Abstract
Background
Lipoprotein(a) (Lp[a]) is proatherosclerotic and prothrombotic, causally related to coronary disease, and associated with other cardiovascular diseases. The association of Lp(a) with incident atrial fibrillation (AF) and with ischemic stroke among individuals with AF remains to be elucidated.
Methods and Results
In the community‐based ARIC (Atherosclerosis Risk in Communities) study cohort, Lp(a) levels were measured by a Denka Seiken assay at visit 4 (1996–1998). We used multivariable‐adjusted Cox models to compare AF and ischemic stroke risk across Lp(a) levels. First, we evaluated incident AF in 9908 participants free of AF at baseline. AF was ascertained by electrocardiography at study visits, hospital International Statistical Classification of Diseases, 9th Revision (ICD‐9) codes, and death certificates. We then evaluated incident ischemic stroke in 10 127 participants free of stroke at baseline. Stroke was identified by annual phone calls, hospital ICD‐9 Revision codes, and death certificates. The baseline age was 62.7±5.6 years. Median Lp(a) levels were 13.3 mg/dL (interquartile range, 5.2–39.7 mg/dL). Median follow‐up was 13.9 and 15.8 years for AF and stroke, respectively. Lp(a) was not associated with incident AF (hazard ratio, 0.98; 95% confidence interval, 0.82–1.17), comparing those with Lp(a) ≥50 with those with Lp(a) <10 mg/dL. High Lp(a) was associated with a 42% relative increase in stroke risk among participants without AF (hazard ratio, 1.42; 95% confidence interval, 1.07–1.90) but not in those with AF (hazard ratio, 1.06; 95% confidence interval, 0.70–1.61 [P interaction for AF=0.25]). There were no interactions by race or sex. No association was found for cardioembolic stroke subtype.
Conclusions
High Lp(a) levels were not associated with incident AF. Lp(a) levels were associated with increased ischemic stroke risk, primarily among individuals without AF but not in those with AF.
Keywords: atrial fibrillation, cardioembolic stroke, epidemiology, lipoprotein, lipoprotein (a), risk factor, stroke
Subject Categories: Epidemiology, Ischemic Stroke, Atrial Fibrillation, Lipids and Cholesterol
Clinical Perspective
What Is New?
High lipoprotein(a) levels are not associated with incident atrial fibrillation.
Lipoprotein(a) levels are associated with increased ischemic stroke risk, primarily in patients without atrial fibrillation.
What Are the Clinical Implications?
Elevated lipoprotein(a) is primarily associated with diseases directly related to atherosclerosis and is not a risk factor for atrial fibrillation.
The association of lipoprotein(a) with ischemic stroke is primarily driven by thrombotic (atherosclerotic) stroke.
Lipoprotein(a) (Lp[a]) is a lipoprotein moiety that has similar lipid composition to low‐density lipoprotein and contains the distinguishing apolipoprotein(a) covalently bound to apoB‐100.1 Apolipoprotein(a) is structurally homologous to plasminogen2 and inhibits tissue factor pathway inhibitor.3 In several cohort studies and meta‐analyses, Lp(a) was associated with an increased incidence of coronary heart disease (CHD) and stroke.4, 5, 6, 7, 8 Over the past 2 decades, Lp(a) has emerged as an important cardiovascular risk factor.9 It has dual mechanisms for promoting cardiovascular disease through both its proatherosclerotic (as a lipoprotein) and prothrombotic (via its similarity to plasminogen) properties. Lp(a) is causally related to CHD in Mendelian randomization studies.10 Lp(a) has adverse effects on the cardiovascular system outside of atherosclerosis and atherothrombosis, such as calcific aortic sclerosis.11
At this time, however, the link between Lp(a) and atrial fibrillation (AF) is uncertain. In a case‐control study from Spain, Lp(a) levels were not associated with AF (n=202).12 Lp(a) levels were not associated with AF recurrence after electrical cardioversion in a cohort of 79 patients and 2 years of follow‐up.13 However, prospective associations of Lp(a) levels with incident AF have not been studied to date. Lp(a) levels are associated with atherosclerotic cardiovascular disease, which, in turn, is associated with incident AF.14, 15 Other markers of atherosclerosis such as coronary calcium score and carotid intima‐ media thickness have been associated with AF.16, 17 The role of Lp(a) as an independent risk factor for AF remains to be elucidated.
Blacks have ≈3‐fold higher Lp(a) levels compared with whites, and women have higher Lp(a) levels by 15% to 20% compared with men.8 Despite higher Lp(a) levels, blacks18, 19 and women20 have a lower incidence of AF, and little is known on whether race or sex could exhibit effect modification on Lp(a)‐related risk. Furthermore, there are limited data on the associations of Lp(a) and the risk of AF‐related stroke. In a case‐control study, patients with AF and cardioembolic stroke had 2‐fold higher Lp(a) levels compared with those with AF and noncardioembolic stroke (n=40).21 In patients with AF, Lp(a) levels were independently associated with the presence of left atrial thrombus22 or a recent thromboembolic event23 (n=150 and n=172). However, prospective associations of Lp(a) levels with incidence of AF‐related stroke have not been studied to date.
Our study had two major aims. The primary aim of this study was to evaluate for prospective associations between Lp(a) levels and incident AF and to assess for potential interactions with race and sex. We hypothesized that elevated Lp(a) levels would be associated with a higher incidence of AF, independently of traditional AF risk factors. We also hypothesized that being black or a woman would attenuate the AF risk conveyed by Lp(a). The secondary aim of our study was to assess for prospective associations of Lp(a) levels and stroke in persons with or without AF. For this secondary aim, we hypothesized that elevated Lp(a) levels would be associated with higher rates of incident ischemic stroke independently of CHA2DS2‐VASc score and that this association would be stronger in participants with a history of prevalent or incident AF compared with those without AF. The ARIC (Atherosclerosis Risk in Communities) study, a community‐based, prospective cohort of individuals with long‐term follow‐up for both AF and stroke events, is uniquely suited to test our hypotheses given its biracial composition.
Materials and Methods
This analysis is based on data from the ARIC study cohort. The data, analytic methods, and study materials can be made available to other researchers upon request, for purposes of reproducing the results, in accordance with ARIC study policies.24
Study Cohort
The ARIC study is a mostly biracial, community‐based, prospective epidemiological trial of cardiovascular disease. A complete description of the study design, objectives, and sampling strategy has been previously described.25 Briefly, the ARIC study enrolled 15 792 participants from 1987 to 1989. Participants were aged 45 to 64 years and came from 4 communities in the United States (Washington County, MD; the suburbs of Minneapolis, MN; Jackson, MS; and Forsyth County, NC). After baseline assessment, participants took part in up to 4 additional examinations (1990–1992, 1993–1995, 1996–1998, and 2011–2013). In addition, ARIC study participants received annual follow‐up calls to screen for hospitalizations or major changes in their health status. The ARIC study protocols were approved by the institutional review boards at all ARIC study sites and the Coordinating Center. All participants provided written informed consent at each study visit. For this analysis, we used ARIC visit 4 (1996–1998), the time of Lp(a) measurement, as baseline. Visit 4 included 11 656 participants.
