Abstract
Functional outcomes in individuals with schizophrenia suggest recovery of cognitive, everyday, and social functioning. Specifically improvement of work status is considered to be most important for their independent living and self-efficacy. The main purposes of the present study were 1) to identify which outcome factors predict occupational functioning, quantified as work hours, and 2) to provide cut-offs on the scales for those factors to attain better work status. Forty-five Japanese patients with schizophrenia and 111 healthy controls entered the study. Cognition, capacity for everyday activities, and social functioning were assessed by the Japanese versions of the MATRICS Cognitive Consensus Battery (MCCB), the UCSD Performance-based Skills Assessment-Brief (UPSA-B), and the Social Functioning Scale Individuals’ version modified for the MATRICS-PASS (Modified SFS for PASS), respectively. Potential factors for work outcome were estimated by multiple linear regression analyses (predicting work hours directly) and a multiple logistic regression analyses (predicting dichotomized work status based on work hours). ROC curve analyses were performed to determine cut-off points for differentiating between the better- and poor work status. The results showed that a cognitive component, comprising visual/verbal learning and emotional management, and a social functioning component, comprising independent living and vocational functioning, were potential factors for predicting work hours/status. Cut-off points obtained in ROC analyses indicated that 60–70% achievements on the measures of those factors were expected to maintain the better work status. Our findings suggest that improvement on specific aspects of cognitive and social functioning are important for work outcome in patients with schizophrenia.
Keywords: Functional outcomes, Cognition, Everyday-living skills, Social functioning, Work outcome
1. Introduction
Cognitive impairment is a core deficit of schizophrenia and known to be one of the deleterious factors for functional outcomes (Green, 1996, Green, 2006). Thus, the development of standard neuropsychological batteries for assessing cognitive functioning has been of a great concern. Accordingly, the MATRICS Consensus Cognitive Battery (MCCB; Nuechterlein and Green, 2006) was produced as an eligible comprehensive cognitive battery tailored for schizophrenia. With advent of this battery, the notion of functional outcomes has been well conceptualized with cognitive function as its continuation (Buchanan et al., 2011).
In order to validate cognitive enhancement assessed by “primary” measure i.e. the MCCB, the developers have sought “co-primary” measures to evaluate concurrent improvement on real-world functioning (Buchanan et al., 2011). The former refers to the assessment of basic cognitive abilities to attend, memorize or manipulate incoming information. The latter, on the other hand, is expected to be more sensitive to real-world functioning including every-day living skills or social functioning. Upon drug approval, the Food and Drug Administration emphasized the importance of improvement on co-primary measures as well as improvement in a cognitive performance endpoint. However, it is rather challenging to evaluate the efficacy of cognitive enhancement on real-world outcomes, as socio-economic factors (e.g. disability payment, local employment rates, or accessibility to social support) intervene between the expected improvement on functional outcomes and cognition-enhancing effects (Buchanan et al., 2011, Rosenheck et al., 2006). This situation has led to implementation of “functional capacity” (Green et al., 2011, Harvey and Velligan, 2011), an ability to perform everyday activities in limited contexts (e.g. role play), as an optimal co-primary measure (Green et al., 2008). With an introduction of functional capacity, which is more likely to be temporally linked to treatment-related changes in cognition, the elusive and hard to define notion of functional outcomes was more clearly modelled; it is a continuum, spanning from cognition to real-world outcomes mediated by functional capacity.
Probably, work is the most critical domain in real world outcomes. The lack of opportunity to work results in economic burden for patients themselves, families, and the government (i.e. medical or welfare costs) (Lee et al., 2008, Rice, 1999). In addition, participating in work itself may have therapeutic effects regardless of payment; working experiences have been shown to alleviate psychiatric symptoms (Bell et al., 1996), enhance self-esteem or efficacy (McGurk and Mueser, 2004), and give better insight for competence in work (Harvey et al., 2012a). Despite these merits of getting jobs, the prevalence of competitive employment in people with mental illness has remained considerably low in developed countries. The percentages of paid-employment are estimated at 10–20% in the US (Mueser et al., 1997), 8–35% in Europe (UK, German, and the France; Marwaha et al., 2007), and around 5% in Japan (Cabinet Office Japan, 2013).
Since the late 1980, work hours have been decreasing in Japan, partly due to several amendments of the Labour Standards Act. However, Japan is still one of the top countries with long work hours (Organization for Economic Co-operation and Development, 2013). This suggests that having a job is regarded as a prerequisite to be accepted into the Japanese society. The relatively greater importance of a homemaker also characterizes the Japanese labour system. Generally, a single person (typically a housewife) is responsible for household chores, caring for a family, and community activities. A survey (Statistics Bureau, Ministry of International Affairs and Communication, Japan, 2010) shows that 40.2% of females are full-time homemakers, despite a rapid increase of dual-earners in Japan.
Previous studies focused on multiple levels of functional outcomes to predict work outcome in patients with schizophrenia. Substantial evidence has been accumulated for the role of cognition as a predictor for employment status (Dickerson et al., 2008, McGurk et al., 2013, Nuechterlein et al., 2011). Also it has been shown that competence in work was associated with higher levels of competence in skills required for everyday activities (Bowie et al., 2006) or social competence (Bowie et al., 2010, Bowie et al., 2008). To date, however, few studies have attempted to examine which functional factor(s) (i.e. cognition, everyday-living skills, and social functioning) most dominantly predict work status in patients with schizophrenia.
Another issue is how work outcome is measured. Most previous studies used non-parametric measurement to evaluate work outcome. Some studies, for instance, assessed work status with a dichotomized variable of employed and unemployed (Dickerson et al., 2008, McGurk et al., 2013, Nuechterlein et al., 2011). Others assessed the capacity for work indirectly through informants’ observations (Bowie et al., 2010, Bowie et al., 2008, Bowie et al., 2006). Although a majority of studies have reported significant associations between their measures (e.g. cognition, functional capacity, or social adaptation) and work status/capacity, quantifiable measures, such as work hours in a certain period, would more precisely reflect the actual work outcome in patients with schizophrenia. For example, in the study by (McGurk et al., 2007), both hours worked and money earned were increased in cases whose cognition was improved by cognitive remediation therapy (CRT). However, there was no assessment of functional capacity in that study.
