Abstract
Objective
In this case-match study, we evaluated the impact of the CYP2C19*2 polymorphism in the occurrence of in-stent restenosis during a 1-year follow-up period despite adequate dual anti-platelet therapy in Iranian patients having undergone percutaneous coronary intervention (PCI).
Methods
This study, conducted at a tertiary referral heart center in Tehran, recruited 100 patients: 50 patients had in-stent restenosis after PCI during a 1-year follow-up and were compared to another 50 patients without in-stent restenosis who were individually matched according to sex. In order to evaluate the impact of the CYP2C19*2 polymorphism, case frequency matching was performed with respect to variables previously shown to be predictors of in-stent restenosis. The CYP2C19*2 polymorphism evaluated using real-time PCR methods.
Results
Among all 100 patients (mean age=60.09±10.29: 72.0% male), 89 (89%) patients had wild (CYP2C19*1/CYP2C19*1) and 11% had a heterozygous (CYP2C19*1/CYP2C19*2) genotypes, and there was no patient with a completely mutant genotype (CYP2C19*2/CYP2C19*2). Conditional logistic regression analysis showed that there was no significant association between genotype CYP2C19*1/CYP2C19*2 and the occurrence of in-stent restenosis after PCI (OR=2.5, p value=0.273).
Conclusion
Our findings indicated that carrying a CYP2C19*2 allele with a functional CYP2C19*1 allele had no significant association with instent restenosis 1 year after PCI. The antiplatelet treatment strategy for non-functional allele carriers is still a matter of controversy. Further studies with larger sample sizes are necessary to determine the prevalence of non-functional alleles in various populations and to achieve a consensus about the effective treatment strategy.
Keywords: genetic polymorphisms, coronary in-stent restenosis, clopidogrel resistance, percutaneous coronary intervention
Introduction
Ischemic heart disease is the leading cause of mortality all over the world, particularly in developing countries (1, 2). According to the last report of the World Health Organization and other regional studies, cardiovascular disease (CVD) is the most important cause of mortality and morbidity in Iran and accounts for nearly 40% of all mortalities (3). Coronary artery revascularization by coronary artery bypass graft surgery (CABG) and percutaneous coronary intervention (PCI) is the first-line treatment and reduces the rate of mortality and morbidity in patients with CAD. PCI is the most common form of myocardial revascularization (4).
Although the development and extensive use of coronary artery stents, particularly the drug-eluting stent (DES), have significantly decreased the rate of thrombosis and restenosis after PCI, in-stent restenosis is still a rare but serious complication of PCI. Many studies have been conducted on the prevention of stent thrombosis with antiplatelet therapy (5, 6). The American Society of Cardiology (ASC) guideline has recommended the administration of clopidogrel, in combination with aspirin, in patients using the bare-metal stent (BMS) for at least 1 month [and up to 12 months in recent studies (7)] and in patients using the DES for at least 12 months (8).
Appropriate function of cytochrome P450 2C19 (CYP2C19) is required to transform the clopidogrel as a pro-drug into its active metabolite, which has antiplatelet effects. Therefore, single-nucleotide polymorphisms of CYP2C19 (with different prevalence in different communities) can cause clopidogrel to have no or reduced antiplatelet effects in some patients having undergone PCI (9, 10). Several CYP2C19 gene polymorphisms have been proposed and investigated, and the results demonstrated that the presence of the CYP2C19*2 allele is particularly more associated with a decreased response to the antiplatelet effect of clopidogrel (11-13). The prevalence of this allele varies between different populations. Although the initial individualized treatment based on the CYP2C19 genotype is still controversial (11, 12), the study of CYP2C19 polymorphisms in each population can be indicative of the prognosis of the response to treatment and of the prevention of complications of stent restenosis in patients undergoing PCI.
In this individual case-match study, we determined the frequency of the CYP2C19*2 polymorphism in Iranian patients having undergone PCI and evaluated its role in the occurrence of in-stent restenosis during a 1-year follow-up period despite adequate dual anti-platelet therapy.