For our primary aim we included all ARIC study participants who were free of prevalent or incident AF occurring before visit 4. Exclusion criteria were: an AF event at or before visit 4 (n=293); missing Lp(a) levels (n=165); racial/ethnic group other than white or black (n=31); blacks from the MN and MD field centers (n=37; low numbers limited our ability to adjust for their race‐center groups); missing covariates (n=1221); or follow‐up that ended on or before visit 4 (n=1). After exclusions, 9908 participants were included in our primary analysis for incident AF (43.9% men, 21.6% blacks) (Figure 1).
Figure 1.
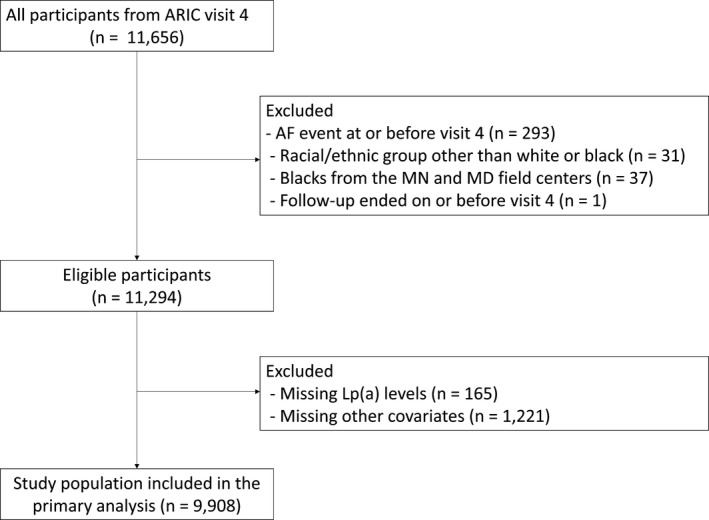
Participant flow diagram for aim 1 (incident atrial fibrillation [AF]). ARIC indicates Atherosclerosis Risk in Communities study; Lp(a), lipoprotein(a).
For our secondary aim, we included all ARIC study participants who were free of prevalent or incident stroke before visit 4. Exclusion criteria were: ischemic stroke at or before visit 4 (n=139); missing Lp(a) levels (n=167); racial/ethnic group other than white or black (n=31); blacks from the MN and MD field centers (n=37); missing covariates (n=1153); or follow‐up that ended on or before visit 4 (n=2). After exclusions, we included 10 127 participants (44.1% men, 21.1% blacks) in our secondary analysis for incident stroke (Figure 2).
Figure 2.

Participant flow diagram for aim 2 (incident stroke, stratified by history of atrial fibrillation vs no history of atrial fibrillation. ARIC indicates Atherosclerosis Risk in Communities study; Lp(a), lipoprotein(a).
Lp(a) Measurement
Lp(a) levels were measured in EDTA plasma collected at ARIC study visit 4 using the Denka Seiken assay (Denka Seiken Co). This is a well‐validated assay, with good reproducibility (coefficient of variation, 1.26–2.22%), that yields robust results and is generally insensitive to apolipoprotein(a) size heterogeneity.26 As per prior ARIC study analyses,8 Lp(a) levels were examined: (1) as a continuous logarithmically transformed variable, and (2) as 5 prespecified Lp(a) categories defined by the arbitrary thresholds of ≤10, >10 to ≤20, >20 to ≤30, >30 to ≤50, and >50 mg/dL.
AF Ascertainment
Our primary outcome was first occurrence of AF (after visit 4) through December 31, 2011. We defined the incidence date of AF as the date for the first ECG showing AF, the first hospital discharge coded as AF, or when AF was listed as a cause of death, whichever occurred earlier. AF was ascertained by 3 different sources: ECGs performed during study visits, hospital discharge International Statistical Classification of Diseases (ICD) codes, and death certificates.19 At each ARIC study visit, a 10‐second 12‐lead ECG was obtained and transmitted to the ARIC ECG Reading Center for coding, interpretation, and storage. All abnormal ECGs were subsequently adjudicated by a trained cardiologist, and both atrial flutter and AF were coded as AF.27 Hospitalizations were detected with annual follow‐up telephone calls and review of local hospital discharges. AF events were identified by the presence of the ICD, 9th Revision, Clinical Modification code of 427.31 (AF) or 427.32 (atrial flutter), listed as a discharge diagnostic code at any position. We excluded AF events associated with cardiac surgery. AF events were also identified if ICD‐9 code 427.3 or ICD‐10 code I48 was listed as a cause of death. More than 98% of incident AF cases were identified from hospital discharge codes, and less than 1% of AF cases were identified from death certificates.28 The sensitivity and specificity of incident AF by hospital discharge was evaluated to be over 80% and 97%.19
Stroke Ascertainment
Our secondary outcome was incident ischemic stroke through December 31, 2013. Stroke events were identified by annual phone calls, hospital ICD‐9 codes 430 to 438 until 1997 and ICD‐9 codes 430 to 436 afterwards (listed as a discharge diagnostic code at any position), or by death certificates. Trained ARIC study personnel abstracted from hospital records, stroke signs and symptoms, and cerebrovascular imaging findings. On the basis of National Survey of Stroke criteria,29 a computer algorithm and a panel of ARIC study physicians (which included a neurologist) categorized all potential stroke events (hospitalized or out‐of‐hospital stroke deaths) as definite or possible strokes; an additional study reviewer adjudicated discrepancies. Strokes were subclassified as ischemic versus hemorrhagic. For this analysis, we included only ischemic strokes. In addition, the ARIC study physicians further classified ischemic strokes into thrombotic, lacunar, or cardioembolic subtypes, according to criteria adopted from the National Survey of Stroke subtype classification.29, 30 Given that the aim of this study was in regards to AF‐related stroke outcomes, we considered only cardioembolic strokes in a sensitivity analysis.
