, IHD, and cerebrovascular disease compared with US‐born Hispanic adults. Rates for US‐born Hispanic persons were 16.6% lower for total CVD deaths, 24.2% lower for IHD deaths, and 9.6% lower for cerebrovascular disease deaths compared with foreign‐born Hispanic persons. Figure 2 shows the effect of nativity status on CVD mortality among the 3 largest Hispanic subgroups. Foreign‐born Cubans, Mexicans, and Puerto Ricans experienced higher mortality than US‐born groups. Notably, foreign‐born Puerto Ricans had higher AMRs for IHD compared with foreign‐born Cubans and Mexicans (9.5% and 34.9% higher, respectively).
Figure 1.
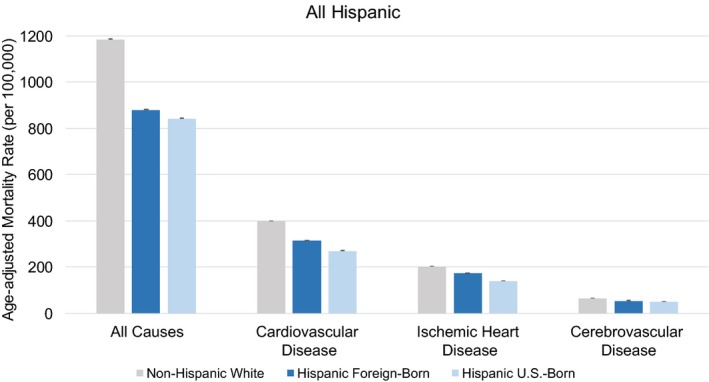
All‐cause and cause‐specific cardiovascular disease age‐adjusted mortality rates (per 100 000 population) with 95% confidence intervals by nativity status for all Hispanic and non‐Hispanic white adults (2003–2012).
Figure 2.
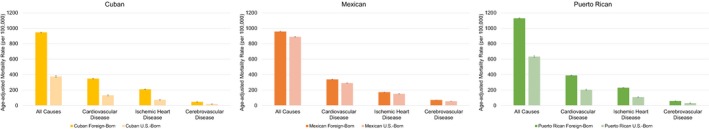
All‐cause and cause‐specific cardiovascular disease age‐adjusted mortality rates (per 100 000 population) with 95% confidence intervals by nativity status for Hispanic subgroups (2003–2012).
Table 2 shows the age‐adjusted death rates for Hispanic and NHW adults by subgroup, nativity status, and sex. In aggregate, foreign‐born Hispanic adults had 315 (95% CI, 314–316) total CVD deaths per 100 000 compared with 270 (95% CI, 269–272) among US‐born Hispanic adults. Foreign‐born Puerto Ricans had the highest CVD death rates, with 390 (95% CI, 386–393) deaths per 100 000 among all other Hispanic groups. The difference between foreign‐ and US‐born mortality rates between subgroups varied by sex. Men experienced higher CVD mortality rates than women. However, the differential between foreign‐ and US‐born mortality was higher among Mexican women for both CVD (309 [95% CI, 306–312] versus 237 [95% CI, 235–239] deaths per 100 000) and IHD (146 [95% CI, 144–149] versus 113 [95% CI, 111–114] deaths per 100 000), whereas mortality rates among foreign and US‐born Mexican men were similar (368 [95% CI, 365–372] versus 354 [95% CI, 351–357] deaths per 100 000 for CVD and 200 [95% CI, 197–312] deaths per 100 000 for IHD).
Table 2.