Methods
This study was conducted at Tehran Heart Center, a tertiary referral hospital in Tehran. Patients who underwent successful PCI were selected from the Tehran Heart Center Registry of Interventional Cardiology, which is described in detail elsewhere (14). Trained physicians and research nurses routinely obtain follow-up data 1, 6, and 12 months after PCI via clinic visits or telephone contact and is available in our registry. Patients were selected for the current analysis as follows: patients with unsuccessful PCI, a history of thrombosis, platelet dysfunction, malignancies, cerebrovascular accident during 3 months before the procedure, clopidogrel sensitivity, patients susceptible to bleeding, susceptible to aortic dissection, patients who took warfarin, glycoprotein IIb/IIIa or other antithrombotic drugs 14 days before PCI, patients with unstable hemodynamics, and patients with hemoglobin less than 10 gr/dL or hematocrit less than 34% were excluded. Among those who met the inclusion criteria, we selected patients who had a redo PCI and instent restenosis as the only event during a 1-year follow-up period and invited them for blood sampling and a genetic study. In total, 50 patients came for the blood sampling and were included in the study. These selected patients were then compared with another group of patients without in-stent restenosis, selected via case matching and invited for the genetic study. In order to evaluate the impact of the CYP2C19*2 polymorphism on the occurrence of in-stent restenosis, case matching was performed individually according to sex and frequency, matched with respect to all available variables previously shown to be predictors of DES and BMS restenosis (15). These variables included diabetes, prior myocardial infarction, chronic occlusions, bifurcation lesions, left anterior descending coronary artery (LAD) or saphenous vein graft (SVG) as the treated vessel, small vessel [defined as vessel diameter <2.75 mm, long lesions (length> 20 mm)], presence of severe calcification, and ostial and type C lesions according to the American College of Cardiology (ACC)/American Heart Association (AHA) categorization. Patients who refused to come were replaced with another matched case until we could complete the required 50 matched samples as controls.
All patients were treated with an aspirin (325 mg) and clopidogrel (600 mg) loading dose before the procedure. A bolus of heparin 5000 UI was administrated. The choice of the stenting technique and devices was left to the operator’s discretion. All patients received dual antiplatelet therapy: aspirin 80 mg/day indefinitely and clopidogrel 75 mg/day for at least 1 month after balloon angioplasty or bare-metal stent implantation and for 12 months after drug-eluting stent implantation, respectively.
Definition of in-stent restenosis
Restenosis is the reduction of lumen diameter after PCI due to arterial damage with subsequent neo-intimal tissue proliferation. Binary angiographic restenosis is defined as 50% luminal narrowing at the follow-up angiography (16). The Academic Research Consortium considered both an assessment of luminal narrowing and the patient’s clinical context and proposed a definition of clinical restenosis, assessed as a requirement for ischemia-driven repeat revascularization (17). The luminal narrowing and the in-stent restenosis were determined via follow-up angiography and evaluated by two experienced interventional cardiologists in at least two views without for shortening and overlapping. In the case of an intermediate lesion, the use of fractional flow reserve or intravascular ultrasound (IVUS) can guide the clinical decision (18). Drug resistance is known as one of the main causes of in-stent restenosis (19).
Genomic DNA extraction
Five milliliters of peripheral blood was collected from each patient in test tubes containing 0.5 M EDTA, and DNA was extracted using the DNPTM Kit (Cinnagen, Iran). Briefly, lysis solution was used to lyse blood cells, and then genomic DNA was selectively precipitated by isopropanol. The precipitated DNA was washed and desalted by ethanol and dissolved in double-distilled water. The quantity and quality of the extracted DNA were examined spectrophotometrically or visually by electrophoresis on a 1% agarose gel.
