Abstract
Importance
Research indicates that e-cigarette use (vaping) among adolescents is associated with the initiation and progression of combustible cigarette smoking, yet the reasons for this association are unknown.
Objective
To evaluate whether use of e-cigarettes with higher nicotine concentrations is associated with subsequent increases in the frequency and intensity of combustible cigarette smoking and vaping.
Design/Setting/Participants
Prospective school-based cohort; surveys were administered in Spring (baseline, 10th grade) and Fall (6-month follow-up, 11th grade) 2015 among past 30-day vapers with available nicotine concentration data (N=181) from 10 high schools in the Los Angeles, CA metropolitan area.
Exposure
Self-report of baseline e-cigarette nicotine concentration (i.e., none [0 mg/mL], low [1–5 mg/mL], medium [6–17 mg/mL] or high [18 mg/mL or greater]) typically used during the past 30-days.
Main Outcome(s) and Measure(s)
Frequency of past 30-day combustible cigarette smoking and e-cigarette use (0 days [none], 1–2 days [infrequent], ≥ 3 days [frequent]) and daily smoking and vaping intensity (number of cigarettes smoked per day, number of vaping episodes per day and number of puffs per vaping episode) at 6-month follow-up.
Results
There were positive associations between baseline e-cigarette nicotine concentration vaped and frequent (vs. no) past 30-day combustible cigarette and e-cigarette use at follow-up. Each successive increase in nicotine concentration (none-to-low, low-to-medium, medium-to-high) was associated with a 2.26 (95% confidence interval [CI]: 1.28, 3.98) and 1.65 (95%CI: 1.09, 2.51) increase in odds of frequent smoking and vaping, respectively, after adjustment for baseline frequency of smoking and vaping and other relevant covariates. Use of high (vs. no) nicotine concentration e-cigarettes was associated with a greater number of cigarettes smoked/day at follow-up (adjusted rate ratio [95%CI] = 7.03 [6.11, 7.95]). Use of low, medium and high nicotine concentrations (vs. no nicotine) were associated with a significantly greater number of vaping episodes per day (adjusted rate ratios: 2.44–3.32) and number of puffs per vaping episode (adjusted rate ratios: 2.05–3.39) at follow-up (ps<.05).
Conclusions and Relevance
The results of this study provide preliminary evidence that use of e-cigarettes with higher nicotine concentrations by youth may increase the frequency and intensity of smoking and vaping.
Keywords: electronic cigarettes, nicotine concentration, youth, smoking, vaping
INTRODUCTION
In 2016, 11% of US 10th grade students reported using e-cigarettes (vaping) in the past 30-days.1 Prospective data demonstrates that youth who vape are more likely to subsequently initiate2–6 and progress to more frequent and heavy smoking.7 However, the reasons for these associations remain largely unknown. Identifying factors that underlie the progression of smoking and vaping among adolescents is critical for understanding, predicting and preventing adverse health consequences of youth e-cigarette use.
Nicotine is the principal constituent of combustible cigarettes that maintains smoking dependence, particularly during early adolescence—a critical developmental period in which the brain is especially vulnerable to the addictive properties of nicotine.8 E-cigarettes are available with a wide variety of nicotine concentrations, ranging from 0 mg/mL (i.e., no nicotine) to over 25 mg/mL,9 and use of e-cigarettes with higher nicotine concentrations has been shown to increase nicotine delivery to the blood stream and enhance the rewarding effects of vaping.10, 11 Accordingly, adolescents who use e-cigarettes with higher levels of nicotine may be at greater risk of developing a tolerance to and dependence on nicotine, which could contribute to both the persistence and progression of vaping as well as use of combustible tobacco products.
Recent cross-sectional studies suggest that there is considerable variation in the nicotine concentrations used by adolescent vapers,12–14 and that use of e-cigarettes with (vs. without) nicotine is associated with a greater likelihood of cigarette smoking and heavier e-cigarette use.14 However, it is unknown whether gradations in nicotine concentrations are longitudinally associated with subsequent progression to higher levels of smoking and vaping. Since e-cigarette solutions containing nicotine were recently deemed tobacco products and fall under FDA regulatory jurisdiction,15 assessing associations of e-cigarette nicotine concentration with use of tobacco products can inform regulatory policy addressing nicotine concentration in e-cigarette products. In the current study, we examined associations between baseline e-cigarette nicotine concentration vaped and subsequent frequency and intensity of combustible cigarette smoking and e-cigarette vaping at a 6-month follow-up among a sample of high school vapers.
