Abstract
Background
Patients with schizophrenia show overconfidence in memory and social cognition errors. The present investigation examined whether this cognitive distortion also manifests in perceptual tasks.
Methods
A total of 55 individuals with schizophrenia, 58 with obsessive–compulsive disorder (OCD) as well as 45 non-clinical controls were presented 24 blurry black and white pictures, half of which contained a hidden object; the other half contained (“snowy”) visual noise. Participants had to judge whether the pictures depicted an object or not and how confident they were in this judgment.
Results
Participants with schizophrenia showed overconfidence in errors and an enhanced knowledge corruption index (i.e. rate of high-confident errors on all high-confident responses) relative to both control groups. In contrast, accuracy scores did not differ between clinical groups. Metacognitive parameters were correlated with self-rated levels of current paranoia.
Discussion
To the best of our knowledge, this is the first study to demonstrate overconfidence in errors among individuals with psychosis using a visual perception task. Speaking to the specificity of this abnormality for schizophrenia and its pathogenetic relevance, overconfidence in errors and knowledge corruption were elevated in patients with schizophrenia relative to both control groups and were correlated with paranoia.
Keywords: Paranoia, Schizophrenia, Confidence, Delusions, Knowledge corruption, Visual illusions
1. Introduction
Delusional ideas are commonly defined as false beliefs that are held with conviction and are not amenable to change. Although there is no symptom pathognomonic for schizophrenia (Carpenter et al., 1973), extreme paranoid beliefs such as feeling persecuted by the secret service or the feeling that electrodes have been implanted into one's head by a criminal organization are indicative of schizophrenia-spectrum disorders. Importantly, some delusion-prone ideas, such as feelings of being watched, are quite frequent in the general population (Ellett et al., 2003, Lincoln, 2007, Moritz and Van Quaquebeke, 2014, Peters et al., 1999, Verdoux and van Os, 2002). Freeman (2006) estimated that 1% to 3% of the nonclinical population have clinically relevant delusions; another 5% to 6% display milder delusions, and 10% to 15% have fairly regular subclinical delusional ideations (see also van Os et al., 2009, van Os et al., 2010).
Paranoid ideas usually do not come out of the blue as was presumed decades ago, but evolve over time (Fusar-Poli et al., 2013, Klosterkötter, 1992) and are often closely linked to biographical and situational factors. There is accumulating evidence that cognitive biases are involved in the development of psychotic symptoms. Biases are defined as distortions in the processing, selection and appraisal of information (Moritz et al., 2010b). Cognitive biases are not abnormal per se and do not necessarily lead to problems. To illustrate, biases like a self-serving attribution and unrealistic optimism are fairly normal and may even promote well-being (Pohl, 2004). However, specific cognitive biases, such as jumping to conclusions, may – in combination with other factors – become toxic and result in severe psychopathological problems (Moritz et al., 2010a). The focus of much research in schizophrenia has been the jumping to conclusions bias (i.e., patients gather less information for decision-making than controls; for a review see Fine et al., 2007, Garety et al., 1991, Moritz and Woodward, 2005), the bias against disconfirmatory evidence (i.e., counterevidence is not considered for reasoning; Moritz and Woodward, 2006b, Woodward et al., 2006, Woodward et al., 2007, Woodward et al., 2008), as well as overconfidence in errors. The latter bias constitutes the main focus of the present article.
Numerous studies have shown that patients with schizophrenia are poor at calibrating their level of confidence (Gaweda et al., 2012, Moritz and Woodward, 2002, Moritz et al., 2003, Moritz et al., 2008, Peters et al., 2007, Peters et al., 2013). Apart from questionnaires such as the Beck Cognitive Insight Scale (BCIS; e.g. "My interpretations of my experiences are definitely right."; Beck et al., 2004), which require a high level of introspection (some patients may not be aware of their biases; Freeman et al., 2006, Kother et al., 2012), response confidence is often captured by experimental cognitive tasks. When compared to healthy and psychiatric controls, response confidence is usually enhanced for erroneous judgments in schizophrenia patients. In contrast, some studies demonstrate that patients are less confident than controls when they are actually correct. We have coined the term reduced confidence gap for this response pattern (i.e., enhanced confidence in errors versus reduced confidence in correct responses). The majority of studies on overconfidence have been conducted with memory tasks (Gaweda et al., 2012, Moritz and Woodward, 2002, Moritz et al., 2003, Moritz et al., 2008, Peters et al., 2007, Peters et al., 2013). Recently, overconfidence in errors has been replicated with social cognition tasks, whereby facial recognition items were complemented by confidence judgments (Kother et al., 2012, Moritz et al., 2012b).
Factors that modulate overconfidence in errors and/or underconfidence in correct responses are only partially understood. Using difficult knowledge questions, we recently found underconfidence in correct responses, but no difference in overconfidence in errors between groups. We argue that awareness of one's deficits may enhance reluctance to make strong (high-confident) judgments. Moreover, the dopamine system is likely involved. Antipsychotic medication attenuates confidence (Andreou et al., 2014, Moritz et al., 2003), while dopamine in turn enhances certainty (Lou et al., 2011). Importantly, overconfidence in errors and other biases has been found to be present in neutral (i.e. delusion-irrelevant) scenarios, precluding tautological inferences.