In addition, previous findings did not provide a practical implication for patients under recovery. It would be beneficial to examine the threshold in performance on testing scales to discriminate between patients functioning well in terms of work and those who are not.
The main purpose of the present study was to determine potential factors to predict work outcome, evaluated by quantitative measure (i.e. work hours in a certain period), in patients with schizophrenia. In particular, we focused on multiple levels of functioning (i.e. cognitive performance, observer-rated everyday functioning, and social functioning). Two types of regression analyses were conducted to detect relevant outcome factors. A multiple regression analysis was conducted to directly predict work hours in recent months, while a multiple logistic regression analysis was used to examine the variables to dichotomize subjects into the better vs. poor work status based on total work hours in recent months. The secondary purpose was to provide cut-offs for the measures discriminating work status. ROC curve analyses were performed to estimate optimal cut-off points and cut-off proportions for the factors identified as significant predictors for work outcome.
2. Methods
2.1. Participants
Forty-five Japanese patients meeting DSM-IV-TR criteria for schizophrenia and 111 healthy adults entered the study. Table 1 summarizes demographic and clinical profiles of the participants. Patients were treated in Okayama University Hospital in Okayama Prefecture, Toyama University Hospital and Joganji Hospital in Toyama Prefecture. Diagnosis was established based on DSM-IV-TR (American Psychiatric Association, 2000) criteria by experienced psychiatrists using a structured interview, reference to medical history, and all available information. Patients known to be abusing alcohol or illicit drugs, or those with epilepsy, brain damage, or neurologic disorders, were excluded from the study. Psychiatric symptoms were assessed on the Brief Psychiatric Rating Scale (BPRS), 18-item version (Overall and Gorham, 1962). They were all outpatients and the majority had work either outside (employed) or at home (homemaking) (currently at work=26, currently absent from work=9, no work in recent 3 months=10). The employed subjects engaged in relatively simple jobs such as delivery, stocktaking, or easy office work.
Table 1.
Characteristics of participants.
| HC | SCZ | t/F | df | p | |
|---|---|---|---|---|---|
| N (M/F) | 111 (78/33) | 45 (23/22) | |||
| Age | 30.9 (10.2)a | 36.98 (10.0) | − 3.40 | 154 | 0.001 |
| Education | 15.8 (1.6) | 14.0 (2.1) | 5.99 | 153 | < 0.000 |
| Duration | - | 9.5 (7.5) | - | - | - |
| Onset | - | 27.1 (8.4) | - | - | - |
| Drug (mg)b | - | 528.1 (526.9) | - | - | - |
| BPRS_Total | - | 34.0 (12.2) | - | - | - |
| BPRS_Positive | - | 9.0 (5.5) | - | - | - |
| BPRS_Negative | - | 7.1 (3.5) | - | - | - |
| MCCB Composite | 517.0 (62.7) | 375.5 (73.6) | 114.95 | 1, 154 | < 0.000 |
| UPSA-B | |||||
| Total | 83.4 (8.6) | 70.3 (13.9) | 7.11 | 154 | < 0.000 |
| Finance | 48.7 (3.1) | 44.4 (7.8) | 4.88 | 154 | < 0.000 |
| Communication | 34.7 (7.6) | 26.0 (9.6) | 6.02 | 154 | < 0.000 |
| SFS Total | 141.1 (16.4) | 102.3 (27.9) | 10.79 | 154 | < 0.000 |
| Healthy workersc | SCZ | t/F | df | p | |
| N (M/F) | 81 (69/12) | 45 (23/22) | |||
| Work hours per week | 57.5 (13.4) | 18.7 (20.2) | 12.92 | 124 | < 0.000 |
| Total work hours c | 690.1 (160.4) | 170.0 (227.2) | 14.97 | 124 | < 0.000 |
HC: Healthy controls, SCZ: patients with schizophrenia.
SD.
CPZ equivalent.
Total hours in recent 3 months.
Healthy adults were recruited at Okayama University and Fukushima University. The sample consisted of workers (N= 81) and university students (N= 30). The total sample (N= 111) was used for a group comparison and principal component analyses to show normative performance of young to middle- aged healthy adults. For subsequent regression analyses, only workers’ data was used as students’ study hours were deviated from work hours of workers.
Written informed consent was obtained from all participants. The study protocol was approved by ethics committees at the participating sites.