METHODS
Participants
Participants were 10th grade students from 10 high schools in the Los Angeles, CA metropolitan area followed as part of a longitudinal survey of substance use and mental health.2 Data were collected and processed at five semiannual assessments beginning in fall 2013 when the cohort was beginning 9th grade through the fall of 2015. The e-cigarette nicotine concentration used by youth vapers was first assessed when the cohort was in 10th grade during spring of 2015 (baseline for this report). We included data from all past 30-day e-cigarette users who reported the nicotine concentration they vaped at baseline and who completed the 6-month follow-up during 11th grade (N=181). All data were collected via paper questionnaires at the participants’ high schools; participants who were not available on the day’s data were collected completed telephone or Internet surveys. Parental consent was obtained and youth assented to participation. Individual participants were not monetarily compensated, however each participating high school’s general fund was remunerated for staff time. The study was approved by the USC IRB.
Measures
E-Cigarette Nicotine Concentration
E-cigarette nicotine concentration levels typically vaped during the past 30 days at baseline were assessed with the question, “What level of nicotine (strength of e-liquid or juice) did you usually use in your e-cigarette?” The response options included no-nicotine (0 mg/mL), low- (1–5 mg/mL), medium- (6–17 mg/mL) and high-nicotine (18 mg/mL or greater) or “I don’t know.”16 Participants who did not know the nicotine concentration they typically vaped were excluded (N=28).
Past 30-Day Frequency of Combustible Cigarette and E-Cigarette Use
At baseline and follow-up, participants completed two survey questions assessing the number of days they smoked cigarettes and the number of days they vaped e-cigarettes in the past 30 days (response options: 1–2 days, 3–5 days, 6–9 days, 10–14, 15–19 days, 20–24, 25–29 days, all 30 days).1 Responses were collapsed into a three-level past 30-day smoking and vaping frequency variable: (1) no use (0 days); (2) infrequent use (1–2 days); and (3) frequent use (≥ 3 days) as in previous research due to lower frequency counts in categories of greater use (eFigure 1 and eFigure 2).7
Intensity of Combustible Cigarette and E-Cigarette Use
Participants reported the number of cigarettes they smoked on each smoking day (0 cigarettes, 1 cigarette, 2–5 cigarettes, 6–10 cigarettes, 11–15 cigarettes, 16–20 cigarettes, 20 or more cigarettes) in the past 30 days. The survey included two questions to characterize vaping intensity: (1) the number of vaping episodes per day, assessed with the question, “On the days you vaped, how many times did you usually pick up your e-cigarette device to vape?” (response options: 1 time, 2 times, 3–5 times, 6–9 times, 10–14 times, 15–20 times, or ≥ 20 times); and (2) the number of puffs taken during each vaping episode, assessed with the question, “Each time you picked up your e-cigarette to vape, how many puffs did you usually take before putting it away?” (response options: 0 puffs, 1 puff, 2 puffs, 3–5 puffs, 6–9 puffs, 10–14 puffs, 15–20 puffs, or ≥ 20 puffs).17, 18 These response categories were recoded into quantitative count variables by taking the lowest value of each ordinal smoking (i.e., 0, 1, 2, 6, 11, 16, 20 cigarettes/day) and vaping (i.e., 0, 1, 2, 3, 6, 10, 15, 20 puffs or episodes) category for use in the intensity analyses.
Covariates
Interpersonal, intrapersonal, and demographic factors measured at baseline that have previously been shown to be associated with tobacco product use were included as a priori covariates to address possible confounding of associations.19 Demographic characteristics such as gender, age, race/ethnicity (Hispanic, White, Asian and Other Race) and highest level of parental education (college degree or greater vs. other) were assessed with self-report measures. Interpersonal characteristics included peer vaping and smoking behavior (assessed with the questions, “In the last 30 days, how many of your 5 closest friends have smoked/vaped?” [no friends vs. 1 or more friends]), which were classified into a composite peer tobacco product use variable (yes/no). A variable was also created for lifetime use of tobacco products other than e-cigarettes and combustible cigarettes (e.g., cigars, hookah) at baseline (yes/no). Intrapersonal characteristics included depressive symptomology, delinquent behavior and sensation seeking. Depressive symptomology was measured using the Center for Epidemiologic Studies Depression Scale,20 a well-validated 20-item measure of past week frequency of experiencing depressive symptoms (internal consistency estimate: α = .93). Past 6-month delinquent behavior was assessed with an 11-item measure summing the reported frequency of engaging in deviant behaviors (e.g., stealing, destroying property, lying to parents, running away, physically fighting; score range: 1 [never] to 6 [≥10 times]; α = .93).21 Sensation seeking was measured with the sum score of the 12-item subscale of the UPPS Impulsive Behavior Scale (e.g., “I quite enjoy taking risks”, “I generally seek new and exciting experiences and sensations”; α = .93).22
Data Analysis
Preliminary analyses involved calculating descriptive statistics and distributional properties (i.e., skewness and kurtosis) for all tobacco product outcomes and covariates, stratified by baseline nicotine concentration. Chi-squared and one-way ANOVA tests assessed differences in covariates by baseline nicotine concentration. Primary analyses utilized generalized-linear mixed models with a random intercept to account for the clustering of students within their respective high schools.