Assessment of Other Covariates
We included demographic and clinical variables collected during ARIC study visit 4 as follows: age, sex, race, study site, systolic blood pressure (BP), diastolic BP, hypertension treatment, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, N‐terminal pro–B type natriuretic peptide, diabetes mellitus, smoking, personal history of CHD (history of myocardial infarction, myocardial infarction indicated on baseline ECG, or revascularization), personal history of stroke, personal history of systemic embolism, personal history of heart failure (HF), and personal history of peripheral artery disease. We calculated the CHA2DS2‐VASc score.31 Hypertension was defined as systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg, or BP medication use in the past 2 weeks. Diabetes mellitus was considered present if one of the following criteria was met: (1) fasting glucose ≥126 mg/dL or nonfasting glucose ≥200 mg/dL, (2) self‐reported physician diagnosis of diabetes mellitus, or (3) current use of medication for diabetes mellitus. Prevalent HF was identified by the Gothenburg criteria during visit 132 or an incident HF‐related admission ascertained by ARIC study investigators between visit 1 and 4. Peripheral artery disease was defined as an ankle‐brachial index <0.9 assessed at visit 4 or peripheral artery disease–related hospitalization, amputation, leg revascularization, or intermittent claudication as assessed by annual questionnaire.33
Statistical Analysis
We presented baseline characteristics of study participants as mean±SD for continuous variables that were normally distributed, median (interquartile range) for continuous variables that were not normally distributed, and proportions for categorical variables, across the 5 Lp(a) categories. We used progressively adjusted multivariable Cox proportional hazards models to estimate the hazard ratios (95% confidence intervals) of incident AF and incident stroke across different Lp(a) levels, as further described below. We performed analyses using Lp(a) as a categorical variable with the 5 defined groups and as a logarithmically transformed continuous variable.
Primary outcome (incident AF)
We assessed the association of Lp(a) with incident AF using multivariable‐adjusted analyses for 3 prespecified Cox models as follows: model 1 (demographics) adjusted for age, sex, race‐center groups (whites‐Minnesota; whites‐Maryland; whites‐North Carolina; blacks‐North Carolina; blacks‐Mississippi). Model 2 (+CVD risk factors and prevalent CVD) adjusted for model 1 variables+smoking, systolic and diastolic BP, treatment for hypertension, heart rate, height, body mass index, left ventricular hypertrophy, PR interval, prevalent HF, CHD, and diabetes mellitus. Model 3 (+other lipids and BNP) included model 2+low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, lipid‐lowering medication and log‐transformed N‐terminal pro–B type natriuretic peptide. We assessed for effect modification of AF risk, related to Lp(a) levels, by race and sex using Wald tests.
Secondary outcome (incident stroke)
The association of Lp(a) with stroke has already been published for the overall ARIC study cohort.8 However, a priori, we planned to stratify results among those with a history of AF (prevalent or incident during the ARIC study) versus those with no AF history, to see whether the association of Lp(a) with incident ischemic stroke was stronger among those with an AF history. We considered AF (occurring at any time during ARIC study follow‐up) as a time‐dependent covariate. We assessed for interactions of the Lp(a)‐related stroke risk with history of AF status. Stratified by AF status, we performed multivariable‐adjusted analysis in 3 prespecified Cox models as follows: model 1 (demographics) adjusted for age, sex, and race‐center groups. Model 2 (+CVD risk factors and prevalent CVD) adjusted for model 1 covariates+smoking, systolic and diastolic BP, treatment for hypertension, heart rate, height, body mass index, left ventricular hypertrophy, PR interval, prevalent HF, prevalent CAD, diabetes mellitus, and CHA2DS2‐VASc score. Model 3 (+other lipids) included model 2+low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, and lipid‐lowering medication.
We also used restricted cubic splines to visually depict the associations between Lp(a) levels and risk for AF and stroke for each outcome. We confirmed the assumption of proportional hazards using Schoenfeld residuals and graphic methods (ln[‐ln] survival plots). We performed statistical analysis using Stata 14 (StataCorp). All P values were 2‐sided and we set the α criterion for statistical significance at 0.05.
Results
Baseline Characteristics
The mean age of the study population was 62.7 years (5.6 years). Baseline characteristics, stratified by Lp(a) levels, are shown in Table 1. Women had higher Lp(a) levels. Low‐density lipoprotein cholesterol levels and the percentage of participants taking lipid‐lowering medications increased with increasing Lp(a) levels. Prevalence of CHD was higher in participants with higher Lp(a) levels.
Table 1.
Baseline Characteristics of the Study Cohort (ARIC Study Visit 4 1996–1998)a
| Characteristic | Lp(a) Categories, mg/dL | P Valueb | ||||
|---|---|---|---|---|---|---|
| ≤10 | >10 to 20 | >20 to 30 | >30 to 50 | >50 | ||
| No. | 4229 | 1732 | 887 | 1177 | 1883 | |
