Abstract
The incidence of breast cancer is on the rise in sub-Saharan Africa (SSA) and efforts at early diagnosis have not been very successful because the public has scant knowledge about the disease, a large percentage of breast cancer cases are diagnosed late and mainly rural SSA women's practice of breast self-examination is poor. In this paper, we argue that an examination of the social and cultural contexts of SSA that influence breast cancer diagnosis and management in the region is needed. We discuss the implications of sociocultural factors, such as gender roles and spirituality, on breast cancer diagnosis and management in SSA.
Keywords: breast cancer, culture, social, sub-Saharan Africa, women's health
Breast cancer has not been prioritized as a women's health issue in sub-Saharan Africa (SSA), even though it is the most common cancer among women in SSA [1]. The low life expectancy in the region means that women often do not live long enough to be diagnosed; researchers cite the absence of population-specific cancer registries and lack of screening equipment, and competing health needs including HIV/AIDS, tuberculosis and malaria as contributing to the limited data on breast cancer [2]. The outcome has created a situation in which we have scant research, knowledge and awareness about breast cancer in SSA [3–5].
In this paper, we argue that more research on breast cancer is needed because the incidence of the disease is expected to rise as SSA becomes urbanized, its people access more formal education and life expectancy increases [2,3]. To gain a full picture of the scope of breast cancer in SSA, research attention should focus on sociocultural aspects of the disease that have previously been overlooked. We need to research breast cancer not only from a biomedical perspective but also from a sociocultural perspective, which considers how social, cultural and economic factors impact the presentation and experience of the disease in SSA. This perspective is important given that the present education efforts do not address prevention and early detection of breast cancer in a culturally sensitive manner for the increasing at-risk population in SSA [2,3].
It is vital to consider how social, cultural and economic factors impact breast cancer diagnosis and treatment, because these factors influence cancer care in resource-limited settings such as SSA [6]. The health sector in SSA is plagued by inadequate health personnel, poor health insurance programs and limited facilities for cancer screening and treatment. In instances where cancer-screening facilities are available, they are accessible to very few people [7–9]. In most countries in SSA, treatment of cancer and other chronic conditions are not covered by national health insurance programs, requiring women to pay for the cost of breast cancer screening and treatment out of pocket [10]. Also, the costs of breast biopsies and pathologic examinations are not covered by health insurance systems in most countries in SSA leading to delayed diagnosis [11]. Added to this are social beliefs and practices including gender roles, which are often misunderstood, miscommunicated and misapplied by health workers and community members including women. This has led to negative attitudes toward and/or overvaluing of these practices thus inhibiting appropriate and timely use of health services by women [12].
These social, cultural and economic issues influence women's experience of breast cancer, public knowledge and understanding of the disease and steps taken to manage the disease [5,13–15]. For instance, economics and social beliefs about women's bodies in SSA have contributed to failure to adhere to treatment or discontinuation of treatment for breast cancer particularly among rural women [7,10,16,17]. Because sociocultural factors affect both pre- and post-treatment experiences of breast cancer, we focus on the implications of sociocultural factors for breast cancer diagnosis and management in SSA [18].
Breast cancer in SSA
Breast cancer is the most frequently diagnosed cancer and the second leading cause of cancer death among African women. It has surpassed cervical cancer, which is now the second common cancer in African women and the leading cause of cancer death [1]. The incidence rates of breast cancer vary across the regions of Africa, with the highest occurrence being among women in southern Africa [1,19]. The disease presents in younger, premenopausal women in SSA; some of the known risk factors include lower parity, irregular menstruation and environmental and socioeconomic factors [2,7,19–21]. Research shows that age at menarche can be a protective factor against the disease among African women [22,23]. The average age at which breast cancer is diagnosed in SSA women is 10 years younger than that for women in western countries; however, the mortality rate of the disease is higher in SSA because the disease is often diagnosed late (i.e., stages III or IV) and because breast cancer tends to be more aggressive in younger patients [1,3–4,10,24].
Women diagnosed with breast cancer fear death and deformation by mastectomy and chemotherapy, and some women in SSA associate breast cancer and its treatments with death [1,4,25]. For example, Clegg-Lamptey et al. found that over 60% of breast cancer patients in Ghana do not know anyone who has survived the disease [25]. This fear causes most women in SSA to live in denial of their risks of the disease and evade or delay treatment [4,5,24]. Breast cancer is treated mostly by surgery (e.g., mastectomy) in SSA due to the late presentation of the disease and because the cost of surgery is lower compared with other forms of treatment [4,16,25]. However, mastectomy is still not fully integrated into the SSA culture as evidenced in the number of women who experience divorce following the procedure [26]. In a study examining the psychological effects of mastectomy on married women in Nigeria, Odigie et al. reported that about 70% of their study population felt a loss of their femininity as a result of mastectomy; the women had difficulties breastfeeding, felt less desired by their spouses and felt their body image was altered negatively by mastectomy [26]. In the same study, about 38% of the women reported being divorced or separated from their husbands 3 years after having a mastectomy. Thus, relational and image fears coupled with fear of death contribute to the late presentation of the disease in the region suggesting that attention needs to be given to these factors for improved diagnosis and management of the disease. It is important to note that the effect of mastectomy on the identity of women is nearly universal as studies from other parts of the world reported findings similar to those in SSA [27–31]. However, in the SSA context, these problems with mastectomy lead to delayed presentation of the disease.