AMRs (Per 100 000 Population) for All‐Hispanic, Cuban, Mexican, Puerto Rican, and NHW Adults by Cardiovascular Subtype, Nativity Status, and Sex (95% CIs)
| Decedent Characteristics | All Hispanic | Cuban | Mexican | Puerto Rican | NHW | ||||
|---|---|---|---|---|---|---|---|---|---|
| Foreign‐Born AMR (95% CI) | US‐Born AMR (95% CI) | Foreign‐Born AMR (95% CI) | US‐Born AMR (95% CI) | Foreign‐Born AMR (95% CI) | US‐Born AMR (95% CI) | Foreign‐Born AMR (95% CI) | US‐Born AMR (95% CI) | US‐Born AMR (95% CI) | |
| Female | |||||||||
| All cause | 741 (739–744) | 689 (686–692) | 751 (744–757) | 306 (292–320) | 847 (842–852) | 729 (725–732) | 911 (904–919) | 508 (496–521) | 1014 (1013–1015) |
| CVD | 271 (269–272) | 221 (219–223) | 277 (274–281) | 108 (100–117) | 309 (306–312) | 237 (235–239) | 325 (320–329) | 168 (160–176) | 335 (334–335) |
| IHD | 143 (141–144) | 104 (103–105) | 162 (159–164) | 57 (51–64) | 146 (144–149) | 113 (111–114) | 186 (183–189) | 84 (78–90) | 153 (153–153) |
| Cerebrovascular disease | 52 (51–52) | 47 (46–48) | 42 (41–43) | 17 (14–21) | 69 (68–71) | 51 (50–52) | 51 (49–52) | 28 (25–31) | 65 (65–65) |
| Male | |||||||||
| All cause | 1059 (1055–1063) | 1033 (1029–1037) | 1191 (1181–1200) | 461 (442–482) | 1077 (1071–1083) | 1085 (1080–1090) | 1420 (1409–1431) | 788 (770–806) | 1407 (1406–1408) |
| CVD | 371 (369–374) | 332 (329–334) | 434 (428–439) | 161 (149–174) | 368 (365–372) | 354 (351–357) | 479 (472–485) | 250 (238–261) | 479 (478–479) |
| IHD | 215 (213–217) | 187 (185–189) | 270 (265–274) | 94 (85–104) | 200 (197–202) | 200 (198–203) | 291 (285–296) | 140 (132–148) | 269 (269–270) |
| Cerebrovascular disease | 59 (58–60) | 54 (53–55) | 52 (50–54) | 20 (15–24) | 71 (69–72) | 59 (58–60) | 65 (62–67) | 34 (30–39) | 65 (65–66) |
| Total | |||||||||
| All cause | 881 (879–883) | 844 (841–846) | 948 (942–953) | 377 (365–389) | 959 (955–962) | 890 (887–893) | 1129 (1123–1136) | 634 (623–645) | 1186 (1186–1187) |
| CVD | 315 (314–316) | 270 (269–272) | 348 (344–351) | 132 (125–140) | 338 (336–340) | 290 (288–291) | 390 (386–393) | 204 (197–211) | 399 (398–399) |
| IHD | 174 (173–175) | 140 (139–141) | 210 (208–213) | 74 (69–79) | 172 (170–173) | 151 (150–153) | 230 (227–233) | 109 (104–114) | 203 (203–203) |
| Cerebrovascular disease | 55 (55–56) | 50 (50–51) | 47 (45–48) | 18 (16–21) | 70 (69–71) | 55 (54–56) | 57 (55–58) | 30 (28–33) | 66 (66–66) |
AMR indicates age‐adjusted mortality rate; CI, confidence interval; CVD, cardiovascular disease; IHD, ischemic heart disease; NHW, non‐Hispanic white.
Table 3 shows the rate ratios (with 95% CIs) of all‐Hispanic, Cuban, Mexican, and Puerto Rican adults for foreign‐born decedents, with respective US‐born groups as the reference group. Foreign‐born Cubans had 2.51 (95% CI, 2.42–2.61) times higher all‐cause mortality rates compared with US‐born Cubans, and mortality rates were 2.64 (95% CI, 2.46–2.81) times higher for CVD, 2.84 (95% CI, 2.63–3.09) times higher for IHD, and 2.61 (95% CI, 2.14–3.00) times higher for cerebrovascular disease. Rate ratios for foreign‐born/islander Puerto Ricans were approximately twice as high as those of US‐born Puerto Ricans for all CVD mortality.
Table 3.
