Abstract
Spontaneous preterm birth (sPTB) is the leading cause of neonatal morbidity and mortality globally. Accurate prediction of sPTB would enable targeting of interventions such as admission to hospital, antenatal corticosteroids, magnesium sulphate and in utero transfer as well as guiding prophylactic treatment (e.g., cerclage or progesterone). Measurement of fetal fibronectin concentration in the cervicovaginal fluid is a known predictor of sPTB. Traditionally a positive/negative test (defined by a threshold of 50 ng/ml), recent work has demonstrated improved prediction when used as a quantitative test, whereby the concentration of fetal fibronectin is measured by an automated bedside reader. This review examines the evidence surrounding the use of quantitative fetal fibronectin in asymptomatic women at high risk of sPTB, as well as those with symptoms of threatened sPTB.
Keywords: cervicovaginal fluid, corticosteroids, prediction, preterm, quantitative fetal fibronectin
Preterm birth, birth of an infant prior to 37 completed weeks of gestation, is responsible for over one million neonatal deaths per year [1]. Those infants who survive may suffer long-term prematurity related complications including cerebral palsy, neurodevelopmental delay, deafness, visual impairment and chronic lung disease. Global estimates of the prevalence of preterm birth are imprecise and varied, but data collected in 2010 from 184 countries suggested that an estimated 11.1% of all live births were preterm [2]. Iatrogenic preterm delivery (physician initiated birth due to concerns about maternal or fetal well-being) accounts for three in ten preterm births, but the remaining 70% are spontaneous in onset, either following spontaneous onset of uterine contractions resulting in delivery, or preterm prelabor rupture of membranes (PPROM) [3]. Although the exact cause of spontaneous preterm birth (sPTB) is unknown, the etiology is thought to be multifactorial with complex interactions between the maternal genome and environment, including infection and inflammation, steroid hormone imbalance, uterine distension, cervical insufficiency and placental vascular causes. Worryingly, the global incidence of preterm birth is thought to be rising [2].
Currently, the treatment of threatened sPTB is focused on optimizing neonatal outcomes for the preterm infant. Antenatal corticosteroids are administered to develop the immature lungs of the fetus, magnesium sulphate given as neuroprotection to reduce the risk of cerebral palsy and tocolytic drugs (which suppress uterine contractions) may delay delivery by 48 h to 7 days, allowing time for antenatal drugs to be administered and/or transfer of the mother prior to delivery to a more appropriate birth setting. Prior to presenting with symptoms of sPTB, preventative treatments can be targeted to asymptomatic women considered high risk for subsequent preterm birth (e.g., previous preterm birth or late miscarriage, uterine anomaly or previous invasive cervical surgery). While trials have shown conflicting results, the use of cervical cerclage (an operative stitch), Arabin pessary (silicon device placed around the cervix to provide structural support and encourage remodeling) and vaginal progesterone pessaries, have been demonstrated to reduce the risk of premature birth by approximately 50% in women at high risk in whom cervical shortening (<25 mm) is detected on transvaginal ultrasound scan [4–6].
The majority of women presenting with symptoms of threatened preterm labor will deliver at term in the absence of any intervention. Furthermore, some women who receive prophylactic intervention may still deliver prematurely. The challenge is therefore to predict which women are at the highest risk of sPTB, in order to target preventative intervention, admission to hospital, place of birth decisions and in utero therapies to improve fetal outcomes, to those who will benefit most, avoiding unnecessary treatment in those women who do not need it. This review will describe the potential role of the quantitative fetal fibronectin (qfFN) test in both asymptomatic and symptomatic women for prediction of sPTB.
Fetal fibronectin
Fetal fibronectin (fFN) is an extracellular matrix glycoprotein produced by fetal cells located between the chorion and decidua at the interface of the amniotic membranes. Prior to the fusion of the decidua and fetal membranes, fFN may leak into the cervicovaginal fluid (CVF). After fusion, fFN concentrations should drop to low levels and may become undetectable from 18 weeks' gestation. After this time, it may be released into the CVF after presumed inflammatory, infectious or mechanical damage to the extracellular matrix; its presence at high concentrations is thus associated with high risk of subsequent sPTB. The CVF sample is obtained using a dacron swab introduced into the posterior fornix of the vagina and left to saturate for 10 s, during speculum examination. The swab is then placed in a buffer solution, and analyzed immediately by pipetting 200 μl of the sample onto a cassette containing a lateral flow immunochromatographic test strip which is read using a bedside automated instrument (Rapid fFN TLiIQ analyzer; Hologic, MA, USA), or alternatively, a visually interpreted dipstick test (QuikCheck™, Hologic). Testing is not recommended after recent sexual intercourse (<48 h) [7] or in the presence of moderate or gross vaginal bleeding due to known interference with the assay, giving a false-positive estimation of risk. It can be performed with minimal training by anyone competent to use a vaginal speculum.
