Abstract
Background
Patients with atrial fibrillation (AF) often undergo AV junction ablation (AVJA) and pacemaker implantation. Right ventricular (RV) pacing contributes to increased risk of heart failure (HF), which may be mitigated by biventricular pacing. We sought to determine the impact of AVJA concurrent with RV versus biventricular pacemaker implantation on AF and HF hospitalizations.
Methods and Results
The MarketScan Commercial and Medicare Supplemental claims database was used to select 18‐ to 100‐year‐old patients with AF with pacemaker implantation. Patients were divided into those with an RV and a biventricular pacemaker and further into those who did (AVJA +) or did not undergo concurrent ablation. Separately, the AVJA+ group was divided into those receiving RV versus biventricular pacemakers. AF and HF hospitalization rates were compared between groups after matching on demographics, comorbidities, and baseline hospitalization rates. The study included 24 361 patients, with RV (n=23 377) or biventricular (n=984) pacemakers; 1611 patients underwent AVJA. AVJA + was associated with reduced AF hospitalization risk (RV hazard ratio [HR], 0.31; P<0.001; biventricular HR, 0.20; P=0.003) compared with no AVJA. However, HF hospitalization risk was increased for RV (HR, 1.63; P=0.001), but not biventricular (HR, 0.98; P=0.942), pacemakers. In AVJA + patients, biventricular pacing was associated with reduced risk of HF hospitalization versus RV pacing (HR, 0.62; P=0.017).
Conclusions
In a large cohort of patients with AF, AVJA + significantly reduced AF hospitalizations, irrespective of whether an RV or a biventricular pacemaker was implanted. However, AVJA was associated with a marked HF hospitalization increase in patients with an RV pacemaker, which was ameliorated with biventricular pacing.
Keywords: ablation, atrial fibrillation, biventricular pacing, heart failure, pacemaker
Subject Categories: Atrial Fibrillation, Heart Failure, Pacemaker, Quality and Outcomes, Catheter Ablation and Implantable Cardioverter-Defibrillator
Clinical Perspective
What Is New?
We analyzed a large database of patients with atrial fibrillation who underwent ablation of the AV junction, followed by either right ventricular or biventricular pacemaker implantation, and found that AV junction ablation was associated with a reduced likelihood and rate of atrial fibrillation–related hospitalization, irrespective of pacemaker type implanted.
Right ventricular pacing was associated with a greater likelihood and rate of heart failure hospitalizations, whereas this was not observed in patients with a biventricular pacemaker.
Implantation of a biventricular pacemaker was associated with a 38% reduction in heart failure hospitalizations, and this translated into a 27% reduction in annual payments.
What Are the Clinical Implications?
In a large national cohort of patients with atrial fibrillation undergoing AV junction ablation, a marked increase in heart failure hospitalizations was observed in patients implanted with a right ventricular pacemaker, whereas this was not observed with biventricular pacing.
Thus, studies comparing a selective conduction system with biventricular pacing in this patient population are needed to define the optimal post–AV junction ablation pacing strategy.
In patients with atrial fibrillation (AF), hospitalizations to manage symptoms of AF or those related to development of heart failure (HF) are common. AV junction ablation (AVJA) is sometimes necessary to achieve ventricular rate control and to mitigate the need for recurrent AF‐ or HF‐related hospitalizations.1, 2 By nature of the ablation procedure, patients require pacemaker implantation to maintain an adequate heart rate. Although right ventricular (RV) pacing has been most commonly used, concerns have been raised about the deleterious impact of RV pacing on clinical outcomes; in some patients, clinical deterioration can occur within months of pacemaker implantation.3 Thus, several investigators have explored the role of biventricular pacing in this patient population.4, 5, 6, 7, 8 However, these studies have produced conflicting results, likely in part because of the relatively few patients enrolled and variability in follow‐up duration. Therefore, in this large retrospective study using real‐world data from a cohort of patients with AF who were undergoing pacemaker implantation, we sought to determine the following: (1) the impact of AVJA at pacemaker implantation on subsequent AF‐ and HF‐related hospitalizations and associated costs and (2) whether these differed in patients implanted with an RV versus a biventricular pacemaker after AVJA.
Methods
Data Source
This retrospective, observational, cohort study used data from inpatient hospital encounters and outpatient physician office visits collected in the Truven Health MarketScan Commercial Claims and Medicare Supplemental databases. The databases capture paid and adjudicated claims for privately insured and Medicare Advantage (supplemental) patients throughout the United States, and include records from >170 million enrollees since 1995.9 A monthly enrollment indicator is used to determine when a patient is followed up in MarketScan. Health outcomes research using MarketScan data has been widely published in peer‐reviewed journals, including studies of patients undergoing cardiac procedures and receiving implantable electronic devices.10, 11, 12 This study was a retrospective analysis of a deidentified database and, thus, the research was exempt from institutional review board review under 45 CFR 46.101(b)(4). All codes used to identify implants, baseline characteristics, and events are listed in Table 1.
Table 1.
ICD‐9, CPT, and HCPCS Codes Used for Clinical Diagnoses, AVJA, Pacemaker Implantation, and Pacemaker Follow‐Up
| Codes used for patient characterization and outcomes | |
| Atrial fibrillation | 427.31 |
| Heart failure | 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4‐425.9, 428.x |
| VT/VF | 427.1, 427.4x |
| Coronary artery disease | 410.x‐414.x, 429.2, V45.81 |
| Hypertension | 401.x‐405.x, 437.2 |
| Cerebrovascular disease | 362.34, 430.x‐438.x |
| Diabetes mellitus | 250.x |
| Valve disease | 394.x‐397.x, 424.x, 746.x, V42.2, V43.3 |
| Peripheral vascular disease | 093.0, 437.3, 440.x, 441.x, 443.1‐443.9, 447.1, 557.1, 557.9, V43.4 |
| Chronic pulmonary disease | 416.8, 416.9, 490.x‐505.x, 506.4, 508.1, 508.8 |
| Chronic kidney disease | 403.1, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 582.x, 583.0‐583.7, 585.x, 586, 588.0, V42.0, V56.x |
| Rheumatic disease | 446.5, 710.0‐710.4, 714.0‐714.2, 714.8, 725.x |
| Peptic ulcer disease | 531.x‐534.x |
| Liver disease | 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 070.6, 070.9, 456.0‐456.1, 570.x, 571.x, 572.2‐572.8, 573.3, 573.4, 573.8, 573.9, V42.7 |
| Hypothyroidism | 240.9, 243.x, 244.x, 246.1, 246.8 |
| Cancer | 140.x‐172.x, 174.x‐194.x, 195.0‐195.8, 196.x, 197.0‐197.8, 198.0‐198.8x, 1990‐1992, 200.x‐208.x, 238.6 |
| Dementia | 290.x, 331.0, 331.2 |
| Depression | 300.4, 309.x, 311 |
| AIDS/HIV | 042 |
| Hemiplegia/paraplegia | 334.1, 342.00‐342.92, 343.x, 344.1, 344.2, 344.5, 344.9 |
| Obesity | 278.00 |
| Codes used for AVJA, pacemaker implantation, and follow‐up | |
| AVJA | 93650 |
| Dual‐chamber RV pacemaker | 33208, C1785, C2619 |
| Single‐chamber RV pacemaker | 33206, 33207, C1786, C2620, 3781, 3782 |
| Biventricular pacemaker | 33224, 33225, 0050, 0052, C2621, C1900 |
| Pacemaker follow‐up | 93279‐93281, 93286, 93288, 93293, 93294, 93296, 93724, 93731‐93736, 89.45‐89.48, E0610 |
AVJA indicates AV junction ablation; CPT, Current Procedural Terminology; HCPCS, healthcare common procedure coding system; ICD‐9, International Classification of Diseases, Ninth Revision; RV, right ventricular; and VT/VF, ventricular tachycardia/ventricular fibrillation.