Frequency outcomes
Polytomous (multinomial) regression models were used to test associations between baseline e-cigarette nicotine concentration (i.e., none, low, medium, high) and past 30-day use frequency (i.e., 0 days, 1–2 days, ≥ 3–5 days) at follow-up. Nicotine concentration was treated as a continuous variable (i.e., grouped-linear term [0=no nicotine; 1=low-nicotine; 2=medium-nicotine; 3=high-nicotine]). Combustible cigarette and e-cigarette use outcomes were evaluated in separate models with no past 30-day use of each product at follow-up as the reference group. Models were first tested as unadjusted without covariates and were then adjusted for baseline past 30-day smoking frequency, past 30-day vaping frequency, and all interpersonal, intrapersonal, and demographic covariates listed above.
Intensity outcomes
Since the daily intensity outcome variables (i.e., cigarettes per day, vaping episodes per day, puffs per vaping episodes) were not normally distributed (i.e., overdispersed), negative binomial regression models were used to assess associations with baseline nicotine concentration.23 Baseline nicotine concentration was treated first as a continuous and then as a categorical variable, with no-nicotine serving as the reference category. The negative binomial regression coefficients were exponentiated to obtain rate ratios (RRs). After testing unadjusted models, adjusted models controlling for all demographic, interpersonal, and intrapersonal covariates as well as past 30-day frequency and respective baseline intensity measure matching the outcome (i.e., cigarettes per day, puffs per vaping episode, or vaping episodes per day) were tested. Only observations with complete data on respective vaping and smoking variables were used. To address missing covariate data in the adjusted models, five multiply-imputed data sets were generated via the Markov-chain Monte Carlo method with available covariate data.24 The parameter estimates (OR or RR) from the polytomous and negative binomial regression models in each imputed data set were pooled and presented as a single estimate. SPSS version 24 (IBM Corp., Armonk, NY) and SAS version 9.4 (SAS Institute Inc.) were used for analyses; significance was set to .05 and all tests were two-tailed.
RESULTS
Sample Demographics and Baseline Vaping Characteristics
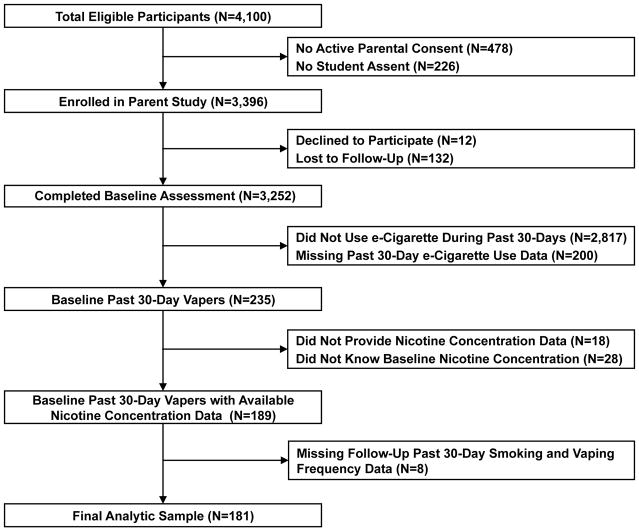
Among the N=4,100 students eligible to enroll in the parent study at the outset of 9th grade, assent and parental consent was obtained from 3,396 students, 3,252 of whom completed the spring 10th grade assessment (baseline for this report). At baseline, 235 students (7.2%) reported vaping in the past 30 days; 54 total participants were excluded from the analytic sample—18 did not answer the nicotine concentration question, 28 responded, “I don’t know” and eight participants were excluded for an absence of data at follow-up (Figure 1). Past 30-day vapers who were excluded from the analytic sample did not significantly differ from those included on any covariates or smoking and vaping variables (ps > .64).
Figure 1.
Flow of Adolescent e-Cigarette Users in Study
Note. Figure depicts flow of adolescents in study to assess e-cigarette nicotine concentration vaped at baseline and subsequent use of combustible cigarettes and e-cigarettes. Baseline assessment = Spring 2015, 10th grade.
The analytic sample (N=181) was relatively evenly distributed between males and females (53.0% male), majority Hispanic (50.8%), less than half of the participant’s parents attended college (37.0%) and 35% were past 30-day smokers (i.e., dual-users) at baseline (Table 1). There were significant differences in peer smoking/vaping, delinquent behavior and baseline patterns of combustible and e-cigarette use between the nicotine concentration groups, with participants who vaped higher nicotine concentrations exhibiting greater levels or likelihood of each characteristic (Table 1). At baseline, more than half of participants (59.7%) reported vaping a solution with nicotine during the past 30-days: 28.7% vaped a low-nicotine concentration, 19.3% vaped a medium-nicotine concentration and 11.6% vaped a high-nicotine concentration (Table 1).