2.2. Measures
2.2.1. Cognitive assessment
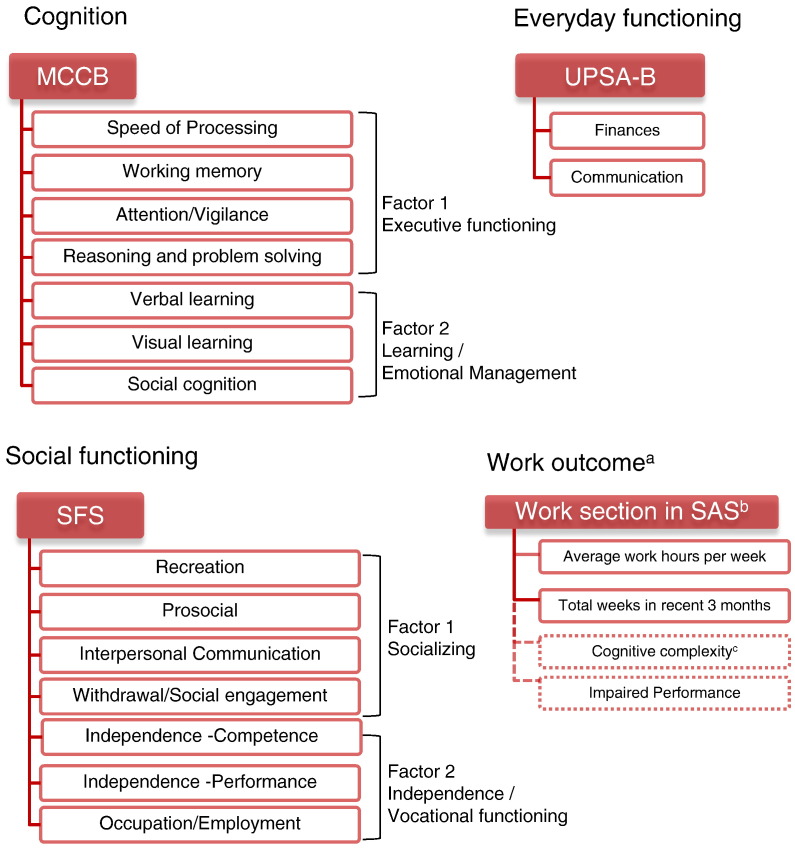
The MATRICS Cognitive Consensus Battery (MCCB) Japanese version (Kaneda et al., 2013, Sato et al., 2010) was administered to all participants. The MCCB is a comprehensive battery for assessing cognitive functioning in patients with schizophrenia (Nuechterlein and Green, 2006). It consists of neuropsychological subtests covering seven cognitive domains, as summarized in Fig. 1. The raw scores were transformed to the T-score, then the domain scores (Attention/Vigilance, Verbal learning, Visual learning, Reasoning and Problem solving, and Social cognition); the composite scores (Working memory, Speed of processing, and MCCB Total) were produced according to the manual (Kern et al., 2008, Nuechterlein and Green, 2006). The T-score of each task corresponds to the domain score except for Speed of Processing (Trail Making Test, BACS Symbol Coding, and Fluency) and Working memory (Letter Number Sequencing and Wechsler Memory Scale Spatial Span). For these domains, domain scores were calculated by summing the T-scores of tests included in the domains. The total composite score was the sum of the seven domain scores. The method for converting to T-score in the Japanese version was presented in our previous study (Sumiyoshi et al., 2014).
Fig. 1.
Schematic representation for the construct of functional outcome measures. a. Work outcome was evaluated by multiplying Average work hours per week by Total weeks in recent 3 months. b. Work section in the Modified SAS was used. c. Cognitive complexity and Impaired performance were not analyzed in the current study.
2.2.2. Performance-based assessment
The UCSD Performance-based Skills Assessment-Brief (UPSA-B; Mausbach et al., 2007) Japanese version (Sumiyoshi et al., 2011) was used to assess everyday functioning. This battery consisted of Finances and Communication subdomains (Fig. 1). The former includes basic financial skills such as counting change or extracting information from a bill payment. The latter evaluates communicative ability such as speaking on the phone or rescheduling an appointment. All the tasks are role-played. Each task score is summed by subscales and then transformed to standard scores (0-50). The total score is the sum of the subscale standard scores (0-100). The Japanese version was developed based on the international version of the UPSA-B, with some modifications to adjust for differences in everyday living skills in Japan (Sumiyoshi et al., 2011). The equivalency to its original version and the discriminative validity was confirmed in our previous study (Sumiyoshi et al., 2014).
2.2.3. Social functioning and work outcome
The Modified Social Functioning Scale/Social Adaptation Scale for MATRICS-PASS (Modified SFS/SAS for MATRICS-PASS) was used to evaluate overall social functioning and work outcome. Data were collected from the participants’ self-rating/reports. This scale was designed by the MATRICS-Psychometric and Standardization Study (MATRICS-PASS; Kern et al., 2008, Nuechterlein et al., 2008) for the validation study of the MCCB. It comprises the Social Functioning Scale Individuals’ version (SFS; Birchwood et al., 1990, Nemoto et al., 2008) (Fig. 1, bottom left), and the Work Outcome section from the modified Social Adaptation Scale (modified SAS; Subotnik et al., 2008) (Fig. 1, bottom right). The SFS part, consisting of 7 domains, assesses social competence by asking subjects’ status or activities. To enhance the accuracy of self-rating, most items were accompanied by anchor points (frequencies). For example, the degree of activities of ‘Visiting friends’ is well defined as ‘Never’=0 times [0 point]; Rarely = more than once in recent 3 months [1]; Sometimes = more than once in a month [2]; Often=more than once in a week [3]. A positive correlation between scores of this Japanese version of the SFS and MCCB has been reported in our preliminary study (Sumiyoshi and Sumiyoshi, 2015).
The Work Outcome section of the SAS is a self-report assessment of quantity of work, work role and activities, and impairment in work role activities. It consists of Work for Pay, Work at Home, and Student sections, and subjects are asked to fill in the most relevant section. We have implemented the Work at Home section, considering the importance of this work role in Japan. Each section includes average work hours per week, total number of weeks worked in the past 3 months, activities or responsibilities in the work role(s), and items related to work role impairment (Cognitive Complexity and Impaired Performance are assessed) (Fig. 1, bottom right). The work outcome measure was the total work hours in the past 3 months. This was obtained by multiplying the average work hours/week by total number of weeks worked in the past 3 months. For instance, if a participant worked 20 hours/week for 10 weeks in the past 3 months, the total work hours would be 200 hours. In addition, subjects were asked to briefly fill in major responsibilities in their work role(s) as well as its cognitive complexity and impaired performance. Cognitive complexity and Impaired performance were 4-point scales, ranging from 1=None to 5=Very High. Although these ratings were not analyzed in subsequent analyses, they were included to encourage patients to report work hours as accurately as possible. Based on this information, the validity of the self-reported work hours was verified by psychologists and/or by a direct interview when the report forms were submitted.
2.3. Statistical analyses
SPSS ver. 22.0 (IBM SPSS Statistics, 2013) was used for statistical analyses.
2.3.1. Group comparisons
Group differences of each measure were compared by t-test except for the MCCB. Performance on the MCCB was tested by ANCOVA controlling for Education.
2.3.2. Principal Component Analysis
A principal component analysis (PCA) was carried out for the MCCB and the SFS independently to reduce the number of variables for use in regression analyses. Data from healthy controls was used to obtain the normative components of those measures. Factors with eigenvalues ≥ 1 were extracted as independent components. Component scores were the sums of task scores highly loaded on the extracted factors and they were used in the subsequent regression analyses.