Breast cancer education & awareness in SSA
Efforts to promote breast cancer education and awareness in SSA are mostly in the forms of public awareness campaigns, speeches and marches aimed at encouraging early diagnosis [10,32]. The mass media are the most common source of breast cancer information for the public and help to generate and sustain public interest in the disease [5,17,32]. Breast cancer education and awareness programs aim to teach women about the symptoms of the disease and how to conduct breast self-examinations. Breast self-examination is emphasized because it is cost-effective, can be done in private and because mammography is believed to be less efficacious in younger populations such as those in SSA [8,33]. However, as much as regular breast self-examination is encouraged among women in SSA because of the reasons noted above, SSA women also must be encouraged and empowered to seek early healthcare for any abnormalities discovered in the breasts, as that is how accurate diagnosis can be made.
Efforts at encouraging breast self-examinations have been somewhat effective at increasing knowledge about the disease. Research demonstrates that younger SSA women are aware of the importance of breast self-examination for the early detection of breast cancer, but this knowledge often does not translate into accurate practice of the procedure [33–37]. For instance, Tieng'o et al. found that women in Botswana had a positive attitude toward breast cancer examination, but their knowledge and practice of the procedure were poor [38]. Sambanje and Mafuvadze also found a lack of knowledge about breast cancer among university students in Angola, though the students agreed that monthly breast self-examinations could help detect breast lumps early [33]. Other studies however suggest that breast cancer education programs in SSA do increase knowledge, attitude and practice of early breast cancer detection strategies. Researchers in Ghana found that over 80% of participants in a breast cancer education program had accurate knowledge about breast cancer compared with about 50% of those who did not participate in the program; participants in the program were also more likely to practice breast self-examinations compared with those who did not participate [39].
Mixed research findings such as the above and the continual late presentation of the disease have raised concerns about the effectiveness of breast cancer awareness and education efforts in SSA [10,16]. Women in SSA wait for an average of 11 months after the onset of symptoms of breast cancer before they report to hospitals [7]. Interestingly, the literacy levels of women have no bearing on their attitudes and knowledge about breast cancer [10,16,21]. Delays in presentation of breast cancer result from patient delay or provider/system delay [40]. Provider/system delays are caused by factors including lack of access to breast cancer specialists and treatment facilities and inability of healthcare professionals to accurately diagnose and refer patients to oncologists [41]. A study conducted in Cameroon showed that patients had to consult with an average of four healthcare professional before diagnoses of breast cancer, Kaposi sarcoma and lymphoma were finally made and patients were not referred to oncologists in a timely manner [41]. In another study in Nigeria, researchers found that over 50% of breast cancer patients in the study population experienced provider delays including delayed or nonreferrals, false reassurances from health practitioners and failure by physicians to get biopsy or histology reports when the patients were initially evaluated [42].
Researchers and practitioners urge focusing on the reasons why women discontinue treatment, education and awareness efforts to address women's fears and misconceptions and the stigma associated with the disease [16,43,44]. Breast cancer awareness campaigns in resource-limited settings, such as SSA, should focus on dispelling myths about the disease (e.g., that breast cancer is a death sentence, that it is caused by witchcraft and that mastectomy kills) and promoting knowledge that the disease is curable if detected early. One idea for breast cancer awareness and education efforts is to use survivors and patients' experiences to emphasize that the disease can be survived [43,45]. This is particularly useful in the SSA context where the disease is shrouded in secrecy such that women do not know other patients or survivors [25]. When the general population and women, in particular, can identify others who have survived the disease, it may lessen their fears and encourage them to seek and adhere to treatment [45]. Also, women should be informed about and involved in decisions regarding surgical treatments for breast cancer to ensure satisfaction and acceptance of treatment outcomes [46]. Failure to do so can negatively affect women's psychological health, as shown in a study conducted in Ghana where breast cancer patients reported receiving inadequate information about their diagnoses and treatments, consequently leading to unpleasant treatment experiences [25], and another study in Nigeria where over 40% of depressive disorders were recorded in breast cancer patients [47].
Another idea for breast cancer awareness campaigns is to involve trusted community members in the efforts to help engender trust and further break down barriers relating to language and sociocultural beliefs. For instance, Abuidris et al. found improvement in early detection of breast lumps when local volunteers were involved in breast screening programs in Sudan [48]. Women could relate better with volunteers because they share the same beliefs and value systems and speak the same language. Similarly, community health workers can play instrumental roles in helping women access timely breast cancer care. As trusted members of communities, community health workers can be trained to perform clinical breast examinations and help women navigate complex healthcare systems when diagnoses and referrals are made; thus, helping women develop trust in healthcare systems. This can lead to early diagnosis and improved outcomes of the disease; it can also lead to patient adherence to breast cancer treatment recommendations [49].
Recognizing the unique challenges of promoting cancer care in resource-constrained environments such as SSA and the recognition that guidelines and programs which are effective in high-resource countries may not work in resource-poor settings, the Breast Health Global Initiative (BHGI) identified some guidelines for breast care at its first Global Summit in 2002 to cater for the specific needs of regions of the world such as SSA. Subsequent Global Summits held in 2005 and 2007, for instance, focused on healthcare systems and how to implement the BHGI guidelines as they pertain to management of breast cancer in resource-constrained settings [50,51]. The BHGI is co-sponsored by the Fred Hutchinson Cancer Research Center and the Susan G Komen Breast Cancer Foundation [6]. The unique element about the BHGI guidelines is that they challenge researchers and stakeholders working to address breast cancer in resource-limited settings not to merely adopt research findings but also to examine the values laden in these findings to address prevailing socioeconomic factors, gender inequality and affordable health services in a particular location [6]. We consider the call relevant to the SSA context and the argument that sociocultural factors matter in breast cancer diagnosis and management in SSA.
