Abstract
Poor mental health and substance use are associated with food insecurity, however, their potential combined effects have not been studied. This study explored independent associations and effect modification between lifetime substance use and mood disorder in relation to food insecurity. Poisson regression analysis of data from British Columbia respondents (n = 13,450; 12 years+) in the 2007/08 Canadian Community Health Survey was conducted. Measures included The Household Food Security Survey Module (7.3% food insecure), recent diagnosis of a mood disorder (self-reported; 9.5%), lifetime use of cannabis, cocaine/crack, ecstasy, hallucinogens, and speed, any lifetime substance use, sociodemographic covariates, and the interaction terms of mood disorder by substance. For those with recent diagnosis of a mood disorder the prevalence of lifetime substance use ranged between 1.2 to 5.7% and were significantly higher than those without recent mood disorder diagnosis or lifetime use of substances (p’s < 0.05). For respondents with a recent mood disorder diagnosis or who used cannabis, food insecurity prevalence was higher compared to the general sample (p < 0.001); prevalence was lower for cocaine/crack use (p < 0.05). Significant effect modification was found between mood disorder with cannabis, ecstasy, hallucinogen and any substance use over the lifetime (PRs 0.51 to 0.64, p’s 0.022 to 0.001). Independent associations were found for cocaine/crack and speed use (PRs 1.68, p’s < 0.001) and mood disorder (PRs 2.02, p’s < 0.001). Based on these findings and the existing literature, future study about coping and resilience in the context of substance use, mental health, and food insecurity may lead to the development of relevant interventions aimed at mental well-being and food security.
Introduction
Food insecurity–which occurs when people are physically or economically unable to consume a diet of sufficient quantity of food, or have uncertainty in their ability to do so [1]–profoundly impacts mental well-being. Several studies have reported associations between food insecurity and various indicators of poor mental health such as depression, suicide ideation and substance use and some of these relationships may be bidirectional [2–7]. A better understanding of these associations could help provide the information needed to develop comprehensive policy and program interventions that would mitigate food insecurity.
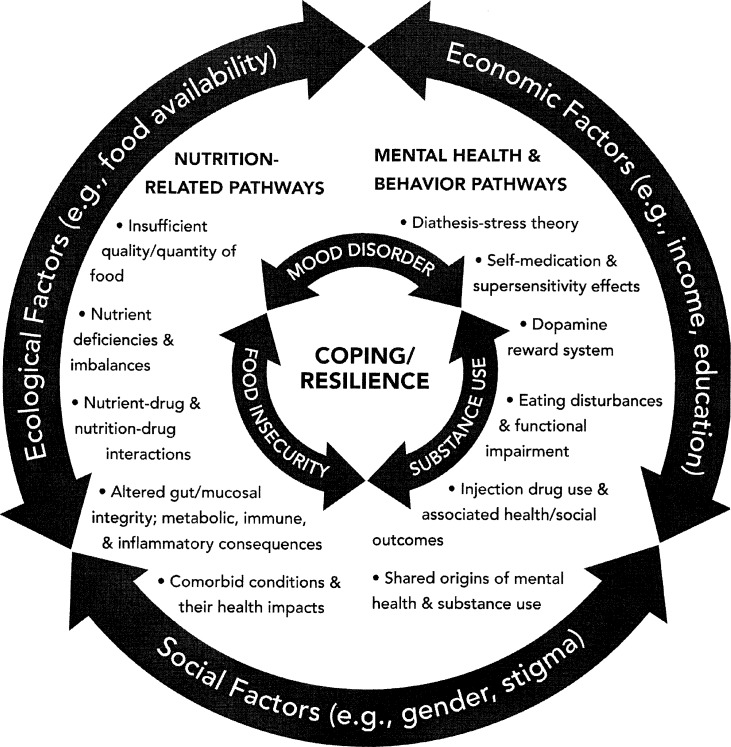
While studies about food insecurity and mental health have often controlled for substance use as a potential confounder, no studies have measured for possible effect modification between poor mental health and substance use. A number of mechanisms related to economic (income, education), social (gender, stigma), macro-level drivers (e.g., food environments), and biological pathways (e.g., stress response, inadequate nutrients) [8, 9] explain potential inter-relations among poor substance use, mental health, and food insecurity (Fig 1). Poor mental health among those who are food insecure [10–12] can contribute to high stress levels, challenges in coping, and increased risk to use substances. Studies about food insecurity and injection drug use suggest that between 30% and 70% of individuals who use drugs report some level of food insecurity [2, 13–18]. Nutritional inadequacy, which is often correlated with food insecurity [19] and substance use [20–24], is linked with poor mental health [25–28]. Stress, due to feelings of deprivation and/or anxiety about food supply [7, 29–31], can be a contributor to or outcome of food insecurity, mental health, and/or substance use.