Study Population
Patients implanted with a de novo single‐chamber, dual‐chamber, or biventricular pacemaker from any manufacturer between April 1, 2008, and March 31, 2014, were included. De novo implants were identified as patients with a pacemaker without a prior device implant and without a remote or in‐office pacemaker follow‐up visit in the 1 year before implantation. Patients were required to have at least 1 year of continuous enrollment in the MarketScan database before and after pacemaker implant, to be ≥18 and ≤100 years old at the implantation, and to have a diagnosis of AF (International Classification of Diseases, Ninth Revision [ICD‐9] code 427.31) within 1 year before pacemaker implantation.
To evaluate the impact of AVJA (Current Procedural Terminology code 93650) on clinical outcomes, patients with AF were dichotomized into those with an AVJA (AVJA+) versus those without an AVJA (AVJA−) at pacemaker implantation. Patients with an AVJA occurring on a day other than the day of pacemaker implantation were excluded from the analysis. To compare the effect of AVJA on patients with biventricular versus RV‐only pacing, patients implanted with biventricular pacemakers were evaluated separately from those implanted with single‐ or dual‐chamber pacemakers.
Patient demographics included age, sex, US region, year of pacemaker implantation, and number of pacing leads (patients with an RV pacemaker only). In addition, 20 baseline comorbidities (based on the Charlson comorbidity index) were determined using diagnosis and procedure codes collected across all available fields in the MarketScan inpatient and outpatient encounters in the 1 year before pacemaker implantation (Table 1), as previously validated.13, 14 US regions included Northeast, North Central, South, and West. Propensity scores for undergoing an AVJA were calculated for every patient in the study cohort on the basis of a multivariable logistic regression model, including all covariates used in the patient characterization and cumulative AF and HF hospitalization rates in the 1 year before pacemaker implantation. Patients were propensity score matched using greedy matching without replacement. A match ratio of 1:1 was used for patients implanted with biventricular pacemakers. For those implanted with RV pacemakers, a 4:1 match ratio was used because of the large proportion of AVJA− patients.
Outcomes
Primary outcomes included AF and HF hospitalizations occurring in the 3 years after pacemaker implantation. AF and HF hospitalizations were identified by any inpatient encounter for which the primary diagnosis was AF or HF related, respectively. A 1‐week postimplantation blanking window was used to exclude complications associated with pacemaker implantation or AVJA. The secondary outcome was annualized total payments associated with AF or HF hospitalizations, evaluated over the 3 years after pacemaker implantation.
AVJA+ Subanalysis
To directly compare the impact of biventricular versus RV‐only pacing on HF hospitalizations after AVJA, a subanalysis was performed in only AVJA+ patients. Propensity scores for receiving an RV versus a biventricular pacemaker were computed, as described previously. Patients with RV and biventricular pacemakers were 1:1 propensity score matched using greedy matching without replacement. HF hospitalizations and associated payments were compared between the matched RV and biventricular pacemaker cohorts.
Statistical Analyses
For the primary analysis, baseline characteristics were compared between matched AVJA− and AVJA+ patients within the RV and biventricular pacemaker cohorts. For the AVJA+ subanalysis, baseline characteristics were compared for patients implanted with RV versus biventricular pacemakers. Continuous variables, including follow‐up duration and age, were compared using a Student t test or Mann‐Whitney test if the distribution was not normal. Categorical variables, such as sex and baseline comorbidities, were compared using a χ2 test. In addition, the standardized mean differences were computed for all variables. Standardized mean difference values >0.1 are considered meaningful. Standardized mean differences were computed with the tableone package in R, using previously described methods.15
Cumulative rates of AF and HF hospitalizations (events per 100 patient‐years) were compared between matched groups using a Poisson regression. Event‐free survival was measured by the Kaplan‐Meier method, and differences between matched cohorts were compared using a univariate marginal Cox proportional hazards model to account for possible correlation or clustering in matched groups. The proportional hazards assumption was tested using Schoenfeld residuals and was met for all comparisons. Patients were censored at hospitalization, at the end of MarketScan enrollment, or at an administrative censoring date set at 3 years after pacemaker implantation. In addition, patients implanted with RV pacemakers were censored at biventricular upgrade. For multivariate analysis on the prematched cohorts, a Cox regression was performed with the propensity score as the covariate. Statistical significance was determined using α=0.05.
For the secondary outcome of costs associated with AF or HF hospitalizations, a 2‐part model was used to compare inpatient hospitalization payments between matched cohorts. The 2‐part model is a well‐established econometric modeling technique that accounts for samples with a large proportion of 0 measurements, common to healthcare data in which healthy participants incur no medical costs. In part 1, a logistic regression was used to model the likelihood of incurring non‐0 payments after pacemaker implantation, adjusting for therapy group, follow‐up duration, and the computed propensity score. Using this model, the numeric probability of incurring non‐0 payments at 1 year after implantation was then estimated for each patient. In part 2, using only those patients who had non‐0 hospitalization payments in the 3 years after pacemaker implantation, a linear regression with γ distribution and log link was used to model the total hospitalization costs, adjusting for therapy group, follow‐up duration, and the computed propensity score. The total payments at 1 year after implantation were then predicted for all patients using results from the linear regression model. The final adjusted cost for each patient was computed as the product of the probability from part 1 and the predicted payments from part 2. A Mann‐Whitney test was used to compare the median adjusted costs between groups.