TaqMan SNP genotyping assay
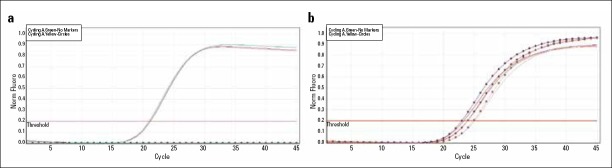
Primers and probes were purchased from Applied Biosystems Co. (C_25986767_70 for CYP2C19 *2), and genotyping of the extracted DNA for CYP2C19*2 was performed using the TaqMan SNP genotyping assay in two real-time PCR instruments, including a RotorGene 6000 (Corbett Life Science) and ABI 7500 sequence detection system (Applied Biosystems, USA) (Fig. 1). According to the manufacturer’s instructions, the genotyping for the samples was examined in final reaction volumes of 20 μL with 100 ng of DNA, 10 μL of Premix TaqMan (Takara, Shiga, Japan), and 1.25 μL of working stock of SNP Genotyping Assay. The PCR reaction was performed as follows: initial denaturation at 95°C for 10 min, followed by 45 cycles of denaturation at 95°C for 15 sec and annealing/extension at 60°C for 34 sec. All of the experiments were conducted in duplicate.
Figure 1.
a, b. Taqman analysis curves of two genotype patterns for the detection of cytochrome P 450 2 C19 *2 polymorphism. (a) Normal homozygous genotype pattern (CYP2C19*1/CYP2C19*1). (b) Heterozygous genotype pattern (CYP2C19*2/CYP2C19*1)
The real-time data were then analyzed by ABI TaqMan Genotyper and Linreg software. It was claimed by the ABI Company that the primer and probes were tested in 45 individuals from four ethnicities and that no more verification was needed. Nonetheless, 1% of the results were replicated by PCR-RFLP using polyacrylamide gel electrophoresis and BamH1 and Sma1 restriction enzymes for CYP2C19*2, and the accuracy of the methods was confirmed by sequencing the randomly selected samples for each genotype.
Statistical analysis
The continuous data were presented as mean and standard deviation (SD) and were compared between groups of patients with and without in-stent restenosis. Normality of the distribution of continuous variables was tested using Kolmogorov-Smirnov test, and student t-test or Mann-Whitney U test was used accordingly. The categorical variables were presented with frequency and percentage and were compared between groups with and without in-stent restenosis using the chi-squared or Fisher exact test. To evaluate the association between Cyp2c19 and in-stent restenosis, conditional logistic regression for matched pairs was used, and the association was reported through odds ratio (OR) with the 95% confidence interval (CI).
The statistical analyses were conducted using SPSS (SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc.) and R software (R Core Team. R: A Language and Environment for Statistical Computing. 3.0.0 ed: R Foundation for Statistical Computing, Vienna, Austria.; 2013).
Results
In total, 100 patients (mean age=60.09±10.29: 72.0% male) were included in the current study. Of this total, 50 patients had in-stent restenosis during the follow-up period (median follow-up=6.88 months) and were compared with a group of 50 patients without in-stent restenosis selected by case-matching. Comparisons of all baseline and procedural characteristics between these two groups of patients are shown in Tables 1 and 2. Among all 100 patients, 89 (89%) patients had wild (CYP2C19*1/ CYP2C19*1) and 11% had heterozygous (CYP2C19*1/CYP2C19*2) genotypes. There was no patient with a completely mutant genotype (CYP2C19*2/CYP2C19*2) among the patients included in the current study. The frequency of the heterozygous genotype was higher in patients with in-stent restenosis. However, this difference was not statistically significant (Table 1). Conditional logistic regression analysis was done to evaluate the association between the genotype CYP2C19*1/CYP2C19*2 and the occurrence of in-stent restenosis after PCI. The odds ratio was 2.5 (95% confidence interval =0.49-12.89). However, this association was not statistically significant (p value=0.273).
Table 1.