2.3.3. Multiple linear regression analysis
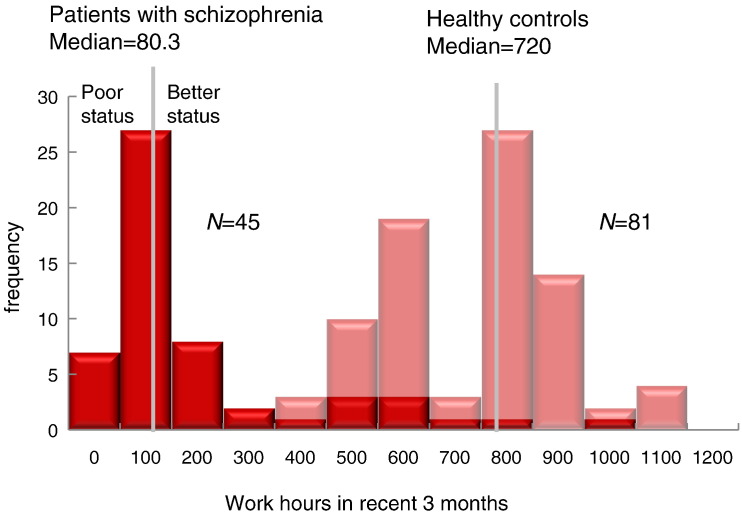
Multiple regression analyses with a backward selection method was conducted to estimate the best linear combination of predictors for work hours in healthy controls and patients with schizophrenia. The criterion of models was set p ≤ 0.10 for the F statistics. Component scores of the MCCB and the SFS, noted above, and the subscale scores of the UPSA-B (Finances, Communication) were independent variables. The total work hours in the recent 3 months were a dependent variable. A log-arithmetic transformation was performed on work hours and the UPSA-B measures due to the skewed distribution in the former (Fig. 2), and the ceiling effect found in the latter.
Fig. 2.
Total work hours in recent 3 months in healthy adults and patients with schizophrenia.
2.3.4. Multiple logistic regression analysis
Multiple logistic regression analyses with a backward exclusion method (likelihood ratio criteria) was conducted on the same data set used in the multiple linear regression analyses. The total work hours were dichotomized into either better or poor work status by means of a median sprit (i.e. longer vs. less than the median work hours of the patients group and the healthy comparison group; Fig. 2), and they were used as dependent variable.
2.3.5. ROC curve analysis
Receiver operating characteristic (ROC) curves analyses were conducted on significant predictors identified in regression analyses. Sensitivity was indexed by the area under curve (AUC) with the 95% confidential interval (95% CI) and d′ (d-prime(Gescheider, 1985). The larger values suggest higher sensitivity. Optimal cut-off points were determined at scores where the sum of sensitivity (% of hit) and specificity (% of correct rejection) were maximized (Mausbach et al., 2011, Youden, 1950). Besides, cut-off proportions were calculated to show what percentages were achieved on the cut-off points. For example, if a cut-off point is 150 at the measurement with maximum score of 200, the cut-off proportion would be 75% (=(150/200)×100). This proportion suggests that 75% or higher achievement is expected on that measurement to exceed the cut-off point, and thus, to be classified as “better” work status.
3. Results
3.1. Group comparisons
Table 1 presents the results from t-test and ANCOVA. Healthy controls were significantly younger and more educated than patients. Also, they performed better on the cognitive and functional outcome measures.
3.2. Principal component analysis
The results of PCA are presented in Table 2. Two factors were extracted both for the MCCB and the SFS. For the MCCB, subtests included in Working memory, Speed of processing, Reasoning/Problem solving, and Attention/Vigilance yielded higher loadings on Factor 1, while two learning subtests (HVLT-R and BVMT-R) and a social cognition task (MSCEIT Emotional management) loaded heavily on Factor 2. The former reflected executive function, while the latter was oriented to social cognition and learning. Thus, these components were interpreted as the Executive functioning component and the Learning/Emotional management component, respectively. Likewise, two factors of the SFS were assumed to represent prosocial activities (Factor 1: Recreation, Prosocial, Interpersonal Communication, and Withdrawal/Social engagement) and independence/work (Factor 2: Independence–Competence, Independence–Performance, and Occupation/Employment). Therefore, they were labelled as the Socializing component and the Independence/Vocational functioning component. These components are also depicted in Fig. 1.
Table 2.
Factor loadings on the MCCB and the SFS derived from principal component analyses for healthy controls (N=111).
| MCCB domains | F1 |
F2 |
SFS domains | F1 |
F2 |
|---|---|---|---|---|---|
| Executive functioning | Learning/Emotional management | Socializing | Independence/Vocational functioning | ||
| Speed of Processing | 0.78 | − 0.06 | Recreation | 0.75 | − 0.14 |
| Working memory | 0.70 | 0.21 | Prosocial | 0.66 | − 0.07 |
| Attention/vigilance | 0.64 | − 0.32 | Interpersonal Communication | 0.66 | − 0.06 |
| Reasoning and problem solving | 0.55 | − 0.56 | Withdrawal/Social Engagement | 0.64 | − 0.50 |
| Verbal learning | 0.37 | 0.64 | Independence -Competence | 0.32 | 0.80 |
| Visual Learning | 0.47 | 0.49 | Independence -Performance | 0.43 | 0.76 |
| Social cognition | − 0.15 | 0.39 | Occupation/Employment | − 0.21 | 0.32 |
| eigenvalue | 2.20 | 1.28 | eigenvalue | 2.17 | 1.59 |
| R2 | 49.68 | R2 | 53.69 | ||
3.3. Multiple regression analysis
The Learning/Emotional management (β= 0.34, t= 3.23, p= 0.002) and the Independence/Vocational functioning (β= 0.57, t= 4.83, p< 0.0001) remained significant in the patient group, accounting for around 40% (R2= 0.39) of total variance in work hours (Table 3, the upper part). The former variable reached significance even after the Occupation/Employment score in the SFS was removed from Independence/Vocational functioning component (results in parentheses in Table 3). For the control group, all variables excluded from the initial model, failing to reach the significance.