A reduced confidence gap (e.g., Moritz et al., 2003) in combination with an enhanced error rate may culminate in a state termed inflated “knowledge corruption” (i.e., the proportion of high confidence errors on all high confident responses). In other words, a high proportion of what the individual believes to be true is actually wrong. If individuals cannot distinguish between correct and incorrect subjective facts, momentous mistakes may happen, which may foster paranoid ideation (for a review see Moritz and Woodward, 2006c). In line with this, a recent study found a linear relationship between the level of subjective conviction for a (simulated) paranoid scenario, and emotional, as well as behavioral consequences, for example, arming oneself and being prepared to hurt someone when feeling threatened (Moritz and Van Quaquebeke, 2014). In our view, errors are not necessarily momentous if a false assumption is further tested and is not regarded as a definite truth. However, caution is warranted as some studies have not found cross-sectional associations between high confidence errors and delusional ideation (e.g., Moritz and Woodward, 2006c).
So far, most studies on overconfidence have employed memory or social cognition tests. Replication is needed for perceptual tasks. A multitude of investigations suggests that perceptual functions are compromised in the disorder (Chen, 2011, Silverstein and Keane, 2011, Tan et al., 2013, van Assche and Giersch, 2011, Yoon et al., 2013), including early visual processes (Knebel et al., 2011). One of the best replicated visual deficits pertains to smooth pursuit movements as well as other eye tracking dysfunctions (Levy et al., 2010, O'Driscoll and Callahan, 2008), which recently has been linked with a failure to use efference copy information (Spering et al., 2013). As Javitt (2009) points out, impairments in basic perceptual processes may elicit higher order cognitive processing deficits. Hence, the study of visual, auditory and other perceptual aspects may help to reveal more about the origins of cognitive deficits in schizophrenia.
As of yet, it has not been studied whether errors in perceptual tasks are also accompanied by overconfident appraisals. In a recent investigation on a nonclinical population (Moritz et al., 2014), we assessed whether the liability to delusions would be associated with overconfidence in errors in a perceptual task (embedded figures task) that did not demand memory or social skills. Healthy individuals with high scores on core paranoid symptoms were overconfident in incorrect responses and demonstrated a significantly enhanced knowledge corruption index relative to subjects with lower scores (20% vs. 12%).
For the present study, we hypothesized that schizophrenia patients would display overconfidence in errors for perceptual judgments and would show an enhanced knowledge corruption relative to both healthy and psychiatric controls. We chose patients with obsessive–compulsive disorder as the psychiatric control group because of interesting similarities and differences to psychosis. While OCD has been sometimes dubbed “disorder of doubt”, as patients constantly worry about things they usually know are unfounded and absurd, paranoia can be dubbed “disorder of conviction” as confidence in delusional beliefs is high per definitionem. At the same time, the demarcation is sometimes blurry as many OCD patients perceive their obsessions as partly perceptual (Moritz et al. 2014a) and a subgroup of OCD patients shows poor illness insight, which has been added to the DSM-V, recently.
2. Methods
2.1. Participants
The present study was part of a larger trial investigating the effects of mindfulness training on subjective well-being in patients with schizophrenia spectrum disorders and obsessive–compulsive disorder (OCD) compared with healthy controls. Participants were allocated either to mindfulness training (self-help manual attached as pdf file) or a waitlist control group and were assessed before and six weeks after treatment. We report cross-sectional data from the post assessment, which included the visual perception task (not presented at baseline). The effect of the intervention will be presented elsewhere. In short, mindfulness did not have any impact on psychosis symptoms in any of the three groups. Therefore, the treatment trial did not confound results for the present project.
Different recruitment strategies were applied. A number of participants with schizophrenia and OCD were recruited using lists of previously discharged patients of the Departments of Psychiatry and Psychotherapy of the University Clinic Hamburg-Eppendorf (UKE) and the Central Institute of Mental Health Mannheim (CIMH). All participants had been previously treated in one of our institutions and had provided written informed consent to be recontacted for future studies. Other individuals had participated in previous online studies (some of these trials requested a diagnostic telephone interview with the MINI diagnostic instrument (Sheehan et al., 1998) to confirm the primary psychiatric diagnosis). Additional subjects were recruited with the help of the German association for OCD (DGZ) and several moderated German online discussion platforms providing people with OCD or psychosis with the opportunity to exchange information. A study was posted on these platforms (e.g., www.psychose.de) and a web-link provided access to the internet questionnaire. Participation was anonymous to foster unbiased responses (this made it impossible to discern the proportion of patients with previously verified diagnoses). Nonclinical participants were recruited from online panels and via word of mouth.
2.2. Security and inclusion criteria
The study was implemented with unipark®/questback®. Electronic informed consent was obtained online from participants in accordance with the department of data security in Hamburg and the local Ethics committee. “Cookies” prevented multiple accesses from the same computer. The following exclusion criteria were applied; 1. age below 18 or above 65 years, 2. failure to complete the questionnaires 3. no diagnosis of either schizophrenia or OCD (applies to the clinical groups only), 4. disclosure that the participant had not responded openly (final question), and 5. a diagnosis of bipolar disorder. We also excluded subjects with stereotypical responses (same value entered on the psychometric scales) and checked for deviant responses on the psychosis lie scale (Moritz et al., 2013a). For OCD, a diagnosis of OCD on the web-based screening questionnaire (WSQ; Donker et al., 2009) for common mental disorders was mandatory, whereas a prior episode of schizophrenia or bipolar disorder led to exclusion. For healthy controls, suspected psychiatric diagnoses (WSQ and self-reported diagnoses) or previous psychiatric treatment resulted in exclusion.