| Age, y | 62.8 (5.7) | 62.8 (5.5) | 62.6 (5.7) | 62.6 (5.7) | 62.5 (5.6) | 0.3 |
| Men, No. (%) | 1999 (47.3) | 772 (44.6) | 373 (42.1) | 500 (42.5) | 702 (37.3) | <0.001 |
| Black, No. (%) | 284 (6.7) | 338 (19.5) | 357 (40.2) | 524 (44.5) | 633 (33.6) | <0.001 |
| Current smoking, No. (%) | 604 (14.3) | 274 (15.8) | 140 (15.8) | 162 (13.8) | 287 (15.2) | <0.001 |
| SBP, mm Hg | 126.0 (18.1) | 126.7 (19.0) | 128.7 (18.6) | 129.8 (20.0) | 127.8 (19.4) | <0.001 |
| DBP, mm Hg | 70.2 (9.8) | 71.0 (10.2) | 71.9 (10.5) | 72.3 (10.7) | 71.3 (10.8) | <0.001 |
| Hypertension, No. (%) | 1765 (41.9) | 752 (43.5) | 446 (50.5) | 635 (54.1) | 907 (48.3) | <0.001 |
| Treatment for hypertension, No. (%) | 1598 (37.8) | 651 (37.6) | 380 (42.8) | 572 (48.6) | 855 (45.4) | <0.001 |
| Heart rate, beats per min | 62.5 (9.6) | 62.5 (9.8) | 63.1 (10.0) | 63.2 (10.7) | 62.8 (9.8) | 0.16 |
| Height, cm | 167.9 (9.5) | 167.8 (9.4) | 167.4 (9.4) | 167.7 (8.9) | 167.0 (9.0) | 0.01 |
| BMI, kg/m2 | 28.4 (5.2) | 28.4 (5.4) | 29.0 (5.8) | 29.2 (5.7) | 28.8 (5.8) | <0.001 |
| ECG LVH, No. (%) | 120 (2.8) | 62 (3.6) | 45 (5.1) | 68 (5.8) | 87 (4.6) | <0.001 |
| PR interval, ms | 166.3 (26.1) | 165.5 (25.7) | 168.1 (27.0) | 168.4 (27.5) | 167.5 (26.9) | 0.01 |
| LDL‐C, mg/dL | 117.3 (32.0) | 123.2 (32.4) | 124.9 (35.1) | 125.3 (34.7) | 132.6 (32.6) | <0.001 |
| HDL‐C, mg/dL | 49.3 (16.6) | 49.7 (15.3) | 51.3 (16.3) | 51.4 (16.7) | 52.6 (16.8) | <0.001 |
| Triglycerides, mg/dL | 146.5 (72.3) | 132.1 (62.4) | 125.7 (59.2) | 127.8 (62.6) | 129.0 (61.0) | <0.001 |
| Pro‐NT‐BNP, pg/mLc | 65.0 (33.4–123.8) | 64.1 (30.0–120.5) | 60.4 (28.3–122.6) | 67.0 (33.1–127.3) | 65.0 (33.4–123.8) | <0.001 |
| Lipid‐lowering medications, No. (%) | 577 (13.6) | 213 (12.3) | 98 (11.0) | 156 (13.3) | 334 (17.7) | <0.001 |
| Prevalent CHF, No. (%) | 47 (1.1) | 24 (1.4) | 18 (2.0) | 21 (1.8) | 38 (2.0) | 0.04 |
| Diabetes mellitus, No. (%) | 623 (14.7) | 215 (12.4) | 138 (15.6) | 228 (19.4) | 306 (16.3) | <0.001 |
| Ischemic stroke, No. (%) | 217 (5.1) | 107 (6.2) | 54 (6.1) | 96 (8.2) | 140 (7.4) | <0.001 |
| CHD, No. (%) | 307 (7.3) | 110 (6.4) | 61 (6.9) | 79 (6.7) | 185 (9.8) | <0.001 |
| CHA2DS2‐VASc | 1.7 (1.2) | 1.8 (1.2) | 1.9 (1.2) | 2.0 (1.3) | 1.9 (1.3) | <0.001 |
ARIC indicates Atherosclerosis Risk in Communities; BMI, body mass index; CHD, coronary heart disease; CHF, congestive heart failure; DBP, diastolic blood pressure; HDL‐C, high‐density lipoprotein cholesterol; LVH, left ventricular hypertrophy; LDL‐C, low‐density lipoprotein cholesterol; LP(a), lipoprotein(a); pro–NT‐BNP, N‐terminal pro–B type natriuretic peptide; SBP, systolic blood pressure.
Data are expressed as mean (SD) or number (percentage) unless otherwise indicated.
P values were obtained with ANOVA for continuous variables and chi‐square test for categorical variables.
Median (interquartile range).
Incident AF
The median follow‐up was 13.9 years (interquartile range, 12.4–14.8 years). Among 9908 participants free of AF at baseline (visit 4), the incidence rate of AF was 8.8 events per 1000 person‐years overall, and was higher in whites compared with blacks (9.5 versus 6.1 events per 1000 person‐years) and men compared with women (10.8 versus 7.3 events per person‐years). There was no association between Lp(a) levels and incidence of AF (Table 2). The AF incidence rate was similar in participants with Lp(a) ≤10 mg/dL and those with >50 mg/dL (9.1 versus 8.4 events per 1000 person‐years). In the fully adjusted model (adjusted for demographics, prevalent CHD, other CVD risk factors, and lipids), the hazard ratio of AF for high Lp(a) levels ≥50 mg/dL compared with <10 mg/dL was 0.98 (95% confidence interval, 0.82–1.17). Figure 3 shows a restricted cubic spline of AF risk across increasing levels of Lp(a), using the 10th percentile of Lp(a) levels as a reference. There was no effect modification of the association between Lp(a) levels and AF risk by race (P interaction=0.39) or sex (P interaction=0.38).
Table 2.
Risk of AF for Different Lp(a) Levels: the ARIC Study 1996–2011
| IRa | Model 1b | Model 2c | Model 3d | |
|---|---|---|---|---|
| Lp(a) categoriese | ||||
| ≤10 mg/dL | 9.1 | Reference (1) | Reference (1) | Reference (1) |
| >10 to 20 mg/dL | 8.8 | 1.01 (0.86–1.20) | 1.04 (0.88–1.23) | 1.03 (0.87–1.22) |
| >20 to 30 mg/dL | 9.2 | 1.12 (0.90–1.40) | 1.13 (0.90–1.40) | 1.16 (0.93–1.45) |
| >30 to 50 mg/dL | 7.6 | 0.94 (0.76–1.16) | 0.93 (0.75–1.15) | 0.94 (0.76–1.16) |
| >50 mg/dL | 8.4 | 1.06 (0.90–1.26) | 1.02 (0.86–1.21) | 0.98 (0.82–1.17) |
| Log‐Lp(a)e | 1.01 (0.96–1.05) | 1.00 (0.96–1.05) | 0.99 (0.95–1.04) | |
Values are expressed as incidence rates (IRs) and hazard ratios (95% confidence intervals). AF indicates atrial fibrillation; ARIC, Atherosclerosis Risk in Communities; LP(a), lipoprotein(a).
IR per 1000 person‐years.
Model 1 includes: age, sex, and race‐center groups.
Model 2 includes: model 1+smoking, systolic blood pressure, diastolic blood pressure, treatment for hypertension, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, prevalent heart failure, coronary artery disease, and diabetes mellitus.
Model 3: model 2+low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, lipid‐lowering medication, and log‐transformed (Log) N–terminal pro‐B type natriuretic peptide.
3 Interactions of Lp(a) and AF by race and sex were P=0.11 and P=0.92 for Lp(a) categories and P=0.39 and P=0.38 for continuous Lp(a), respectively.
Figure 3.
