Abstract
Objective:
Vulvovaginal atrophy (VVA) is characterized by vaginal changes, dyspareunia, and itching/irritation. Efficacy and safety of a lower-dose estradiol vaginal cream (0.003%) were evaluated in postmenopausal women with VVA-related dyspareunia.
Methods:
This was a phase 3, randomized, double-blind, placebo-controlled study. Sexually active postmenopausal women with moderate–severe dyspareunia as the most bothersome symptom, ≤5% vaginal superficial cells, and vaginal pH >5.0 were randomized (1:1) to 0.003% estradiol vaginal cream (15 μg estradiol; 0.5 g cream) or placebo (0.5 g cream) applied daily for 2 weeks followed by three applications/week for 10 weeks. Coprimary outcomes were changes in dyspareunia severity, vaginal cytology, and vaginal pH from baseline to final assessment. Additional efficacy outcomes and safety were assessed.
Results:
A total of 550 participants (average age, 58 y) were randomized. Compared with placebo, estradiol reduced dyspareunia severity (mean change from baseline ± SD: −1.5 ± 1.0 estradiol vs −1.2 ± 0.9 placebo), decreased vaginal pH (−1.36 ± 0.89 vs −0.53 ± 0.92), and improved vaginal cytology (percentage superficial and parabasal cells 10.1 ± 16.7 vs 1.4 ± 6.1 and −48.5 ± 45.1 vs −14.6 ± 39.6; P < 0.001, all) at the final assessment. In addition, estradiol decreased dyspareunia severity at weeks 8 and 12, vaginal/vulvar irritation/itching at weeks 4 and 12, and dryness at week 12 versus placebo (P < 0.01, all). VVA severity, pH, and cytology improved at week 12 with estradiol versus placebo (P < 0.001, all). Vulvovaginal mycotic infections were more frequent with estradiol. One serious event leading to discontinuation occurred with estradiol. No deaths occurred.
Conclusions:
Lower-dose estradiol vaginal cream (0.003%) dosed three applications/week is an effective and well-tolerated treatment for VVA-related dyspareunia.
Keywords: Dyspareunia, Genitourinary syndrome of menopause, Vaginal estrogen, Vulvovaginal atrophy
The reduced estrogen levels that occur after menopause are associated with vulvovaginal atrophy (VVA), a chronic condition that leads to increased vaginal pH, thinning of the vaginal and lower genitourinary epithelial lining, and loss of vaginal elasticity.1-3 Symptoms include dyspareunia, dysuria, and vaginal or vulvar dryness, itching, irritation, and burning,1,2,4 any of which can negatively impact sexual health and quality of life.5 In the large US REVIVE survey of postmenopausal women, the most commonly reported VVA symptoms were vaginal dryness (55%) and dyspareunia (44%).3 In addition to these vulvovaginal symptoms, lower urinary tract symptoms can also occur after menopause onset; this led to the 2014 proposal to replace VVA with the more inclusive term genitourinary syndrome of menopause (GSM).1 For the purposes of this article, the term VVA will be used to avoid inconsistencies in terminology as US prescribing inserts of treatments discussed herein commonly refer to vulvar and vaginal atrophy rather than GSM.
Although there is a high prevalence of VVA (over 50% of postmenopausal women report symptoms),2 it is typically underdiagnosed and undertreated, with only 56% of postmenopausal survey participants with vulvovaginal symptoms reporting a discussion of their problem with a healthcare provider.3 Although other bothersome symptoms of menopause—such as flushes, hot flashes, and night sweats—can wane over time, vulvovaginal symptoms are chronic and can intensify if untreated.5 Nonhormone moisturizers and lubricants can relieve mild symptoms, but have a brief window of effectiveness (<24 h per use) and fail to reverse many atrophic signs.2 In the 2017 position statement from The North American Menopause Society (NAMS), it is recommended that estrogen treatment for vulvovaginal symptoms be individualized by offering the most appropriate dose, route of administration, regimen, and duration of use that results in maximal benefits with minimal risk. For example, lower-dose vaginal estrogen is recommended for vulvovaginal symptoms that fail to respond to nonhormone measures or are moderate–severe in their intensity.5 Using appropriately low vaginal estrogen doses is consistent with the US Food and Drug Administration (FDA) guidance on estrogen treatment for menopause symptoms.6 Topical, localized estrogen treatments via vaginal tablets, rings, or creams reduce systemic estrogen exposure.2,7
The estradiol vaginal cream 0.01% (Estrace [Allergan USA, Inc, Irvine, CA], 0.1 mg estradiol/g) is an FDA-approved topical treatment for postmenopausal VVA.8 The objective of this study was to examine the efficacy and safety of 3 times weekly dosing of a lower-dose estradiol vaginal cream (0.003% estradiol/g; 15 μg estradiol in 0.5 g cream) compared with placebo vaginal cream in postmenopausal women with VVA signs and dyspareunia.