All analyses were performed on Revolution Analytics Revolution R Enterprise with Open Source R version 3.1.1. Matching was performed in SAS version 9.3 using the OneToManyMTCH macro.
Results
Study Population
The study cohort included 24 361 patients with a pacemaker followed up for a median of 2.20 (quartile 1–quartile 3, 1.55–3.21) years. Overall, 1611 patients (4.8%) underwent a pacemaker implantation and same‐day AVJA. Of these patients, 798 were implanted with an RV and 363 were implanted with a biventricular pacemaker (Figure 1). Matched cohorts in the RV pacemaker arm included 2924 AVJA− and 731 AVJA+ patients (age, 76.3±10.6 years; 31% men). Biventricular pacemaker matched cohorts included 294 AVJA− and 294 AJVA+ patients (age, 75.2±11.2 years; 51% men). Baseline characteristics after propensity score matching are presented in Table 2. The groups were well matched in terms of baseline characteristics (Table 2) and cumulative AF and HF hospitalization rates (Table 3) in the 1 year before pacemaker implantation.
Figure 1.
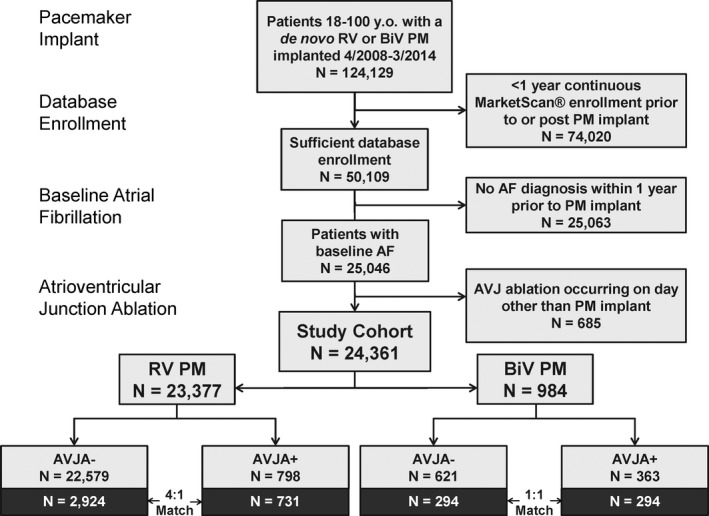
Cohort diagram. Schematic of patients included in the study cohort, including those with and without AV junction ablation (AVJA + and AVJA −, respectively) on the same day as pacemaker implantation. AF indicates atrial fibrillation; and RV, right ventricular (single or dual chamber). BiV indicates biventricular; PM, pacemaker.
Table 2.
Baseline Characteristics for Matched Patients: AVJA+ and AVJA− Groups
| Characteristics | Matched RV Pacemaker | Matched Biventricular Pacemaker | ||||||
|---|---|---|---|---|---|---|---|---|
| AVJA− (N=2924) | AVJA+ (N=731) | SMD | P Value | AVJA− (N=294) | AVJA+ (N=294) | SMD | P Value | |
| Demographics | ||||||||
| Follow‐up, y | 2.20 (1.54–3.25) | 2.16 (1.57–3.10) | 0.033 | 0.422 | 2.13 (1.51–3.05) | 1.95 (1.47–3.06) | 0.063 | 0.442 |
| Male sex | 900 (31) | 244 (33) | 0.056 | 0.190 | 146 (50) | 151 (51) | 0.034 | 0.741 |
| Age, y | 76.2±10.8 | 76.8±9.8 | 0.056 | 0.163 | 75.2±11.6 | 75.1±10.8 | 0.012 | 0.888 |
| Device type | ||||||||
| Dual chamber | 1708 (58) | 425 (58) | 0.006 | 0.926 | NA | NA | NA | NA |
| Implant year | ||||||||
| 2009 | 548 (19) | 132 (18) | 0.131 | 0.043 | 38 (13) | 30 (10) | 0.231 | 0.102 |
| 2010 | 769 (26) | 167 (23) | 70 (24) | 81 (28) | ||||
| 2011 | 717 (25) | 192 (26) | 94 (32) | 72 (24) | ||||
| 2012 | 703 (24) | 205 (28) | 77 (26) | 99 (34) | ||||
| 2013 | 187 (6) | 35 (5) | 15 (5) | 12 (4) | ||||
| US region | ||||||||
| Northeast | 546 (19) | 101 (14) | 0.179 | 0.002 | 41 (14) | 43 (15) | 0.052 | 0.942 |
| North Central | 1006 (34) | 283 (39) | 120 (41) | 113 (38) | ||||
| South | 910 (31) | 254 (35) | 92 (31) | 97 (33) | ||||
| West | 459 (16) | 93 (13) | 41 (14) | 41 (14) | ||||
| Unknown | 3 (0.1) | 0 (0) | 0 (0) | 0 (0) | ||||
| Comorbidities | ||||||||
| Heart failure | 887 (30) | 239 (33) | 0.051 | 0.234 | 116 (40) | 138 (47) | 0.151 | 0.080 |
| VT/VF | 233 (8) | 70 (10) | 0.057 | 0.182 | 33 (11) | 32 (11) | 0.011 | 1.000 |
| Coronary artery disease | 1539 (53) | 376 (51) | 0.024 | 0.590 | 151 (51) | 155 (53) | 0.027 | 0.804 |
| Hypertension | 2406 (82) | 588 (80) | 0.047 | 0.268 | 239 (81) | 236 (80) | 0.026 | 0.834 |
| Cerebrovascular disease | 600 (21) | 171 (23) | 0.069 | 0.099 | 69 (24) | 62 (21) | 0.057 | 0.552 |
| Diabetes mellitus | 909 (31) | 218 (30) | 0.027 | 0.537 | 95 (32) | 87 (30) | 0.059 | 0.532 |
| Valve disease | 1353 (46) | 334 (46) | 0.012 | 0.810 | 156 (53) | 134 (46) | 0.15 | 0.083 |
| Peripheral vascular disease | 573 (20) | 138 (19) | 0.018 | 0.699 | 62 (21) | 58 (20) | 0.034 | 0.759 |
| Chronic pulmonary disease | 1122 (38) | 284 (39) | 0.01 | 0.845 | 107 (36) | 121 (41) | 0.098 | 0.271 |
| Chronic kidney disease | 444 (15) | 107 (15) | 0.015 | 0.755 | 48 (16) | 50 (17) | 0.018 | 0.912 |
| Rheumatic disease | 114 (4) | 40 (6) | 0.074 | 0.073 | 11 (4) | 8 (3) | 0.058 | 0.641 |
| Peptic ulcer disease | 55 (2) | 13 (2) | 0.008 | 0.976 | 7 (2) | 7 (2) | 0.000 | 1.000 |
| Liver disease | 109 (4) | 43 (6) | 0.101 | 0.012 | 11 (4) | 14 (5) | 0.051 | 0.683 |