fFN is increasingly used in Europe and North America as a prediction test for asymptomatic women at high risk of sPTB, and women who present with symptoms of sPTB, who are yet to show signs of cervical dilation. Until recently, it has been used as a qualitative test, giving a positive or negative result based on a CVF fFN concentration of above and below 50 ng/ml. This threshold was assigned as a balance between optimal sensitivity and specificity [8], and its greatest value lies in its high negative predictive value (building on the already low prevalence of preterm birth even among high-risk women). In a cohort of 2929 asymptomatic women tested at 24–26 weeks of gestation, the Preterm Prediction Study [9] demonstrated a negative predictive value of 96% for sPTB less than 35 weeks of gestation. Similarly, among women presenting with symptoms of preterm labor between 24 and 34 weeks of gestation with cervical dilation less than 3 cm, the negative predictive value (NPV) is 82–99% for subsequent delivery within 14 days [10,11], enabling reassurance, and discharge from intensive surveillance. Unfortunately, the positive predictive value (PPV) is suboptimal for both symptomatic and asymptomatic women (<30%) [9–12]. Given that a recent Cochrane meta-analysis suggested that knowledge of cervicovaginal fFN test status results in lower spontaneous PTB rates by identifying a much higher risk group of women [13], a test with improved positive prediction, enabling enhanced targeting of intervention to women most likely to benefit would likely be of great value.
Quantitative fetal fibronectin
qfFN, a measure of the absolute concentration of fFN in the CVF, has been demonstrated to improve prediction compared with the traditional qualitative test. Secondary analysis of the Preterm Prediction study, 2926 asymptomatic patients with an average risk of sPTB, demonstrated that the risk of sPTB increased as a function of rising fFN concentration from 20 to 300 ng/ml [9]. These findings were mirrored by secondary analysis from Kurtzman et al. [14] who demonstrated that in women with at least one previous preterm birth (n = 563), rates of sPTB rose progressively with rising qfFN concentrations at 24 weeks (relative risk [RR]: 9.9 for women with qfFN concentration >200 ng/ml compared with 0 ng/ml). The EQUIPP study (Evaluation of a Quantitative Instrument for the Prediction of Preterm Birth) was the first to prospectively demonstrate the enhanced value of quantification of fFN (detectable range 0 to >500 ng/ml), measured using an automated bedside analyzer (Rapid fFN 10Q analyzer; Hologic). For both asymptomatic and symptomatic women, use of alternative fFN thresholds (10, 50, 200 and 500 ng/ml) enhanced the PPV for sPTB, while the NPV remained high at every threshold. One thousand four hundred and forty eight high-risk women (previous premature birth, premature rupture of the fetal membranes or late miscarriage, previous cervical surgery, uterine abnormality or short cervix <25 mm) asymptomatic of threatened preterm labor had CVF qfFN concentration (blinded) measurements between 22 and 27 weeks of gestation. Rate of sPTB (<34 weeks of gestation) increased from 3, 11, 15, 34 and 48% respectively with increasing fFN threshold concentrations. A threshold of 200 ng/ml had a superior positive prediction (38%) compared with the qualitative positive test (14%), while maintaining high specificity (96%; see Table 1). Women with the lowest concentration of qfFN (<10 ng/ml, comprising 70% of the cohort) could therefore be reassured that despite their high-risk status, their risk of sPTB is no higher than the background hospital population rate, enabling reassurance and discharge from intensive cervical surveillance [15]. Women with higher qfFN concentrations may benefit from more frequent cervical surveillance, and intervention such as cerclage, bed rest and antenatal fetal therapies could be targeted to those at the highest risk.
Table 1.