A total of 301 persons completed the visual perception task. A total of 158 (i.e., healthy, n = 45; schizophrenia, n = 55; OCD, n = 58) participants fulfilled the aforementioned criteria. The main reason for exclusion was poor diagnostic fit (n = 85; participants had psychiatric disorders other than schizophrenia or OCD). Moreover, 36 participants who considered themselves healthy either acknowledged a history of psychological and psychiatric treatment and/or had social phobia, depression and substance dependence according to the WSQ. Finally, in order to match the groups for age and levels of education, some participants (n = 22) were excluded blind to test results. All patients with schizophrenia confirmed that they received medication for their disorder. At the time of participation 73% of the schizophrenia participants and 59% of the OCD participants were in treatment, mainly in outpatient facilities (schizophrenia: 47%; OCD: 34%).
2.3. Community Assessment of Psychic Experiences Scale (CAPE)
The Community Assessment of Psychic Experiences Scale (CAPE; Stefanis et al., 2002) was administered in its authorized German translation. It consists of 42 items that are rated on a four-point Likert scale (“Never”, “Sometimes”, “Often” and “Nearly always”) and tap into the psychosis phenotype. The CAPE has three subscales measuring positive (“Do you ever feel as if things in magazines or on TV were written especially for you?”), negative (“Do you ever feel that you experience few or no emotions at important events?”) and depressive (“Do you ever feel pessimistic about everything?”) symptoms. Good reliability and (factorial) validity of the scale have been reported (Fonseca-Pedrero et al., 2012, Konings et al., 2006). We added four lie scale items (cut-off: 8 points) capturing common misconceptions about psychosis: a. seeing tiny objects like white mice (indicative of delirium rather than psychosis); b. alien abduction (a rare but highly publicized (face-valid) cliché symptom), c. being a famous historical personality (a rare but highly publicized (face-valid) cliché symptom), d. mental lapses during which one becomes another person (i.e., split personality; a rare/implausible but highly publicized cliché symptom).
Moreover, the 18-item frequency scale of the Paranoia Checklist (Freeman et al., 2005b) was administered. Previous studies have confirmed good psychometric properties for the scale (Freeman et al., 2005, Lincoln et al., 2010a, Lincoln et al., 2010b, Peters et al., 1999). According to factor analysis (Moritz et al., 2012a), the scale is best represented by two dimensions called suspiciousness (“Bad things are being said about me behind my back”) and core paranoia (“I can detect coded messages about me in the press/TV/radio”). The online version has been tested before and contains a high internal consistency and test–retest reliability (Moritz et al., 2014b).
Intermixed with items from the Paranoia Checklist, the 20-item Center for Epidemiologic Studies-Depression Scale (CES-D; Hautzinger and Brähler, 1993, Radloff, 1977) was applied along with 10 core items from the 18-item Obsessive Compulsive Inventory-R (OCI-R; Foa et al., 2002). The latter scale was used to make the rationale of the study (i.e., investigation of cognitive correlates of paranoid ideation) less transparent to participants in order to prevent response biases.
2.4. Visual pattern perception (Snowy Pictures Task)
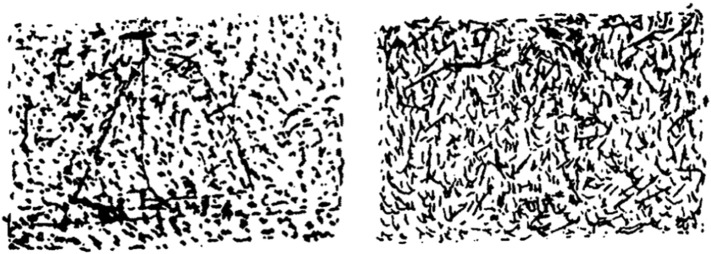
The Snowy Pictures Task was adopted from a study by Whitson and Galinsky (2008). Participants were presented 24 granulated black and white pictures (see Fig. 1). For half of the pictures, the original image had been removed digitally. All pictures were shown with comparable brightness and contrast. No time constraint was set. Pictures with or without objects were presented in pseudorandom order. For each item, participants had to endorse on a four-point Likert scale whether an object was present or not, graded for confidence (i.e., "yes–very sure"; “yes–unsure”; “no–unsure"; “no–very sure”). We used a 4-point scale as scales with broader ranges are prone to response tendencies (i.e., endorsing extreme values).
Fig. 1.
Examples: the left panel depicts a hidden sailboat; the object has been removed from the picture in the right panel.
3. Results
Groups did not differ in age or gender (Table 1). Although healthy subjects showed a tendency towards higher education, group differences were insignificant on this variable. Schizophrenia patients made less hits (i.e., correct identification of an object, irrespective of confidence) and less overall correct responses (i.e., hits and correct rejections) relative to healthy controls but not compared with psychiatric controls (see Table 2). No group differences emerged for false alarms (i.e., object mistakenly perceived as present). Regarding metacognitive parameters, a number of schizophrenia-specific impairments were seen. Compared with OCD patients and healthy controls, individuals with psychosis showed a greater amount of high-confident errors on all errors, a greater frequency of high-confident incorrect responses and accordingly a higher knowledge corruption index (% of all high-confident errors on all high-confident responses; see Table 2). Relative to healthy controls but not schizophrenia participants, OCD participants showed a lower number of high-confident correct responses as well as a lower percentage of high-confident correct responses on all correct responses.