| Hypothyroidism | 622 (21) | 157 (22) | 0.005 | 0.944 | 52 (18) | 56 (19) | 0.035 | 0.749 |
| Cancer | 423 (15) | 114 (16) | 0.032 | 0.476 | 45 (15) | 36 (12) | 0.089 | 0.338 |
| Dementia | 61 (2) | 19 (3) | 0.034 | 0.480 | 10 (3) | 7 (2) | 0.061 | 0.623 |
| Depression | 225 (8) | 74 (10) | 0.085 | 0.039 | 28 (10) | 31 (11) | 0.034 | 0.784 |
| AIDS/HIV | 3 (<0.1) | 0 (0) | 0.045 | 0.885 | 1 (<1) | 0 (0) | 0.083 | 1.000 |
| Hemiplegia/paraplegia | 27 (1) | 10 (1) | 0.042 | 0.386 | 2 (1) | 3 (1) | 0.037 | 1.000 |
| Obesity | 193 (7) | 53 (7) | 0.026 | 0.586 | 21 (7) | 24 (8) | 0.038 | 0.756 |
Values are reported as median (quartile 1–quartile 3), mean±SD, or count (percentage). + indicates did undergo AVJA; −, did not undergo AVJA; AVJA, AV junction ablation; NA, not applicable; RV, right ventricular (single or dual chamber); SMD, standardized mean difference; and VT/VF, ventricular tachycardia/ventricular fibrillation.
Table 3.
Cumulative Hospitalization Rates and Annualized Adjusted Payments for Matched Patients: AVJA+ and AVJA− Groups
| Variables | Matched RV Pacemaker | Matched Biventricular Pacemaker | ||||
|---|---|---|---|---|---|---|
| AVJA− (N=2924) | AVJA+ (N=731) | P Value | AVJA− (N=294) | AVJA+ (N=294) | P Value | |
| Atrial fibrillation hospitalizations | ||||||
| Preimplantation event rate (per 100 patient‐years) | 27.6 (25.7–29.6) | 31.1 (27.2–35.4) | 0.117 | 24.2 (18.9–30.5) | 25.2 (19.8–31.6) | 0.803 |
| Postimplantation event rate (per 100 patient‐years) | 3.9 (3.4–4.4) | 1.3 (0.8–1.9) | <0.001 | 3.2 (1.9–4.9) | 0.6 (0.2–1.7) | 0.004 |
| Annualized adjusted payments ($/y) | 866 (828–953) | 241 (231–267) | <0.001 | 1488 (1175–1929) | 294 (231–386) | <0.001 |
| Heart failure hospitalizations | ||||||
| Preimplantation event rate (per 100 patient‐years) | 6.6 (5.7–7.6) | 7.4 (5.6–9.6) | 0.485 | 11.9 (8.3–16.6) | 11.2 (7.7–15.8) | 0.808 |
| Postimplantation event rate (per 100 patient‐years) | 6.4 (5.8–7.0) | 9.4 (7.9–11.0) | <0.001 | 8.4 (6.3–10.9) | 7.5 (5.5–10.0) | 0.572 |
| Annualized adjusted payments ($/y) | 1801 (1690–2062) | 2404 (2263–2733) | <0.001 | 4157 (3572–4922) | 3152 (2709–3733) | <0.001 |
Values are reported as median (quartile 1–quartile 3). Preimplantation events analyzed during the 1 year before pacemaker implantation; postimplantation events analyzed over the 3 years after pacemaker implantation. + indicates did undergo AVJA; −, did not undergo AVJA; AVJA, AV junction ablation; and RV, right ventricular (single or dual chamber).
AF Hospitalizations and Payments After Pacemaker Implantation
In the 3 years after pacemaker implantation, AVJA+ patients were associated with a significantly reduced risk for AF hospitalization compared with matched AVJA− patients, whether they were implanted with an RV (hazard ratio [HR], 0.31; 95% confidence interval [CI], 0.18–0.53; P<0.001) or a biventricular (HR, 0.20; 95% CI, 0.07–0.59; P=0.003; Figure 2A) pacemaker. Likewise, the cumulative rate of AF hospitalizations after pacemaker implantation was significantly lower for AVJA+ patients compared with matched AVJA− patients in both RV and biventricular pacemaker cohorts (Table 3). These rate reductions translated to significantly lower adjusted healthcare payments associated with AF hospitalizations, regardless of device type. Patients implanted with an RV pacemaker at AVJA were associated with a 72.2% reduction in annualized inpatient AF payments compared with matched patients with an RV pacemaker without an AVJA (Table 3). Those implanted with a biventricular pacemaker at AVJA were associated with an even greater reduction of 80.2% in annualized inpatient AF payments (Table 3).
Figure 2.
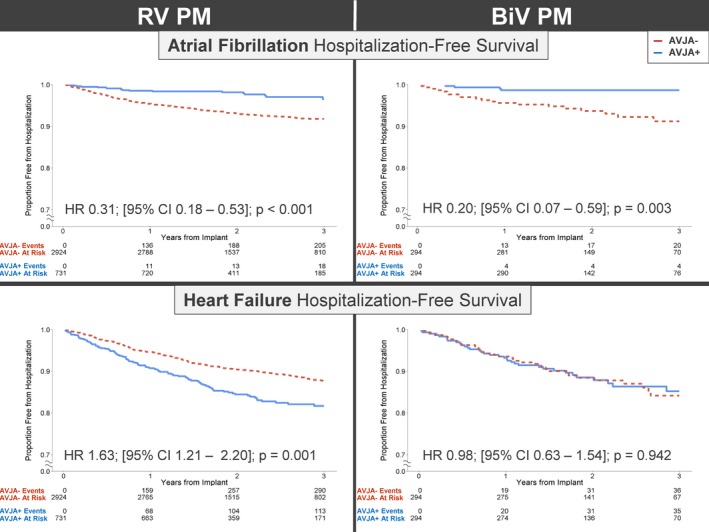
Risk of hospitalization after pacemaker implantation. Kaplan‐Meier survival curves for risk of atrial fibrillation (A) or heart failure hospitalization (B) in matched patients with vs without AV junction ablation (AVJA + and AVJA −, respectively) at pacemaker implantation. CI indicates confidence interval; HR, hazard ratio; and RV, right ventricular (single or dual chamber). BiV indicates biventricular; PM, pacemaker.