Prediction of spontaneous preterm birth within 2 weeks of testing according to quantitative fetal fibronectin threshold in symptomatic women (n = 300).
| Predictive variable | Fetal fibronectin threshold (ng/ml) | |||
|---|---|---|---|---|
| 10 or greater | 50 or greater | 200 or greater | 500 or greater | |
| Sensitivity (%) | 82.4 | 76.5 | 58.8 | 35.3 |
| Specificity (%) | 59.3 | 81.1 | 93.9 | 97.5 |
| NPV (%) | 98.2 | 98.3 | 97.4 | 96.1 |
| PPV (%) | 10.9 | 19.7 | 37.0 | 46.2 |
| Positive likelihood ratio | 2.02 | 4.04 | 9.69 | 14.12 |
| Negative likelihood ratio | 0.30 | 0.29 | 0.44 | 0.66 |
NPV: Negative predictive value; PPV: Positive predictive value.
Adapted with permission from [16].
Similar trends were seen in the symptomatic cohort (n = 300). Only 1.8% of women symptomatic of threatened preterm birth between 22 and 35 weeks of gestation with a qfFN concentration of <10 ng/ml (comprising 57% of the cohort of 300 women) delivered within 2 weeks of testing. In comparison, the PPV for delivery before 34 weeks of gestation increased from 19, 32, 61 and 75% and for delivery within 14 days; 11, 20, 37 and 46% with increasing thresholds (10, 50, 200 and 500 ng/ml) [16], while the NPV remained greater than 95% (see Table 2). These results have been successfully validated [17,18], with area under the receiver operating characteristic (ROC) curve for prediction of sPTB <30–37 weeks' gestation of 0.77–0.99 [16,17].
Table 2.
Prediction of spontaneous preterm birth before 34 weeks of gestation according to quantitative fetal fibronectin threshold for asymptomatic women (n = 1433).
| Predictive variable | Fetal fibronectin threshold (ng/ml) | |||
|---|---|---|---|---|
| 10 or greater | 50 or greater | 200 or greater | 500 or greater | |
| Sensitivity (%) | 73.3 | 46.5 | 28.7 | 9.9 |
| Specificity (%) | 72.2 | 88.7 | 96.4 | 99.2 |
| PPV (%) | 16.7 | 23.7 | 37.7 | 47.6 |
| NPV (%) | 97.3 | 95.6 | 94.7 | 93.6 |
| Positive likelihood ratio | 2.64 | 4.10 | 7.97 | 12.0 |
| Negative likelihood ratio | 0.37 | 0.60 | 0.74 | 0.91 |
NPV: Negative predictive value; PPV: Positive predictive value.
Adapted with permission from [15].
It is likely that qfFN can be used alongside, indeed enhancing the value of, other predictive tests for sPTB tests such as cervical length (CL) measurement. CL measurement has been demonstrated to predict sPTB when used as a mid-trimester screening test at a similar magnitude to use of qfFN alone; ROC area under the curve (AUC) for prediction of delivery less than 34 weeks of gestation using CL was AUC 0.82 (0.77–0.87) versus 0.78 (073–0.84) using qfFN in the EQUIPP cohort [15] using qfFN. In this cohort, a combination of CL and qfFN predicted sPTB less than 34 weeks ROC AUC of 0.84 (0.79–0.89). This was superior to fFN alone (0.79; 0.74–0.85; p<0.01). However, use of concurrent qfFN testing has been show to risk discriminate among those women found to have a short cervix. In the EQUIPP asymptomatic cohort [15], among women screened between 22 and 27 weeks of gestation and found to have a CL of <25 mm, 9.5% delivered prematurely <34 weeks of gestation if qfFN concentration was <10 ng/ml, compared with 55.1% with concentration >200 ng/ml. In isolation both CL and fFN can be used depending on the skills and equipment available. If knowledge of risk proves to be valuable, then both can be used as they are partly independent. Given that many women with a short cervix will not deliver early, the additional risk discrimination afforded by qfFN may help inform which women are most likely to benefit from prophylactic intervention (such as progesterone or cerclage) currently recommended for women with a short cervix. Furthermore, a proportion of women who deliver prematurely have a long cervix at the time of mid-trimester screening. Further trials are required to evaluate how qfFN may be used to identify asymptomatic women who would benefit from prophylactic intervention, both in the presence and absence of cervical shortening.