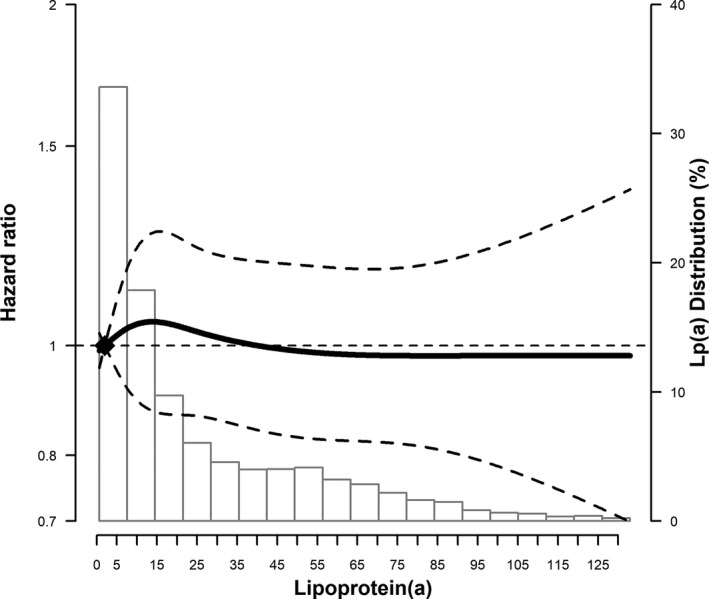
Atrial fibrillation (AF) risk across lipoprotein(a) (Lp[a]) levels. Multivariable‐adjusted restricted cubic spline model showing the hazard ratios of AF (95% confidence intervals) by Lp(a) levels at visit 4. The solid line represents hazard ratios and the dashed lines represent 95% confidence intervals. Knots at 5th, 35th, 65th, and 95th percentiles (corresponding to 1.3, 7.7, 23.9, and 83.1 mg/L). The spline is centered at the 10th percentile. The histogram shows the distribution of Lp(a) levels. Restricted cubic spline is truncated at the 1st and 99th percentiles of Lp(a). The model is adjusted for age, sex, race‐center groups, smoking, systolic and diastolic blood pressure, treatment for hypertension, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, prevalent heart failure, coronary artery disease, diabetes mellitus, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, lipid‐lowering medication, and log‐transformed N‐terminal pro–B type natriuretic peptide.
Incident Stroke
The median follow‐up was 15.8 years (interquartile range, 13.6–16.7 years). Among 10 127 participants free of stroke at baseline (visit 4), the incidence of stroke was higher by 4‐fold in participants with AF compared with those without (10.8 versus 2.9 events per 1000 person‐years). Among participants without a history of prevalent AF, those with Lp(a) >50 mg/dL had 42% higher risk of developing a stroke compared with those with ≤10 mg/dL (hazard ratio, 1.42; 95% confidence interval, 1.07–1.90), even after adjustment for numerous cardiovascular disease risk factors, other lipid markers, and CHA2DS2‐VASC score (Table 3). On the other hand, we failed to demonstrate a statistically significant relative increase in ischemic stroke risk among participants with a history of prevalent AF (hazard ratio, 1.06; 95% confidence interval, 0.70–1.61); however, there was no statistically significant interaction by AF status (P value for interaction=0.25). The relative hazard of stroke was not increased in participants with or without AF for intermediate Lp(a) levels of >10 to 20, >20 to 30, and >30 to 50 mg/dL compared with those with ≤10 mg/dL (Table 3). Figure 4 shows restricted cubic splines of the risk of stroke across increasing levels of Lp(a) in participants with and without AF, using the 10th percentile of Lp(a) levels as a reference. There was no effect modification of the association between Lp(a) levels and stroke risk by race or sex; the 3‐way multiplicative interactions of Lp(a) and AF by race and sex were P=0.85 and P=0.45, respectively, for continuous Lp(a).
Table 3.
Risk of Ischemic Stroke for Different Lp(a) Levels (mg/dL), Stratified by Prevalent AF Status: the ARIC Study 1996–2013
| No AF (n=8891) | AF (n=1236) | P Interaction by AF Statuse | |||||||
|---|---|---|---|---|---|---|---|---|---|
| IRa | Model 1b | Model 2c | Model 3d | IRa | Model 1b | Model 2c | Model 3d | ||
| Lp(a) categories | 0.25 | ||||||||
| ≤10 | 2.3 | Reference (1) | Reference (1) | Reference (1) | 10.6 | Reference (1) | Reference (1) | Reference (1) | |
| >10 to 20 | 2.9 | 1.14 (0.85–1.55) | 1.18 (0.87–1.60) | 1.21 (0.89–1.64) | 8.4 | 0.73 (0.46–1.17) | 0.71 (0.44–1.14) | 0.70 (0.44–1.13) | |
| >20 to 30 | 2.9 | 1.01 (0.67–1.50) | 1.03 (0.69–1.53) | 1.05 (0.70–1.58) | 7.4 | 0.49 (0.26–0.95) | 0.52 (0.27–1.01) | 0.52 (0.27–1.02) | |
| >30 to 50 | 3.6 | 1.19 (0.85–1.66) | 1.18 (0.84–1.65) | 1.19 (0.85–1.67) | 15.2 | 1.21 (0.74–2.00) | 1.23 (0.75–2.03) | 1.22 (0.74–2.02) | |
| >50 | 3.8 | 1.42 (1.07–1.88)f | 1.40 (1.06–1.86)f | 1.42 (1.07–1.90)f | 13.1 | 1.06 (0.71–1.59) | 1.04 (0.70–1.56) | 1.06 (0.70–1.61) | |
| Log‐Lp(a) | 1.08 (0.99–1.17) | 1.08 (0.99–1.17) | 1.08 (0.99–1.18) | 0.98 (0.87–1.11) | 0.98 (0.87–1.11) | 0.99 (0.87–1.12) | 0.26 | ||
Values are expressed as incidence rates (IRs) and hazard ratios (95% confidence intervals). AF indicates atrial fibrillation; ARIC, Atherosclerosis Risk in Communities; Log, log‐transformed; LP(a), lipoprotein(a).
IR per 1000 person‐years.
Model 1 includes: age, sex, and race‐center groups.
Model 2 includes: model 1+smoking, systolic and diastolic blood pressure, treatment for hypertension, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, prevalent heart failure, coronary artery disease, diabetes mellitus, and CHA2DS2‐VASc score.
Model 3 includes: model 2+low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, and lipid‐lowering medication.
The 3‐way multiplicative interactions of Lp(a) and atrial fibrillation by race and sex were P=0.85 and P=0.45 for continuous Lp(a), respectively.
p <0.05.
Figure 4.
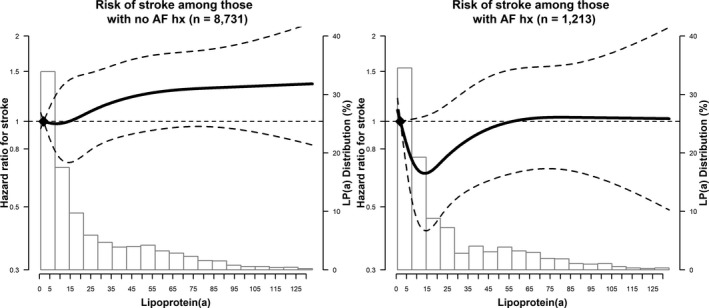
Ischemic stroke risk across lipoprotein(a) (Lp[a]) levels stratified by atrial fibrillation (AF) status. Multivariable‐adjusted restricted cubic spline models showing the hazard ratio of ischemic stroke (95% confidence intervals) by Lp(a) levels at visit 4. The solid line represents the hazard ratio and the dashed lines represent the 95% confidence intervals. Knots at 5th, 35th, 65th, and 95th percentiles (corresponding to 1.3, 7.7, 23.9, and 83.1 mg/L). The splines are centered at the 10th percentile. The histograms show the distribution of Lp(a) levels. Restricted cubic splines are truncated at the 1st and 99th percentiles of Lp(a). The models are adjusted for age, sex, race‐center groups, smoking, systolic and diastolic blood pressure, treatment for hypertension, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, prevalent heart failure, coronary artery disease, and diabetes mellitus. hx indicates history.