HF Hospitalizations and Payments After Pacemaker Implantation
Although the risk of HF hospitalization was significantly increased for AVJA+ compared with matched AVJA− patients implanted with RV pacemakers (HR, 1.63; 95% CI, 1.21–2.19; P=0.001), this was not the case for those implanted with biventricular pacemakers (HR, 0.98; 95% CI, 0.63–1.54; P=0.942; Figure 2B). After RV pacemaker implantation, the cumulative rate of HF hospitalizations was significantly higher for AVJA+ patients compared with the matched AVJA− cohort (Table 3). This translated to a 33.5% increase in annualized payments related to HF hospitalizations for AVJA+ versus AVJA− patients with an RV pacemaker (Table 3). In contrast, the cumulative rate of HF hospitalizations was similar between matched AVJA+ and AVJA− patients implanted with biventricular pacemakers (Table 3). For those implanted with biventricular pacemakers, AVJA+ patients were associated with 24.2% lower annualized HF hospitalization payments compared with matched AVJA− patients (Table 3).
AVJA+ Subanalysis
From the 798 patients with an RV and 363 patients with a biventricular pacemaker in the study cohort with an AVJA, propensity score matching yielded 357 patients with an RV and 357 patients with a biventricular pacemaker. The matched cohorts did not differ in baseline characteristics (Table 4) or cumulative AF and HF hospitalization rates in the 1 year before implantation (Table 5). Compared with patients implanted with RV pacemakers after AVJA, those implanted with biventricular pacemakers were associated with a significantly reduced risk of HF hospitalization (HR, 0.62; 95% CI, 0.41–0.92; P=0.017) in the 3 years after implantation (Figure 3). Minimal heterogeneity was observed within subgroups on the basis of patient age, sex, and baseline comorbidities, with all stratifications showing either a nonsignificant or a reduced risk for HF hospitalizations associated with biventricular versus RV pacemaker implantation after AVJA (Figure 4). The cumulative rate of HF hospitalizations was significantly lower for AVJA+ patients implanted with biventricular pacemakers compared with matched patients implanted with RV pacemakers (Table 5). These results correlated with a 27.2% reduction in annualized HF hospitalization payments for AVJA+ patients implanted with biventricular versus RV pacemakers (Table 5).
Table 4.
Baseline Characteristics for Matched AVJA+ Patients Implanted With RV and Biventricular Pacemakers
| Characteristics | Matched AVJA+ Patients | |||
|---|---|---|---|---|
| RV Pacemaker (N=357) | Biventricular Pacemaker (N=357) | SMD | P Value | |
| Demographics | ||||
| Follow‐up, y | 2.14 (1.55–2.89) | 2.01 (1.47–3.06) | 0.005 | 0.952 |
| Male sex | 150 (42) | 164 (46) | 0.079 | 0.327 |
| Age, y | 74.7±10.2 | 74.3±11.2 | 0.038 | 0.616 |
| Year of implant | ||||
| 2009 | 41 (11) | 37 (10) | 0.110 | 0.709 |
| 2010 | 85 (24) | 98 (27) | ||
| 2011 | 105 (29) | 92 (26) | ||
| 2012 | 113 (32) | 115 (32) | ||
| 2013 | 13 (4) | 15 (4) | ||
| US region | ||||
| Northeast | 48 (13) | 50 (14) | 0.053 | 0.919 |
| North Central | 137 (38) | 143 (40) | ||
| South | 127 (36) | 124 (35) | ||
| West | 45 (13) | 40 (11) | ||
| Unknown | 0 (0) | 0 (0) | ||
| Comorbidities | ||||
| Heart failure | 169 (47) | 160 (45) | 0.051 | 0.548 |
| VT/VF | 46 (13) | 45 (13) | 0.008 | 1.000 |
| Coronary artery disease | 190 (53) | 178 (50) | 0.067 | 0.410 |
| Hypertension | 282 (79) | 293 (82) | 0.078 | 0.345 |
| Cerebrovascular disease | 85 (24) | 69 (19) | 0.109 | 0.172 |
| Diabetes mellitus | 108 (30) | 104 (29) | 0.025 | 0.806 |
| Valve disease | 151 (42) | 163 (46) | 0.068 | 0.407 |
| Peripheral vascular disease | 72 (20) | 67 (19) | 0.035 | 0.705 |
| Chronic pulmonary disease | 142 (40) | 151 (42) | 0.051 | 0.543 |
| Chronic kidney disease | 48 (13) | 58 (16) | 0.079 | 0.343 |
| Rheumatic disease | 22 (6) | 14 (4) | 0.103 | 0.231 |
| Peptic ulcer disease | 8 (2) | 7 (2) | 0.02 | 1.000 |
| Liver disease | 26 (7) | 17 (5) | 0.106 | 0.208 |
| Hypothyroidism | 88 (25) | 78 (22) | 0.066 | 0.425 |
| Cancer | 44 (12) | 47 (13) | 0.025 | 0.822 |
| Dementia | 10 (3) | 7 (2) | 0.055 | 0.623 |
| Depression | 39 (11) | 36 (10) | 0.027 | 0.807 |
| AIDS/HIV | 0 (0) | 0 (0) | 0.000 | 1.000 |
| Hemiplegia/paraplegia | 4 (1) | 2 (1) | 0.061 | 0.682 |
| Obesity | 37 (10) | 46 (13) | 0.079 | 0.350 |
Values are reported as median (quartile 1–quartile 3), mean±SD, and count (percentage). + indicates did undergo AVJA; AVJA, AV junction ablation; RV, right ventricular (single or dual chamber); SMD, standardized mean difference; and VT/VF, ventricular tachycardia/ventricular fibrillation.
Table 5.