Clinical implications of qfFN testing
Use of these qfFN thresholds could enable clinicians to make decisions based on individual risk. To be useful in this context, a predictive test must have a high sensitivity (proportion of preterm births correctly identified), and a high NPV (the proportion with negative tests who do not go onto give birth preterm). For both symptomatic and asymptomatic women, using a threshold of 10 ng/ml has sufficiently high sensitivity and NPV to determine which high-risk women are unlikely to deliver preterm. It would provide reassurance for the woman presenting with symptoms of preterm labor, and give the clinician confidence to discharge and avoid a costly admission to hospital or unnecessary in utero therapies. This is particularly pertinent when considering timing of antenatal corticosteroid administration. In current clinical practice, it has become commonplace to administer steroids to all women presenting to hospital with signs of preterm labor, as these have been shown to reduce risk of fetal and neonatal death (RR: 0.77; 95% CI: 0.67–0.89) with a 44% reduction in subsequent respiratory distress syndrome (RR: 0.66; 95% CI: 0.59–0.73; 21 studies; 4038 infants) [19]. However, timing of these steroids is crucial for conferring optimal benefit; the steroid-associated mortality reduction was only seen in those infants who were born within 48 h of receiving steroids, and reduction in respiratory distress only in those delivering within 7 days of administration. Given that the majority of women who present with preterm contractions, do not deliver within 7 days, but may still deliver preterm, the benefit of steroids to reduce mortality and RDS would be lost by premature administration of the drug, and the woman may require repeat doses of corticosteroids if risk of sPTB remains high [20]. Furthermore, use of steroids is associated with an associated reduction in infant birthweight, particularly pronounced for infants who received steroids but delivered after 7 days of administration (placebo vs steroids; mean difference: −147.01 g; 291.97–2.05 g) [19] and those who received repeated courses of steroids (mean difference: −75.79 g; 117.63 to −33.96). With low qfFN concentrations, steroids could confidently be withheld from those with levels below 10 ng/ml.
In contrast, a higher qfFN threshold (e.g., 200 ng/ml) has a higher specificity and PPV. High qfFN supersedes most other clinical parameters [17,18], in other words, there is little value in adding clinical features to the result thus interventions such as magnesium sulfate (for fetal neuroprotection when used within 24 h before birth) or in utero transfer to an alternative hospital with more appropriate neonatal care, could be reserved for women with higher qfFN concentrations. A predictive algorithm has been developed and successfully validated in an inner London high-risk teaching hospital patient population using data from the EQUIPP study, incorporating previous risk factors, presence or absence of symptoms, gestational age at testing and CL measurement (for asymptomatic women) [17,18]. From these data, clinicians can generate an individual's risk of sPTB within 2 and 4 weeks and before 34 and 37 weeks of gestation, enabling them to tailor management accordingly. This tool is now available on the app store for iphone (QUIPP) and a version for android device is under development.
Alternative technologies
A number of other commercially available biochemical tests for prediction of preterm birth in symptomatic women are available. These are summarized in Table 3.
Table 3.
Biochemical tests to predict spontaneous preterm birth in symptomatic women: summary of predictive statistics.
| Predictive test | Threshold | Specimen collection/measurement | Prediction of sPTB <14 days from presentation (22–36 weeks') with symptoms (%) | Cautions | |||
|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | ||||
| fFN | 50 ng/ml | Vaginal swab via speculum with dipstick test, between 22 and 34 weeks' gestation | 60–87 | 76–84 | 10–35 | 82–99 | Avoid testing within 48 h after sexual intercourse or if vaginal bleeding is present |
| qfFN† | Continuous variable | As above | 35–82 | 59–98 | 10–46 | 96–98 | As above |
| phIGFBP-1 | 30 μg/l | Vaginal swab via speculum with dipstick test, between 22 and 36 weeks' gestation | 44 | 74 | 4 | 98 | Avoid testing if vaginal bleeding is present. Not thought to be affected by recent sexual intercourse |
| PAM-G‡ | 4 pg/μl | Vaginal swab inserted into vagina without speculum, between 20 and 37 weeks' gestation | 80 | 96 | 87 | 93 | Collect test prior to digital vaginal exam, use of lubricants or medications in the vagina. Not recommended if significant blood present on swab |
Varies according to concentration threshold used.
Limited evidence, needing confirmation.
Reproduced with permission from [21].
phIGFBP-1
Produced by the placental decidual cells, this protein is released into the CVF after presumed tissue damage to the interface between the chorion and decidua l interface [22]. A qualitative test (positive/negative), it is measured from a speculum obtained vaginal swab, using a commercial immunochromatography based dipstick test (Actim Partus, Medix Biochemica). A recent study confirmed a high NPV (>95%) for sPTB within 7 days and 2 weeks, supporting its use as a ‘rule out’ test, though sensitivity and positive predictive value was poor [23].