Even though there are debates about how breast cancer awareness should be promoted, there is no doubt about the benefits of awareness [45,52]. Increased awareness about breast cancer in SSA can help reduce the cancer burden by encouraging screening, which can lead to early detection and avoidance of practices and behaviors that increase the risk of the disease [53]. In sum, while education and awareness are crucial to early diagnosis and improved management of breast cancer in SSA, it is important to recognize that the potential barriers include social, cultural and economic factors. We now turn our attention to these factors.
Social & cultural factors & breast cancer in SSA
Cultural beliefs about the cause of breast diseases and associations of the female breasts with nurturance, motherhood and femininity influence diagnosis and management of breast cancer in SSA. As noted earlier, social and cultural factors influence women's experiences of breast cancer, social constructions of the disease and allocations of resources to manage the disease [5,13–15]. In traditional African society, good health is understood as a desirable relationship between the living and the dead and harmony between individuals and their environments. Thus, disease is conceptualized as involving malfunctioning of the body organs and lack of harmony with supernatural/ancestral forces [54]. This understanding influences how diseases are diagnosed and treated, steps taken to manage the disease and ultimately how the disease is experienced.
In SSA breast cancer is associated with supernatural forces, hence the preference to seek alternative treatments such as healing/prayer camps for breast diseases. Most women in SSA use traditional medicine and/or alternative treatments first and only report to hospitals when their breast cancer symptoms have worsened [5,17,25]. Associating breast cancer with supernatural and ancestral causes produces guilt and lack of control over the disease for most SSA women [13]. Women feel guilty that they have wronged their ancestors, and therefore believe they are being punished with breast cancer because of the belief that the living cannot contend with the dead. Ancestors are believed to have powers to protect, heal and kill; thus, a good relationship with the ancestors is linked to good health [54]. Not all Africans hold this traditional belief in ancestral spirits, however, in most instances, health and illness are believed to be in the hands of a higher power – be it God, Allah or ancestral spirits. Hence, it is common practice in most African communities to combine traditional and western/modern medicine for treatments of ailments [54]. Because these belief systems and practices impact breast cancer management in SSA, we suggest that they must be addressed in breast cancer awareness and education programs.
Some scholars suggest that seeking alternative treatment for breast cancer indicates a preference for traditional medicine instead of western/modern medicine in SSA [15,21]. In contrast to western medicine, traditional medicine is considered affordable, readily accessible, trustworthy and holistic because it involves the body, soul and spirit [43,54]. Traditional healers are trusted because women believe they look for both scientific and metaphysical causes and treatment/cures for diseases including cancers [15,54,55]. For instance, Mdondolo et al. found that women in Xhosa, South Africa, preferred using traditional medicine to treat breast diseases, because it is less painful, does not involve incisions and can be completed quickly compared with western medicine [5]. Similarly, Wright found that black breast cancer patients in South Africa discontinued biomedical treatment for the disease to seek traditional treatment due to trust in traditional medicine as more appropriate and less harmful [15]. The women also felt their privacy was secured when using traditional treatment for breast cancer as opposed to western medicine where the cancer ward is open and accessible to the public [15]. This is important in the SSA context where breast cancer is still stigmatized, and women prefer privacy.
Another sociocultural factor that impacts the diagnosis and management of breast cancer in SSA is the traditional African notion of the ‘whole’ and beautiful body. Perceptions of attractiveness and the ideal body type differ from culture to culture, reflecting particular social and cultural values [56]. To be considered beautiful, Africans believe that a woman should have all parts of her body intact especially those body features that define her femininity including the breasts. Ironically, mastectomy considered a ‘mutilation’ of a woman's body is the most common form of treatment for breast cancer in SSA [15,16]. Thus, this treatment for breast cancer clashes with popular views about the beautiful body, offering some insights into why women are afraid of the procedure. In South Africa, for instance, there is an expectation for women who have had a mastectomy to undergo breast reconstruction surgery because a mastectomy violates cultural notions about the ‘whole’ body. This belief is so prevalent that some men reportedly prevent their wives from having mastectomies or seeking treatment for breast diseases if they cannot afford the cost of breast reconstruction surgeries [57]. Some women, however, prefer not to have breast reconstruction surgeries after their mastectomies and use breast prostheses instead [58]. This indicates women's awareness of cultural expectations of how their bodies are supposed to look and how they need to present these postmastectomy bodies to society; women are doubly plagued with concern for their health and the presentation of their bodies after a breast cancer diagnosis. It is, therefore, not surprising that women in SSA continue to deny their risks of breast cancer – a situation that thwarts efforts aimed at early diagnosis.