Relative Rate Ratios and 95% CIs of Foreign‐Born to US‐Born Age‐Adjusted CVD Mortality Rates by Hispanic Subgroups (Cubans, Mexicans, and Puerto Ricans)
| All Hispanic | Cuban | Mexican | Puerto Rican | |
|---|---|---|---|---|
| All cause | 1.04 (1.04–1.05) | 2.51 (2.42–2.61) | 1.08 (1.07–1.08) | 1.78 (1.74–1.82) |
| CVD | 1.17 (1.15–1.17) | 2.64 (2.46–2.81) | 1.17 (1.15–1.18) | 1.91 (1.83–1.99) |
| IHD | 1.24 (1.23–1.26) | 2.84 (2.63–3.09) | 1.14 (1.11–1.15) | 2.11 (1.99–2.24) |
| Cerebrovascular disease | 1.10 (1.07–1.12) | 2.61 (2.14–3.00) | 1.27 (1.23–1.31) | 1.90 (1.67–2.07) |
CI indicates confidence interval; CVD, cardiovascular disease; IHD, ischemic heart disease.
Discussion
Using a decade of national data, we found that foreign‐born Cubans, Mexicans, and Puerto Ricans experienced higher age‐adjusted CVD mortality than their US‐born counterparts. This pattern was consistent across the 3 largest Hispanic subgroups, albeit strongest among Cubans and weakest among Mexicans. Our study generally supports the Hispanic paradox by showing that both foreign‐ and US‐born Hispanic adults had lower CVD mortality than NHW adults but contradicts the healthy immigrant effect because foreign‐born Hispanic adults had higher mortality rates than US born Hispanic adults.
There are several possible explanations for our findings against the healthy immigrant effect. First, we used a large national sample that included a heterogeneous population of Hispanic subgroups, a major limitation of prior work that has focused largely on Mexicans in 1 geographic region29 and on risk factors rather than mortality.30, 31, 32 US‐born Cubans and Puerto Ricans, in particular, had lower AMRs, suggesting a protective effect of generational status among these subgroups. As shown in our data, foreign‐born Hispanic adults are significantly older and have lower educational attainment than both US‐born Hispanic and NHW adults. The gradient between socioeconomic status and health has been extensively documented.33, 34 It is likely that lower socioeconomic status among foreign‐born Hispanics translates to worse CVD risk profiles and access to care and thus higher CVD death rates. Hispanic persons born in the United States are more likely to be insured, to seek regular preventive services, and to have higher English language proficiency—factors that may, in turn, mitigate cardiovascular risk and mortality.
The role of acculturation in Hispanic CVD health remains uncertain.12, 35, 36, 37 Whereas some studies have shown that greater acculturation is associated with greater prevalence of CVD risk factors,38 others have shown that lower acculturation is associated with worse risk factor control.35 In addition, the role of acculturation and chronic disease risk factor control varies by country of origin and the acculturation metric (nativity, language, duration of residence) that is studied.39 The healthy immigrant effect postulates that new immigrants are healthier than average compared with persons in both their native and host countries, likely due to selective migration,40 although a study from the Mexican Family Life Survey documented weak support for this hypothesis.41 Large studies supporting the healthy immigrant effect and mortality have examined duration of residence in immigrant populations, rather than nativity status, as a marker of acculturation.42
Our results challenge the commonly held notions of the “healthy migrant” or the “salmon bias hypothesis.”12, 13 These theories contend that those who migrate to the United States are healthier and younger than those who chose not to migrate, resulting in a health advantage over the host population. Similarly, the salmon bias theory proposes that migrants return to their native country to die, thereby spuriously lowering mortality rates in the United States. We found consistently higher AMRs for foreign‐born Hispanic adults across all‐cause mortality, all CVD, IHD, and cerebrovascular disease deaths. However, this foreign‐ versus US‐born difference was lowest for Mexican Americans and highest for Cubans, which may in part be influenced by ease of reverse migration to these respective countries.