Baseline demographic and clinical characteristics according to in-stent restenosis
| Variable | Total n=100 |
Patients with ISR n=50 |
Patients without ISR n=50 |
P |
|---|---|---|---|---|
| Age, years | 60.09±10.29 | 59.62±10.31 | 60.56±10.34 | 0.650 |
| Male (%) | 72 (72.0) | 36 (72.0) | 36 (72.0) | 0.999 |
| Body mass index, kg/m2 | 27.46±5.13 | 27.86±4.80 | 27.09±5.44 | 0.477 |
| Positive family history (%) | 11 (11.1) | 5 (10.0) | 6 (12.2) | 0.722 |
| Diabetes mellitus (%) | 26 (26.0) | 14 (28.0) | 12 (24.0) | 0.648 |
| Hypertension (%) | 51 (51.5) | 24 (48.0) | 27 (55.1) | 0.480 |
| Hyperlipidemia (%) | 62 (62.6) | 30 (60.0) | 32 (65.3) | 0.585 |
| Current smoking (%) | 20 (20.0) | 8 (16.0) | 12 (24.5) | 0.309 |
| Previous MI (%) | 57 (57.0) | 28 (56.0) | 29 (58.0) | 0.840 |
| Previous PCI (%) | 7 (7.0) | 6 (12.0) | 1 (2.0) | 0.112 |
| LVEF (%) | 51.08±8.93 | 50.23±9.34 | 51.84±8.58 | 0.878 |
| Serum creatinine, mg/dL, (Median, 25%-75%) | 1.00 (0.8-1.2) | 0.95 (0.8-1.2) | 1.0 (0.9-1.2) | 0.753 |
| Genotype | 0.338 | |||
| Wild (CYP2C19*1/CYP2C19*1) | 89 (89.0) | 43 (86.0) | 46 (92.0) | |
| Heterozygote (CYP2C19*1/CYP2C19*2) | 11 (11.0) | 7 (14.0) | 4 (8.0) | |
| Mutant (CYP2C19*2/CYP2C19*2) | - | - | - | |
| Functional Class IV | 15 (28.8) | 7 (26.9) | 8 (30.8) | 0.760 |
| Follow-up duration (Median, 25%-75%) | 6.88 (3.85-8.94) | 6.75 (3.76-8.88) | 7.0 (3.88-9.00) | 0.611 |
Values are presented as mean±standard deviation (SD), n (%) or median and 25%-75% percentiles.
ISR - in-stent restenosis; LVEF - left ventricular ejection fraction; MI - myocardial infarction; PCI - percutaneous coronary intervention
Table 2.
Angiographic and procedural characteristics according to in-stent restenosis
| Variable | Total n=100 |
Patients with ISR n=50 |
Patients without ISR n=50 |
P |
|---|---|---|---|---|
| Diseased vessels | 0.591 | |||
| 1-VD (%) | 40 (40.0) | 19 (38.0) | 21 (42.0) | |
| 2-VD (%) | 39 (39.0) | 18 (36.0) | 21 (42.0) | |
| 3-VD (%) | 20 (20.0) | 12 (24.0) | 8 (16.0) | |
| Left main disease | 1 (1.0) | 1 (2.0) | 0 (0.0) | |
| Lesion | ||||
| Total lesion length per patient | 21.73±11.14 | 21.02±10.36 | 22.44±11.94 | 0.423 |
| At least one lesion with >20 mm length (%) | 50 (50.0) | 25 (50.0) | 25 (50.0) | 0.999 |
| RVD mean (%) | 3.17±0.50 | 3.13±0.47 | 3.22±0.54 | 0.370 |
| Small vessel (diameter <2.75 mm) | 33 (33.0) | 16 (32.0) | 17 (34.0) | 0.999 |
| Total occlusion | 4 (4.0) | 2 (4.0) | 2 (4.0) | 0.999 |
| Lesion type C | 64 (64.0) | 32 (64.0) | 32 (64.0) | 0.999 |
| Bifurcation | 15 (15.2) | 8 (16.3) | 7 (14.0) | 0.747 |
| Ostial lesion | 11 (11.0) | 6 (12.0) | 5 (10.0) | 0.749 |
| Proximal | 40 (40.0) | 22 (44.0) | 18 (36.0) | 0.414 |
| Calcification | 2 (2.0) | 1 (2.0) | 1 (2.0) | 0.999 |
| Tortuosity or angulation | 39 (39.4) | 19 (38.8) | 20 (40.0) | 0.901 |
| Type of PCI | 0.908 | |||
| Elective | 63 (63.0) | 32 (64.0) | 31 (62.0) | |
| Ad hoc | 28 (28.0) | 13 (26.0) | 15 (30.0) | |
| Primary | 9 (9.6) | 5 (10.0) | 4 (8.0) | |
| Number of treated lesions | 0.806 | |||
| Multi-lesion PCI | 21 (21.0) | 10 (20.0) | 11 (22.0) | |
| Single-lesion PCI | 79 (79.0) | 40 (80.0) | 39 (78.0) | |
| PCI of LAD | 58 (58.0) | 29 (58.0) | 29 (58.0) | 0.999 |
| PCI of SVG | 4 (4.0) | 2 (4.0) | 2 (4.0) | 0.999 |
| Stents | ||||
| Type of stent | 0.315 | |||
| BMS | 55 (55.0) | 30 (60.0) | 25 (50.0) | |
| DES | 45 (45.0) | 20 (40.0) | 25 (50.0) | |
| Multi-stents | 6 (6.1) | 3 (6.1) | 3 (6.1) | 0.999 |
Values are presented as mean±SD and n (%).