Cumulative HF Hospitalization Rates and Annualized Adjusted Payments for Matched AVJA+ Patients Implanted With RV and Biventricular Pacemakers
| Variables | RV Pacemaker Group (N=357) | Biventricular Pacemaker Group (N=357) | P Value |
|---|---|---|---|
| Preimplantation event rate (per 100 patient‐years) | 7.8 (5.2–11.3) | 10.1 (7.1–14.0) | 0.319 |
| Postimplantation event rate (per 100 patient‐years) | 10.2 (8.1–12.8) | 6.5 (4.8–8.6) | 0.013 |
| Adjusted annualized payments ($/y) | 3513 (2472–4699) | 2556 (1800–3417) | <0.001 |
Values are reported as median (quartile 1–quartile 3). Preimplantation events analyzed during the 1 year before pacemaker implantation; postimplantation events analyzed over the 3 years after pacemaker implantation. + indicates did undergo AVJA; AVJA, AV junction ablation; HF, heart failure; and RV, right ventricular (single or dual chamber).
Figure 3.
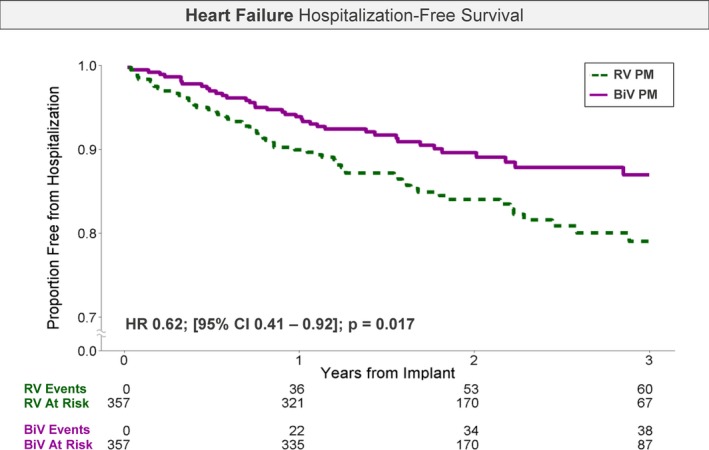
Risk of heart failure hospitalization after AV junction ablation (AVJA). Kaplan‐Meier survival curve for risk of heart failure hospitalization in matched patients implanted with a biventricular vs a right ventricular (RV; single or dual chamber) pacemaker at AVJA. CI indicates confidence interval; and HR, hazard ratio.
Figure 4.
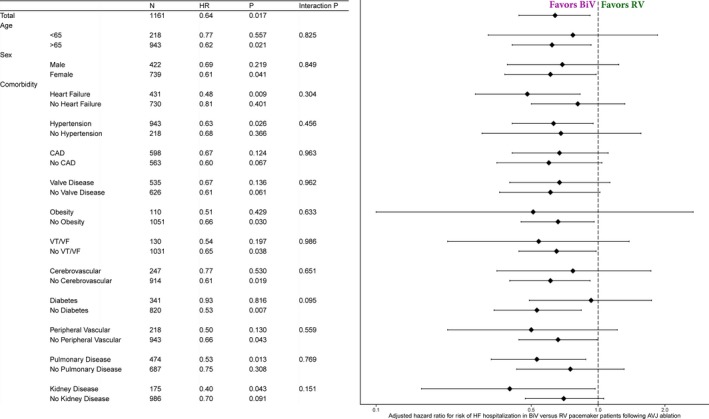
Forest plot showing adjusted risk of heart failure (HF) hospitalization after AV junction ablation (AVJA). Propensity score–adjusted risk of HF hospitalization in patients implanted with a biventricular vs a right ventricular (RV; single or dual chamber) pacemaker at AVJA. CAD indicates coronary artery disease; HR, hazard ratio; and VT/VF, ventricular tachycardia/ventricular fibrillation. BiV indicates biventricular; PM, pacemaker.
During a median of 2.08 (quartile 1–quartile 3, 1.51−2.95) years after AVJA, 60 patients (16.8%) with an RV pacemaker and 38 patients (10.6%) with a biventricular pacemaker were hospitalized for HF (P=0.022). In both device groups, most hospitalized patients incurred only 1 or 2 HF hospitalizations during the follow‐up, with only 5 patients incurring between 3 and 5 total hospitalizations (Figure 5). These results suggest that the observed difference in HF hospitalization rates may be attributed to the higher proportion of patients with an RV pacemaker hospitalized, rather than an accumulation of hospitalizations in either group.
Figure 5.
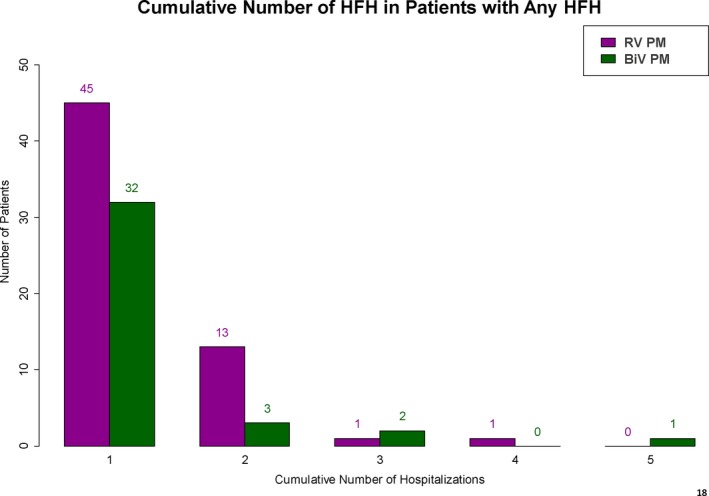
Bar plot showing the distribution of cumulative heart failure hospitalizations (HFHs) during a median 2.08 years of follow‐up after AV junction ablation (AVJA). After AVJA, the cumulative number of HFHs in matched biventricular and right ventricular (RV; single or dual chamber) pacemaker cohorts. BiV indicates biventricular; PM, pacemaker.
Discussion
This retrospective investigation using data from the Truven Health MarketScan Commercial Claims and Medicare Supplemental databases represents the largest analysis to date of patients undergoing AVJA and concomitant RV or biventricular pacemaker implantation. In addition, the 3‐year follow‐up represents the longest reported follow‐up in an AVJA patient cohort. The principal findings of this study are as follows: (1) AVJA was associated with a significantly reduced likelihood and rate of AF‐related hospitalization, irrespective of whether an RV or a biventricular pacemaker was implanted; (2) RV pacing was associated with a significantly greater likelihood and rate of HF hospitalizations after AVJA, whereas this was not observed in patients with a biventricular pacemaker; (3) after AVJA, implantation of a biventricular pacemaker was associated with a 38% reduction in HF hospitalizations compared with patients with an RV pacemaker; and (4) this translated into a 27% reduction in annual payments related to HF hospitalizations.