Our findings also emphasize the importance of data disaggregation by Hispanic subgroup in national reports. Although our prior work has highlighted heterogeneity between Hispanic subgroups and CVD mortality,24 granulizing data even further by nativity status (especially for largely foreign‐born populations) has demonstrated further heterogeneity in outcomes. Foreign‐born Cubans were shown to have the largest CVD mortality differential compared with US‐born Cubans, highlighting a potentially missed opportunity in cardiovascular prevention among immigrants. Contrary to the Hispanic paradox, we also found that foreign‐born/islander Puerto Ricans experienced higher mortality for IHD compared with NHW adults and other Hispanic subgroups. Foreign‐born Mexicans experienced the highest rates of cerebrovascular disease mortality at younger ages, perhaps explained by differences in risk factors, healthcare access, or genetic susceptibility to disease.43 Similar to our findings, a study of insured Hispanic persons in Northern California also documented that the Hispanic mortality paradox was attenuated by taking into account nativity status, with higher CVD mortality among Mexican‐born Hispanic persons compared with US‐born Mexicans.44
Our analysis provides a contemporary overview of mortality outcomes by Hispanic subgroups and nativity status. The recent HCHS/SOL indicated that recent immigrants with <10 years of residence in the United States had more favorable cardiovascular health.45 Given the younger age of participants in these cohort data (ie, mean age ≈40–47 years for foreign‐born versus 31 years for US‐born adults), it is possible that the observed health advantages may attenuate over time among foreign‐born Hispanic persons with increasing acculturation, which is then associated with worsening of CVD health.38 It is likely that many of the foreign‐born decedents in our study had longer years of residence in the United States, partly explaining the higher mortality.
Our study has several strengths including national level data, multiple years of data analyzed, and consideration of both Hispanic subgroups and major CVD subtypes. We also included older adults, a major limitation of prior studies that have focused on young and middle‐aged Hispanic adults.46 Limitations include the use of nativity as a crude measure of acculturation, which fails to fully capture the complexity and multiple dimensions of the acculturative process. We were unable to distinguish foreign‐born individuals who migrated to the United States at younger versus older ages or to include years of residence in the United States in our analyses. Given the limitations inherent to mortality records, we were unable to adjust for sociodemographic or risk factor differences that may partially explain our findings. Misclassification of race and ethnicity data on mortality records may have led to under‐ or overestimation of mortality rates. However, studies have ascertained that Hispanic classification on death records is reasonably accurate, with a net ascertainment of Hispanic classification just 3% higher on survey records compared with death certificates.47 Both sensitivity (88–93%) and positive predictive value (91–96%) are reasonably high. With a potential 3% misclassification of Hispanic race/ethnicity on the death records, it is possible that rates may be slightly underestimated, and this relatively small misclassification rate may vary across subgroups.48 Statistical immortality conferred by reverse migration (ie, individuals may migrate to their country of origin to die) may result in an underestimation of deaths, although this would not likely explain the results seen for Puerto Ricans (captured in US mortality data) or Cubans (unable to easily return back to their country of origin). Finally, the group “all‐Hispanic” includes a heterogeneous population including Dominicans, South, and Central Americans, which could not be further disaggregated given small sample sizes. In addition, CVD mortality may vary by geography and other socioeconomic factors that were not included in the analyses.
Conclusion
In a large national study of 10 years of mortality data, we showed that foreign‐born Hispanic adults experienced higher age‐adjusted mortality rates from CVD compared with US‐born Hispanic adults; this difference was particular pronounced among Cubans and Puerto Ricans. Our findings suggest that public health strategies to improve the cardiovascular health of Hispanic adults in the United States need to consider Hispanic subgroup and nativity status.
Sources of Funding
This work was supported by the National Institute on Minority Health and Health Disparities (R01 MD007012) and the National Heart, Lung, and Blood Institute (F32HL132396).
Disclosures
None.
Acknowledgments
The authors would like to thank Derek Boothroyd, PhD, from the Quantitative Sciences Unit at Stanford University School of Medicine, for his statistical guidance.