METHODS
This study was performed in compliance with the International Conference on Harmonization Harmonized Tripartite Guideline for good clinical practice guidelines and in accordance with the ethical principles originating from the Declaration of Helsinki and the US FDA Code of Federal Regulations Title 21, parts 50, 56, and 312. The protocol was reviewed and approved by Institutional Review Boards and all participants provided written informed consent.
Study design
This was a phase 3, randomized, double-blind, placebo-controlled, multicenter study in postmenopausal women reporting dyspareunia as the most bothersome symptom of VVA. Once screening and baseline assessments were completed, participants were randomized (1:1) to estradiol vaginal cream 0.003% (15 μg estradiol; 0.5 g cream) or placebo cream (0.5 g of cream). During the 2-week initial treatment period, estradiol and placebo creams were applied vaginally every day for 2 weeks to rapidly maximize vaginal response. Dosages for both treatments were then reduced to three maintenance applications per week for 10 weeks. After completion of the 12-week trial, those participants who had an intact uterus at baseline were provided a progestin for 14 days; the type and dose of progestin were determined by the investigator.
Participants
Postmenopausal women were recruited if they met at least one of the following criteria: (1) ≥40 years of age with hysterectomy and follicle-stimulating hormone (FSH) levels >40 mIU/mL; (2) ≥35 years of age with bilateral oophorectomy and FSH levels >40 mIU/mL; (3) ≥40 years of age with 12 months of amenorrhea; or (4) ≥40 years of age with 6 months of amenorrhea and FSH levels >40 mIU/mL. Participants were also required to self-identify as sexually active and experiencing dyspareunia of moderate–severe intensity that was considered by the participants to be the most bothersome VVA symptom. Additional inclusion criteria included ≤5% superficial cells on a vaginal cytology smear; vaginal pH >5.0; documentation of a negative mammogram if >40 years of age; and a normal clinical breast examination before enrollment.
Exclusion criteria for the study were as follows: untreated hypertension; porphyria; abnormal history of or suspected genetic component for thrombophlebitis or thromboembolic disorders; or abnormal Pap smear at screening suggestive of at least a low-grade squamous intraepithelial lesion. Participants could not be using vaginal (eg, creams, gels, rings) or transdermal estrogen products within 4 weeks, hormonal intrauterine devices or oral estrogen products within 8 weeks, progestin implants or estrogen injections within 3 months, or estrogen pellet or progestin injections within 6 months of screening.
Assessments
Severity of dyspareunia was measured in sexually active participants via self-assessment using a 4-point scale: 0 = none (symptom is not present); 1 = mild (symptom is present but may be intermittent and does not interfere with activities/lifestyle); 2 = moderate (symptom is present and only occasionally interferes with activities/lifestyle); and 3 = severe (symptom is present and bothersome and activities/lifestyle have been modified because of it). Vaginal pH was measured using pH paper (values <4 or >7 were recorded as 4 or 7, respectively) at screening and week 12, and participants were asked to abstain from sexual intercourse for 48 h before assessment. Vaginal cytology was assessed at screening and week 12 to determine the percentage of superficial and parabasal cells. Vaginal and/or vulvar itching, dysuria, and vaginal dryness were self-assessed on a 4-point scale (0 = none; 1 = mild; 2 = moderate; and 3 = severe), and vaginal bleeding associated with sexual activity was classified as present or not present if the participant verified sexual activity. Extent of vaginal atrophy, pallor, vaginal dryness, friability, and petechiae were determined by the investigator via visual examination using a 4-point scale (0 = none; 1 = mild; 2 = moderate; and 3 = severe). These assessments occurred at screening and weeks 2, 4, 8, and 12.