Table 1.
Group differences on background and psychopathological characteristics.
| Healthy (n = 45) | Schizophrenia (n = 55) | OCD (n = 58) | Statistics (Bonferroni-corrected) | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Gender (% male) | 31% | 40% | 38% | χ2(1) = 0.90, p > .6 |
| Mean age (years) | 37.24 (13.93) | 38.22 (8.61) | 40.26 (10.66) | F(2,155) = 1.01, p > .3 |
| Formal school education (% 13th grade; qualification to enter university in Germany) | 86% | 69% | 67% | χ2(1) = 5.21, p = .07 |
| CAPE | ||||
| Positive | 1.23 (0.17) | 1.80 (0.39) | 1.40 (0.30) | F(2,155) = 33.76, p < .001; S > O > H |
| Negative | 1.63 (0.35) | 2.32 (0.54) | 2.22 (0.54) | F(2,155) = 20.25, p < .001; S, O > H |
| Depressed | 1.65 (0.36) | 2.31 (0.45) | 2.38 (0.43) | F(2,155) = 30.47, p < .001; O, S > H |
| OCI-R total (abbreviated) | 3.96 (4.55) | 6.29 (8.24) | 8.22 (6.72) | F(2,155) = 44.18, p < .001; O > S > H |
> = difference significant at p < .05.
Table 2.
Group differences on accuracy and metacognitive parameters.
| Healthy (n = 45) | Schizophrenia (n = 55) | OCD (n = 58) | Statistics (Bonferroni-corrected) | |
|---|---|---|---|---|
| Accuracy | ||||
| Hits | 8.82 (1.80) | 7.58 (2.35) | 8.47 (2.34) | F(2,155) = 4.31, p = .015; H > S |
| All correct (i.e., hits and correct rejections) | 19.16 (2.33) | 17.55 (2.51) | 18.31 (2.24) | F(2,155) = 5.76, p = .004; H > S |
| False alarms | 1.67 (2.60) | 2.04 (2.80) | 2.16 (2.46) | F(2,155) = 0.46, p > .6 |
| Metacognition (confidence) | ||||
| High confident incorrect | 1.02 (1.20) | 2.49 (2.61) | 1.50 (1.96) | F(2,155) = 6.85, p = .001; S > O, H |
| High confident correct | 13.07 (4.16) | 10.64 (5.06) | 9.69 (4.40) | F(2,155) = 7.13, p = .001; H > S, O |
| Percentage high confident correct/all correct | 68.05 (19.32) | 60.89 (28.03) | 53.39 (24.36) | F(2,155) = 4.59, p = .012; H > O |
| Percentage high confident incorrect/all incorrect | 21.31 (25.44) | 37.30 (33.11) | 23.27 (29.06) | F(2,155) = 4.60, p = .012; S > O, H |
| Knowledge corruption* | 6.53 (7.20) | 17.24 (15.59) | 10.35 (12.93) | F(2,155) = 9.31, p < .001; S > O, H |
> = difference significant at p < .05.
if no high-confident responses were made, the Knowledge Corruption Index (KCI) was set at 0%.
3.1. Correlation analyses
When looking at associations between metacognitive parameters and paranoia in the entire sample, the Paranoia Checklist was significantly correlated with knowledge corruption (r = .17, p = .028) and the number of high-confident errors (r = .18, p = .021), while it was inversely correlated with the number of high-confident correct responses (r = − .28, p < .001). The core paranoia subscale score of the Paranoia Checklist was significantly correlated with knowledge corruption (r = .24, p = .003) and the number of high-confident errors (r = .26, p = .001). Again, it was inversely correlated with the number of high-confident correct responses (r = − .20, p = .01). In the OCD group, none of these parameters was correlated with the OCI-R total score (abbreviated version). Again, the Paranoia Checklist was negatively correlated with the number of all high-confident correct responses (r = − .36, p = .005) and the number of high-confident incorrect responses (r = − .27, p = .038) in this group. In the schizophrenia sample, the Paranoia Checklist correlated with the knowledge corruption index at trend level (r = .23, p = .098) and significantly with the number of high-confident incorrect responses (r = .29, p = .029). The core paranoia subscale correlated with both the knowledge corruption index (r = .32, p = .018) and with the number high-confident incorrect responses (r = .34, p = .01).
3.2. Psychometric properties
Test–retest reliability was excellent for all scales (Paranoia checklist total score: r = .85; CES-D depression scale: r = .84, OCI-R (abbreviated): r = .88; all p < .001).
4. Discussion
Overconfidence in errors is a hallmark symptom of delusions. A growing number of findings suggest that this bias also manifests in non-delusional scenarios. The present study elucidated overconfidence in errors in a visual perception task in schizophrenia participants confirming our primary hypothesis: Overconfidence in errors and knowledge corruption in schizophrenia are not confined to memory (Gaweda et al., 2012, Moritz and Woodward, 2002, Moritz et al., 2003, Moritz et al., 2008, Peters et al., 2007) and social cognitive tasks (Kother et al., 2012, Moritz et al., 2012b), but extend to perception. Schizophrenia patients were overconfident about false perceptual judgments, while showing less certainty for correct judgments. These results corroborate earlier findings obtained in a nonclinical sample divided for paranoia scores using the same task (Moritz et al., 2014). Interestingly, between-group differences were found compared not only to healthy controls but also to OCD patients, supporting the hypothesis of specific dysfunctions of metacognition in schizophrenia. In contrast, while patients with schizophrenia performed worse than nonclinical controls in terms of accuracy, in line with other studies on the embedded figures tasks (Malaspina et al., 2004), scores did not differ between clinical groups (Moritz and Woodward, 2006a).