PAMG-1
PAMG-1 is a glycoprotein synthesized by the decidua, usually found in low concentrations in the CVF. Concentration is measured from a vaginal swab (obtained without speculum), and measured using an immunoassay bedside ‘dipstick test’ (PartoSure™ TTD Test, Qiagen). One small study [24] (n = 101) has demonstrated 97% NPV and 78% PPV for delivery within 7 days in symptomatic women, with similarly high predictive value for delivery within 2 weeks. While clearly requiring evaluation in a larger group of women, this has promising short-term prediction potential, although prediction of delivery greater than 14 days after testing is not clear. At present, however, there is insufficient evidence for its use compared with CL and other biochemical markers.
Cervical length measurement
CL measurement by transvaginal ultrasound scan is an established screening test for preterm birth. Traditionally performed between 14 and 24 weeks in women who are thought to be at high risk of preterm birth (by virtue of previous history or other obstetric risk factor), several studies have demonstrated that risk of preterm delivery is substantially greater in high-risk women with a CL less than 25 mm, and that this risk increases exponentially with decreasing CL [25]. Reduction of this risk has been demonstrated with early prophylactic intervention such as cerclage or progesterone therapy [4,5]. Unlike biochemical testing, CL screening requires a trained provider and expensive ultrasound equipment. A combination of CL and qfFN has been demonstrated to improve predictive accuracy, particularly in those women with a short cervix [15] and it is likely that combining CL measurement with other biochemical testing affords improved prediction.
Current status of the qfFN test
While registrations are currently ongoing, QfFN is currently approved for use for the prediction of sPTB in a number of European countries (including the UK, Austria, Germany, France, Belgium, The Netherlands, Luxemburg, Portugal, Spain and Switzerland), Australia, New Zealand and parts of the Middle East (Jordan, Kuwait, United Arab Emirates and Qatar).
Conclusion
QfFN measured in the CVF, alone or in combination with CL measurement, has been demonstrated to predict preterm birth when used as a screening test in asymptomatic high-risk women, as well as in women presenting with threatened preterm labor with a superior positive prediction compared with the traditional test, and maintaining excellent negative prediction. Women with low qfFN concentrations may be reassured that their risk of early delivery is extremely low, enabling discharge from intensive surveillance, and preventing admission to hospital, in utero transfer or unnecessary (and potentially harmful) intervention, with significant healthcare reduction costs. While the positive predictive value is improved compared with the traditional qualitative test, the false-positive result remains high, and women will still be incorrectly identified as high risk, and ‘over-treated’. However, given the benefit of interventions such as steroids and magnesium sulfate, overtreatment is inevitable to avoid missing an infant who may have benefited from intervention. For those identified earlier in their pregnancy as high risk before symptoms arise, prophylactic interventions including cerclage and progesterone have a limited evidence base and few robust clinical guidelines exist; currently women are identified as requiring intervention on the basis of history and CL measurement. It may be that qfFN is able to further triage these women according to risk, and improve identification of women who are most likely to benefit from such intervention. Furthermore, the value of serial qfFN testing to optimize timing of antenatal interventions must be explored. Further research, with appropriately designed clinical trials, is needed to evaluate how qfFN may be used to identify asymptomatic women who would benefit from prophylactic intervention, but may well in the future enable CVF qfFN to be incorporated into clinical pathways where certain thresholds can aid prophylactic management decisions.
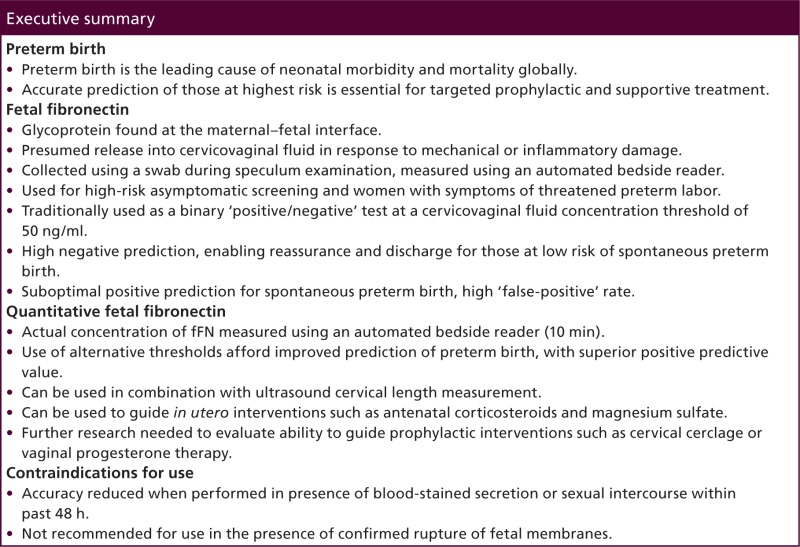
Executive summary
Preterm birth
Preterm birth is the leading cause of neonatal morbidity and mortality globally.