Fig 1. Food insecurity, poor mental health, and substance use: Explanatory pathways [9, 45].
Mental health symptoms (e.g., loss of interest in usual activities, impairment in cognition) [10] can also alter food skills (e.g., reduced concentration to follow recipes) and choices (e.g., selection of more convenient options), reduce income, and/or impact housing and accommodation [32] and thereby contribute to food insecurity. Structural based stresses, including insufficient income, poor housing, lack of secure, well-paid employment, and inadequate social support further compound challenges related to food insecurity, coping, and mental health [33].
It is well established that poor mental health and substance use frequently co-occur [34–36]. Substance use may be a cause or consequence of mental ill health or share a common origin with mental ill health. An alternative explanation is that mental ill health and substance use interact and maintain each other [37]. Given these reported relationships, it would seem reasonable to expect that substance use would be a direct effect modifier of mental health in relation to the outcome of food insecurity. Applying an effect modification analysis to examine the associations between substance use and mental health could help to address the complex issue of food insecurity in and lead to the development of effective prevention tools in vulnerable subpopulations.To better understand these relationships, national data that provides measures of previous substance use, recent mood disorder diagnosis (past 12 months), and household food security (past 12 months) was analyzed to examine: 1) the prevalence of food insecurity among those with recent diagnosis of a mood disorder and that reported lifetime use of selected substances; 2) effect modification between lifetime substance use and recent mood disorder diagnosis in relation food insecurity. In this analysis prior substance use is considered a direct effect modifier of mental health (exposure variable) and its relationship to food insecurity (outcome). We hypothesized that: 1) the prevalence of food insecurity would be higher in those with a recent diagnosis of a mood disorder and that reported lifetime substance use compared to those without a recent diagnosis of a mood disorder or reported lifetime substance use; and 2) there would be significant effect modification between all types of substance use and recent mood disorder diagnosis in relation to food insecurity.
Materials and methods
Sampling method and sample
The sample (Canadians 12 years+) was derived from the 2007/08 (Cycles 4.1/4.2) Canadian Community Health Survey (CCHS). Respondents are selected using a multi-stage sampling strategy [38] and do not include persons living on reserves and other Aboriginal settlements in the provinces; full-time members of the Canadian Forces; the institutionalized population; and children aged 12–17 that are living in foster care. Collectively, these exclusions represent less than 3% of the Canadian population aged 12 and over. At the time of household contact for data collection, the interviewer sees a list of all members of the household listed and a person aged 12 years or over is automatically selected using various selection probabilities based on age and household composition. All Individuals sampled, including those between 12 to 18 years, answered the questions on their own. However, for some questions (e.g., income) consulation with a parent or guardian may have been necessary. The study sample were respondents from British Columbia, a province which opted to include measures of substance use (n = 13,450). Approval for use of the de-identified CCHS dataset was granted by Statistics Canada. All data was vetted by a Statistics Canada analyst prior to release to ensure that respondent privacy was maintained.
Measurements
Food insecurity
Food insecurity was measured using the 18-item Household Food Security Survey Module (HFSSM) [39]. To help reduce respondent burden, CCHS respondents were first screened based on responses to either of the "food sufficiency questions" which asked whether the household, in the past 12 months sometimes did not have enough to eat or often did not have enough to eat. Those who answered affirmatively to the screening questions were then administered the HFSSM. The food security classifications used for this study included: 1) Food secure: 0 or 1 affirmative response on HFSSM’s adult and/or child scale; indicates access, at all times in the previous year, to enough food for an active, healthy life for all household members; 2) Food insecure: included categories of moderate (2 to 5 affirmative responses on HFSSM’s adult and/or child scale) or severe food insecurity (> 6 affirmative responses on HFSSM’s adult and/or child scale); indicates that any household member had compromised in quality and/or quantity of food consumed which may have disrupted eating patterns.