In a sensitivity analysis, examining the risk of incident cardioembolic stroke (n=129 of 541 ischemic stroke), there was no association between Lp(a) levels and cardioembolic stroke (Table 4).
Table 4.
Risk of Cardioembolic Stroke for Different Lp(a) Levels: the ARIC Study 1996–2013
| N case (IRa) | Model 1b | Model 2c | Model 3d | |
|---|---|---|---|---|
| Lp(a) categories | ||||
| ≤10 mg/dL | 55 (0.9) | Reference (1) | Reference (1) | Reference (1) |
| >10 to 20 mg/dL | 18 (0.7) | 0.77 (0.45–1.32) | 0.78 (0.45–1.33) | 0.79 (0.46–1.35) |
| >20 to 30 mg/dL | 11 (0.9) | 0.84 (0.43–1.63) | 0.83 (0.43–1.63) | 0.86 (0.44–1.68) |
| >30 to 50 mg/dL | 15 (0.9) | 0.85 (0.47–1.55) | 0.80 (0.44–1.46) | 0.82 (0.45–1.51) |
| >50 mg/dL | 30 (1.1) | 1.12 (0.70–1.78) | 1.09 (0.69–1.74) | 1.15 (0.71–1.86) |
| Log‐Lp(a) | 0.96 (0.83–1.11) | 0.96 (0.83–1.10) | 0.97 (0.84–1.12) | |
Values are expressed as incidence rates (IRs) and hazard ratios (95% confidence intervals). AF indicates atrial fibrillation; ARIC, Atherosclerosis Risk in Communities; Log, log‐transformed; LP(a), lipoprotein(a).
IR per 1000 person‐years.
Model 1 includes: age, sex, and race‐center groups.
Model 2 includes: model 1+smoking, systolic and diastolic blood pressure, treatment for hypertension, heart rate, height, body mass index, ECG left ventricular hypertrophy, PR interval, prevalent heart failure, coronary artery disease, diabetes mellitus, and CHA2DS2‐VASc score.
Model 3 includes: model 2+low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, triglycerides, and lipid‐lowering medication.
Discussion
In this large, community‐based cohort we found that there was no association between Lp(a) levels and AF risk. This null association was similar among whites and blacks and men and women. Participants in the highest Lp(a) category (>50 mg/dL) who were free of AF had a 42% higher risk of developing ischemic stroke compared with participants with Lp(a) ≤10 mg/dL. This relative risk increase conferred by high Lp(a) is ≈10‐fold lower compared with the risk for stroke conveyed by AF itself.34 Participants with Lp(a) levels between >10 and 50 were not at increased risk of stroke compared with those with Lp(a) ≤10 mg/dL. There was no association of Lp(a) with the cardioembolic subtype of ischemic stroke.
Our results complement the small body of literature examining associations between Lp(a) levels and risk of AF.12, 13 We confirmed that circulating levels of Lp(a) at baseline are not a risk factor for AF. Although Lp(a) levels are associated with atherosclerotic cardiovascular disease, which, in turn, is associated with incident AF,14, 15 in this cohort, Lp(a) was not associated with AF, even before adjusting for CHD. Our results are consistent with a recent large‐scale genetic study showing that although genetically lowered Lp(a) levels are associated with a lower risk of peripheral artery disease, stroke, HF, and aortic stenosis, they are not related to lower risk of AF.35 Collectively, this evidence suggests that although Lp(a) is a risk factor for diseases that have atherosclerosis as the underlying mechanism, it is not for AF.
This study expands the literature on the associations of Lp(a) and ischemic stroke. Lp(a) is a well‐established risk factor for stroke7, 8 and patients with Lp(a) ≥30 mg/dL have on average 80% higher relative risk of stroke, independently of race/ethnicity.36 There is only one small case‐control study that evaluated stroke risk in patients with AF, showing that patients with cardioembolic stroke had 2‐fold higher Lp(a) levels compared with those with noncardioembolic stroke (n=40).21 Here, we show that Lp(a) levels >50 mg/dL are associated with higher risk for ischemic stroke among individuals without AF. We failed to demonstrate a statistically significant relative increase in stroke risk for elevated Lp(a) levels in participants with AF, but there was no statistically significant interaction between Lp(a) and history of AF with the outcome of stroke.
We propose 2 mechanisms to explain these findings. First, the attributable risk of stroke from AF is considerably higher (an order of magnitude higher) compared with that attributed to Lp(a). AF increases the risk of stroke by 5‐fold,34 while in our study, Lp(a) levels >50 mg/dL increased the risk of stroke by 0.4‐fold compared with those with Lp(a) ≤10 mg/dL. As a result, the effect of Lp(a) on stroke risk may be overshadowed by the stroke risk conveyed by AF itself. Thus, Lp(a) levels may have little incremental contribution to stroke risk if AF is already present. Second, since Lp(a) promotes atherosclerosis, elevated Lp(a) levels might be primarily related to atheroembolic stroke, rather than cardioembolic stroke, but patients with AF experience primarily cardioembolic strokes. Indeed, in our sensitivity analysis, we found no association of Lp(a) with the subtype of cardioembolic strokes, although the numbers were smaller. Thus, Lp(a) might not increase the risk for cardioembolic stroke.
Study Strengths
Our study has several strengths. First, we utilized a large, biracial cohort with adequate AF and stroke events to test our hypotheses. The ARIC study's design enabled assessment for statistical interaction by race and sex. The ARIC study employed standardized protocols that facilitated accurate collection of outcomes and covariates. Second, Lp(a) levels were measured with a well‐validated assay that is robust to different apolipoprotein(a) isoform sizes. Third, AF was an adjudicated outcome in data collected from ARIC study visits, although AF events detected using ICD codes were not adjudicated. However, the use of ICD codes to ascertain AF in the ARIC study is a valid method, as ≈90% of AF cases were confirmed in a physician review of discharge summaries from 125 possible AF cases.19 Last, stroke events and their subtypes were adjudicated by trained study physicians including neurologists.