Table 1.
Sample Demographic, Covariate, and Tobacco Use Variables by Baseline E-cigarette Nicotine Concentration
| Variable | Totala (N=181) | Baseline e-Cigarette Nicotine Concentrationab | P valuec | |||
|---|---|---|---|---|---|---|
|
| ||||||
| None (N=73) | Low (N=52) | Medium (N=35) | High (N=21) | |||
| Sociodemographic characteristics | ||||||
| Male | 96 (53.0) | 39 (53.4) | 24 (46.2) | 20 (57.1) | 13 (61.9) | .60 |
| Age, mean (SD), y (n=180)g | 16.1 (.4) | 16.1 (.4) | 16.0 (.4) | 16.1 (.4) | 16.0 (.3) | .30 |
| Race/ethnicity (n=177)g | .42 | |||||
| Hispanic | 88 (49.7) | 33 (45.8) | 27 (52.9) | 17 (50.0) | 11 (55.0) | |
| White | 38 (21.5) | 12 (16.7) | 12 (23.5) | 11 (32.4) | 3 (15.0) | |
| Asian | 34 (19.2) | 17 (23.6) | 9 (17.6) | 3 (8.8) | 5 (25.0) | |
| Other | 17 (9.6) | 10 (13.9) | 3 (5.9) | 3 (8.8) | 1 (5.0) | |
| Parental college degree or higher (n=154)g | 67 (43.5) | 33 (52.4) | 17 (36.2) | 10 (35.7) | 7 (43.8) | .29 |
| Interpersonal factors | ||||||
| Peer smoking or vaping (n=161)g | 141 (87.6) | 51 (77.3) | 46 (95.8) | 24 (92.3) | 20 (95.2) | .01 |
| Other tobacco product use (n=172)g | 138 (80.2) | 57 (79.2) | 41 (83.7) | 27 (90.0) | 13 (61.9) | .08 |
| Intrapersonal factors | ||||||
| UPPS Impulsive Behavior Scale Sensation Seeking score, mean (SD),d (n=154)g | 33.7 (9.1) | 34.4 (8.9) | 33.0 (7.7) | 33.4 (8.2) | 33.1 (13.6) | .85 |
| CESD score, mean (SD),e (n=176)g | 17.4 (12.7) | 16.0 (11.2) | 17.6 (13.2) | 16.5 (10.8) | 22.9 (17.9) | .18 |
| Delinquent behavior score, mean (SD),f (n=176)g | 19.3 (8.5) | 17.9 (6.1) | 19.1 (8.4) | 19.8 (7.5) | 24.4 (14.9) | .03 |
| Smoking variables | ||||||
| Cigarette smoking in past 30 d | ||||||
| Baseline (n=180)g | .001 | |||||
| 0 d | 117 (65.0) | 57 (79.2) | 34 (65.4) | 17 (48.6) | 9 (42.9) | |
| 1–2 d | 35 (19.4) | 6 (8.3) | 13 (25.0) | 12 (34.3) | 4 (19.0) | |
| ≥ 3 d | 28 (15.6) | 9 (12.5) | 5 (9.6) | 6 (17.1) | 8 (38.1) | |
| Follow-up | .001 | |||||
| 0 d | 138 (76.2) | 62 (84.9) | 42 (80.8) | 24 (68.6) | 10 (47.6) | |
| 1–2 d | 18 (9.9) | 7 (9.6) | 5 (9.6) | 4 (11.4) | 2 (9.5) | |
| ≥ 3 d | 25 (13.8) | 4 (5.5) | 5 (9.6) | 7 (20.0) | 9 (42.9) | |
| No. of cigarettes smoked per d, mean (SD) | ||||||
| Baseline (n=179)g | .6 (1.7) | .2 (.5) | .5 (1.0) | .7 (1.2) | 1.9 (4.5) | .002 |
| Follow-up | .5 (2.2) | .2 (.5) | .4 (1.0) | .3 (.6) | 2.5 (5.9) | <.001 |
| Vaping variables | ||||||
| Use in past 30 d | ||||||
| Baseline | .001 | |||||
| 1–2 d | 83 (45.9) | 43 (58.9) | 26 (50.0) | 10 (28.6) | 4 (19.0) | |
| ≥3 d | 98 (54.1) | 30 (41.1) | 26 (50.0) | 25 (71.4) | 17 (81.0) | |
| Follow-up | .03 | |||||
| 0 d | 92 (50.8) | 45 (61.6) | 24 (46.2) | 16 (45.7) | 7 (33.3) | |
| 1–2 d | 34 (18.8) | 15 (20.6) | 10 (19.2) | 7 (20.0) | 2 (9.5) | |
| ≥ 3 d | 55 (30.4) | 13 (17.8) | 18 (34.6) | 12 (34.3) | 12 (57.1) | |
| No. of episodes per d, mean (SD) | ||||||
| Baseline (n=179)g | 4.6 (6.3) | 3.5 (5.8) | 3.8 (4.9) | 5.7 (6.7) | 8.6 (8.6) | .005 |
| Follow-up (n=171)g | 2.8 (5.4) | 1.3 (4.0) | 3.2 (5.4) | 3.7 (6.0) | 5.2 (7.8) | .02 |
| No. of puffs per vaping episode, mean (SD) | ||||||
| Baseline | 6.8 (6.1) | 5.5 (5.5) | 5.6 (5.0) | 9.0 (6.6) | 10.3 (7.3) | <.001 |
| Follow-up (n=170)g | 3.1 (5.6) | 1.3 (3.3) | 3.0 (4.9) | 6.1 (7.6) | 4.6 (7.1) | <.001 |
Abbreviations: CESD, Center for Epidemiologic Studies Depression Scale; e-cigarette, electronic cigarette.