Safety was evaluated throughout the study including through adverse event (AE) reporting and vital signs at each visit and at baseline and week 12 via physical and gynecological examinations and clinical laboratory tests.
Outcomes
The three coprimary outcomes of this study were change in self-assessed severity of dyspareunia, change in the vaginal cytology (the percentage of vaginal superficial and parabasal cells), and vaginal pH from baseline to final assessment. Secondary outcomes were change from baseline to weeks 2, 4, 8, and 12 in severity of dyspareunia, change from baseline to weeks 2, 4, 8, 12, and final assessment in severity vaginal/vulvar irritation, itching, dysuria, and the number of participants with vaginal bleeding related to sexual activity. Additional outcomes included change from baseline to week 12 and final assessment in vaginal atrophy, pallor, dryness, friability, and petechiae, which were scored and analyzed.
Statistical analysis
The safety population included all participants who were randomized and took ≥1 dose of study drug. Baseline demographic and clinical characteristics, vital signs, AEs, gynecological examination results, and clinical laboratory values were summarized by treatment in the safety population using descriptive statistics. The modified intention-to-treat population (mITT) consisted of all safety population participants who had ≥1 postbaseline efficacy assessment and met all specific inclusion criteria. Efficacy analyses were performed in the mITT population. For the primary outcomes, normality was assessed via Shapiro–Wilk test in conjunction with normality figures/plots and homogeneity of variance was determined via Levene's test and significance was set at 0.05 for both. If the assumptions of normality and homogeneity of variance were met, an analysis of covariance (ANCOVA) was used with treatment and site as fixed effects and baseline value as the covariate. If assumptions were not met, a ranked ANCOVA9 was used with the same model as above. Estradiol vaginal cream was considered efficacious versus placebo if all three coprimary efficacy variables provided P values <0.05. No adjustment for multiple comparisons was made for this study.
Secondary efficacy outcomes were evaluated via ANCOVA or rank ANCOVA with the same methods as described for the primary outcomes, with the exception of vaginal bleeding associated with sexual activity. This outcome was analyzed with the Cochran–Mantel–Haenszel test using pooled site as a stratification factor. Responses of “not applicable” (NA) to dyspareunia severity with or without (including NA) the presence of vaginal bleeding were excluded.
It was estimated that a total of 454 participants needed to be enrolled to allow for a final population of 440 participants. This sample size would provide at least 90% power to find a difference between the estradiol vaginal cream and placebo treatment with an overall α-level of 0.05. A greater number of participants were randomized as a result of protocol amendments requiring all screened and randomized participants to have ≤5% superficial cells on vaginal smear, a vaginal pH >5, and moderate–severe dyspareunia as the most bothersome VVA symptom. All statistical analyses were performed using SAS (v 9.3); all tests were 2-sided, and significance was set at 0.05.
RESULTS
A total of 550 participants were randomized in the study with 548 participants in the safety population and 472 in the mITT population (Fig. 1). Most participants were white and had an average age of 58 years (Table 1). The mean ± SD study drug applications for both treatment groups combined were 13.6 ± 1.5 in weeks 1 and 2 (daily applications) and 28.7 ± 4.5 after week 2 (3 times weekly applications for 10 weeks), for a total of 41.4 ± 7.6 applications.
FIG. 1.