Study Limitations
Our study has several limitations. First, this was a community‐based sample unselected for lipid disorders, and extreme phenotypes of high Lp(a) levels (ie, >100 mg/dL) were rare and could not be examined. Thus, whether extremely high Lp(a) levels are associated with AF risk or stroke in patients with AF remains unknown. Second, we included only whites and blacks and thus these results may not generalize to other racial/ethnic groups. Third, we only had a single measure of Lp(a) at baseline. However, since Lp(a) levels are genetically determined,37 levels are generally stable in men and postmenopausal women over time. Although Lp(a) levels can be modifiable with lipid therapy, we did adjust for use of lipid‐lowering medications in our analyses. Fourth, we did not include data from the Centers for Medicare and Medicaid Services that were linked to ARIC study participants. However, more than half of ARIC participants were younger than 65 years (mean age, 63 years), which would not be captured by this Centers for Medicare and Medicaid Services data set, and it has previously been shown that adding Medicare data does not have a meaningful impact in most associations between AF and risk factors in the ARIC study cohort.38 Last, this is an observational study and we cannot exclude residual confounding, despite adjusting for potential covariates.
Conclusions
Elevated Lp(a) levels were not associated with incident AF in whites or blacks, but were associated with increased risk of ischemic stroke, primarily among individuals without AF. This relative risk increase is comparable between whites and blacks. Elevated Lp(a) is primarily associated with diseases directly related to atherosclerosis and is not a risk factor for AF. We did not find an association of Lp(a) with cardioembolic stroke, suggesting that the association of Lp(a) with ischemic stroke was primarily driven by thrombotic (atherosclerotic) stroke. It remains unknown whether extremely elevated Lp(a) levels could be associated with AF. Whether reduction of Lp(a) levels by lifestyle modifications or with medical therapy (currently being evaluated) results in reduction of stroke risk remains to be determined.
Sources of Funding
The ARIC study is performed as a collaborative trial supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). Drs Michos and Zhao are also supported by the Blumenthal Scholars Fund for Preventive Cardiology Research. Additional support was provided by American Heart Association grant 16EIA26410001 (Alonso).
Disclosures
Dr Ballantyne has received consultant fees/honoraria from Abbott Diagnostic, Amarin, Amgen, Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Esperion, Ionis, Matinas Bio Pharma Inc, Merck, Novartis, Pfizer, Regeneron, Roche Diagnostic, and Sanofi‐Synthelabo, and has received research grants from Abbott Diagnostic, Amarin, Amgen, Eli Lilly, Esperion, Ionis, Novartis, Pfizer, Regeneron, Roche Diagnostic, Sanofi‐Synthelabo. Dr Michos has received consultant fees/honoraria from Siemens Healthcare Diagnostics and a speaking fee from Bioquest Global. Dr Hoogeveen has received research grants from Denka Seiken, Ltd. Nazarian has received consultant fees/honoraria Biosense Webster Inc, CardioSolv, St Jude Medical; and research grants from Biosense Webster Inc. Dr Martin has received consultant fees/honoraria from Amgen Inc., Quest Diagnostics, Sanofi‐Regeneron and research grants from Aetna Foundation, Apple, Google. Dr. Aronis is supported by an NIH T32 training grant (5T32HL007227–42). The remaining authors have no disclosures to report.
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
(J Am Heart Assoc. 2017;6:e007372 DOI: 10.1161/JAHA.117.007372.)29246963
References
- 1. Fless GM, Rolih CA, Scanu AM. Heterogeneity of human plasma lipoprotein (a). Isolation and characterization of the lipoprotein subspecies and their apoproteins. J Biol Chem. 1984;259:11470–11478. [PubMed] [Google Scholar]
- 2. McLean JW, Tomlinson JE, Kuang WJ, Eaton DL, Chen EY, Fless GM, Scanu AM, Lawn RM. cDNA sequence of human apolipoprotein(a) is homologous to plasminogen. Nature. 1987;330:132–137. [DOI] [PubMed] [Google Scholar]
- 3. Caplice NM, Panetta C, Peterson TE, Kleppe LS, Mueske CS, Kostner GM, Broze GJ Jr, Simari RD. Lipoprotein (a) binds and inactivates tissue factor pathway inhibitor: a novel link between lipoproteins and thrombosis. Blood. 2001;98:2980–2987. [DOI] [PubMed] [Google Scholar]
- 4. Danesh J, Collins R, Peto R. Lipoprotein(a) and coronary heart disease. Meta‐analysis of prospective studies. Circulation. 2000;102:1082–1085. [DOI] [PubMed] [Google Scholar]
- 5. Emerging Risk Factors C , Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, Marcovina SM, Collins R, Thompson SG, Danesh J. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smolders B, Lemmens R, Thijs V. Lipoprotein (a) and stroke: a meta‐analysis of observational studies. Stroke. 2007;38:1959–1966. [DOI] [PubMed] [Google Scholar]
- 7. Nave AH, Lange KS, Leonards CO, Siegerink B, Doehner W, Landmesser U, Steinhagen‐Thiessen E, Endres M, Ebinger M. Lipoprotein (a) as a risk factor for ischemic stroke: a meta‐analysis. Atherosclerosis. 2015;242:496–503. [DOI] [PubMed] [Google Scholar]
- 8. Virani SS, Brautbar A, Davis BC, Nambi V, Hoogeveen RC, Sharrett AR, Coresh J, Mosley TH, Morrisett JD, Catellier DJ, Folsom AR, Boerwinkle E, Ballantyne CM. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2012;125:241–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Expert Panel on Detection E and Treatment of High Blood Cholesterol in A . Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 10. Kamstrup PR, Tybjaerg‐Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301:2331–2339. [DOI] [PubMed] [Google Scholar]
- 11. Kamstrup PR, Tybjaerg‐Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol. 2014;63:470–477. [DOI] [PubMed] [Google Scholar]
- 12. Diaz‐Peromingo JA, Alban‐Salgado A, Garcia‐Suarez F, Sanchez‐Leira J, Saborido‐Frojan J, Iglesias‐Gallego M. Lipoprotein(a) and lipid profile in patients with atrial fibrillation. Med Sci Monit. 2006;12:CR122–CR125. [PubMed] [Google Scholar]