Data are expressed as number (percentage) of participants unless otherwise indicated.
None indicates 0 mg/mL; low, 1 to 5 mg/mL; medium, 6 to 17 mg/mL; and high, 18 mg/mL or greater.
Tests of differences in sample characteristics by baseline nicotine concentration vaped were conducted with χ2 tests for categorical variables and 1-way analysis of variance for continuous variables.
Possible range of scores from 0–48, with higher scores indicating greater levels of sensation seeking.
Possible range of scores from 0–60, with higher scores indicating greater severity of depressive symptoms.
Possible range of scores from 11–66, with higher scores indicating greater frequency of engaging in deviant behaviors.
The available sample for this variable is provided due to missing data.
Associations between Baseline Nicotine Concentration and Smoking and Vaping Frequency at Follow-Up
The prevalence of smoking and vaping frequency at follow-up by baseline nicotine concentration level are reported in independent models (Table 2). For each one-level increase in baseline nicotine concentration (i.e., none-to-low, low-to-medium, medium-to-high), the odds of participants reporting frequent past 30-day smoking (vs. no smoking) at follow-up was 2.43 times greater (OR [95% CI] = 2.43 [1.58, 3.76]). This association remained significant after adjustment for covariates (OR [95% CI] = 2.26 [1.28, 3.98]). Use of higher e-cigarette nicotine concentrations at baseline was not associated with increased odds of infrequent (versus no) past 30-day smoking in the unadjusted or adjusted models (ps = .44–.62; Table 2).
Table 2.
Association Between Baseline Nicotine Concentration and Study Outcomes
| Nicotine concentrationa | Frequency of Nicotine Product Use in Past 30 d at Follow-Up, OR (95%)b | Daily Intensity of Nicotine Product Use at Follow-Up, RR (95% CI)c | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Smoking | Vaping | No. of Cigarettes Per Day | No. of Vaping Episodes Per Day | No. of Puffs Per Vaping Episode | |||
| 1–2 d | ≥3 d | 1–2 d | ≥3 d | ||||
|
|
|
|
|
||||
| Unadjusted Models | |||||||
| Low (N=52) | NA | NA | NA | NA | 2.05 (1.09, 3.01) | 2.46 (1.62, 3.30) | 2.41 (1.65, 3.18) |
| Medium (N=35) | NA | NA | NA | NA | 1.92 (1.05, 2.78) | 2.77 (1.89, 3.66) | 4.90 (4.16, 5.65) |
| High (N=21) | NA | NA | NA | NA | 14.17 (13.00, 15.33) | 3.90 (2.94, 4.86) | 3.67 (2.77, 4.57) |
| Trend effectsd | 1.21 (0.72,1.98) | 2.43 (1.58, 3.76) | 1.06 (0.69, 1.59) | 1.73 (1.24, 2.41) | 2.32 (1.50, 3.59) | 1.76 (1.33, 2.33) | 1.57 (1.18, 2.08) |
| Adjusted Modelse | |||||||
| Low (N=52) | NA | NA | NA | NA | 1.65 (0.73, 2.57) | 3.32 (2.61, 4.03) | 2.05 (1.41, 2.70) |
| Medium (N=35) | NA | NA | NA | NA | 1.63 (0.77, 2.49) | 3.32 (2.54, 4.10) | 3.39 (2.66, 4.11) |
| High (N=21) | NA | NA | NA | NA | 7.03 (6.11, 7.95) | 2.44 (1.63, 3.24) | 2.23 (1.42, 3.03) |
| Trend effectsd | 1.01 (0.54, 1.89) | 2.26 (1.28, 3.98) | 0.98 (0.59, 1.60) | 1.65 (1.09, 2.51) | 1.74 (1.27, 2.37) | 1.42 (1.09, 1.85) | 1.69 (1.14, 2.19) |
Abbreviations: e-cigarette, electronic cigarette; NA, insufficient size to calculate effects; OR, odds ratio; RR, rate ratio.