Metacognitive dysfunctions, particularly overconfidence in errors, have been linked to liberal acceptance (i.e., a lowered threshold for accepting hypotheses as true), which has also been implicated in jumping to conclusions (Moritz et al., 2007, Moritz et al., 2008). If hypotheses are prematurely accepted as true, the individual is less likely to look for further proof and may thus ignore or miss contradictory information. Confidence for these false responses is probably enhanced relative to participants who arrive at false conclusions based on a more thorough examination as more careful consideration will lead to a more ambiguous appraisal. Liberal acceptance (for an early account see Miller, 1976) may also explain underconfidence for correct judgments, which was also found within the schizophrenia sample in the present study (relative to healthy but not OCD controls): a premature termination of search processes limits chances of finding additional valid information, which could have further raised confidence.
This study has several limitations, including the mode of recruitment. Diagnoses of most participants relied on self-report, while only a subsample of subjects had verified diagnoses from previous hospitalizations. Also, some symptoms such as flat affect and disorganization of thought, which have been related to visual perception impairments before, are difficult to detect through self-report. However, good internal consistencies as well as plausible mean scores (mean scores in the CAPE are comparable to clinical patients with verified diagnoses; Moritz et al., 2013b) suggest high quality of the obtained data. Moreover, previous studies suggest that online studies are harder to sabotage than often presumed (Moritz et al., 2013b). Further, because of the rather large sample size, the findings are quite robust. Finally, we used a psychosis lie detection scale to prevent false-positive diagnoses of schizophrenia. Another limitation relates to the fact that the study only explored visual perception. Perceptual deficits have been identified for other sensory channels as well, including auditory (Nguyen et al., 2010) and olfactory perception (Nguyen et al., 2010) so that our approach needs to be tested for these modalities.
There are a number of questions that need to be addressed in further studies: First, we need to find out more about specific conditions that foster or attenuate overconfidence in errors such as task difficulty, "lure" strengths in studies using the false memory paradigms (Lee et al., 2007, Moritz et al., 2008), and the role of dopaminergic processes (Andreou et al., 2014). Second, it must be clarified how the response mode (sometimes confidence is measured with binary scales, sometimes with scales using a greater range of options) impacts results. Since overconfidence in errors is partly related to acute symptoms as a state marker, we assume that performance may vary over time, depending on the severity of illness. In order to address these questions, longitudinal designs, preferably with multiple, short-interval assessment points should be applied. This would allow to analyze whether fluctuations in confidence levels are a predictor of later-onset paranoid symptoms. Moreover, it could substantiate our finding that problems with calibrating confidence in distinguishing correct from incorrect responses represent a risk factor for the emergence of paranoia and subsequent emotional and behavioral problems (Moritz and Van Quaquebeke, 2014). Interventions that highlight the fallibility of human judgment per se and the consequences of highly confident but erroneous judgments, such as Metacognitive Training (Moritz et al., 2010b, Moritz et al., 2013c), Social Cognition and Interaction Training (Roberts and Penn, 2009) or the Maudsley Reasoning Program (Waller et al., 2011), may reduce paranoid ideas. These programs teach how an escalation of cognitive biases can create problems and even foster psychotic symptoms. Patients are encouraged to be more cautious in their decision-making processes and to search for further confirmatory or disconfirmatory evidence if information is equivocal (“better safe than sorry").
In conclusion, our study demonstrates that schizophrenia patients show a reduced confidence gap and enhanced knowledge corruption relative to both healthy and OCD controls.
Role of Funding Source
None
Contributors
All authors contributed substantially to this paper.
Conflict of Interest
None. The study did not deal with any substances, agents, patents or products that may create a conflict of interest.
Acknowledgements
None.