BMS - bare-metal stents; DES - drug-eluting stents; ISR - in-stent restenosis; LAD - left ascending descending artery; PCI - percutaneous coronary intervention; RVD - reference vessel diameter; SVG - saphenous vein graft; VD - vessel disease
Discussion
In this study, we compared two groups of 50 Iranian CAD patients who underwent successful PCI and received dual-antiplatelet therapy with and without in-stent restenosis during a 1-year follow-up period. We matched all cases in these two groups with respect to the patients’ gender. Frequency matching was also performed for all variables proven to be predictors of in-stent restenosis in order to evaluate the pure impact of the CYP2C19 polymorphism. The overall frequency of the heterozygous polymorphism was 11% in this population, and there was no patient with the mutant genotype. Our findings indicated that despite the high odds ratio (OR=2.5), carrying a CYP2C19*2 allele with a functional CYP2C19*1 allele (heterozygous genotype) had no significant association with in-stent restenosis 1 year after PCI.
Some recent studies have demonstrated that the prevalence of the CYP2C19*2 allele in the Iranian population with suspected coronary disease is approximately 13% (20), which is remarkably less than that in Asian populations (i.e., 47% of 2146 Korean patients who received a DES had at least one CYP2C19*2 allele) (21). On the other hand, the risk of in-stent restenosis in people with at least one non-functional allele has been reported to be 1.77-fold higher than that in people with a wild (functional) genotype (22). Another study reported that CYP2C19*2 carriers had a 30% greater risk of major cardiovascular events than non-carriers. In our study, it is unknown whether the non-significant association between the heterozygous genotype and the occurrence of in-stent restenosis was due to the low prevalence of the CYP2C19*2 allele among Iranians or due to the small sample size and, consequently, low statistical power.
It is recommended that treatment choice be based on the presence of a non-functional CYP2C19 polymorphism and the patient’s genotype. However, according to recent review studies, this approach is controversial (11, 12, 22). The supporters highlight the importance of other factors that could influence the response to clopidogrel, such as drug interactions. For instance, it is necessary for some patients to concurrently take clopidogrel-aspirin dual antiplatelet with proton pump inhibitors (PPIs), statins, and other medications that reduce CYP2C19 activity. Thus, drug interactions should be monitored more thoroughly in carriers of the CYP2C19*2 allele (23). On the other hand, a study by Cuisset et al. (24) demonstrated that increasing the dose of clopidogrel in patients undergoing PCI who had not responded appropriately to the drug was effective in those who had no CYP2C19*2 allele. Another study suggested that adding cilostazol to the clopidogrel-aspirin regimen can significantly reduce platelet activity in patients carrying the non-functional allele (25).
Study limitations
First and foremost, among the limitations of the present study is its small sample size, although we tried to overcome this shortcoming by matching the cases. We calculated our sample size based on the frequency of the CYP2C19*2 allele in the Iranian population. However, our achieved power was markedly reduced due to the low frequency of the non-functional allele in our study population. Moreover, while we focused on CYP2C19*2 as the most important allele responsible for the resistance to clopidogrel therapy, we did not study the prevalence of other non-functional CYP2C19 alleles. Further cohort studies with larger samples and on different races in the Iranian population are required to determine the effects of the CYP2C19 polymorphism on the prognosis of CAD patients who have undergone PCI and are receiving dual anti-platelet therapy.