(J Am Heart Assoc. 2017;6:e007207 DOI: 10.1161/JAHA.117.007207.)29237590
References
- 1. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Pina IL, Ramirez SM, Rodriguez B, Sims M; American Heart Association Council on E, Prevention, American Heart Association Council on Clinical C, American Heart Association Council on C and Stroke N . Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. y González MP. Puerto Ricans in the United States. Santa Barbara: Greenwood Publishing Group; 2000. [Google Scholar]
- 3. Massey DS, Bitterman B. Explaining the paradox of Puerto Rican segregation. Soc Forces. 1985;64:306–331. [Google Scholar]
- 4. Korrol VS. From Colonia to Community: the History of Puerto Ricans in New York City. Oakland: University of California Press; 1994. [Google Scholar]
- 5. Collazo SG, Ryan CL, Bauman KJ. Profile of the Puerto Rican population in United States and Puerto Rico: 2008. 2010.
- 6. Rusin S, Zong J, Batalova J. Cuban immigrants in the United States. The Online Journal of the Migration Policy Institute. 2015.
- 7. Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. Current Population Reports. 2014.
- 8. Dominguez K, Penman‐Aguilar A, Chang M‐H, Moonesinghe R, Castellanos T, Rodriguez‐Lainz A, Schieber R. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States—2009–2013. MMWR Morb Mortal Wkly Rep. 2015;64:469–478. [PMC free article] [PubMed] [Google Scholar]
- 9. Stepler R, Brown A. Statistical portrait of Hispanics in the United States. Hispanic Trends. 2016.
- 10. Writing Group M , Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:447–454. [DOI] [PubMed] [Google Scholar]
- 11. Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60:S68–S75. [DOI] [PubMed] [Google Scholar]
- 12. Medina‐Inojosa J, Jean N, Cortes‐Bergoderi M, Lopez‐Jimenez F. The Hispanic paradox in cardiovascular disease and total mortality. Prog Cardiovasc Dis. 2014;57:286–292. [DOI] [PubMed] [Google Scholar]
- 13. Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 14. Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta‐analysis of the longitudinal literature. Am J Public Health. 2013;103:e52–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13:477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kennedy S, McDonald JT, Biddle N. The healthy immigrant effect and immigrant selection: evidence from four countries. Available at: https://link.springer.com/article/10.1007/s12134-014-0340-x. Accessed July 1, 2017.
- 17. Abraido‐Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory‐driven model of acculturation in public health research. Am J Public Health. 2006;96:1342–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65:237–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Le‐Scherban F, Albrecht SS, Bertoni A, Kandula N, Mehta N, Diez Roux AV. Immigrant status and cardiovascular risk over time: results from the Multi‐Ethnic Study of Atherosclerosis. Ann Epidemiol. 2016;26:429–435.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thomson MD, Hoffman‐Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69:983–991. [DOI] [PubMed] [Google Scholar]
- 22. Lutsey PL, Diez Roux AV, Jacobs DR Jr, Burke GL, Harman J, Shea S, Folsom AR. Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the Multi‐Ethnic Study of Atherosclerosis. Am J Public Health. 2008;98:1963–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Daviglus ML, Pirzada A, Durazo‐Arvizu R, Chen J, Allison M, Aviles‐Santa L, Cai J, Gonzalez HM, Kaplan RC, Schneiderman N, Sorlie PD, Talavera GA, Wassertheil‐Smoller S, Stamler J. Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: the Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc. 2016;5:e003929 DOI: 10.1161/JAHA.116.003929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rodriguez F, Hastings KG, Boothroyd DB, Echeverria S, Lopez L, Cullen M, Harrington RA. Disaggregation of cause‐specific cardiovascular disease mortality among Hispanic subgroups. JAMA Cardiol. 2017;2:240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hastings KG, Jose PO, Kapphahn KI, Frank AT, Goldstein BA, Thompson CA, Eggleston K, Cullen MR, Palaniappan LP. Leading causes of death among Asian American subgroups (2003–2011). PLoS One. 2015;10:e0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abraido‐Lanza AF, Dohrenwend BP, Ng‐Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US‐ and foreign‐born women in major US racial and ethnic groups. Am J Public Health. 1996;86:837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Borrell LN, Crawford ND. All‐cause mortality among Hispanics in the United States: exploring heterogeneity by nativity status, country of origin, and race in the National Health Interview Survey‐linked Mortality Files. Ann Epidemiol. 2009;19:336–343. [DOI] [PubMed] [Google Scholar]