Closely linked to the discussion above is the value attached to the breasts as symbols of nurturance and motherhood, which makes losing a breast to cancer devastating for most women in SSA. The idea of losing one's femininity to breast cancer produces fear and shame and explains why most women hide discovering lumps in their breasts [5]. In addition, cultural notions of who has access to the female body impacts women's comfort level and inhibits their seeking prompt medical care for breast cancer. For example, Mdondolo et al. discovered that women in the Xhosa community in South Africa find it embarrassing to have male doctors examine their breasts, hence their reluctance to seek medical care for breast lumps [5]. In another study about Ghanaian women's attitude toward cervical cancer screening, Williams noted that women failed to get screened for the disease due to shyness about exposing their private parts to male doctors [59]. Abuidris et al. also found that rural Sudanese women were hesitant to seek clinical screening for breast cancer, because their Islamic faith requires women to cover up their bodies [48]. Also in parts of Northern Ghana cultural taboos about touching parts of one's body including the breasts were seen as a factor discouraging women from carrying out breast self-examinations [43].
This situation is further compounded by the prohibition of open expression of pain and suffering in most communities in SSA. In the African context, pain is considered a natural consequence of diseases and injury thus, it is often not given special consideration. Men, in particular, are not expected to openly express pain and emotion as that amounts to weakness; women are also expected to be stoic and resilient during childbirth [60,61]. These beliefs about pain can influence pain management and assessment practices [62,63]. This means that the standard for illness is often set high for women in SSA in line with the heavy workload they perform including childbearing, housework, and work outside the home. Thus, most women in SSA tend to seek medical treatment late because the ‘threshold of illness recognized by the society on the illness-health continuum is so high for women that they endure so much in order not to disrupt household organization’ [64]. Wright found that women in South Africa preferred to hide their breast cancer in order to avoid stigmatization and being labeled as sick and unable to work and care for their families; the social and economic cost of being a breast cancer patient is simply too great [15]. Also, in rural Sudan, women do not want to visit hospitals for breast cancer treatment, because they do not want to disrupt the community life. Members in communities put aside work to accompany a sick community member to the hospital; thus, in order not to inconvenience the entire community, women prefer to stay home when they are sick instead of visiting the hospital [48].
These sociocultural beliefs and practices have spurred denial of risk of breast cancer, fear of mastectomy and chemotherapy, failure to adhere to treatment, among other attitudes that inhibit early diagnosis and management of the disease in SSA [5,10]. As important as these sociocultural factors are in the management of breast cancer in SSA, there is limited research addressing these issues [5]. We need to capture the attention of the biomedical and social scientific research community to help in awareness, education and intervention efforts.
It is important to note that there may be differences in how these sociocultural factors and practices impact attitudes toward breast cancer in rural and urban areas in SSA. This is because the disease is believed to be more common in urban communities than in rural areas due to adoption of western lifestyles by people in the urban centers [1,65]; although some scholars have explained that this difference could be due to misreporting of places of residence by women [19]. Also, there are differences in knowledge about breast cancer between urban and rural SSA women. For instance, Muthoni and Miller [66] found differences in knowledge, attitude, and practice of early breast cancer detection practices between urban and rural women in Kenya. Additionally, Pillay [67] observed in a study that rural women in South Africa were less knowledgeable about cancers of the breast and cervix and were more likely to use traditional healers to treat breast diseases than urban women.
Implications for breast cancer diagnosis & management
The sociocultural issues we discussed have implications for how breast cancer is diagnosed and managed in SSA. First, these issues demand that discourse around breast cancer needs to be modified to reflect the holistic experience of women. Breast cancer should be explained not only as a dysfunction of cells in the body, but also as a disease that affects the totality of women's lives including their self-esteem and relationships. When the functions and/or dysfunctions of cells of the body are projected as the main elements at stake in breast cancer, it reduces treatment efforts to addressing the physical presentation of the disease and to seeing the self as autonomous and able to fight off the disease alone [68]. However, this limited perspective of the self, disease and health is foreign to most communities in SSA. In fact, cancer is a foreign term in most parts of SSA; there is no word in some languages for the disease [43,48]. Understanding cancer as a cultural phenomenon helps make it clear that explanation of the disease including its causes and cures needs to be culturally appropriate [68]. Women's lived experiences of the disease should not be overlooked in an attempt to package breast cancer for public consumption and to encourage research funding; breast cancer advocates and researchers in SSA must be careful to address the core issues affecting its actual experience [69]. Thus, the scientific discourse around breast cancer in SSA has to incorporate traditional African understanding of the concepts of health, diseases and the self and acknowledge challenges women with the disease face.
Second, culturally sensitive and appropriate breast cancer education and awareness efforts should be stepped up and targeted at everyone including women, community and religious leaders, family members, men and health workers. As explained, decisions regarding treatment options and choices for breast cancer in SSA are a collective process involving several members in the woman's social network [15,48]. We should not assume that these community members do not matter in issues related to breast cancer because they do not bear the physical marks of the disease on their bodies; their opinions influence the lives of women affected by breast cancer [43,45,48]. In particular, husbands should be encouraged to be involved in the management of their wives' breast cancer from the prediagnosis stages to the postdiagnosis treatment decisions. Making husbands a part of their wives' breast cancer experience can help them to be more understanding and appreciative of the daily struggles of the breast cancer experience. Targeting these community members in breast cancer education programs can go a long way in improving how the disease is theorized and perceived in SSA; it can also significantly improve metaphors used to discuss the disease and the effects of these on the experience and management of the disease. Metaphors such as fear, death, deformity and witchcraft associated with breast cancer in SSA impact understanding of the disease and whether or not women seek medical treatment [70]. It can also lead to designing intervention programs that address both systemic and cultural issues. Thus, sensitizing entire communities about breast cancer can improve early diagnosis and management of the disease.