Accurate prediction of those at highest risk is essential for targeted prophylactic and supportive treatment.
Fetal fibronectin
Glycoprotein found at the maternal–fetal interface.
Presumed release into cervicovaginal fluid in response to mechanical or inflammatory damage.
Collected using a swab during speculum examination, measured using an automated bedside reader.
Used for high-risk asymptomatic screening and women with symptoms of threatened preterm labor.
Traditionally used as a binary ‘positive/negative’ test at a cervicovaginal fluid concentration threshold of 50 ng/ml.
High negative prediction, enabling reassurance and discharge for those at low risk of spontaneous preterm birth.
Suboptimal positive prediction for spontaneous preterm birth, high ‘false-positive’ rate.
Quantitative fetal fibronectin
Actual concentration of fFN measured using an automated bedside reader (10 min).
Use of alternative thresholds afford improved prediction of preterm birth, with superior positive predictive value.
Can be used in combination with ultrasound cervical length measurement.
Can be used to guide in utero interventions such as antenatal corticosteroids and magnesium sulfate.
Further research needed to evaluate ability to guide prophylactic interventions such as cervical cerclage or vaginal progesterone therapy.
Contraindications for use
Accuracy reduced when performed in presence of blood-stained secretion or sexual intercourse within past 48 h.
Not recommended for use in the presence of confirmed rupture of fetal membranes.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Financial & competing interests disclosure
NL Hezelgrave and AH Shennan received financial assistance providing educational talks on preterm birth from Hologic, USA, and received funding for research paid to their institution. AH Shennan is an unpaid member of the Hologic European Perinatal Advisory Board since December 2013. NL Hezelgrave is funded by a National Institute for Health Research (NIHR) Doctoral Research Fellowship (DRF-2013-06-171). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod. Health 10(Suppl. 1), S2 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.An excellent review of the most recent epidemiology of preterm birth in a global context.
- 2.Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379(9832), 2162–2172 (2012). [DOI] [PubMed] [Google Scholar]
- 3.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 371, 75–84 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet. Gynecol. 106, 181–189 (2005). [DOI] [PubMed] [Google Scholar]
- 5.Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: a systematic review and metaanalysis of individual patient data. Am. J. Obstet. Gynecol. 206, 124. e1–124.e19 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): an open-label randomised controlled trial. Lancet 379, 1800–1806. [DOI] [PubMed] [Google Scholar]
- 7.McLaren JS, Hezelgrave NL, Ayubi H, Seed PT, Shennan AH. Prediction of spontaneous preterm birth using quantitative fetal fibronectin after recent sexual intercourse. Am. J. Obstetr. Gynecol. 212, 89.e1–89.e5 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Lockwood CJ, Senyei AE, Dische MR, et al. Fetal fibronectin in cervical and vaginal secretions as a predictor of preterm delivery. N. Engl. J. Med. 325, 669–674 (1991). [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg RL, Mercer BM, Meis PJ, Copper RL, Das A, McNellis D. The Preterm Prediction Study: fetal fibronectin testing and spontaneous preterm birth. Obstet. Gynecol. 87, 643–648 (1996). [DOI] [PubMed] [Google Scholar]
- 10.Honest H, Bachmann LM, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervicovaginal fetal fibronectin test in predicting risk of spontaneous preterm birth: systematic review. BMJ 325, 301 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peaceman AM, Andrews WW, Thorp JM, et al. Fetal fibronectin as a predictor of preterm birth in patients with symptoms: a multicenter trial. Am. J. Obstetr. Gynecol. 177, 13–18 (1997). [DOI] [PubMed] [Google Scholar]
- 12.Shennan A, Jones G, Hawken J, et al. Fetal fibronectin test predicts delivery before 30 weeks of gestation in high risk women, but increases anxiety. BJOG 112, 293–298 (2005). [DOI] [PubMed] [Google Scholar]
- 13.Berghella V, Hayes E, Visintine J, Baxter JK. Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database Syst. Rev. (4), CD006843 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- ••.Cochrane review synthesising the effect of fetal fibronectin (fFN) testing on rates of spontaneous preterm birth.