References
- Andreou C., Moritz S., Veith K., Veckenstedt R., Naber D. Dopaminergic modulation of probabilistic reasoning and overconfidence in errors: a double-blind study. Schizophr. Bull. 2014;40:558–565. doi: 10.1093/schbul/sbt064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T., Baruch E., Balter J.M., Steer R.A., Warman D.M. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr. Res. 2004;68:319–329. doi: 10.1016/S0920-9964(03)00189-0. [DOI] [PubMed] [Google Scholar]
- Carpenter W.T., Jr., Strauss J.S., Muleh S. Are there pathognomonic symptoms in schizophrenia? An empiric investigation of Schneider's first-rank symptoms. Arch. Gen. Psychiatry. 1973;28:847–852. doi: 10.1001/archpsyc.1973.01750360069010. [DOI] [PubMed] [Google Scholar]
- Chen Y. Abnormal visual motion processing in schizophrenia: a review of research progress. Schizophr. Bull. 2011;37:709–715. doi: 10.1093/schbul/sbr020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T., van Straten A., Marks I., Cuijpers P. A brief Web-based screening questionnaire for common mental disorders: development and validation. J. Med. Internet Res. 2009;11:e19. doi: 10.2196/jmir.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellett L., Lopes B., Chadwick P. Paranoia in a nonclinical population of college students. J. Nerv. Ment. Dis. 2003;191:425–430. doi: 10.1097/01.NMD.0000081646.33030.EF. [DOI] [PubMed] [Google Scholar]
- Fine C., Gardner M., Craigie J., Gold I. Hopping, skipping or jumping to conclusions? Clarifying the role of the JTC bias in delusions. Cogn. Neuropsychiatry. 2007;12:46–77. doi: 10.1080/13546800600750597. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Huppert J.D., Leiberg S., Langner R., Kichic R., Hajcak G. The Obsessive–Compulsive Inventory: development and validation of a short version. Psychol. Assess. 2002;14:485–496. [PubMed] [Google Scholar]
- Fonseca-Pedrero E., Paino M., Lemos-Giraldez S., Muniz J. Validation of the Community Assessment Psychic Experiences-42 (CAPE-42) in Spanish college students and patients with psychosis. Actas Esp. Psiquiatr. 2012;40:169–176. [PubMed] [Google Scholar]
- Freeman D. Delusions in the nonclinical population. Curr. Psychiatry Rep. 2006;8:191–204. doi: 10.1007/s11920-006-0023-1. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P.A., Bebbington P.E., Smith B., Rollinson R., Fowler D. Psychological investigation of the structure of paranoia in a non-clinical population. Br. J. Psychiatry. 2005;186:427–435. doi: 10.1192/bjp.186.5.427. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P., Kuipers E., Colbert S., Jolley S., Fowler D. Delusions and decision-making style: use of the Need for Closure Scale. Behav. Res. Ther. 2006;44:1147–1158. doi: 10.1016/j.brat.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Borgwardt S., Bechdolf A., Addington J., Riecher-Rossler A., Schultze-Lutter F. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–120. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garety P.A., Hemsley D.R., Wessely S. Reasoning in deluded schizophrenic and paranoid patients. Biases in performance on a probabilistic inference task. J. Nerv. Ment. Dis. 1991;179:194–201. doi: 10.1097/00005053-199104000-00003. [DOI] [PubMed] [Google Scholar]
- Gaweda L., Moritz S., Kokoszka A. Impaired discrimination between imagined and performed actions in schizophrenia. Psychiatry Res. 2012;195:1–8. doi: 10.1016/j.psychres.2011.07.035. [DOI] [PubMed] [Google Scholar]
- Hautzinger M., Brähler M. Hogrefe; Göttingen: 1993. Allgemeine Depressionsskala (ADS) [General Depression Scale] [Google Scholar]
- Javitt D.C. When doors of perception close: bottom-up models of disrupted cognition in schizophrenia. Annu. Rev. Clin. Psychol. 2009;5:249–275. doi: 10.1146/annurev.clinpsy.032408.153502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klosterkötter J. The meaning of basic symptoms for the genesis of the schizophrenic nuclear syndrome. Jpn. J. Psychiatry Neurol. 1992;46:609–630. doi: 10.1111/j.1440-1819.1992.tb00535.x. [DOI] [PubMed] [Google Scholar]
- Knebel J.F., Javitt D.C., Murray M.M. Impaired early visual response modulations to spatial information in chronic schizophrenia. Psychiatry Res. 2011;193:168–176. doi: 10.1016/j.pscychresns.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konings M., Bak M., Hanssen M., van Os J., Krabbendam L. Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr. Scand. 2006;114:55–61. doi: 10.1111/j.1600-0447.2005.00741.x. [DOI] [PubMed] [Google Scholar]
- Kother U., Veckenstedt R., Vitzthum F., Roesch-Ely D., Pfueller U., Scheu F. "Don't give me that look" — overconfidence in false mental state perception in schizophrenia. Psychiatry Res. 2012;196:1–8. doi: 10.1016/j.psychres.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Lee Y.S., Iao L.S., Lin C.W. False memory and schizophrenia: evidence for gist memory impairment. Psychol. Med. 2007;37:559–567. doi: 10.1017/S0033291706009044. [DOI] [PubMed] [Google Scholar]
- Levy D.L., Sereno A.B., Gooding D.C., O'Driscoll G.A. Eye tracking dysfunction in schizophrenia: characterization and pathophysiology. Curr. Top. Behav. Neurosci. 2010;4:311–347. doi: 10.1007/7854_2010_60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln T.M. Relevant dimensions of delusions: continuing the continuum versus category debate. Schizophr. Res. 2007;93:211–220. doi: 10.1016/j.schres.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Lincoln T.M., Peter N., Schafer M., Moritz S. From stress to paranoia: an experimental investigation of the moderating and mediating role of reasoning biases. Psychol. Med. 2010;40:169–171. doi: 10.1017/S003329170999095X. [DOI] [PubMed] [Google Scholar]