Third, basic cancer education should be incorporated into health worker training programs in SSA as a way of encouraging a more positive attitude toward the disease by health workers [10]. Health workers are expected to know more about disease conditions such as breast cancer in order to educate lay people; they are also one of the trusted sources of health information in SSA. But what happens when these health workers lack knowledge about the issues they are to educate the public about? The result is misinformation, miscommunication and evidently misconceptions [12]. Thus, when health workers are trained to understand breast cancer as it is–a disease–it can enhance their attitude toward the disease and help transmit that to those affected. This can produce a ripple effect where the positivity of health workers can encourage communities to view the disease in a positive light and understand that attitudes toward the disease can affect the time of diagnosis and the prognosis.
Advanced breast cancer is harder and more difficult to manage and often has poor prognosis [21,71]; hence the aim should be early diagnosis. Early diagnosis can be cost-effective and can potentially save lives. However, patients need to be encouraged, through public education, to be engaged in the diagnosis and treatment/management process [6]. Accurate diagnosis of breast cancer is an important step in the management of the disease. When the disease is accurately diagnosed, it will lead to prompt and accurate treatment programs and certainty about the prognosis which will direct the course of counseling for patients, where necessary, to allay their fears [7]. However, accurate breast cancer screening and treatment equipment is lacking in most countries in SSA. Therefore, there is a need to improvise and use available tools and resources to diagnose and treat the disease even though some of these may not be of the highest quality [52]. For instance, in the absence of mammography, ultrasound equipment can be used in detecting breast masses. In resource-limited settings including SSA, ultrasound instead of mammographic equipment can be used to screen for breast lumps because the equipment is less expensive, readily available, is more efficacious in younger, premenopausal women and can be used for other purposes other than breast imaging [6,8]. Early diagnosis will be effective when the screening tools are good and when an entire population has coverage for screening and adhere to treatment recommendations [45].
Conclusion
Breast cancer management is multidimensional in that prognosis of the disease depends on a chain of related factors including the time of diagnosis, available treatment options, attitude toward to disease and sociocultural factors [7,21]. Thus, efforts at improving diagnosis and management of the disease also need to use a multidisciplinary approach giving equal attention to biomedical as well as sociocultural factors. The inter-relatedness of scientific knowledge, cultural, social and economic factors in the diagnosis and management of breast cancer in SSA needs to be acknowledged. As the scientific research community and other stakeholders strive to improve diagnosis and management of the disease, we suggest a need to focus on the role of social and cultural factors, especially in the SSA context. This is because the manner in which breast cancer is diagnosed, managed and experienced, to some extent, can be explained in sociocultural terms [13].
Some of these sociocultural factors can be addressed through increased education whereas others require a tailored approach to breast cancer diagnosis and management taking into consideration religion, culture and other social factors [45]. Incorporating cultural norms, beliefs and values into breast cancer intervention programs has been recommended for culturally heterogeneous populations including Latinas [18] thus, it has potential for success in the SSA context as well. Breast cancer often presents late in SSA because of factors including cultural beliefs about the origin of breast diseases, cultural expectations of women that they manage not only the breast cancer, its treatments and side effects, but also that they hide or modify their postmastectomy bodies in order to be accepted by society [72]. We suggest that these issues warrant attention in our efforts to identify ways to better manage the disease in the SSA region.
Future perspective
The social and cultural contexts of SSA influence breast cancer diagnosis and management. It is important that consideration is given to not only how these issues affect women's lives post-treatment but also how these may be inhibiting efforts at improving diagnosis and management of the disease. We suggest that these sociocultural factors be incorporated into breast cancer awareness, education and intervention initiatives in SSA. This will encourage women to report breast cancer symptoms earlier, making the aim of early diagnosis and treatment feasible.
Executive summary
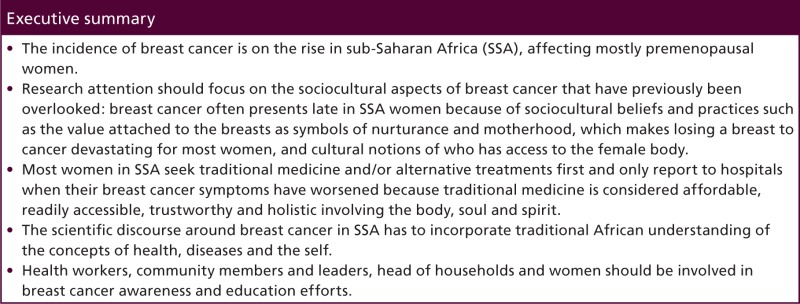
The incidence of breast cancer is on the rise in sub-Saharan Africa (SSA), affecting mostly premenopausal women.
Research attention should focus on the sociocultural aspects of breast cancer that have previously been overlooked: breast cancer often presents late in SSA women because of sociocultural beliefs and practices such as the value attached to the breasts as symbols of nurturance and motherhood, which makes losing a breast to cancer devastating for most women, and cultural notions of who has access to the female body.
Most women in SSA seek traditional medicine and/or alternative treatments first and only report to hospitals when their breast cancer symptoms have worsened because traditional medicine is considered affordable, readily accessible, trustworthy and holistic involving the body, soul and spirit.
The scientific discourse around breast cancer in SSA has to incorporate traditional African understanding of the concepts of health, diseases and the self.