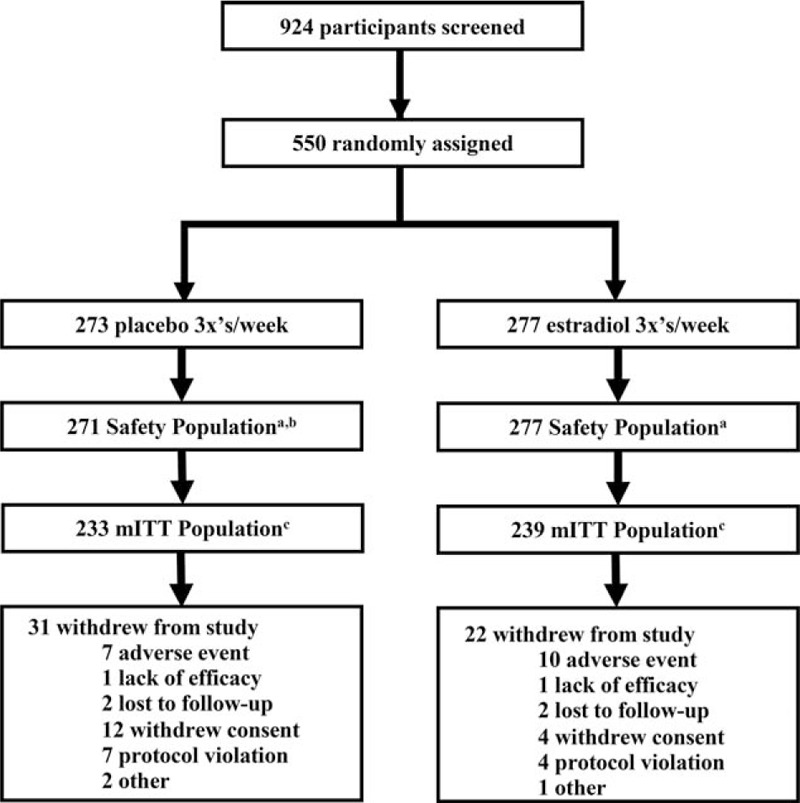
Participant disposition. aIncludes all randomized participants who received at least one dose of study drug. bTwo randomized participants returned all dispensed study drug unused, with seals intact. cIncludes safety population participants who had at least one postbaseline primary efficacy assessment and met all of the following inclusion criteria: ≤5% superficial cells on a vaginal wall smear; >5.0 vaginal pH; moderate–severe dyspareunia as the most bothersome symptom. mITT, indicates modified intent-to-treat.
TABLE 1.
Baseline demographic and clinical characteristics of randomized participants
| Demographic variablesa | Placebo (n = 271) | Estradiol (n = 277) |
| Age (y), mean ± SD | 58.6 ± 6.1 | 58.7 ± 6.4 |
| Not Hispanic/Latino ethnicity, n (%) | 248 (91.5) | 249 (89.9) |
| Race, n (%)b | ||
| White | 248 (91.5) | 255 (92.1) |
| Black | 23 (8.5) | 21 (7.6) |
| Asian | 2 (0.7) | 1 (0.4) |
| American Indian/Alaska Native | 0 | 2 (0.7) |
| Native Hawaiian/Pacific Islander | 1 (0.4) | 0 |
| Height (m), mean ± SD | 1.63 ± 0.07 | 1.63 ± 0.07 |
| Weight (kg), mean ± SD | 70.9 ± 13.6 | 70.8 ± 15.0 |
| BMI (kg/m2), mean ± SD | 26.7 ± 5.3 | 26.7 ± 5.2 |
| Clinical characteristics, mean ± SDc | Placebo (n = 233) | Estradiol (n = 239) |
| Dyspareuniad | 2.7 ± 0.4 | 2.7 ± 0.5 |
| Vaginal pHd | 6.35 ± 0.66 | 6.37 ± 0.66 |
| Percentage of vaginal cellsd | ||
| Superficial | 0.2 ± 0.8 | 0.2 ± 0.7 |
| Parabasal | 50.6 ± 43.1 | 53.5 ± 42.0 |
| Vaginal and/or vulvar irritation/itching | 0.9 ± 0.9 | 1.0 ± 0.9 |
| Dysuria | 0.4 ± 0.7 | 0.4 ± 0.7 |
| Vaginal dryness | 2.3 ± 0.8 | 2.3 ± 0.7 |
Dyspareunia, vaginal/vulvar irritation/itching, dysuria, and vaginal dryness severity scores: 0 = none, 1 = mild, 2 = moderate, 3 = severe.
BMI, body mass index; mITT, modified intent-to-treat.
aSafety population.
bFive participants reported multiple races.
cmITT population.
dCoprimary assessments.