Table 3.
Results from regression analyses for patients with schizophrenia (N=45).
| Linear Regression | B | SE B | β | t | df | p |
|---|---|---|---|---|---|---|
| MCCB_Emotional management/Memory | 0.03 | 0.01 | 0.34 | 3.23 | 0.002 | |
| (0.03)a | (0.01) | (0.39) | (3.05) | (0.004) | ||
| SFS_Independence/Vocational functioning | 0.06 | 0.01 | 0.57 | 4.83 | < 0.0001 | |
| (0.06) | (0.02) | (0.51) | (4.02) | (< 0.0001) | ||
| F | 11.16 (11.18) | 2, 42 | < 0.0001 | |||
| (< 0.0001) | ||||||
| R2 | 0.39 (0.32) | |||||
| Logistic Regression | B | SE B | Wald | df | p | Odds ratio |
| MCCB_Emotional management/Memory | 0.03 | 0.01 | 4.44 | 1 | 0.035 | 1.03 |
| (0.03) | (0.01) | (4.34) | (0.037) | (1.03) | ||
| SFS_Independence/Vocational functioning | 0.05 | 0.02 | 4.82 | 1 | 0.028 | 1.05 |
| (0.04) | (0.02) | (3.52) | (0.061) | (1.04) | ||
| χ2 | 10.37 (8.38) | 2 | 0.006 | |||
| (0.015) | ||||||
| Predicting accuracy | 77.8 % (75.6 %) | |||||
Parentheses represent results when SFS_Occupation/Employment score are excluded from the SFS_Independence/Vocational functioning component. No variables remained significant for the healthy comparison group.
3.4. Multiple logistic regression analysis
The final model was presented in Table 3 (the bottom part). Similar to the linear regression analyses, the Learning/Emotional management (B= 0.03, p= 0.035) and the Independence/Vocational functioning (B= 0.04 p= 0.028) remained as significant predictors (χ2= 10.37, p= 0.006) in the optimal (i.e. most parsimonious) model, yielding 77.8% predicting accuracy. No variables contributed to predicting work status in the healthy comparison group. The most powerful variable was the Independence/Vocational functioning, but it failed to reach significance (B=−0.05, p= 0.13).
3.5. ROC curve analysis
Table 4 summarizes the results from ROC analyses for the two significant factors in the patients group found in the regression analyses. The AUC was 0.71 (95% CI: 0.55–0.87) for Learning/Emotional management, while it was 0.78 (95% CI: 0.64–0.93) for the Independence/Vocational functioning. Both were significantly greater than 0.5 (i.e. no discriminative power). d’s were estimated as 1.29 and 1.83, respectively. Both AUC and d' indices suggest that Learning/Emotional management and Independence/Vocational functioning have good sensitivity to differentiate between the better and poor work status.
Table 4.
Cut-off points and the proportions for differentiating between better- and poor work status in patients with schizophrenia (N=45).
| AUC | 95% CI |
d' | cut-off point | cut-off proportiona | ||
|---|---|---|---|---|---|---|
| lower | upper | |||||
| Learning/Emotional managementb | 0.71 | 0.55 | 0.87 | 1.29 | 153.4 | 76.7% |
| Independence/Vocational functioningc | 0.78 | 0.64 | 0.93 | 1.83 | 53.5 | 60.8% |
Note. AUC: Area under the curve, 95% CI: 95% confidence interval.
(cut-off point / maximum score) x 100.
maximum score=200.
maximum score=88.
The optimal cut-off points were estimated as 153.4 for the Learning/Emotional management and 53.5 for the Independence/Vocational functioning. Those scores correspond to 76.7% and 60.8% cut off proportions, respectively. Those proportions suggest that 76.7% or higher performance was expected on the Learning/Emotional management to reach the better work status, while it was 60.8% for the Independence/Vocational functioning.
4. Discussion
The current study investigated potential factors to predict work outcome in Japanese patients with schizophrenia. First, we clarified that certain domains of cognitive functioning and social functioning predicted work outcome, assessed with a quantifiable measure (i.e. work hours in recent 3 months). Specifically, the cognitive domain consisting of verbal/visual learning (HVLT-R and BVMT-R) and social cognition (MSCEIT Emotional management), and the social functioning domain including independence and vocational functioning, were found to predict hours/status, as revealed by both a linear regression analysis and a logistic regression analysis. Second, cut-off points for differentiating between the better- and poor work status were presented for those critical factors. Cut-off proportions of 60–70%, estimated from the cut-off points, may be an indicator in the classification of the better vs. poor work status.
The current findings are roughly consistent with previous studies reporting that cognitive improvement is a determinant for better employment/work status in patients with schizophrenia (Green et al., 2000, Nuechterlein et al., 2011). We further clarified that the ability to acquire new information and to control emotion are important to maintain a job. Our finding that domains of the SFS (Independence/Vocational functioning) was significantly associated with better work outcome supports a previous report that patients currently engaging in work attained a higher SFS score than unemployed patients (Harvey et al., 2012b).
Relatively stronger association between the SFS and work outcome may be due to the fact that the majority of patients in our study preserved ability to work, although the total amount of work hours varied to a certain degree (Fig. 2). Presumably, those subjects were better aware of their capacity for independent behavior (self-care) and vocational functioning. In fact, it has been reported that ever- or currently employed patients were able to more accurately estimate their ability to work compared to those who were not experiencing employment (Gould et al., 2013). Thus, it is assumed that patients with greater capacity for work more precisely estimate current social functioning.
We did not find significant contribution of everyday functioning, assessed with the UPSA-B, for predicting work hours/status. Mixed results have been presented about the significance of this level of functional outcome for work outcome. Studies using the full version of the UPSA (Patterson et al., 2001) reported a significant relationship between everyday functioning and work outcome (Bowie et al., 2008, Bowie et al., 2006), while two studies that used the UPSA-B (Bowie et al., 2010, Vesterager et al., 2012) did not. However, one recent large-scaled (N> 800) study (Strassnig et al., submitted for publication) did demonstrate a relationship between the UPSA-B and work outcomes assessed by the Specific Level of Functioning (SLOF; Schneider and Struening, 1983) scale, although they found that UPSA-B scores predicted the SLOF subscale of everyday activities more strongly than that of work outcome. In addition, (Mausbach et al., 2011) has shown that the UPSA-B has a good sensitivity to work outcome, presenting a cut-off point around 80 could satisfactory discriminate working (≥ 20 hours per week) vs. not-working (< 20 hours) patients with schizophrenia.