Mood disorder
A composite variable to describe presence of a mood disorder was based on responses to two survey questions: 1) a question that asked whether an individual had been diagnosed with a mood disorder such as depression, bipolar disorder, mania, or dysthymia by a healthcare professional in the past 12 months; plus 2) a question that asked about having an anxiety disorder such as a phobia, obsessive- compulsive disorder or a panic disorder. We compared results of analysis (substance use in relation to food insecurity) between those diagnosed with mood disorder versus those with a diagnosed mood disorder that also indicated they had other mental health conditions and found no significant differences. Therefore respondents who indicated they had been diagnosed with a mood disorder in the past 12 months, including those with reported comorbidities of anxiety, obsessive-compulsive or panic disorder, were included in the analysis.
Substance use
Assessment of substance use was based on questions derived from Canada’s Alcohol and Other Drugs Survey [40] that asked about lifetime use of: 1) marijuana, cannabis or hashish (> once); 2) cocaine or crack; 3) speed (amphetamine); 4) ecstasy (3,4-methylenedioxy-methamphetamine) or similar drugs; or 5) hallucinogens, phencyclidine (PCP) or lysergic acid diethylamide (LSD). We analyzed each substance separately as current literature is limited about their relationships with food insecurity. We also analyzed a composite variable that measured any lifetime substance use; a derived variable from the survey. While data on other substances (e.g., steroids) was collected and the opportunity existed to also examne polysubstance use, the frequencies on these measures were too low to enable analysis.
Covariates
Covariates were selected based on a literature search of factors that may confound or mediate the relationships among food insecurity, mental health, and substance use. The covariates sex, age (categorized as < 18 years, 18 to 29 years, 30 to 39 years, 40 to 49 years, 50 to 59 years, and > 60 years), education (four categories: no post- secondary degree, certificate or diploma; secondary school graduation, no post- secondary education; some post-secondary education; or post-secondary degree/diploma), and relationship status (in a relationship as married or common-law versus not in a relationship that included widowed, separated, divorced, single, never married). We also included the covariate income, dichotomized as low versus adequate income, that was based on a derived variable which measured the ratio between the total income of the respondent's household and the low income cut-off corresponding to the number of persons in the household and the size of the community.
Data analysis
The secured data was analyzed using STATA 11.0 [41] in a Statistics Canada Research Data Center. The bootstrap method was used to account for the complex survey design [42]. Descriptive analysis was done for all variables. Bivariate and stratified analyses were done to assess relationships between all variables and food insecurity. Using Poisson regression with robust variance, adjusted prevalence ratios (proportion with food insecurity/proportion exposed to a substance during their lifetime and proportion with food insecurity/proportion diagnosed with a mood disorder in the previous year) were analyzed. Poisson regression was selected for this cross-sectional data as the exposure (e.g., lifetime substance use) refers to the beginning of the presumed individual risk periods.
In total, six models were analyzed; one for each of the five substances and one which included a composite variable of any lifetime substance use. In each model, interaction terms were generated for substance by mood disorder in order to test for effect modification. The analysis for each of the six models first consisted of including all individual variables and the interaction terms (full model). If the interaction terms were not significant, then subsequent analyses were conducted with the non-significant interaction terms removed. Goodness-of-fit chi-squared tests assessed for model fit.
Results
In the sample of 13,450 individuals from British Columbia, 7.3% (95% CI 6.9–7.7) were food insecure. Of those who were recently diagnosed with a mood disorder (n = 1280), the prevalence of food insecurity was significantly higher compared to the general sample (19.0%, 95% 16.8–21.1, p < 0.0001). In addition, those with recent mood disorder diagnosis had significantly higher prevalence estimates of lifetime use for each substance (1.2 to 5.7%) compared to those without recent mood disorder diagnosis or lifetime use of substances (p’s < 0.05). Of those who reported having a mood disorder, there were significant differences according to age, relationship status, income level and food insecurity status (p’s < 0.05) (Table 1) compared to those without a mood disorder. Of the different types of substances used by those who reported having a mood disorder, the prevalence of food insecurity (13.7%, 95% CI 11.8–15.6) was significantly higher for cannabis use versus non-use (5.9%, 95% CI 4.6–7.2, p < 0.001). Conversely, the prevalence of food insecurity (6.9%, 95% CI 5.5–8.3) was significantly lower for cocaine and crack use versus non-use (12.7%, 95% CI 10.9–14.6, p < 0.05).