Although a single‐center retrospective study suggested that AVJA, followed by RV pacing, was not associated with an adverse impact on left ventricular (LV) ejection fraction,16 this was not confirmed by a randomized clinical trial, especially in patients with underlying LV dysfunction or symptomatic HF.4 Furthermore, the deleterious effect of RV pacing was mitigated by the use of biventricular pacing. Around the same time, Brignole et al randomized 56 patients with permanent AF who were undergoing AVJA and implantation of a biventricular pacing system to undergo either RV‐ or LV‐only pacing.6 Three months later, the patients were crossed over to the other arm. Subsequently, the patients were randomized to RV or biventricular pacing and then crossed over 1 final time 3 months later. The primary end points were quality of life and exercise capacity at the end of each 3‐month period. Much of the observed benefit was a direct result of the AVJA itself; LV or biventricular pacing provided, at best, only modest additional benefit.
These conflicting results led several investigators to conduct randomized clinical trials. Orlov et al randomized 108 patients in a 4:1 manner to biventricular versus RV pacing after AVJA.8 Six months after AVJA, RV pacing was associated with a significantly greater increase in left atrial volume, LV end‐systolic volume, and LV mass compared with biventricular pacing. To assess hard clinical outcomes, Brignole et al reported on 186 patients with permanent AF who underwent AVJA and were then randomized to receive either biventricular or RV‐only pacing.5 The primary end point was a composite of death from HF, hospitalization attributable to HF, and worsened HF, with a median follow‐up of 20 months. The biventricular group had a 63% reduction in the composite outcome, which was driven by a 73% reduced likelihood of worsening HF and an 80% reduced likelihood of HF hospitalization. The benefit of biventricular was observed in both patients with and without LV dysfunction.
These prior studies have been limited by small sample size, the disparate timing between pacemaker implantation and AVJA, short duration of follow‐up (most commonly just 6 months), and lack of comparison to a group of patients who did not undergo AVJA. In contrast, our study has several important advantages. First, this is the largest study reported to date of patients undergoing AVJA. Second, we have a matched population of patients who did not undergo AVJA. In addition, for the first time ever, we have event rate data on these patients for 1 year before pacemaker implantation. This allowed us to make a more meaningful comparison of outcomes between patients with AF who did or did not undergo AVJA, stratified by whether they received an RV or a biventricular pacemaker. Before pacemaker implantation, the RV and biventricular pacemaker cohorts had a similar number of AF‐ and HF‐related hospitalizations. Subsequently, hospitalization attributable to AF was less common in patients who underwent AVJA, irrespective of whether they received an RV or a biventricular pacemaker. In contrast, HF hospitalizations increased dramatically in patients who underwent AVJA followed by RV pacing. This adverse effect was not observed in patients who received a biventricular pacemaker. In an analysis of a matched cohort, biventricular pacing was associated with a 38% reduction in HF hospitalization, consistent with data reported from a prior meta‐analysis.17 Third, payments in patients receiving a biventricular pacemaker after an AVJA were $957 per year lower than in those receiving an RV pacemaker, a decrease of 27.2% in HF hospitalization–related costs. Previous analyses of MarketScan data found total annual medical expenditures to be $11 528 in patients with AF18 and $11 394 in patients with HF,19 so $957 accounts for ≈8% of the annual payments in patients with these conditions. These savings pertain solely to avoidance of HF hospitalizations and are likely underestimates of total savings associated with reducing HF hospitalizations, because they do not account for other expenses incurred by patients experiencing HF, such as increase in medication, home care, and loss of productivity. Total medical expenditures in patients with congestive HF can range between $33 000 and $40 000.19, 20 In the RV group, when patients required an HF hospitalization, most experienced 1 or 2 hospitalizations; this was enough to result in the increased expenditure in this patient population.
Limitations
The limitations of this type of analysis have been reported previously.2 We have no information about LV ejection fraction and, thus, cannot distinguish between HF with preserved versus reduced ejection fraction. Similarly, because we used ICD‐9 codes to diagnose AF, we cannot distinguish paroxysmal from persistent and permanent forms of AF, and there is no way to assess the success of AF management. We also cannot reliably determine the pacemaker implantation indication. Lack of information on ejection fraction, pacemaker indication, and AF may introduce confounding. Finally, mortality data are not available in the data set used for this analysis. When MarketScan enrollment ends for a particular patient, we cannot determine whether this was because of death or other reasons, such as cancellation in health insurance coverage or transfer to Medicare. However, because the primary end point of an inpatient or outpatient HF diagnosis is likely to precede an HF‐related mortality event, it is expected that our analysis reflects the real‐world incidence of new‐onset HF after pacemaker implantation.2
Conclusions
In a large national cohort of patients with AF, those who underwent AVJA had a significantly lower likelihood of hospitalization for AF, irrespective of whether an RV or a biventricular pacemaker was implanted. However, AVJA was associated with a marked increase in HF hospitalizations in patients implanted with an RV pacemaker, whereas this was not observed with biventricular pacing. Similarly, a recent study found that His‐bundle pacing after AVJA significantly improved echocardiographic measurements, New York Heart Association symptom class, and requirement for diuretics in patients with AF with a narrow QRS, irrespective of whether the LV ejection fraction was preserved or reduced.21 Thus, we await the results of ongoing studies (eg, NCT0280546522) that compare selective conduction system pacing with biventricular pacing in this patient population to define the optimal post‐AVJA pacing strategy.
Sources of Funding
This research was supported by Abbott.
Disclosures
Mittal and Hoskins report receiving consulting fees from Abbott. Prillinger reports owning stock in Abbott and Medtronic and receives a salary from Abbott. Roberts reports receiving a salary from Abbott. Nabutovsky reports owning stock in and receiving a salary from Abbott. Musat and Merchant have no disclosures to report.