- 13. Naji F, Sabovic M. Lipoprotein(a) and inflammation in patients with atrial fibrillation after electrical cardioversion. J Negat Results Biomed. 2011;10:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chamberlain AM, Agarwal SK, Folsom AR, Soliman EZ, Chambless LE, Crow R, Ambrose M, Alonso A. A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the Atherosclerosis Risk in Communities [ARIC] study). Am J Cardiol. 2011;107:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D'Agostino RB Sr, Newton‐Cheh C, Yamamoto JF, Magnani JW, Tadros TM, Kannel WB, Wang TJ, Ellinor PT, Wolf PA, Vasan RS, Benjamin EJ. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community‐based cohort study. Lancet. 2009;373:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen LY, Leening MJ, Norby FL, Roetker NS, Hofman A, Franco OH, Pan W, Polak JF, Witteman JC, Kronmal RA, Folsom AR, Nazarian S, Stricker BH, Heckbert SR, Alonso A. Carotid intima‐media thickness and arterial stiffness and the risk of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) Study, Multi‐Ethnic Study of Atherosclerosis (MESA), and the Rotterdam Study. J Am Heart Assoc. 2016;5:e002907 DOI: 10.1161/JAHA.115.002907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O'Neal WT, Efird JT, Dawood FZ, Yeboah J, Alonso A, Heckbert SR, Soliman EZ. Coronary artery calcium and risk of atrial fibrillation (from the Multi‐Ethnic Study of Atherosclerosis). Am J Cardiol. 2014;114:1707–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perez MV, Wang PJ, Larson JC, Soliman EZ, Limacher M, Rodriguez B, Klein L, Manson JE, Martin LW, Prineas R, Connelly S, Hlatky M, Wassertheil‐Smoller S, Stefanick ML. Risk factors for atrial fibrillation and their population burden in postmenopausal women: the Women's Health Initiative Observational Study. Heart. 2013;99:1173–1178. [DOI] [PubMed] [Google Scholar]
- 19. Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ, Folsom AR. Incidence of atrial fibrillation in whites and African‐Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158:111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–125. [DOI] [PubMed] [Google Scholar]
- 21. Okura H, Inoue H, Tomon M, Nishiyama S, Yoshikawa T. Increased plasma lipoprotein(a) level in cardioembolic stroke with non‐valvular atrial fibrillation. Intern Med. 1998;37:995. [DOI] [PubMed] [Google Scholar]
- 22. Igarashi Y, Yamaura M, Ito M, Inuzuka H, Ojima K, Aizawa Y. Elevated serum lipoprotein(a) is a risk factor for left atrial thrombus in patients with chronic atrial fibrillation: a transesophageal echocardiographic study. Am Heart J. 1998;136:965–971. [DOI] [PubMed] [Google Scholar]
- 23. Igarashi Y, Kasai H, Yamashita F, Sato T, Inuzuka H, Ojima K, Aizawa Y. Lipoprotein(a), left atrial appendage function and thromboembolic risk in patients with chronic nonvalvular atrial fibrillation. Jpn Circ J. 2000;64:93–98. [DOI] [PubMed] [Google Scholar]
- 24. ARIC Internal Data Distribution Agreement 2017. Available at: https://www2.cscc.unc.edu/aric/distribution-agreements. Accessed October 11, 2017.
- 25. The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. The ARIC Investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 26. Dati F, Tate JR, Marcovina SM, Steinmetz A; International Federation of Clinical C, Laboratory M and Standardization IWGfLA . First WHO/IFCC international reference reagent for lipoprotein(a) for immunoassay–Lp(a) SRM 2B. Clin Chem Lab Med. 2004;42:670–676. [DOI] [PubMed] [Google Scholar]
- 27. Soliman EZ, Prineas RJ, Case LD, Zhang ZM, Goff DC Jr. Ethnic distribution of ECG predictors of atrial fibrillation and its impact on understanding the ethnic distribution of ischemic stroke in the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2009;40:1204–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Misialek JR, Rose KM, Everson‐Rose SA, Soliman EZ, Clark CJ, Lopez FL, Alonso A. Socioeconomic status and the incidence of atrial fibrillation in whites and blacks: the Atherosclerosis Risk in Communities (ARIC) study. J Am Heart Assoc. 2014;3:e001159 DOI: 10.1161/JAHA.114.001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. The National Survey of Stroke. National Institute of Neurological and Communicative Disorders and Stroke. Stroke. 1981;12:I1–I91. [PubMed] [Google Scholar]
- 30. Autenrieth CS, Evenson KR, Yatsuya H, Shahar E, Baggett C, Rosamond WD. Association between physical activity and risk of stroke subtypes: the Atherosclerosis Risk in Communities study. Neuroepidemiology. 2013;40:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. [DOI] [PubMed] [Google Scholar]
- 32. Eriksson H, Caidahl K, Larsson B, Ohlson LO, Welin L, Wilhelmsen L, Svardsudd K. Cardiac and pulmonary causes of dyspnoea—validation of a scoring test for clinical‐epidemiological use: the Study of Men Born in 1913. Eur Heart J. 1987;8:1007–1014. [DOI] [PubMed] [Google Scholar]
- 33. Wattanakit K, Folsom AR, Selvin E, Weatherley BD, Pankow JS, Brancati FL, Hirsch AT. Risk factors for peripheral arterial disease incidence in persons with diabetes: the Atherosclerosis Risk in Communities (ARIC) study. Atherosclerosis. 2005;180:389–397. [DOI] [PubMed] [Google Scholar]
- 34. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Emdin CA, Khera AV, Natarajan P, Klarin D, Won HH, Peloso GM, Stitziel NO, Nomura A, Zekavat SM, Bick AG, Gupta N, Asselta R, Duga S, Merlini PA, Correa A, Kessler T, Wilson JG, Bown MJ, Hall AS, Braund PS, Samani NJ, Schunkert H, Marrugat J, Elosua R, McPherson R, Farrall M, Watkins H, Willer C, Abecasis GR, Felix JF, Vasan RS, Lander E, Rader DJ, Danesh J, Ardissino D, Gabriel S, Saleheen D, Kathiresan S; CHARGE–Heart Failure Consortium; CARDIoGRAM Exome Consortium . Phenotypic characterization of genetically lowered human lipoprotein(a) levels. J Am Coll Cardiol. 2016;68:2761–2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Boden‐Albala B, Kargman DE, Lin IF, Paik MC, Sacco RL, Berglund L. Increased stroke risk and lipoprotein(a) in a multiethnic community: the Northern Manhattan Stroke Study. Cerebrovasc Dis. 2010;30:237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tsimikas S. A test in context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol. 2017;69:692–711. [DOI] [PubMed] [Google Scholar]
- 38. Bengtson LG, Kucharska‐Newton A, Wruck LM, Loehr LR, Folsom AR, Chen LY, Rosamond WD, Duval S, Lutsey PL, Stearns SC, Sueta C, Yeh HC, Fox E, Alonso A. Comparable ascertainment of newly‐diagnosed atrial fibrillation using active cohort follow‐up versus surveillance of centers for Medicare and Medicaid services in the Atherosclerosis Risk in Communities study. PLoS One. 2014;9:e94321. [DOI] [PMC free article] [PubMed] [Google Scholar]