Health workers, community members and leaders, head of households and women should be involved in breast cancer awareness and education efforts.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Jemal A, Bray F, Forman D, O'Brien M, et al. Cancer burden in Africa and opportunities for prevention. Cancer 118(18), 4372–4384 (2012). [DOI] [PubMed] [Google Scholar]
- ••.Reviews current patterns of the common cancers in Africa and discusses how the cancer burden can be reduced.
- 2.Adebamowo CA, Adekunle OO. Case-controlled study of the epidemiological risk factors for breast cancer in Nigeria. Br. J. Surg. 86, 665–668 (1999). [DOI] [PubMed] [Google Scholar]
- 3.Akarolo-Anthony SN, Ogundiran TO, Adebamowo CA. Emerging breast cancer epidemic: evidence from Africa. Breast Cancer Res. 12(Suppl. 4), S8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- ••.Discusses breast cancer as an emerging epidemic in Africa.
- 4.Fregene A, Newman LA. Breast cancer in sub-Saharan Africa: how does it relate to breast cancer in African-American women? Cancer 103, 1540–1560 (2005). [DOI] [PubMed] [Google Scholar]
- 5.Mdondolo N, de Villiers L, Ehlers VJ. Cultural factors associated with management of breast lumps amongst Xhosa women: research. Health SA, Gesondheid 8(3), 86–97 (2004). [Google Scholar]
- •.Discusses cultural factors influencing health seeking behaviors of Xhosa breast cancer patients.
- 6.Anderson BO, Shyyan R, Eniu A, et al. Breast cancer in limited-resource countries: an overview of the breast health global initiative 2005 guidelines. Breast J. 12 (Suppl. 1), S3–S15 (2006). [DOI] [PubMed] [Google Scholar]
- ••.Discusses the Breast Health Global Initiative guidelines as a framework for using cost-effective strategies to manage breast cancer in resource-limited settings.
- 7.Adesunkanmi ARK, Lawal OO, Adelusola KA, et al. The severity, outcome and challenge of breast cancer in Nigeria. Breast 15, 399–409 (2006). [DOI] [PubMed] [Google Scholar]
- 8.Galukande M, Kiguli-Malwadde E. Rethinking breast cancer screening strategies in resource-limited settings. Afr. Health Sci. 10, 89–92 (2010). [PMC free article] [PubMed] [Google Scholar]
- 9.Gondos A, Brenner H, Wabinga H, et al. Cancer survival in Kampala, Uganda. Br. J. Cancer 92, 1808–1812 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anyanwu SNC, Egwuonwu OA, Ihekwoaba EC. Acceptance and adherence to treatment among breast cancer patients in Eastern Nigeria. Breast 20, S51–S53 (2011). [DOI] [PubMed] [Google Scholar]
- •.Discusses sociocultural barriers to adherence of breast cancer treatment in Nigeria.
- 11.Abdel-Fattah MM, Anwar MA, Mari E, et al. Patient-and system-related diagnostic delay in breast cancer. Eur. J. Publ. Health 9(1), 15–19 (1999). [Google Scholar]
- 12.Aubel J, Rabei H, Mukhtar M. Health workers' attitude can create communication barriers. World Health Forum 12, 466–471 (1991). [PubMed] [Google Scholar]
- 13.Schlebusch L, Van Oers H. Psychological stress adjustment and cross-cultural considerations in breast cancer patients. S. Afr. J. Psy. 29, 30–35 (1999). [Google Scholar]
- 14.Thorne SE, Murray C. Social constructions of breast cancer. Health Care Women Int. 21, 141–159 (2000). [DOI] [PubMed] [Google Scholar]
- 15.Wright SV. An investigation into the causes of absconding among black African breast cancer patients. S. Afr. Med. J. 87, 1540–1543 (1997). [PubMed] [Google Scholar]
- 16.Clegg-Lamptey JNA, Hodasi WM. A study of breast cancer in Korle Bu Teaching Hospital: assessing the impact of health education. Gh. Med. J. 14(2), 72–77 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Assesses the impact of health education on breast cancer awareness in Ghana.
- 17.Opoku SY, Benwell M, Yarney J. Knowledge, attitudes, beliefs, behaviour and breast cancer screening practices in Ghana, West Africa. Pan Afr. Med. J. 11, 28 (2012). [PMC free article] [PubMed] [Google Scholar]
- 18.Molina Y, Thompson B, Espinoza N, Ceballos R. Breast cancer interventions serving US-based Latinas: current approaches and directions. Women's Health 9(4), 335–350 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinton LA, Figueroa JD, Awuah B, et al. Breast cancer in sub-Saharan Africa: opportunities for prevention. Br. Cancer Res. Treat. 144(3), 467–478 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adebamowo CA, Ogundiran TO, Adenipekun AA, et al. Obesity and height in urban Nigerian women with breast cancer. Ann. Epidemiol. 13(6), 455–461 (2003). [DOI] [PubMed] [Google Scholar]
- 21.Tesfamariam A, Gebremichael A, Mufunda J. Breast cancer clinicopathological presentation, gravity and challenges in Eritrea, East Africa: management practice in a resource-poor setting. S. Afr. Med. J. 103(8), 526–528 (2013). [DOI] [PubMed] [Google Scholar]
- 22.Sighoko D, Kamaté B, Traore C, et al. Breast cancer in premenopausal women in West Africa: analysis of temporal trends and evaluation of risk factors associated with reproductive life. Breast 22, 828–835 (2013). [DOI] [PubMed] [Google Scholar]
- 23.Huo D, Adebamow CA, Ogundiran TO, et al. Parity and breastfeeding are protective against breast cancer in Nigerian women. Br. J. Cancer 98, 992–996 (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ajekigbe AT. Fear of mastectomy: the most common factor responsible for late presentation of carcinoma of the breast in Nigeria. Clin. Oncol. 3, 78–80 (1991). [DOI] [PubMed] [Google Scholar]
- 25.Clegg-Lamptey JNA, Dakubo JCB, Attobra YN. Psychosocial aspects of breast cancer treatment in Accra, Ghana. East Afr. Med. J. 86(7), 348–353 (2009). [DOI] [PubMed] [Google Scholar]
- 26.Odigie VI, Tanaka R, Yusufu LMD, et al. Psychosocial effects of mastectomy on married African women in northwestern Nigeria. Psychooncology 19, 893–897 (2010). [DOI] [PubMed] [Google Scholar]
- •.A study about the effects of mastectomy on women in Nigeria.