Given those supportive results for the association between the UPSA-B and work outcome, we examined a cut off-point of the UPSA-B Total score for differentiating between better- and poor work status although it was not a significant predictor. Interestingly, the cut-off point was 81.6, almost consisting with the above-noted study (Mausbach et al., 2011). In sum, mixed findings were obtained for an association between performance on the UPSA-B and work outcome and therefore, further studies should be aimed to clarify that the everyday functioning, assessed by the UPSA-B, is one of the key factors for work outcome in patients with schizophrenia.
The current study showed that self-ratings with the SFS could predict total working hours in recent months. Self-reports have sometimes been considered to be less reliable compared to performance-based assessment or informants’ observations, partly due to poor insights of patients (for a review, Bellack et al., 2007, Durand et al., 2015). It might be concerned that work hours in the current study was obtained by self-report, which could induce a biased association with the self-rated scores in the SFS (i.e. both measures might have been over-estimated). The possibility could be excluded by several reasons. First, it has been shown that patients and informants ratings on the SFS were highly correlated (Dickerson et al., 1997). Second, the SFS ratings have been reported to be correlated with those of the SLOF, which is an informant-based objective measure (Sumiyoshi et al., unpublished data).
Third, as shown in the regression analyses, a performance-based measure of the MCCB (Learning/Emotional management component) remained as a significant factor to predict work hours and status, providing an objective support for the accuracy of the self-report on work hours. To further examine this issue, we conducted a supplementary regression analysis assuming that at least one of the performance measures (either the MCCB or the UPSA-B) would certainly contribute to prediction of work hours in patients with schizophrenia. This time, predicting variables were the MCCB Overall composite score, the SFS Total score, and UPSA-B Total score were directly regressed on work hours in recent 3 months using a forced-enter method. As a result, the model was significant (F= 7.78, df= 3, 41, p < 0.01), accounting for 31.4 % of the total variance for work hours (R2= 0.31). The most dominant predictor was the SFS total score (β=0.52, t= 4.30, p < 0.01), followed by the MCCB Overall composite score (β=27, t= 1.98, p= 0.05). The UPSA-B Total score was at a trend level only (p= 0.07). Although the partial coefficient of the MCCB was near to marginal significance, the result confirmed the contribution of the performance-based measure to prediction of work hours, validating the self-evaluation in the current study.
Several limitations should be noted. First, the sample size of this study was relatively small. Latent predictors might have become significant in the regression analyses with a larger number of patients. Second, we did not include variables related to psychiatric symptoms, which have been shown to affect work outcome (Bowie et al., 2010, Bowie et al., 2008, Bowie et al., 2006, McGurk and Mueser, 2004). Future studies will be aimed to address these issues.
To conclude, our study showed that certain aspects of cognition and social functioning determine work outcome, quantified as work hours in recent months, in patients with schizophrenia. Expected performances to maintain better work status were also presented for those measures.
Role of Funding Source
This work was supported by Japan Society for the Promotion of Science (JSPS) Grant-in-Aid for Scientific Research (C) No. 22530691 to CS and No. 26461761 to TS7, as well as Health and Labour Sciences Research Grants for Comprehensive Research on Disability, Health, and Welfare (H24-Seishin-Ippan-002 and H26-Seishin-Ippan-011) and Intramural Research Grant for Neurological and Psychiatric Disorders of NCNP (21-1) and (27-1) to TS7.
Contributors
CS and PH designed the study. TS7 and IS supervised the study. CS, MT, YO, and TS7 collected data. KS and TS4 prepared materials. CS analyzed data, and wrote the draft. TS7, PH, and MT revised the draft critically for important intellectual content. All authors contributed to manuscript writing.
Conflict of interest
The authors report no potential conflicts of interest
Acknowledgements
The authors thank for Nao Imai, Mayumi Yabe, Shimako Nishiyama, Yuko Mizukami, and Miki Katou for organizing the data, and for Atsushi Igarashi for his advice on the early version of the manuscript.