Nicotine concentration vaped at baseline indicates the regressor. No nicotine indicates 0 mg/mL; low 1 to 5 mg/mL; medium, 6 to 17 mg/mL; and high, 18 mg/mL or greater.
Polytomous (multinomial) regression model (contrast category for respective outcome: 0 days of use).
Negative binomial regression model (reference group for regressor: No nicotine [0 mg/mL]).
Nicotine concentration is a continuous predictor (scored: No nicotine = 0, low = 1; medium = 2; high = 3)
Adjusted for age, sex, race/ethnicity, highest parental educational level, baseline lifetime other tobacco product use, baseline e-cigarette or combustible cigarette topography in the past 30 days, baseline e-cigarette or combustible cigarette use in the past 30 days, baseline peer vaping, baseline peer smoking, sensation seeking, depressive symptoms, and delinquent behavior.
Sample sizes range from 170–181 for unadjusted models and 168–179 for adjusted models.
For each 1-level increase in baseline nicotine concentration, the odds of being frequent past 30-day vapers (i.e., ≥ 3 days) compared to non-vapers at follow-up were 1.73 times greater (OR [95% CI] = 1.73 [1.24, 2.41]). This association remained significant after adjustment for covariates (OR [95% CI] = 1.65 [1.09, 2.51)]). In both unadjusted and adjusted models, e-cigarette nicotine concentration used at baseline was not associated with infrequent vaping (ps = .81–.98; Table 2).
Associations between Baseline Nicotine Concentration and Smoking and Vaping Intensity at Follow-Up
There were no significant differences in daily smoking quantity between youth who did not vape nicotine and youth who either vaped low- or medium-nicotine concentrations at baseline (Table 2). Compared to youth who did not vape nicotine at baseline, those who vaped high-nicotine concentrations smoked 14.1 times as many cigarettes per day (RR [95% CI] = 14.1 [13.0, 15.3]), and this association remained significant after adjustment for covariates (RR [95% CI] = 7.03 [6.11, 7.95]).
Youth who vaped low-nicotine concentrations vaped about 2.4 times as many puffs per vaping episode (RR [95% CI] = 2.41 [1.65, 3.18]), youth who vaped medium-nicotine concentrations vaped about 4.9 times as many puffs per vaping episode (RR [95% CI] = 4.90 [4.16, 5.65]) and youth who vaped high nicotine concentrations vaped about 3.7 as many puffs per vaping episode (RR [95% CI] = 3.67 [2.77, 4.57]), demonstrating a positive linear trend (RR [95% CI] = 1.57 [1.16, 2.11]). Similarly, youth who vaped low-nicotine concentrations had about 2.5 times as many vaping episodes per day (RR [95% CI] = 2.46 [1.62, 3.30]), youth who vaped medium-nicotine concentrations had about 2.8 times as many vaping episodes per day (RR [95% CI] = 2.77 [1.89, 3.66]) and youth who vaped high-nicotine concentrations had 3.9 times as many vaping episodes per day (RR [95% CI] = 3.90 [2.94, 4.86]), demonstrating a positive linear trend (RR [95% CI] = 1.76 [1.33, 2.33]). All associations between baseline nicotine concentration vaped and vaping intensity outcomes remained significant after adjustment for covariates (Table 2).
DISCUSSION
Youth who vaped e-cigarettes with higher nicotine concentrations at baseline were generally more likely to progress to higher frequency and intensity levels of both vaping and smoking at a 6-month follow-up, after adjusting for baseline e-cigarette and combustible cigarette use. While previous studies have examined cross-sectional associations of e-cigarette nicotine concentrations used by youth and patterns of smoking and vaping,12–14 to our knowledge this is the first prospective study to evaluate the impact of varying e-cigarette nicotine concentrations on future smoking and vaping behavior. In the context of research demonstrating that youth who use e-cigarettes are more likely to initiate2–6 and progress7 to higher levels of combustible cigarette use, the current findings suggest that the overrepresentation of frequent and high-intensity smoking among vapers may be accounted for by nicotine concentration in e-cigarettes.
Intensity of combustible cigarette smoking at younger ages is associated with increased nicotine dependence later in life.25, 26 Exposure to higher levels of nicotine during early adolescence increases the risk of nicotine dependence,27 and adversely impacts attentional processes,28–30 executive functioning and inhibitory control.31 Youth in this study who vaped higher nicotine concentrations at baseline may have developed a tolerance to and dependence on nicotine, increasing their levels of vaping and smoking to accommodate nicotine-induced adaptations resulting from e-cigarette related nicotine exposure. Given the potential neurocognitive effects caused by nicotine exposure to the adolescent brain,32, 33 teens who vaped higher nicotine concentrations may also be prone to poor decision making and risk-taking behaviors, including increased vaping and smoking. While biologically plausible, whether nicotine-induced tolerance, dependence, neural dysregulation or other cognitive (e.g., expectancies) and social (e.g., peer affiliations) factors explain the observed associations warrants further investigation.