From baseline to final assessment, estradiol significantly reduced the severity of dyspareunia (mean change from baseline ± SD: −1.5 ± 1.0 estradiol vs −1.2 ± 0.9 placebo), decreased vaginal pH (−1.36 ± 0.89 vs −0.53 ± 0.92), increased the percentage of superficial cells (10.1 ± 16.7 vs 1.4 ± 6.1), and decreased the percentage of parabasal cells compared with placebo (−48.5 ± 45.1 vs −14.6 ± 39.6; P < 0.001, all; Table 2). Dyspareunia severity was significantly reduced in the estradiol versus the placebo group by weeks 8 (−1.5 ± 1.0 vs −1.2 ± 0.9; P = 0.004) and 12 (−1.5 ± 1.0 vs −1.2 ± 0.9; P < 0.001; Fig. 2A). There were no significant improvements with estradiol on severity of vaginal/vulvar irritation/itching (Fig. 2B). Estradiol significantly reduced the severity of vaginal dryness at week 12 (−1.2 ± 0.9 vs −0.9 ± 1.0; P = 0.001) and final assessment (−1.2 ± 1.0 vs −0.8 ± 1.0; P < 0.001; Fig. 2C). There were no discernable differences between placebo and estradiol on severity of dysuria (data not shown).
TABLE 2.
Change from baseline to final assessment in primary outcomes (mITT population)
| Mean ± SD | Placebo (n = 233) | Estradiol (n = 239) | Pa |
| Severity of vaginal dyspareunia | −1.2 ± 0.9 | −1.5 ± 1.0 | <0.001 |
| Vaginal pH | −0.53 ± 0.92 | −1.36 ± 0.89 | <0.001 |
| Percentage of vaginal cells | |||
| Superficial | 1.4 ± 6.1 | 10.1 ± 16.7 | <0.001 |
| Parabasal | −14.6 ± 39.6 | −48.5 ± 45.1 | <0.001 |
Dyspareunia severity scores: 0 = none, 1 = mild, 2 = moderate, 3 = severe. Italic values indicate significance.
mITT, modified intent-to-treat.
aAnalysis of covariance on rank vs placebo.
FIG. 2.
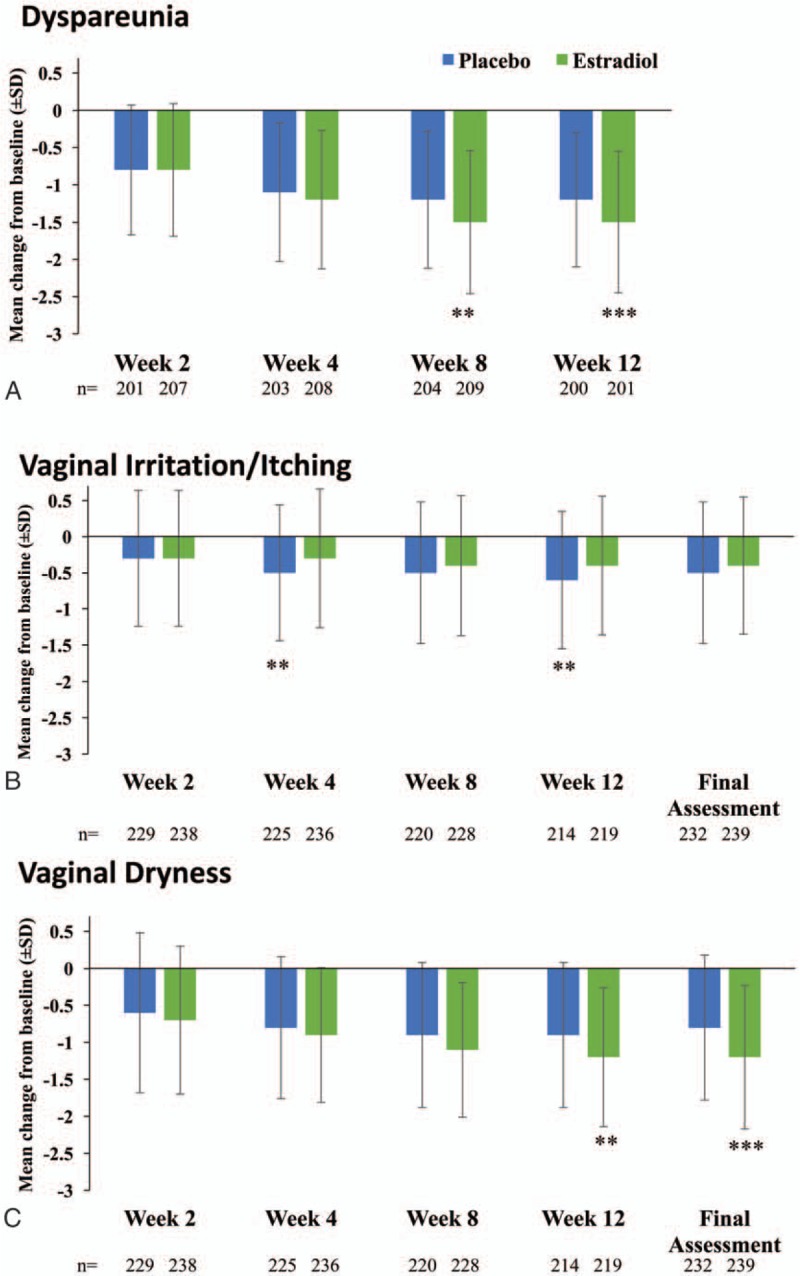
Mean (±SD) change from baseline in self-assessed severity of dyspareunia (A), vaginal irritation/itching (B), and vaginal dryness (C; mITT Population). Dyspareunia, vaginal/vulvar irritation/itching, and vaginal dryness, severity scores: 0 = none, 1 = mild, 2 = moderate, 3 = severe. Data for final assessment for vaginal dryness was a coprimary endpoint and is reported in Table 2 above. ∗∗∗P < 0.001; ∗∗P < 0.01; panels A and C; vs estradiol, panel B. mITT, modified intent-to-treat.