- 14.Kurtzman J, Chandiramani M, Briley A, Poston L, Das A, Shennan A. Quantitative fetal fibronectin screening in asymptomatic high-risk patients and the spectrum of risk for recurrent preterm delivery. Am. J. Obstetr. Gynecol. 200, 263.e1–263.e6 (2009). [DOI] [PubMed] [Google Scholar]
- 15.Abbott DS, Hezelgrave NL, Seed PT, et al. Quantitative fetal fibronectin to predict preterm birth in asymptomatic women at high risk. Obstet. Gynecol. 125, 1168–1176 (2015). [DOI] [PubMed] [Google Scholar]
- ••.First prospective study to evaluate predictive potential of fFN using a bedside reader, for prediction of preterm birth in asymptomatic women at high risk of preterm birth between 22 and 27 weeks of gestation.
- 16.Abbott DS, Radford SK, Seed PT, Tribe RM, Shennan AH. Evaluation of a quantitative fetal fibronectin test for spontaneous preterm birth in symptomatic women. Am. J. Obstetr. Gynecol. 208, 122. e1–208. e6 (2013). [DOI] [PubMed] [Google Scholar]
- ••.First prospective study to evaluate predictive potential of fFN using a bedside reader, for prediction of preterm birth in women symptomatic of preterm labor as between 22 and 35 weeks of gestation.
- 17.Kuhrt K, Hezelgrave N, Foster C, Seed PT, Shennan AH. Development and validation of a predictive tool for spontaneous preterm birth, incorporating quantitative fetal fibronectin, in symptomatic women. Ultrasound Obstetr. Gynecol. doi:10.1002/uog.14894 (2015) (Epub ahead of print). [DOI] [PubMed]
- •.Validation of predictive algorithm incorporating quantitative fFN, prior history and gestational age to predict individual risk of preterm birth in symptomatic women.
- 18.Kuhrt K, Smout E, Hezelgrave N, Seed PT, Carter J, Shennan AH. Development and validation of a predictive tool for spontaneous preterm birth incorporating cervical length and quantitative fetal fibronectin in asymptomatic high-risk women. Ultrasound Obstetr. Gynecol. doi:10.1002/uog.14865 (2015) (Epub ahead of print). [DOI] [PubMed]
- •.Validation of predictive algorithm incorporating quantitative fFN, cervical length, prior history and gestational age to predict individual risk of preterm birth in asymptomatic women.
- 19.Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst. Rev. (3), CD004454 (2006). [DOI] [PubMed] [Google Scholar]
- 20.Crowther CA, McKinlay CJ, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst. Rev. (6), CD003935 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hezelgrave N, Shennan A, David A. Tests to predict imminent delivery in threatened preterm labour. BMJ 350, h2183 (2015). [DOI] [PubMed] [Google Scholar]
- 22.Akercan F, Kazandi M, Sendag F, et al. Value of cervical phosphorylated insulinlike growth factor binding protein-1 in the prediction of preterm labor. J. Reprod. Med. 49, 368–372 (2004). [PubMed] [Google Scholar]
- 23.Cooper S, Lange I, Wood S, Tang S, Miller L, Ross S. Diagnostic accuracy of rapid phIGFBP-I assay for predicting preterm labor in symptomatic patients. J. Perinatol. 32(6), 460–465 (2011). [DOI] [PubMed] [Google Scholar]
- 24.Nikolova T, Bayev O, Nikolova N, Di Renzo GC. Evaluation of a novel placental alpha microglobulin-1 (PAMG-1) test to predict spontaneous preterm delivery1). J. Perinat. Med. 2(4), 473–477 (2013). [DOI] [PubMed] [Google Scholar]
- 25.Guzman E, Walters C, Ananth C, et al. A comparison of sonographic cervical parameters in predicting spontaneous preterm birth in high-risk singleton gestations. Ultrasound Obstetr. Gynecol. 18, 204–210 (2001). [DOI] [PubMed] [Google Scholar]