It is also possible that shared unmeasured risk factors explain the association between use of e-cigarettes with higher nicotine concentrations and trajectories of accelerated vaping and smoking. While we cannot exclude this possibility, we attempted to address this issue analytically by adjusting for a host of demographic, interpersonal, and intrapersonal risk factors for vaping and smoking, including baseline vaping and smoking levels. Adjusted ORs and RRs did not meaningfully differ from the unadjusted estimates, suggesting that the available covariates are unlikely to confound the associations demonstrated herein.
Among 10th grade students in the 2015 US Monitoring the Future Study, 27% of the 704 ever-vapers and 41% of the 268 participants who vaped 6 or more times in their life, respectively, reported vaping nicotine in their last vaping episode.13 In this study, the prevalence of nicotine vaping among all past 30-day vapers (including in the denominator those who did not know if nicotine was in the e-cigarette they typically used) was 52%. One reason why nicotine vaping may have been more common in the current sample is that participants in this study were all past 30-day vapers who were asked what nicotine concentration they typically vaped over the past 30-days, whereas the Monitoring the Future study assessed the substance vaped in the most recent episode.13 Since youth alternate use of different e-liquids34 that may or may not contain nicotine, nicotine vapers may not necessarily have vaped an e-cigarette containing nicotine during their most recent vaping occasion, which would result in lower nicotine vaping prevalence estimates than assessing the substance typically vaped. Alternatively, the participants in this study were all from California, and it is possible that California adolescent e-cigarette users may vape nicotine at higher rates than national samples.
Strengths of the study are the demographically diverse sample, high rate of retention and detailed assessment of smoking and vaping intensity. Limitations include the relatively small sample, reliance on self-report data, and lack of biochemical verification of reported e-cigarette nicotine concentrations vaped by youth. Evidence suggests that e-liquid nicotine concentrations can be mislabeled, however, since chemically-verified nicotine concentrations have typically been found to be higher than mislabeled concentrations, our estimates may be conservative.35 The observational period in this study captures an important, but brief, window in adolescent development and extension to longer periods of follow-up is warranted. The study did not assess or account for nicotine dependence or other e-cigarette device parameters (e.g., device generation, wattage, machinery efficiency) that may affect nicotine absorption into the blood stream.36, 37 Further research with larger samples is needed to elucidate whether nicotine concentration, per se, exerts a causal effect on smoking and vaping and subsequent nicotine dependence among youth.
CONCLUSIONS
Among the adolescent e-cigarette users in this study, use of e-cigarettes with higher nicotine concentrations at baseline was associated with progression of both smoking and vaping frequency and intensity at a 6-month follow-up. Given the FDA’s 2016 Deeming Rule, the results of this study provide preliminary evidence that regulatory policies addressing nicotine concentration levels in e-cigarette products used by adolescents may impact progression of combustible cigarette and e-cigarette use among youth.
Supplementary Material
KEY POINTS.
Question
Is the use of e-cigarettes with higher nicotine concentrations prospectively associated with greater frequency and intensity of combustible cigarette smoking and vaping in adolescents?
Findings
In this prospective cohort study of 181 high school e-cigarette users, use of e-cigarettes with higher nicotine concentrations at baseline was associated with greater levels of past 30-day combustible cigarette and e-cigarette use at 6-month follow-up and greater intensity of daily use after controlling for baseline use.
Meaning
Use of e-cigarettes with higher nicotine concentrations may contribute to the progression to smoking and vaping at higher levels of frequency and intensity among youth.