Of the participants who reported sexual activity at baseline (239 estradiol; 233 vehicle), 27.0% (63/233) and 28.0% (67/239) of those in the estradiol and placebo groups, respectively, also reported the presence of sexual activity-related vaginal bleeding. Fewer participants reported sexual activity (201 estradiol; 199 placebo) and related bleeding by week 12 (7.5% [15/201] estradiol; 12.1% [24/199] placebo), though no statistically significant differences could be discerned between the estradiol and placebo groups at any time point except final assessment (6.5% [15/231] estradiol; 14.4% [33/229] placebo; P = 0.006). The remaining secondary outcomes of severity of VVA symptoms, pH, and percentage of superficial and parabasal cells on vaginal smear were significantly improved from baseline at week 12 in the estradiol group compared with the placebo group (P < 0.001, all; Table 3). Severity of VVA symptoms were also significantly improved from baseline at final assessment in the estradiol group versus the placebo group (P < 0.001, all; data not shown).
TABLE 3.
Change from baseline to week 12 in secondary outcomes (mITT population)
| Mean ± SD | Placebo (n = 233) | Estradiol (n = 239) | Pa |
| Atrophyb | −0.5 ± 0.8 | −0.9 ± 0.8 | <0.001 |
| Pallorb | −0.6 ± 0.8 | −0.9 ± 0.8 | <0.001 |
| Drynessb | −0.5 ± 0.9 | −0.9 ± 0.9 | <0.001 |
| Friabilityb | −0.6 ± 1.0 | −1.0 ± 1.0 | <0.001 |
| Petechiaeb | −0.3 ± 0.8 | −0.6 ± 0.9 | <0.001 |
| pH | −0.53 ± 0.93 | −1.35 ± 0.89 | <0.001 |
| Percentage of vaginal cells | |||
| Superficial | 1.2 ± 5.4 | 10.5 ± 17.2 | <0.001 |
| Parabasal | −14.9 ± 39.9 | −48.2 ± 45.7 | <0.001 |
Italic values indicate significance.
mITT, modified intent-to-treat.
aAnalysis of covariance on rank vs placebo.
bVisual inspection score: 0 = none, 1 = mild, 2 = moderate, and 3 = severe.
Safety
The number of participants reporting at least one treatment-emergent AE (TEAE) was comparable between the placebo (49.8%) and estradiol groups (52.3%; Table 4). The most frequently reported TEAE (occurring in ≥5% of estradiol treated participants) was vulvovaginal mycotic infections (6.9% estradiol vs 3.3% placebo; Table 4). TEAEs leading to study discontinuation occurred in slightly more participants in the estradiol group (2.9%) than in the placebo group (2.2%). The majority of reported TEAEs were mild–moderate (49.5% estradiol; 46.1% placebo). Serious TEAEs were reported by four participants: one in the placebo group and three in the estradiol group. One serious/severe event (deep vein thrombosis) in the estradiol group was considered related to study drug and led to study discontinuation (Table 4). No deaths occurred. At study end, no clinically relevant trends in laboratory values or vital signs were observed, and no differences were seen on gynecological exams between the two treatment groups (data not shown).