Table 1. Sample and substance use characteristics by food security status in individuals diagnosed with a mood disorder in past 12 monthsa.
| Diagnosis of mood disorder in past 12 months | |||
|---|---|---|---|
| Characteristic | Food secure | Food insecure | χ2, p-value |
| Sex | 0.90, p = 0.342 | ||
| Males | 28.5 | 5.9 | |
| Females | 52.6 | 13.1 | |
| Age | 2.76, p = 0.021 | ||
| 12 to 18 years | 3.9 | 1.0 | |
| 18 to 29 years | 1.1 | 4.2 | |
| 30 to 39 years | 14.8 | 3.6 | |
| 40 to 49 years | 18.5 | 4.9 | |
| 50 to 59 years | 15.4 | 3.6 | |
| > 60 years | 17.3 | 1.8 | |
| Education | 0.94, p = 0.423 | ||
| No post-secondary degree, certificate or diploma | 14.1 | 3.9 | |
| Secondary school graduation, no post-secondary education | 13.7 | 4.0 | |
| Some post-secondary education | 9.9 | 2.4 | |
| Post-secondary degree/diploma | 43.2 | 8.8 | |
| Relationship Status | 11.86, p < 0.001 | ||
| In relationship (married, or common-law) | 47.3 | 6.1 | |
| Not in a relationship (widowed, separated, divorced, single, never married) | 33.7 | 13.0 | |
| Income | 92.50, p < 0.001 | ||
| Adequate income | 70.8 | 9.4 | |
| Low income | 10.2 | 9.6 | |
| Substances: Lifetime Use | 12.46, p = 0.001 | ||
| Marijuana, cannabis or hashish (more than once) | |||
| Yes | 42.6 | 13.7 | |
| No | 37.9 | 5.9 | |
| Cocaine or crack | 8.68, p = 0.003 | ||
| Yes | 16.9 | 6.9 | |
| No | 63.6 | 12.7 | |
| Speed (amphetamines) | 3.59, p = 0.059 | ||
| Yes | 9.0 | 3.4 | |
| No | 71.7 | 16.9 | |
| Ecstasy (3,4-methylenedioxy-methamphetamine; MDMA) or other similar drugs | 1.75, p = 0.186 | ||
| Yes | 10.5 | 3.6 | |
| No | 70.0 | 15.9 | |
| Hallucinogens, PCP (phencyclidine), or LSD (Lysergic acid diethylamide; acid) | 2.37, p = 0.125 | ||
| Yes | 16.6 | 5.2 | |
| No | 63.9 | 14.3 | |
| Lifetime use of any substance | 9.00, p = 0.003 | ||
| Yes | 46.0 | 13.9 | |
| No | 34.5 | 5.7 | |
aTotals for some variables may not exactly be 100 due to rounding
Based on the Poisson regression analysis (Table 2), significant independent associations were found between cocaine/crack (PR 1.68, 95% CI 1.33–2.12), p < 0.001) and speed (PR 1.67, 95% CI 1.29–2.17, p < 0.001) in relation to food insecurity. In the model including cocaine/crack, recent mood disorder diagnosis (PR 2.02, 95% CI 1.64–2.49, p < 0.001), age (PR 0.81, 95% CI 0.77–0.85, p < 0.001), relationship status (PR 1.53, 95% CI 1.22–1.92, p < 0.001), education (PR 1.62, 95% CI 1.30–2.01, p < 0.001), and income (PR 4.29, 95% CI 3.53–5.22, p < 0.001) were also significantly associated with food security status. Similarly, in the model including speed, recent mood disorder diagnosis (PR 2.13, 95% CI 1.75–2.59, p < 0.001), age (PR 0.81, 95% CI 0.77–0.85, p < 0.001), relationship status (PR 1.54, 95% CI 1,23–1.93, p < 0.001), education (PR 1.63, 95% CI 1.30–2.04, p < 0.001), and income (PR 4.29, 3.50–5.21, p < 0.001) were also significantly associated with food security status. Significant effect modification was indicated between presence of mood disorder with cannabis use (0.64, 95% CI 0.43–0.94, p = 0.022), hallucinogen use (0.64, 95% CI 0.41–0.98, p = 0.041), ecstasy use (0.57, 95% CI 0.33–0.97, p = 0.037), and any lifetime substance use (0.51, 95% CI 0.35–0.76, p<0.001) in relation to food insecurity. The goodness-of-fit chi-squared test results were not significant for all final models suggesting that the Poisson model forms fit the data.