References
- 1.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; [Google Scholar]
- 2.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2017;26(1):34–39. doi: 10.1136/tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–1023. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):e20160379. doi: 10.1542/peds.2016-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miech R, Patrick ME, O’Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017 doi: 10.1136/tobaccocontrol-2016-053291. pii: tobaccocontrol-2016–053291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leventhal AM, Stone MD, Andrabi N, et al. Association of e-Cigarette Vaping and Progression to Heavier Patterns of Cigarette Smoking. JAMA. 2016;316(18):1918–1920. doi: 10.1001/jama.2016.14649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General. The health consequences of smoking—50 years of progress: A report of the surgeon general, 2014. 2014. [Google Scholar]
- 9.Grana R, Benowitz N, Glantz SA. E-cigarettes a scientific review. Circulation. 2014;129(19):1972–1986. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez AA, Hiler MM, Soule EK, et al. Effects of Electronic Cigarette Liquid Nicotine Concentration on Plasma Nicotine and Puff Topography in Tobacco Cigarette Smokers: A Preliminary Report. Nicotine Tob Res. 2016;18(5):720–723. doi: 10.1093/ntr/ntv182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawkins LE, Kimber CF, Doig M, Feyerabend C, Corcoran O. Self-titration by experienced e-cigarette users: blood nicotine delivery and subjective effects. Psychopharmacology (Berl) 2016;233(15–16):2933–2941. doi: 10.1007/s00213-016-4338-2. [DOI] [PubMed] [Google Scholar]
- 12.Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. 2015;17(7):810–818. doi: 10.1093/ntr/ntu243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miech R, Patrick ME, O’Malley PM, Johnston LD. What are kids vaping? Results from a national survey of US adolescents. Tob Control. 2016 doi: 10.1136/tobaccocontrol-2016-053014. tobaccocontrol-2016–053014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morean ME, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Nicotine concentration of e-cigarettes used by adolescents. Drug Alcohol Depend. 2016;167:224–227. doi: 10.1016/j.drugalcdep.2016.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Food, Drug Administration H. Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products. Final rule. Federal register. 2016;81(90):28973. [PubMed] [Google Scholar]
- 16.Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15(1):158–166. doi: 10.1093/ntr/nts103. [DOI] [PubMed] [Google Scholar]
- 17.Foulds J, Veldheer S, Yingst J, et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob Res. 2015;17(2):186–192. doi: 10.1093/ntr/ntu204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim H, Davis AH, Dohack JL, Clark PI. E-Cigarettes Use Behavior and Experience of Adults: Qualitative Research Findings to Inform E-Cigarette Use Measure Development. Nicotine Tob Res. 2017;9(2):190–196. doi: 10.1093/ntr/ntw175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 21.Thompson MP, Ho CH, Kingree JB. Prospective associations between delinquency and suicidal behaviors in a nationally representative sample. J Adolesc Health. 2007;40(3):232–237. doi: 10.1016/j.jadohealth.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30(4):669–689. [Google Scholar]
- 23.Wagner B, Riggs P, Mikulich-Gilbertson S. The importance of distribution-choice in modeling substance use data: a comparison of negative binomial, beta binomial, and zero-inflated distributions. Am J Drug Alcohol Abuse. 2015;41(6):489–497. doi: 10.3109/00952990.2015.1056447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 25.Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug and alcohol dependence. 1993;33(2):129–137. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- 26.Riggs NR, Chou C-P, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9(11):1147–1154. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- 27.Slotkin TA. Nicotine and the adolescent brain: insights from an animal model. Neurotoxicol Teratol. 2002;24(3):369–384. doi: 10.1016/s0892-0362(02)00199-x. [DOI] [PubMed] [Google Scholar]
- 28.England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49(2):286–293. doi: 10.1016/j.amepre.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacology & therapeutics. 2009;122(2):125–139. doi: 10.1016/j.pharmthera.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murthy VH. E-Cigarette Use Among Youth and Young Adults A Major Public Health Concern. JAMA Pediatr. 2016;171(3):209–210. doi: 10.1001/jamapediatrics.2016.4662. [DOI] [PubMed] [Google Scholar]
- 31.DeBry SC, Tiffany ST. Tobacco-induced neurotoxicity of adolescent cognitive development (TINACD): a proposed model for the development of impulsivity in nicotine dependence. Nicotine Tob Res. 2008;10(1):11–25. doi: 10.1080/14622200701767811. [DOI] [PubMed] [Google Scholar]
- 32.Swan GE, Lessov-Schlaggar CN. The effects of tobacco smoke and nicotine on cognition and the brain. Neuropsychol Rev. 2007;17(3):259–273. doi: 10.1007/s11065-007-9035-9. [DOI] [PubMed] [Google Scholar]
- 33.Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR. Effects of smoking and smoking abstinence on cognition in adolescent tobacco smokers. Biol Psychiatry. 2005;57(1):56–66. doi: 10.1016/j.biopsych.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 34.Kong G, Morean ME, Cavallo DA, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2014;17(7):847–54. doi: 10.1093/ntr/ntu257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis B, Dang M, Kim J, Talbot P. Nicotine concentrations in electronic cigarette refill and do-it-yourself fluids. Nicotine Tob Res. 2015;17(2):134–41. doi: 10.1093/ntr/ntu080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramôa CP, Hiler MM, Spindle TR, et al. Electronic cigarette nicotine delivery can exceed that of combustible cigarettes: a preliminary report. Tob Control. 2016;25(e1):e6–9. doi: 10.1136/tobaccocontrol-2015-052447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.St Helen G, Havel C, Dempsey DA, Jacob P, 3rd, Benowitz NL. Nicotine delivery, retention and pharmacokinetics from various electronic cigarettes. Addiction. 2016;111(3):535–544. doi: 10.1111/add.13183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.