- Lincoln T.M., Ziegler M., Lüllmann E., Müller M.J., Rief W. Can delusions be self-assessed? Concordance between self- and observer rated delusions in schizophrenia. Psychiatry Res. 2010;178:249–254. doi: 10.1016/j.psychres.2009.04.019. [DOI] [PubMed] [Google Scholar]
- Lou H.C., Skewes J.C., Thomsen K.R., Overgaard M., Lau H.C., Mouridsen K. Dopaminergic stimulation enhances confidence and accuracy in seeing rapidly presented words. J. Vis. 2011;15 doi: 10.1167/11.2.15. [DOI] [PubMed] [Google Scholar]
- Malaspina D., Simon N., Goetz R.R., Corcoran C., Coleman E., Printz D. The reliability and clinical correlates of figure-ground perception in schizophrenia. J. Neuropsychiatry Clin. Neurosci. 2004;16:277–283. doi: 10.1176/jnp.16.3.277. [DOI] [PubMed] [Google Scholar]
- Miller R. Schizophrenic psychology, associative learning and the role of forebrain dopamine. Med. Hypotheses. 1976;2:203–211. doi: 10.1016/0306-9877(76)90040-2. [DOI] [PubMed] [Google Scholar]
- Moritz S., Van Quaquebeke N. Are you sure? Delusion conviction moderates the behavioural and emotional consequences of paranoid ideas. Cogn. Neuropsychiatry. 2014;19:164–180. doi: 10.1080/13546805.2013.819781. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. Memory confidence and false memories in schizophrenia. J. Nerv. Ment. Dis. 2002;190:641–643. doi: 10.1097/00005053-200209000-00012. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. Jumping to conclusions in delusional and non-delusional schizophrenic patients. Br. J. Clin. Psychol. 2005;44:193–207. doi: 10.1348/014466505X35678. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. The contribution of metamemory deficits to schizophrenia. J. Abnorm. Psychol. 2006;115:15–25. doi: 10.1037/0021-843X.15.1.15. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. A generalized bias against disconfirmatory evidence in schizophrenia. Psychiatry Res. 2006;142:157–165. doi: 10.1016/j.psychres.2005.08.016. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S. Metacognitive control over false memories: a key determinant of delusional thinking. Curr. Psychiatry Rep. 2006;8:184–190. doi: 10.1007/s11920-006-0022-2. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S., Ruff C.C. Source monitoring and memory confidence in schizophrenia. Psychol. Med. 2003;33:131–139. doi: 10.1017/s0033291702006852. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S., Lambert M. Under what circumstances do patients with schizophrenia jump to conclusions? A liberal acceptance account. Br. J. Clin. Psychol. 2007;46:127–137. doi: 10.1348/014466506X129862. [DOI] [PubMed] [Google Scholar]
- Moritz S., Woodward T.S., Jelinek L., Klinge R. Memory and metamemory in schizophrenia: a liberal acceptance account of psychosis. Psychol. Med. 2008;38:825–832. doi: 10.1017/S0033291707002553. [DOI] [PubMed] [Google Scholar]
- Moritz S., Veckenstedt R., Hottenrott B., Woodward T.S., Randjbar S., Lincoln T.M. Different sides of the same coin? Intercorrelations of cognitive biases in schizophrenia. Cogn. Neuropsychiatry. 2010;15:406–421. doi: 10.1080/13546800903399993. [DOI] [PubMed] [Google Scholar]
- Moritz S., Vitzthum F., Randjbar S., Veckenstedt R., Woodward T.S. Detecting and defusing cognitive traps: metacognitive intervention in schizophrenia. Curr. Opin. Psychiatry. 2010;23:561–569. doi: 10.1097/YCO.0b013e32833d16a8. [DOI] [PubMed] [Google Scholar]
- Moritz S., Van Quaquebeke N., Lincoln T.M. Jumping to conclusions is associated with paranoia but not general suspiciousness. A comparison of two versions of the probabilistic reasoning paradigm. Schizophr. Res. Treat. 2012;2012:1–9. doi: 10.1155/2012/384039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz S., Woznica A., Andreou C., Kother U. Response confidence for emotion perception in schizophrenia using a Continuous Facial Sequence Task. Psychiatry Res. 2012;200:202–207. doi: 10.1016/j.psychres.2012.07.007. [DOI] [PubMed] [Google Scholar]
- Moritz S., Favrod J., Andreou C., Morrison A.P., Bohn F., Veckenstedt R. Beyond the usual suspects: positive attitude towards positive symptoms is associated with medication noncompliance in psychosis. Schizophr. Bull. 2013;39:917–922. doi: 10.1093/schbul/sbs005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz S., Van Quaquebeke N., Lincoln T.M., Kother U., Andreou C. Can we trust the internet to measure psychotic symptoms? Schizophr. Res. Treat. 2013;2013:457010. doi: 10.1155/2013/457010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz S., Veckenstedt R., Bohn F., Hottenrott B., Scheu F., Randjbar S. Complementary group Metacognitive Training (MCT) reduces delusional ideation in schizophrenia. Schizophr. Res. 2013;151:61–69. doi: 10.1016/j.schres.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Moritz S., Göritz A.S., Van Quaquebeke N., Andreou C., Jungclaussen D., Peters M.J. Knowledge corruption for visual perception in individuals high on paranoia. Psychiatry Res. 2014;30:700–705. doi: 10.1016/j.psychres.2013.12.044. [DOI] [PubMed] [Google Scholar]