We could not discuss bare/DES stent.
Conclusion
Our findings indicated that carrying a CYP2C19*2 allele with a functional CYP2C19*1 allele (heterozygous genotype) had no significant association with in-stent restenosis 1 year after PCI. Hence, the antiplatelet treatment strategy for non-functional allele carriers is still a matter of controversy. Further studies with larger sample sizes are necessary to determine an effective treatment strategy. In addition, the prevalence of non-functional alleles in various populations should be taken into consideration if a consensus is to be achieved.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - Y.N., S.V., M.B.; Design - S.V.; Supervision - Y.N.; Resource - H.P., E.N.; Material - M.B.; Data collection and/or processing - M.S., S.E.K., A.A., M.A., A.M.H.Z.; Analysis and/or Interpretation - S.S., Y.N., S.V.; Literature search - S.S., Y.N., S.V.; Writing - S.S., Y.N., S.V.; Critical review -Y.N., H.P., E.N., S.S., S.V., M.S., S.E.K., A.A., M.A., A.M.H.Z.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors 2001:systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 2.Bolognese L. Changing patterns of ST elevation myocardial infarction epidemiology. Am Heart J. 2010;160:S1–3. doi: 10.1016/j.ahj.2010.10.008. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO), “Iran (Islamic Republic of)”’. WHO’. Washington’, DC’: [accessed 03 Dec 2012]. available at: http://www.who.int/nmh/countries/irn_en.pdf . [Google Scholar]
- 4.Weintraub WS, Grau-Sepulveda MV, Weiss JM, DeLong ER, Peterson ED, O’Brien SM, et al. Prediction of long-term mortality after percutaneous coronary intervention in older adults results from the national cardiovascular data registry. Circulation. 2012;125:1501–10. doi: 10.1161/CIRCULATIONAHA.111.066969. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wenaweser P, Dörffler-Melly J, Imboden K, Windecker S, Togni M, Meier B, et al. Stent thrombosis is associated with an impaired response to antiplatelet therapy. J Am Coll Cardiol. 2005;45:174852. doi: 10.1016/j.jacc.2005.01.058. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Grines CL, Bonow RO, Casey DE, Gardner TJ, Lockhart PB, Moliterno DJ, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents:a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49:734–9. doi: 10.1016/j.jacc.2007.01.003. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 7.Cohen M. Antiplatelet therapy in percutaneous coronary intervention:a critical review of the 2007 AHA/ACC/SCAI guidelines and beyond. Catheter Cardiovasc Interv. 2009;74:579–97. doi: 10.1002/ccd.22021. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jacobs AK, Morrison DA, Williams DO, et al. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines:2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008;117:261–95. doi: 10.1161/CIRCULATIONAHA.107.188208. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 9.Ma TK, Lam YY, Tan VF?Yan BF. Variability in response to clopidogrel:how important are pharmacogenetics and drug interactions? Br J Clin Pharmacol. 2011;72:697–706. doi: 10.1111/j.1365-2125.2011.03949.x. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Price MJ, Murray SS, Angiolillo DJ, Lillie E, Smith EN, Tisch RL, et al. Influence of genetic polymorphisms on the effect of high-and standard-dose clopidogrel after percutaneous coronary intervention the GIFT (Genotype Information and Functional Testing) study. J Am Coll Cardiol. 2012;59:1928–37. doi: 10.1016/j.jacc.2011.11.068. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 11.Price MJ, Tantry US, Gurbel PA. The influence of CYP2C19 polymorphisms on the pharmacokinetics, pharmacodynamics, and clinical effectiveness of P2Y (12) inhibitors. Rev Cardiovasc Med. 2011;12:1–12. doi: 10.3909/ricm0590. [DOI] [PubMed] [Google Scholar]