TABLE 4.
Adverse events (safety population)
| n (%) | Placebo (n = 271) | Estradiol (n = 277) |
| At least 1 TEAE | 135 (49.8) | 145 (52.3) |
| At least 1 treatment-related TEAE | 58 (21.4) | 57 (20.6) |
| TEAEs leading to discontinuation | 6 (2.2) | 8 (2.9) |
| Serious TEAEs | 1 (0.4) | 3 (1.1) |
| Deaths | 0 | 0 |
| TEAEs occurring ≥5% participants in the estradiol treatment group | ||
| Vulvovaginal mycotic infection | 9 (3.3) | 19 (6.9) |
This table presents the number (%) of participants with at least one event in the respective category. Related TEAEs are events reported with “possible” or “probable” relationship to study drug.
TEAE, treatment-emergent adverse event.
DISCUSSION
The results of this study show that a lower-dose estradiol vaginal cream (0.003%/15 μg) met all three coprimary endpoints in postmenopausal women with VVA. Estradiol vaginal cream was efficacious compared with placebo in reducing the severity of dyspareunia, decreasing vaginal pH, and improving the percentage of vaginal smear superficial cells while reducing parabasal cells from baseline to final assessment. These results also indicate that local low-dose vaginal estrogen, delivered at 15 ug/dose, is a highly effective method of treatment. Localized low-dose delivery has the advantage of preventing an appreciable increase in systemic estrogen exposure.5
Significant differences were discerned between estradiol and placebo groups on the secondary outcomes of severity of dyspareunia and dryness by week 12. As there are few lower-dose estrogen studies that treated participants for longer than 12 weeks,10 longer-term trials are needed to determine the safety of extended lower-dose hormonal treatment for VVA. Severity of dysuria only differed between the two treatment groups at week 12, which may have been the result of the population that was enrolled because dyspareunia was the most bothersome VVA symptom and dysuria was not an inclusionary requirement. Thus, dysuria symptom ratings at baseline were mild or absent in most participants (mean score [SD] 0.4 [0.7] in both groups).
Estradiol 0.003% provides a lower vaginal dose of 30 μg/g per application (15 μg/0.5 g in this study), similar to the lower dose vaginal estradiol tablets currently approved in the United States (10-25 μg/tablet)11 and, in contrast to the FDA-approved vaginal estrogen creams currently available, Estrace 0.01% (0.1 mg/g)8 and Premarin (0.625 mg/g).12 This approach corresponds with the NAMS and FDA recommendations to decrease systemic estrogen exposure by using the lowest effective vaginal estrogen dose to treat VVA.5,6 Postmenopausal women with VVA using a prescription estrogen treatment have reported concerns over long-term safety, hormone exposure, and general side effects3; these concerns, which may negatively affect medication adherence,13 provide additional justification to prescribe appropriately low local estrogen doses. Furthermore, local application of low-dose vaginal estrogen may be an appropriate treatment for certain women with moderate–severe VVA for whom systemic absorption of estrogen would pose greater risk than benefit.5
Treatment with the estradiol vaginal cream was well tolerated as demonstrated by the similar rates of TEAEs and discontinuations between the two treatment groups; the exception was the greater frequency of vulvovaginal mycotic infections in the estradiol group. These findings are not unexpected, and may reflect the impact of estrogen on decreasing vaginal pH, a shift in the vaginal microbiome,14 or a direct effect of estrogen on candida species.15
The dosing regimen of this study reflected current clinical guidelines published by NAMS5; initial local estradiol vaginal cream application starts with a daily priming dose for 2 weeks and then decreases the dosing frequency to a lower maintenance level requiring fewer applications. The lower dose contained in the estradiol cream effectively reduced the severity of dyspareunia suggesting that it may be a treatment option for women who have VVA with this primary complaint. Furthermore, the low vaginal dose may help ease participants’ concerns over the safety of systemic hormonal exposure.