References
- American Psychiatric Association . American Psychiatric Association; Washington, D.C.: 2000. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. [Google Scholar]
- Bell M.D., Lysaker P.H., Milstein R.M. Clinical benefits of paid work activity in schizophrenia. Schizophr. Bull. 1996;22(1):51–67. doi: 10.1093/schbul/22.1.51. [DOI] [PubMed] [Google Scholar]
- Bellack A.S., Green M.F., Cook J.A., Fenton W., Harvey P.D., Heaton R.K., Laughren T., Leon A.C., Mayo D.J., Patrick D.L., Patterson T.L., Rose A., Stover E., Wykes T. Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophr. Bull. 2007;33(3):805–822. doi: 10.1093/schbul/sbl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birchwood M., Smith J., Cochrane R., Wetton S., Copestake S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br. J. Psychiatry. 1990;157:853–859. doi: 10.1192/bjp.157.6.853. [DOI] [PubMed] [Google Scholar]
- Bowie C.R., Depp C., McGrath J.A., Wolyniec P., Mausbach B.T., Thornquist M.H., Luke J., Patterson T.L., Harvey P.D., Pulver A.E. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am. J. Psychiatry. 2010;167(9):1116–1124. doi: 10.1176/appi.ajp.2010.09101406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie C.R., Leung W.W., Reichenberg A., McClure M.M., Patterson T.L., Heaton R.K., Harvey P.D. Predicting schizophrenia patients' real-world behavior with specific neuropsychological and functional capacity measures. Biol. Psychiatry. 2008;63(5):505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie C.R., Reichenberg A., Patterson T.L., Heaton R.K., Harvey P.D. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am. J. Psychiatry. 2006;163(3):418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- Buchanan R.W., Keefe R.S., Umbricht D., Green M.F., Laughren T., Marder S.R. The FDA-NIMH-MATRICS guidelines for clinical trial design of cognitive-enhancing drugs: what Do We know 5 years later? Schizophr. Bull. 2011;37(6):1209–1217. doi: 10.1093/schbul/sbq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabinet Office Japan . Annual report on government measures for persons with disabilities. 2013. [Google Scholar]
- Dickerson F.B., Ringel N.B., Parente F. Ratings of social functioning in outpatients with schizophrenia; patients self-report versus caregiver assessment. Eval. Program Plann. 1997;20:415–420. [Google Scholar]
- Dickerson F.B., Stallings C., Origoni A., Boronow J.J., Sullens A., Yolken R. Predictors of occupational status six months after hospitalization in persons with a recent onset of psychosis. Psychiatry Res. 2008;160(3):278–284. doi: 10.1016/j.psychres.2007.07.030. [DOI] [PubMed] [Google Scholar]
- Durand D., Strassnig M., Sabbag S., Gould F., Twamley E.W., Patterson T.L., Harvey P.D. Factors influencing self-assessment of cognition and functioning in schizophrenia: Implications for treatment studies. Eur Neuropsychopharmacol. 2015;25(2):185–191. doi: 10.1016/j.euroneuro.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gescheider G.A. 2nd ed. Lawrence Erlbaum Associates; New Jersey: 1985. Psychophsics. [Google Scholar]
- Gould F., Sabbag S., Durand D., Patterson T.L., Harvey P.D. Self-assessment of functional ability in schizophrenia: milestone achievement and its relationship to accuracy of self-evaluation. Psychiatry Res. 2013;207(1-2):19–24. doi: 10.1016/j.psychres.2013.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M.F. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry. 1996;153(3):321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green M.F. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J. Clin. Psychiatry. 2006;67(Suppl. 9):3–8. (discussion 36–42) [PubMed] [Google Scholar]
- Green M.F., Kern R.S., Braff D.L., Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophr. Bull. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green M.F., Nuechterlein K.H., Kern R.S., Baade L.E., Fenton W.S., Gold J.M., Keefe R.S., Mesholam-Gately R., Seidman L.J., Stover E., Marder S.R. Functional co-primary measures for clinical trials in schizophrenia: results from the MATRICS Psychometric and Standardization Study. Am. J. Psychiatry. 2008;165(2):221–228. doi: 10.1176/appi.ajp.2007.07010089. [DOI] [PubMed] [Google Scholar]
- Green M.F., Schooler N.R., Kern R.S., Frese F.J., Granberry W., Harvey P.D., Karson C.N., Peters N., Stewart M., Seidman L.J., Sonnenberg J., Stone W.S., Walling D., Stover E., Marder S.R. Evaluation of functionally meaningful measures for clinical trials of cognition enhancement in schizophrenia. Am. J. Psychiatry. 2011;168(4):400–407. doi: 10.1176/appi.ajp.2010.10030414. [DOI] [PubMed] [Google Scholar]
- Harvey P.D., Heaton R.K., Carpenter W.T., Jr., Green M.F., Gold J.M., Schoenbaum M. Functional impairment in people with schizophrenia: focus on employability and eligibility for disability compensation. Schizophr. Res. 2012;140(1-3):1–8. doi: 10.1016/j.schres.2012.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey P.D., Sabbag S., Prestia D., Durand D., Twamley E.W., Patterson T.L. Functional milestones and clinician ratings of everyday functioning in people with schizophrenia: overlap between milestones and specificity of ratings. J. Psychiatr. Res. 2012;46(12):1546–1552. doi: 10.1016/j.jpsychires.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey P.D., Velligan D.I. International assessment of functional skills in people with schizophrenia. Innov. Clin. Neurosci. 2011;8(1):15–18. [PMC free article] [PubMed] [Google Scholar]
- Kaneda Y., Ohmori T., Okahisa Y., Sumiyoshi T., Pu S., Ueoka Y., Takaki M., Nakagome K., Sora I. Measurement and Treatment Research toImprove Cognition in Schizophrenia Consensus Cognitive Battery: validation of the Japanese version. Psychiatry Clin Neurosci. 2013;67:182–188. doi: 10.1111/pcn.12029. [DOI] [PubMed] [Google Scholar]
- Kern R.S., Nuechterlein K.H., Green M.F., Baade L.E., Fenton W.S., Gold J.M., Keefe R.S., Mesholam-Gately R., Mintz J., Seidman L.J., Stover E., Marder S.R. The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am. J. Psychiatry. 2008;165(2):214–220. doi: 10.1176/appi.ajp.2007.07010043. [DOI] [PubMed] [Google Scholar]
- Lee I.H., Chen P.S., Yang Y.K., Liao Y.C., Lee Y.D., Yeh T.L., Yeh L.L., Cheng S.H., Chu C.L. The functionality and economic costs of outpatients with schizophrenia in Taiwan. Psychiatry Res. 2008;158(3):306–315. doi: 10.1016/j.psychres.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Marwaha S., Johnson S., Bebbington P., Stafford M., Angermeyer M.C., Brugha T., Azorin J.M., Kilian R., Hansen K., Toumi M. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br. J. Psychiatry. 2007;191:30–37. doi: 10.1192/bjp.bp.105.020982. [DOI] [PubMed] [Google Scholar]