- 27.Arroyo JMG, López MLD. Psychological problems derived from mastectomy: a qualitative study. Int. J. Surg. Oncol. 2011, 132461 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fallbjörk U, Rasmussen BH, Karlsson S, Salander P. Aspects of body image after mastectomy due to breast cancer: a two-year follow-up study. Eur. J. Oncol. Nurs. 17, 340–345 (2013). [DOI] [PubMed] [Google Scholar]
- 29.Karabulut N, Erci B. Sexual desire and satisfaction in sexual life affecting factors in breast cancer survivors after mastectomy. J. Psychosoc. Oncol. 27(3), 332–343 (2009). [DOI] [PubMed] [Google Scholar]
- 30.Piot-Ziegler C, Sassi ML, Raffoul W, Delaloye JF. Mastectomy, body deconstruction, and impact on identity: a qualitative study. Br. J. Health Psychol. 15(3), 479–510 (2010). [DOI] [PubMed] [Google Scholar]
- 31.Shrestha K. Psychological impact after mastectomy among Nepalese women: a qualitative study. Nepal Med. Coll. J. 14(2), 153–156 (2012). [PubMed] [Google Scholar]
- 32.Reichenbach L. The politics of priority setting for reproductive health: breast and cervical cancer in Ghana. Reprod. Health Matters 10(20), 47–58 (2002). [DOI] [PubMed] [Google Scholar]
- 33.Sambanje MN, Mafuvadze B. Breast cancer knowledge and awareness among university students in Angola. Pan Afr. Med. J. 11, 70 (2012). [PMC free article] [PubMed] [Google Scholar]
- 34.Obaikol R, Galukande M, Fualal J. Knowledge and practice of breast self-examination among female students in a sub Saharan African university. East Central Afr. J. Surg. 15(1), 22–27 (2010). [Google Scholar]
- 35.Suh MAB, Atashili J, Fuh EA, Eta VA. Breast self-examination and breast cancer awareness in women in developing countries: a survey of women in Buea, Cameroon. BMC Res. Notes 5(1), 627 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Azubuike SO, Okwuokei SO. Knowledge, attitude and practices of women towards breast cancer in Benin City, Nigeria. Ann. Med. Health Sci. Res. 3(2), 155–160 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ameer K, Abdulie SM, Pal SK, Arebo K, Kassa GG. Breast cancer awareness and practice of breast self-examination among female medical students in Haramaya University, Harar, Ethiopia. Int. J. Interdiscipl. Multidiscipl. Studies 2(2), 109–119 (2014). [Google Scholar]
- 38.Tieng'o JG, Pengpid S, Skaal L, Peltzer K. Knowledge attitude and practice of breast cancer examination among women attending a health facility in Gaborone, Botswana. Gender Behav. 9(1), 3513–3527 (2001). [Google Scholar]
- 39.Mena M, Wiafe-Addai B, Sauvaget C, et al. Evaluation of the impact of a breast cancer awareness program in rural Ghana: a cross-sectional survey. Int. J. Cancer 134, 913–924 (2014). [DOI] [PubMed] [Google Scholar]
- 40.Sharma K, Costas A, Shulman LN, Meara JG. A systematic review of barriers to breast cancer care in developing countries resulting in delayed patient presentation. J. Oncol. 2012, 121873 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Price AJ, Ndom P, Atenguena E, Nouemssi JPM, Ryder RW. Cancer care challenges in developing countries. Cancer 118(14), 3627–3635 (2011). [DOI] [PubMed] [Google Scholar]
- 42.Ezeome ER. Delays in presentation and treatment of breast cancer in Enugu, Nigeria. Nig. J. Clin, Practice 13(3), 311–316 (2010). [PubMed] [Google Scholar]
- 43.Asobayire A, Barley R. Women's cultural perceptions and attitudes towards breast cancer: Northern Ghana. Health Promotion Int. 30(3), 647–657 (2014). [DOI] [PubMed] [Google Scholar]
- ••.Offers insights into some of the social and cultural factors that influence attitude toward breast cancer in northern Ghana.