Table 2. Poisson regression results for food insecurity, mood disorder, and substance—full and reduced models.
| Variable (baseline) | Full Model | Reduced Model | ||
|---|---|---|---|---|
| Prevalence Ratio (95% CI) | p-value | Prevalence Ratio (95% CI) | p-value | |
| Marijuana, cannabis or hashish (more than once) | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.68 (1.93–3.70) | <0.001 | 2.59 (1.89–3.55) | <0.001 |
| Substance (no lifetime use) | 2.42 (1.57–3.75) | <0.001 | 1.95 (1.59–2.40) | <0.001 |
| Sex (male) | 1.16 (0.89–1.52) | 0.277 | 0.92 (0.77–1.12) | 0.414 |
| Age (12 to 18 years) | 0.82 (0.77–0.88) | <0.001 | 0.82 (0.78–0.87) | <0.001 |
| Relationship (single) | 1.58 (1.26–1.97) | <0.001 | 1.55 (1.24–1.95) | <0.001 |
| Education (no high school) | 1.74 (1.39–2.18) | <0.001 | 1.71 (1.37–2.14) | <0.001 |
| Income (low) | 4.87 (3.50–6.79) | <0.001 | 4.41 (3.61–5.39) | <0.001 |
| Substance x mood disorder | 0.61 (0.40–0.92) | 0.019 | 0.64 (0.43–0.94) | 0.022 |
| Cocaine or crack | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.33 (1.82–2.99) | <0.001 | 2.02 (1.64–2.49) | <0.001 |
| Substance (no lifetime use) | 2.29 (1.30–4.01) | 0.004 | 1.68 (1.33–2.12) | <0.001 |
| Sex (male) | 0.99 (0.80–1.22) | 0.930 | 0.94 (0.78–1.13) | 0.512 |
| Age (12 to 18 years) | 0.81 (0.77–0.86) | <0.001 | 0.81 (0.77–0.85) | <0.001 |
| Relationship (single) | 1.53 (1.22–1.92) | <0.001 | 1.53 (1.22–1.92) | <0.001 |
| Education (no high school) | 1.64 (1.32–2.05) | <0.001 | 1.62 (1.30–2.01) | <0.001 |
| Income (low) | 4.56 (3.59–5.80) | <0.001 | 4.29 (3.53–5.22) | <0.001 |
| Substance x mood disorder | 0.67 (0.43–1.06) | 0.084 | — | — |
| Speed (amphetamines) | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.23 (1.79–2.78) | <0.001 | 2.13 (1.75–2.59) | <0.001 |
| Substance (no lifetime use) | 2.48 (1.14–5.37) | 0.022 | 1.67 (1.29–2.17) | <0.001 |
| Sex (male) | 0.97 (0.79–1.18) | 0.748 | 0.96 (0.80–1.15) | 0.635 |
| Age (12 to 18 years) | 0.81 (0.77–0.85) | <0.001 | 0.81 (0.77–0.85) | <0.001 |
| Relationship (single) | 1.54 (1.23–1.92) | <0.001 | 1.54 (1.23–1.93) | <0.001 |
| Education (no high school) | 1.64 (1.31–2.06) | <0.001 | 1.63 (1.30–2.04) | <0.001 |
| Income (low) | 4.40 (3.56–5.45) | <0.001 | 4.27 (3.50–5.21) | <0.001 |
| Substance x mood disorder | 0.77 (0.44–1.36) | 0.371 | — | — |
| Ecstasy (3,4-methylenedioxy-methamphetamine; MDMA) or other similar drugs | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.43 (1.98–2.99) | <0.001 | 2.43 (1.97–2.98) | <0.001 |
| Substance (no lifetime use) | 2.12 (1.23–3.64) | 0.007 | 2.83 (1.99–4.02) | <0.001 |
| Sex (male) | 0.95 (0.78–1.16) | 0.617 | 0.96 (0.80–1.15) | 0.679 |
| Age (12 to 18 years) | 0.82 (0.78–0.87) | <0.001 | 0.83 (0.79–0.87) | <0.001 |
| Relationship (single) | 1.51 (1.21–1.89) | <0.001 | 1.51 (1.21–1.89) | <0.001 |
| Education (no high school) | 1.62 (1.30–2.03) | <0.001 | 1.62 (1.30–2.03) | <0.001 |
| Income (low) | 4.84 (3.86–6.07) | <0.001 | 4.86 (3.87–6.09) | <0.001 |
| Substance x mood disorder | 0.53 (0.30–0.93) | 0.027 | 0.57 (0.33–0.97) | 0.037 |