- 12.Hulot JS, Collet JP, Silvain J, Pena A, Bellemain-Appaix A, Barthélémy O, et al. Cardiovascular risk in clopidogrel-treated patients according to cytochrome P450 2C19*2 loss-of-function allele or proton pump inhibitor coadministration:a systematic meta-analysis. J Am Coll Cardiol. 2010;56:134–43. doi: 10.1016/j.jacc.2009.12.071. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Giusti B, Gori AM, Marcucci R, Saracini C, Sestini I, Paniccia R, et al. Cytochrome P450 2C19 loss-of-function polymorphism, but not CYP3A4 IVS10+12G/A and P2Y12 T744C polymorphisms, is associated with response variability to dual antiplatelet treatment in high-risk vascular patients. Pharmacogenet Genomics. 2007;17:1057–64. doi: 10.1097/FPC.0b013e3282f1b2be. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Salarifar M, Mousavi MR, Saroukhani S, Nematipour E, Kassaian SE, Alidoosti M, et al. Percutaneous coronary intervention to treat chronic total occlusion:predictors of technical success and one-year clinical outcome. Tex Heart Inst J. 2014;41:40–7. doi: 10.14503/THIJ-12-2731. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim MS, Dean LS. In-stent restenosis. Cardiovasc Ther. 2011;29:190–8. doi: 10.1111/j.1755-5922.2010.00155.x. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 16.Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, et al. Angiographic patterns of in-stent restenosis:classification and implications for long-term outcome. Circulation. 1999;100:1872–8. doi: 10.1161/01.cir.100.18.1872. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 17.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials:a case for standardized definitions. Circulation. 2007;115:2344–51. doi: 10.1161/CIRCULATIONAHA.106.685313. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 18.Doi H, Maehara A, Mintz GS, Weissman NJ, Yu A, Wang H, et al. Impact of in-stent minimal lumen area at 9 months poststent implantation on 3-Year target lesion revascularization-free survival:a serial intravascular ultrasound analysis from the TAXUS IV, V, and VI trials. Circ Cardiovasc Interv. 2008;1:111–8. doi: 10.1161/CIRCINTERVENTIONS.108.784660. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 19.Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. 2010;56:1897–907. doi: 10.1016/j.jacc.2010.07.028. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 20.Saber MM, Boroumand M, Behmanesh M. Investigation of CYP2C19 allele and genotype frequencies in Iranian population using experimental and computational approach. Thromb Res. 2014;133:272–5. doi: 10.1016/j.thromres.2013.11.005. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 21.Oh IY, Park KW, Kang SH, Park JJ, Na SH, Kang HJ, et al. Association of cytochrome P450 2C19*2 polymorphism with clopidogrel response variability and cardiovascular events in Koreans treated with drug-eluting stents. Heart. 2012;98:139–44. doi: 10.1136/hrt.2011.227272. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 22.Bauer T, Bouman HJ, van Werkum JW, Ford NF, ten Berg JM, Taubert D. Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel:systematic review and meta-analysis. BMJ. 2011;343:d4588. doi: 10.1136/bmj.d4588. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bates ER, Lau WC, Angiolillo DJ. Clopidogrel-drug interactions. J Am Coll Cardiol. 2011;57:1251–63. doi: 10.1016/j.jacc.2010.11.024. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 24.Cuisset T, Quilici J, Cohen W, Fourcade L, Saut N, Pankert M, et al. Usefulness of high clopidogrel maintenance dose according to CYP2C19 genotypes in clopidogrel low responders undergoing coronary stenting for non ST elevation acute coronary syndrome. Am J Cardiol. 2011;108:760–5. doi: 10.1016/j.amjcard.2011.05.045. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 25.Park KW, Park JJ, Lee SP, Oh IY, Suh JW, Yang HM, et al. Cilostazol attenuates on-treatment platelet reactivity in patients with CYP2C19 loss of function alleles receiving dual antiplatelet therapy:a genetic substudy of the CILON-T randomised controlled trial. Heart. 2011;97:641–7. doi: 10.1136/hrt.2010.216499. [CrossRef] [DOI] [PubMed] [Google Scholar]