- Mausbach B.T., Depp C.A., Bowie C.R., Harvey P.D., McGrath J.A., Thronquist M.H., Luke J.R., Wolyniec P.S., Pulver A.E., Patterson T.L. Sensitivity and specificity of the UCSD Performance-based Skills Assessment (UPSA-B) for identifying functional milestones in schizophrenia. Schizophr. Res. 2011;132(2-3):165–170. doi: 10.1016/j.schres.2011.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach B.T., Harvey P.D., Goldman S.R., Jeste D.V., Patterson T.L. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr. Bull. 2007;33(6):1364–1372. doi: 10.1093/schbul/sbm014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T. Cognitive functioning, symptoms, and work in supported employment: a review and heuristic model. Schizophr. Res. 2004;70(2-3):147–173. doi: 10.1016/j.schres.2004.01.009. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T., Feldman K., Wolfe R., Pascaris A. Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. Am. J. Psychiatry. 2007;164(3):437–441. doi: 10.1176/ajp.2007.164.3.437. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T., Mischel R., Adams R., Harvey P.D., McClure M.M., Look A.E., Leung W.W., Siever L.J. Vocational functioning in schizotypal and paranoid personality disorders. Psychiatry Res. 2013;210(2):498–504. doi: 10.1016/j.psychres.2013.06.019. [DOI] [PubMed] [Google Scholar]
- Mueser K.T., Becker D.R., Torrey W.C., Xie H., Bond G.R., Drake R.E., Dain B.J. Work and nonvocational domains of functioning in persons with severe mental illness: a longitudinal analysis. J. Nerv. Ment. Dis. 1997;185(7):419–426. doi: 10.1097/00005053-199707000-00001. [DOI] [PubMed] [Google Scholar]
- Nemoto T., Fujii C., Miura Y., Chino B., Kobayashi H., Yamazawa R., Murakami M., Kashima H., Mizuno M. Reliability and validity of the Social Functioning Scale Japanese version (SFS-J) Jpn. Bull. Soc. Psychiatry. 2008;17:188–196. [Google Scholar]
- Nuechterlein K.H., Green M.F. MATRICS Assessment Inc.; Los Angeles: 2006. MATRICS consensus cognitive battery manual. [Google Scholar]
- Nuechterlein K.H., Green M.F., Kern R.S., Baade L.E., Barch D.M., Cohen J.D., Essock S., Fenton W.S., Frese F.J., III, Gold J.M., Goldberg T., Heaton R.K., Keefe R.S., Kraemer H., Mesholam-Gately R., Seidman L.J., Stover E., Weinberger D.R., Young A.S., Zalcman S., Marder S.R. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am. J. Psychiatry. 2008;165(2):203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Nuechterlein K.H., Subotnik K.L., Green M.F., Ventura J., Asarnow R.F., Gitlin M.J., Yee C.M., Gretchen-Doorly D., Mintz J. Neurocognitive predictors of work outcome in recent-onset schizophrenia. Schizophr. Bull. 2011;37(Suppl. 2):S33–S40. doi: 10.1093/schbul/sbr084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization for Economic Co-operation and Development . 2013. Average annual hours actually worked per worker. [Google Scholar]
- Overall J.E., Gorham D.R. The brief psychiatric rating scale. Psychol. Rep. 1962;10:799–812. [Google Scholar]
- Patterson T.L., Goldman S., McKibbin C.L., Hughs T., Jeste D.V. UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr. Bull. 2001;27(2):235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Rice D.P. The economic impact of schizophrenia. J. Clin. Psychiatry. 1999;60(Suppl 1):4–6. (discussion 28–30) [PubMed] [Google Scholar]
- Rosenheck R., Leslie D., Keefe R., McEvoy J., Swartz M., Perkins D., Stroup S., Hsiao J.K., Lieberman J. Barriers to employment for people with schizophrenia. Am. J. Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- Sato T., Kaneda Y., Sumiyoshi C., Sumiyoshi T., Sora I. Development of the MATRICS consensus cognitive battery: towards effective treatment of schizophrenia. Rinsho Seishin Yakurigaku. 2010;13(2):289–296. [Google Scholar]
- Schneider L.C., Struening E.L. SLOF: a behavioral rating scale for assessing the mentally ill. Soc. Work Res. Abstr. 1983;19(3):9–21. doi: 10.1093/swra/19.3.9. [DOI] [PubMed] [Google Scholar]
- Statistics Bureau, Ministry of International Affairs and Communication, Japan . 2010. Heisei 22 nendo kokusei chousa (The Consensus of 2010) [Google Scholar]
- Strassnig, M., Raykov, T., O'Gorman, C., Bowie, C., Sabbag, S., Durand, D., Patterson, T. L., Pinkham, A., Penn, D., Harvey, P. D., submitted for publication. Determinants of Different Aspects of Everyday Outcome in Schizophrenia: Differential Roles of Negative Symptoms, Cognition, and Functional Capacity. Schizophr. Bull. [DOI] [PMC free article] [PubMed]
- Subotnik K.L., Nuechterlein K.H., Kelly K.A., Kupic A.L., Brosemer B., Turner L.R. 2008. Modified Social Adjustment Scale-Work Outcome: Administration Social Adjustment Scale-Work Outcome Section (Modified): Available from ksubotnik@mednet.ucla.edu. Originally from Weissman & Bothwell (1976). Archives Gen Psychr, 33,1111–1115. Requests for the original measure, its derivation and psychometrics should be directed to Multi-Health Systems, Inc., P.O. Box 950, North Tonawanda, NY 14120-0950, phone 1-800-456-3003, or 1-416-492-2627, or e mailed to customerservice@mhs.com. Short and screener versions are also available. [Google Scholar]
- Sumiyoshi C., Sumiyoshi T. unctional outcome in patients with schizophrenia: The concept and the measurement. Act. Nerv. Super. 2015 . in press. [Google Scholar]
- Sumiyoshi C., Takaki M., Okahisa Y., Patterson T.L., Harvey P.D., Sumiyoshi T. Utility of the UCSD performance-based skills assessment-brief Japanese version: discriminative ability and relation to neurocognition. Schizophr. Res. Cogn. 2014;1:137–143. doi: 10.1016/j.scog.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumiyoshi T., Sumiyoshi C., Hemmi C. 2011. UCSD performance-based skills assessment-brief (UPSA-B) Japanese version: administration and scoring manual. [Google Scholar]
- Vesterager L., Christensen T.O., Olsen B.B., Krarup G., Melau M., Forchhammer H.B., Nordentoft M. Cognitive and clinical predictors of functional capacity in patients with first episode schizophrenia. Schizophr. Res. 2012;141(2-3):251–256. doi: 10.1016/j.schres.2012.08.023. [DOI] [PubMed] [Google Scholar]
- Youden W.J. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]