- 29. Hunt KJ, Williams K, Resendez RG, Hazuda HP, Haffner SM, Stern MP. All‐cause and cardiovascular mortality among diabetic participants in the San Antonio Heart Study: evidence against the “Hispanic Paradox”. Diabetes Care. 2002;25:1557–1563. [DOI] [PubMed] [Google Scholar]
- 30. Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988–1994. Am J Public Health. 1999;89:723–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mitchell BD, Stern MP, Haffner SM, Hazuda HP, Patterson JK. Risk factors for cardiovascular mortality in Mexican Americans and non‐Hispanic whites. San Antonio Heart Study. Am J Epidemiol. 1990;131:423–433. [DOI] [PubMed] [Google Scholar]
- 33. Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood). 2002;21:60–76. [DOI] [PubMed] [Google Scholar]
- 34. Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896:3–15. [DOI] [PubMed] [Google Scholar]
- 35. Eamranond PP, Wee CC, Legedza AT, Marcantonio ER, Leveille SG. Acculturation and cardiovascular risk factor control among Hispanic adults in the United States. Public Health Rep. 2009;124:818–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eamranond PP, Legedza AT, Diez‐Roux AV, Kandula NR, Palmas W, Siscovick DS, Mukamal KJ. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;157:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Eamranond PP, Patel KV, Legedza AT, Marcantonio ER, Leveille SG. The association of language with prevalence of undiagnosed hypertension among older Mexican Americans. Ethn Dis. 2007;17:699–706. [PubMed] [Google Scholar]
- 38. Kandula NR, Diez‐Roux AV, Chan C, Daviglus ML, Jackson SA, Ni H, Schreiner PJ. Association of acculturation levels and prevalence of diabetes in the Multi‐Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2008;31:1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rodriguez F, Hicks LS, Lopez L. Association of acculturation and country of origin with self‐reported hypertension and diabetes in a heterogeneous Hispanic population. BMC Public Health. 2012;12:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Singh GK, Siahpush M. All‐cause and cause‐specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91:392–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: new findings from the Mexican Family Life Survey. Am J Public Health. 2008;98:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ng E. The healthy immigrant effect and mortality rates. Health Rep. 2011;22:25–29. [PubMed] [Google Scholar]
- 43. Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, Longwell PJ, McFarling DA, Akuwumi O, Al‐Wabil A, Al‐Senani F, Brown DL, Moye LA. Excess stroke in Mexican Americans compared with non‐Hispanic whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Iribarren C, Darbinian JA, Fireman BH, Burchard EG. Birthplace and mortality among insured Latinos: the paradox revisited. Ethn Dis. 2009;19:185–191. [PubMed] [Google Scholar]
- 45. Kershaw KN, Giacinto RE, Gonzalez F, Isasi CR, Salgado H, Stamler J, Talavera GA, Tarraf W, Van Horn L, Wu D. Relationships of nativity and length of residence in the US with favorable cardiovascular health among Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med. 2016;89:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lopez L, Peralta CA, Lee A, Zeki Al Hazzouri A, Haan MN. Impact of acculturation on cardiovascular risk factors among elderly Mexican Americans. Ann Epidemiol. 2014;24:714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rosenberg HM, Maurer JD, Sorlie PD, Johnson NJ, MacDorman MF, Hoyert DL, Spitler JF, Scott C. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat. 1999;2:1–13. [PubMed] [Google Scholar]
- 48. Arias E, Heron M; National Center for Health S , Hakes J; Bureau USC . The validity of race and Hispanic‐origin reporting on death certificates in the United States: an update. Vital Health Stat. 2016;2:1–21. [PubMed] [Google Scholar]