(J Am Heart Assoc. 2017;6:e007270 DOI: 10.1161/JAHA.117.007270.)29180458
References
- 1. Akerstrom F, Rodriguez‐Manero M, Pachon M, Puchol A, Fernandez‐Lopez XA, Martinez‐Sande L, Valderrabano M, Arias MA. Atrioventricular junction ablation in atrial fibrillation: choosing the right patient and pacing device. J Atr Fibrillation. 2015;8:31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wood MA, Brown‐Mahoney C, Kay GN, Ellenbogen KA. Clinical outcomes after ablation and pacing therapy for atrial fibrillation: a meta‐analysis. Circulation. 2000;101:1138–1144. [DOI] [PubMed] [Google Scholar]
- 3. Merchant FM, Hoskins MH, Musat DL, Prillinger JB, Roberts GJ, Nabutovsky Y, Mittal S. Incidence and time course for developing heart failure with high‐burden right ventricular pacing. Circ Cardiovasc Qual Outcomes. 2017;10:e003564. [DOI] [PubMed] [Google Scholar]
- 4. Doshi RN, Daoud EG, Fellows C, Turk K, Duran A, Hamdan MH, Pires LA; for the PAVE Study Group. Left ventricular‐based cardiac stimulation Post AV Nodal Ablation Evaluation (The PAVE Study). J Cardiovasc Electrophysiol. 2005;16:1160–1165. [DOI] [PubMed] [Google Scholar]
- 5. Brignole M, Botto G, Mont L, Iacopino S, De Marchi G, Oddone D, Luzi M, Tolosana JM, Navazio A, Menozzi C. Cardiac resynchronization therapy in patients undergoing atrioventricular junction ablation for permanent atrial fibrillation: a randomized trial. Eur Heart J. 2011;32:2420–2429. [DOI] [PubMed] [Google Scholar]
- 6. Brignole M, Gammage M, Puggioni E, Alboni P, Raviele A, Sutton R, Vardas P, Bongiorni MG, Bergfeld L, Menozzi C, Musso G; Optimal Pacing SITE (OPSITE) Study Investigators. Comparative assessment of right, left, and biventricular pacing in patients with permanent atrial fibrillation. Eur Heart J. 2005;26:712–722. [DOI] [PubMed] [Google Scholar]
- 7. Leclerq C, Walker S, Linde C, Clementy J, Marshall AJ, Ritter P, Djiane P, Mabo P, Levy T, Gadler F, Bailleul C, Daubert JC; on behalf of the MUSTIC Study Group. Comparative effects of permanent biventricular and right‐univentricular pacing in heart failure patients with chronic atrial fibrillation. Eur Heart J. 2002;23:1780–1787. [DOI] [PubMed] [Google Scholar]
- 8. Orlov MV, Gardin JM, Slawsky M, Bess RL, Cohen G, Bailey W, Plumb V, Flathmann H, de Metz K. Biventricular pacing improves cardiac function and prevents further left atrial remodeling in patients with symptomatic atrial fibrillation after atrioventricular node ablation. Am Heart J. 2010;159:264–270. [DOI] [PubMed] [Google Scholar]
- 9. Hansen L, Chang S. White Paper—Health Research Data for the Real World: The MarketScan Databases. Ann Arbor, MI: Truven Health Analytics; 2012. [Google Scholar]
- 10. Lad SP, Petraglia FW III, Kent AR, Cook S, Murphy KR, Dalal N, Karst E, Staats P, Sharan A. Longer delay from chronic pain to spinal cord stimulation results in higher healthcare resource utilization. Neuromodulation. 2016;19:469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ladapo JA, Turakhia MP, Ryan MP, Mollenkopf SA, Reynolds MR. Health care utilization and expenditures associated with remote monitoring in patients with implantable cardiac devices. Am J Cardiol. 2016;117:1455–1462. [DOI] [PubMed] [Google Scholar]
- 12. Nazarian S, Reynolds MR, Ryan MP, Wolff SD, Mollenkopf SA, Turakhia MP. Utilization and likelihood of radiologic diagnostic imaging in patients with implantable cardiac defibrillators. J Magn Reson Imaging. 2016;43:115–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Birman‐Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD‐9‐CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2015;43:480–485. [DOI] [PubMed] [Google Scholar]
- 14. Quan H, Sundararajan V, Halfon P, Fong A, Burnard B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD‐9‐CM and ICD‐10 administrative data. Med Care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 15. Yang D, Dalton JE. A unified approach to measuring the effect size between two groups using SAS® . SAS Global Forum. 2012;335:1–6. [Google Scholar]
- 16. Chen L, Hodge D, Jahangir A, Ozcan C, Trusty J, Friedman P, Rea R, Bradley D, Brady P, Hammill S, Hayes D, Shen WK. Preserved left ventricular ejection fraction following atrioventricular junction ablation and pacing for atrial fibrillation. J Cardiovasc Electrophysiol. 2008;19:19–27. [DOI] [PubMed] [Google Scholar]
- 17. Stavrakis S, Garabelli P, Reynolds DW. Cardiac resynchronization therapy after atrioventricular junction ablation for symptomatic atrial fibrillation: a meta‐analysis. Europace. 2012;14:1490–1497. [DOI] [PubMed] [Google Scholar]
- 18. Mansour M, Karst E, Heist EK, Dalal N, Wasfy JH, Packer DL, Calkins H, Ruskin JN, Mahapatra S. The impact of first procedure success rate on the economics of atrial fibrillation ablation. JACC Clin Electrophysiol. 2016;3:129–138. [DOI] [PubMed] [Google Scholar]
- 19. Martinson M, Bharmi R, Dalal N, Abraham WT, Adamson PB. Pulmonary artery pressure‐guided heart failure management: US cost‐effectiveness analyses using the results of the CHAMPION clinical trial. Eur J Heart Fail. 2017;19:652–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dall TM, Blanchard TD, Gallo PD, Semilla AP. The economic impact of Medicare part D on congestive heart failure. Am J Manag Care. 2013;19:S97–S100. [PubMed] [Google Scholar]
- 21. Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA. Benefits of permanent His bundle pacing combined with atrioventricular node ablation in atrial fibrillation patients with heart failure with preserved and reduced left ventricular ejection fraction. J Am Heart Assoc. 2017;6:e005309 DOI: 10.1161/JAHA.116.005309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. ClinicalTrials.gov [Internet] . Bethesda (MD): National Library of Medicine (US). 2000 Feb 29 ‐ . Identifier NCT02805465, Comparison of His Bundle Pacing and Bi‐Ventricular Pacing in Heart Failure With Atrial Fibrillation; 2016 May 30 [cited 2017 Jul 17]; [about 8 screens]. Available from: https://clinicaltrials.gov/show/NCT02805465