- Moritz S., Claussen M., Hauschildt M., Kellner M. Perceptual properties of obsessive thoughts are associated with low insight in obsessive–compulsive disorder. J. Nerv. Ment. Dis. 2014;202:562–565. doi: 10.1097/NMD.0000000000000156. [DOI] [PubMed] [Google Scholar]
- Moritz S., Voigt M., Köther U., Leighton L., Kjahili B., Babur Z., Jungclaussen D., Veckenstedt R., Grzella K. Can virtual reality reduce reality distortion? Impact of performance feedback on symptom change in schizophrenia patients. J. Behav. Ther. Exp. Psychiatry. 2014;45:267–271. doi: 10.1016/j.jbtep.2013.11.005. [DOI] [PubMed] [Google Scholar]
- Nguyen A.D., Shenton M.E., Levitt J.J. Olfactory dysfunction in schizophrenia: a review of neuroanatomy and psychophysiological measurements. Harv. Rev. Psychiatry. 2010;18:279–292. doi: 10.3109/10673229.2010.511060. [DOI] [PubMed] [Google Scholar]
- O'Driscoll G.A., Callahan B.L. Smooth pursuit in schizophrenia: a meta-analytic review of research since 1993. Brain Cogn. 2008;68:359–370. doi: 10.1016/j.bandc.2008.08.023. [DOI] [PubMed] [Google Scholar]
- Peters E., Day S., McKenna J., Orbach G. Delusional ideation in religious and psychotic populations. Br. J. Clin. Psychol. 1999;38(Pt 1):83–96. doi: 10.1348/014466599162683. [DOI] [PubMed] [Google Scholar]
- Peters M.J., Cima M.J., Smeets T., de Vos M., Jelicic M., Merckelbach H. Did I say that word or did you? Executive dysfunctions in schizophrenic patients affect memory efficiency, but not source attributions. Cogn. Neuropsychiatry. 2007;12:391–411. doi: 10.1080/13546800701470145. [DOI] [PubMed] [Google Scholar]
- Peters M.J., Hauschildt M., Moritz S., Jelinek L. Impact of emotionality on memory and meta-memory in schizophrenia using video sequences. J. Behav. Ther. Exp. Psychiatry. 2013;44:77–83. doi: 10.1016/j.jbtep.2012.07.003. [DOI] [PubMed] [Google Scholar]
- Pohl P.F. Psychology Press; Hove (UK): 2004. Cognitive illusions: a handbook on fallacies and biases in thinking, judgement and memory. [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Roberts D.L., Penn D.L. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res. 2009;166:141–147. doi: 10.1016/j.psychres.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry. 1998;59(Suppl. 20):22–33. [PubMed] [Google Scholar]
- Silverstein S.M., Keane B.P. Vision science and schizophrenia research: toward a re-view of the disorder. Editors' introduction to special section. Schizophr. Bull. 2011;37:681–689. doi: 10.1093/schbul/sbr053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spering M., Dias E.C., Sanchez J.L., Schutz A.C., Javitt D.C. Efference copy failure during smooth pursuit eye movements in schizophrenia. J. Neurosci. 2013;33:11779–11787. doi: 10.1523/JNEUROSCI.0578-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanis N.C., Hanssen M., Smirnis N.K., Avramopoulos D.A., Evdokimidis I.K., Stefanis C.N. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol. Med. 2002;32:347–358. doi: 10.1017/s0033291701005141. [DOI] [PubMed] [Google Scholar]
- Tan H.R., Lana L., Uhlhaas P.J. High-frequency neural oscillations and visual processing deficits in schizophrenia. Front. Psychol. 2013;4:621. doi: 10.3389/fpsyg.2013.00621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Assche M., Giersch A. Visual organization processes in schizophrenia. Schizophr. Bull. 2011;37:394–404. doi: 10.1093/schbul/sbp084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J., Linscott R.J., Myin-Germeys I., Delespaul P., Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med. 2009;39:179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- van Os J., Kenis G., Rutten B.P. The environment and schizophrenia. Nature. 2010;468:203–212. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- Verdoux H., van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr. Res. 2002;54:59–65. doi: 10.1016/s0920-9964(01)00352-8. [DOI] [PubMed] [Google Scholar]
- Waller H., Freeman D., Jolley S., Dunn G., Garety P. Targeting reasoning biases in delusions: a pilot study of the Maudsley Review Training Programme for individuals with persistent, high conviction delusions. J. Behav. Ther. Exp. Psychiatry. 2011;42:414–421. doi: 10.1016/j.jbtep.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitson J.A., Galinsky A.D. Lacking control increases illusory pattern Pperception. Science. 2008;322:115–117. doi: 10.1126/science.1159845. [DOI] [PubMed] [Google Scholar]
- Woodward T.S., Moritz S., Cuttler C., Whitman J.C. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions in schizophrenia. J. Clin. Exp. Neuropsychol. 2006;28:605–617. doi: 10.1080/13803390590949511. [DOI] [PubMed] [Google Scholar]
- Woodward T.S., Buchy L., Moritz S., Liotti M. A bias against disconfirmatory evidence is associated with delusion proneness in a nonclinical sample. Schizophr. Bull. 2007;33:1023–1028. doi: 10.1093/schbul/sbm013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward T.S., Moritz S., Menon M., Klinge R. Belief inflexibility in schizophrenia. Cogn. Neuropsychiatry. 2008;13:267–277. doi: 10.1080/13546800802099033. [DOI] [PubMed] [Google Scholar]
- Yoon J.H., Sheremata S.L., Rokem A., Silver M.A. Windows to the soul: vision science as a tool for studying biological mechanisms of information processing deficits in schizophrenia. Front. Psychol. 2013;4:681. doi: 10.3389/fpsyg.2013.00681. [DOI] [PMC free article] [PubMed] [Google Scholar]