CONCLUSIONS
Lower-dose estradiol vaginal cream dosed 3 times weekly (15 μg/0.5 g per application) is a safe and effective treatment for VVA-related dyspareunia in postmenopausal women. This dosing regimen reflects current clinical guidelines for lower dose estrogen treatment. Lower-dose estradiol vaginal cream may provide another treatment option for women who are concerned over the safety of systemic estrogen exposure or for those whom greater doses of estrogen may be contraindicated.
Acknowledgments
Medical writing and editorial assistance for this manuscript was provided by Lynn M. Anderson, PhD and Jacqueline Benjamin, PhD of Prescott Medical Communication Group (Chicago, IL) and funded by Allergan plc.
Footnotes
Funding/support: Allergan plc.
Financial disclosure/conflicts of interest: RK has received research grants from Allergan, Amneal, Glenmark, Endoceutics, Teva, Izun, and TherapeuticsMD. Dr Kroll has also received consultant fees from Allergan and AMAG. DA reports grants from Actavis/Allergan; grants and personal fees from Bayer Healthcare, grants and personal fees from Endoceutics, personal fees and other from Agile Therapeutics, personal fees from Exeltis, grants from Glenmark, other from InnovaGyn, grants and personal fees from Merck, personal fees from Pfizer, grants and personal fees from Radius health, personal fees from Sermonix Pharmaceuticals, grants and personal fees from Shionogi, personal fees from TEVA Women's Healthcare, grants and personal fees from TherapeuticsMD outside the submitted work. YL and VS are employees of Allergan plc. JL is a consultant to Allergan and Pfizer. Dr Liu is also involved in clinical trials funded by Ferring Pharmaceuticals, AbbVie, Bayer, Palatin, and Allergan.
REFERENCES
- 1.Portman DJ, Gass ML. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and the North American Menopause Society. Menopause 2014; 21:1063–1068. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, et al. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol 2016; 215:704–711. [DOI] [PubMed] [Google Scholar]
- 3.Kingsberg SA, Wysocki S, Magnus L, Krychman ML. Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. J Sex Med 2013; 10:1790–1799. [DOI] [PubMed] [Google Scholar]
- 4.American Family Physician Editors. Practice guidelines: ACOG releases clinical guidelines on management of menopausal symptoms. Am Fam Physician 2014; 90:338–340. [Google Scholar]
- 5.The North American Menopause Society. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause 2017; 24:728–753. [DOI] [PubMed] [Google Scholar]
- 6.US Food and drug Administration. Industry Guidance: Estrogen and Estrogen/Progestin Drug Products to Treat Vasomotor Symptoms and Vulvar and Vaginal Atrophy Symptoms—Recommendations for Clinical Evaluation. Rockville, MD: US Department of Health and Human Services; 2003. [Google Scholar]
- 7.Santen RJ. Vaginal administration of estradiol: effects of dose, preparation and timing on plasma estradiol levels. Climacteric 2015; 18:121–134. [DOI] [PubMed] [Google Scholar]
- 8.Estrace® (estradiol USP, 0.01% vaginal cream). US Prescribing Information. Irvine, CA: Allergan USA, Inc; 2015. Available at: http://www.allergan.com/assets/pdf/estrace_pi [Google Scholar]
- 9.Conover WJ, Iman RL. Analysis of covariance using the rank transformation. Biometrics 1982; 38:715–724. [PubMed] [Google Scholar]
- 10.Rahn DD, Carberry C, Sanses TV, Mamik MM, Ward RM, Meriwether KV, et al. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstet Gynecol 2014; 124:1147–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vagifem® (estradiol vaginal inserts). US Prescribing Information. Plainsboro, NJ: Novo Nordisk Inc; 2016. [Google Scholar]
- 12.Premarin® (conjugated estrogens vaginal cream). US Prescribing Information. Philadelphia, PA: Wyeth Pharmaceuticals Inc; 2014. [Google Scholar]
- 13.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353:487–497. [DOI] [PubMed] [Google Scholar]
- 14.Shen J, Song N, Williams CJ, Brown CJ, Yan Z, Xu C, et al. Effects of low dose estrogen therapy on the vaginal microbiomes of women with atrophic vaginitis. Sci Rep 2016; 6:24380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng G, Yeater KM, Hoyer LL. Cellular and molecular biology of Candida albicans estrogen response. Eukaryot Cell 2006; 5:180–191. [DOI] [PMC free article] [PubMed] [Google Scholar]