- 44.Shulman LN, Willett W, Sievers A, Knaul FM. Breast cancer in developing countries: opportunities for improved survival. J. Oncol. 2010, 595167 (2010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith RA, Caleffi M, Albert U, et al. Breast cancer in limited-resource countries: early detection and access to care. Breast J. 12(Suppl. 1), S16–S26 (2006). [DOI] [PubMed] [Google Scholar]
- 46.Hawley ST. Involving patients in the decision-making process regarding breast cancer treatment: implications for surgery utilization. Women's Health 6(2), 161–164 (2010). [DOI] [PubMed] [Google Scholar]
- 47.Popoola AO, Adewuya AO. Prevalence and correlates of depressive disorders in outpatients with breast cancer in Lagos, Nigeria. Psychooncology 21, 675–679 (2012). [DOI] [PubMed] [Google Scholar]
- 48.Abuidris DO, Elsheikh A, Ali M, et al. Breast-cancer screening with trained volunteers in a rural area of Sudan: a pilot study. Lancet Oncol. 14, 363–370 (2013). [DOI] [PubMed] [Google Scholar]
- 49.Wadler BM, Judge CM, Prout M, Allen JD, Geller AC. Improving breast cancer control via the use of community health workers in South Africa: a critical review. J. Oncol. 2011, pii: 150423 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anderson BO, Yip C, Ramsey SD, et al. Breast cancer in limited-resource countries: health care systems and public policy. Breast J. 12(Suppl. 1), S54–S69 (2006). [DOI] [PubMed] [Google Scholar]
- 51.Anderson BO, Yip C, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the Breast Health Global Initiative Global Summit 2007. Cancer 113 (S8), 2221–2243 (2008). [DOI] [PubMed] [Google Scholar]
- 52.Anderson BO. Breast cancer in sub-Saharan Africa: where can we go from here? J. Surg. Oncol. 110(8), 901–902 (2014). [DOI] [PubMed] [Google Scholar]
- 53.Morhason-Bello IO, Odedina F, Rebbeck TR, et al. Challenges and opportunities in cancer control in Africa: a perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol. 14, e142–e151 (2013). [DOI] [PubMed] [Google Scholar]
- 54.Omonzejele PF. African concepts of health, disease, and treatment: an ethical enquiry. Explore 4(2), 120–125 (2008). [DOI] [PubMed] [Google Scholar]
- 55.Akpomuvie OB. The perception of illness in traditional Africa and the development of traditional medical practice. Int. J. Nurs. 1(1), 51–59 (2014). [Google Scholar]
- 56.Reischer E, Koo KS. The body beautiful: symbolism and agency in the social world. Annu. Rev. Anthropol. 33, 297–317 (2004). [Google Scholar]
- 57.Cooper SE, Mullin VC. Quality of life of cancer patients in underserved populations in South Africa. J. Psychosoc. Oncol 19(2), 39–56 (2001). [Google Scholar]
- 58.Van der Wiel R. “I am happy with one”: re-evaluating the relationship between gender, breast cancer surgery, and survival. Agenda 27(4), 55–64 (2013). [Google Scholar]
- 59.Williams MS. A qualitative assessment of the social cultural factors that influence cervical cancer screening behaviors and the health communication preferences of women in Kumasi, Ghana. J. Cancer Edu. 29, 555–562 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nortjé N, Albertyn R. The cultural language of pain: a South African study. S. Afr. Family Practice 57(1), 24–27 (2015). [Google Scholar]
- 61.The Prevention of Maternal Mortality Network. Barriers to treatment of obstetric emergencies in rural communities of West Africa. Stud. Fam. Plan. 23(5), 279–291 (1992). [PubMed] [Google Scholar]
- 62.Albertyn R, Rode H, Millar AJW, Thomas J. Challenges associated with pediatric pain management in sub Saharan Africa. Int. J. Surg. 7, 91–93 (2009) [DOI] [PubMed] [Google Scholar]
- 63.Rampanjato RM, Florence M, Patrick NC, Finucane BT. Factors influencing pain management by nurses in emergency departments in Central Africa. Emergency Med. J. 24, 475–476 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Okejie CEE. Gender inequalities of health in the third world. Soc. Sci. Med. 39(9), 1237–1247 (1994). [DOI] [PubMed] [Google Scholar]
- 65.Parkin DM, Sitas F, Chirenje M, Stein L, Abratt R, Wabinga H. Part I: cancer in indigenous Africans: burden, distribution, and trends. Lancet Oncol. 9(7), 683–692 (2008). [DOI] [PubMed] [Google Scholar]
- 66.Muthoni A, Miller AN. An exploration of rural and urban Kenyan women's knowledge and attitudes regarding breast cancer and breast cancer early detection measures. Health Care Women Int. 31, 801–816 (2010). [DOI] [PubMed] [Google Scholar]
- 67.Pillay AL. Rural and urban South African women's awareness of cancers of the breast and cervix. Ethnicity Health 7(2), 103–114 (2002). [DOI] [PubMed] [Google Scholar]
- 68.Stacey J. Teratologies: A Cultural Study Of Cancer. Routledge, New York, NY, USA: (1997). [Google Scholar]
- 69.Sulik G. Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. Oxford University Press, New York, NY, USA: (2011). [Google Scholar]
- 70.Sontag S. Illness As Metaphor And AIDS And Its Metaphors. Picador, New York, NY, USA: (1997). [Google Scholar]
- 71.Basro S, Apffelstaedt JP. Breast cancer in young women in a limited-resource environment. World J. Surg. 34(7), 1427–1433 (2010). [DOI] [PubMed] [Google Scholar]
- 72.Lorde A. The Cancer Journals (Special Edition). Aunt Lute Books, San Francisco, CA, USA: (1997). [Google Scholar]