| Hallucinogens, PCP (phencyclidine), or LSD (lysergic acid diethylamide; acid) | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.37 (1.90–2.96) | <0.001 | 2.36 (1.90–2.94) | <0.001 |
| Substance (no lifetime use) | 3.56 (2.07–6.12) | <0.001 | 2.40 (1.81–3.16) | <0.001 |
| Sex (male) | 0.98 (0.80–1.21) | 0.861 | 0.94 (0.78–1.13) | 0.501 |
| Age (12 to 18 years) | 0.82 (0.78–0.86) | <0.001 | 0.81 (0.77–0.85) | <0.001 |
| Relationship (single) | 1.57 (1.26–1.97) | <0.001 | 1.56 (1.25–1.95) | <0.001 |
| Education (no high school) | 1.64 (1.32–2.06) | <0.001 | 1.66 (1.33–2.08) | <0.001 |
| Income (low) | 4.66 (3.69–5.88) | <0.001 | 4.64 (3.68–5.84) | <0.001 |
| Substance x mood disorder | 0.64 (0.42–0.99) | 0.043 | 0.64 (0.41–0.98) | 0.041 |
| Use of any substance over the lifetime (n = 13445) | ||||
| Mood disorder (not diagnosed in previous 12 months) | 2.94 (2.11–4.11) | <0.001 | 2.98 (2.16–4.12) | <0.001 |
| Substance (no lifetime use) | 2.63 (1.71–4.05) | <0.001 | 2.48 (1.91–3.23) | <0.001 |
| Sex (male) | 1.18 (0.90–1.55) | 0.231 | 1.18 (0.90–1.55) | 0.237 |
| Age (12 to 18 years) | 0.83 (0.78–0.88) | <0.001 | 0.83 (0.79–0.87) | <0.001 |
| Relationship (single) | 1.57 (1.26–1.96) | <0.001 | 1.56 (1.25–1.96) | <0.001 |
| Education (no high school) | 1.75 (1.39–2.19) | <0.001 | 1.76 (1.40–2.20) | <0.001 |
| Income (low) | 4.84 (3.45–6.78) | <0.001 | 4.32 (3.54–5.28) | <0.001 |
| Substance x mood disorder | 0.54 (0.35–0.81) | 0.003 | 0.51 (0.35–0.76) | <0.001 |
Discussion
Significant effect modification was found between recent mood disorder diagnosis and lifetime use of cannabis, hallucinogens, ecstasy, and any substance use over the lifetime in relationship with food insecurity were found; all of these PRs were less than the null value. Conversely, independent associations were found for crack/cocaine and speed use. Several correlates, such as age, education, and income were also significantly associated with food insecurity. These results help illustrate how effect modification analyses may highlight potential early indicators of vulnerability to food insecurity [43].
Interestingly, the significant findings for effect modification appear to suggest that lifetime use of cannibis, hallucinogens, or ecstasy was protective against recent mood disorder diagnosis and food insecurity. The explanation for this relationship is not readily apparent. Prior studies have not reported results about effect modification of substance use and mental health in which comparisons can be made. It is possible that survey respondents may have used substances infrequently (e.g., experimented) and their effects were non-existent or minimal. Data about frequency and amount of use of the substances and their relationship with mental health and food insecurity would help ascertain the accuracy of this assumption. Other research has suggested effect modification occurs with age when examining associations between mental health and substance use [44] suggesting that future study should focus on effects specific to adolesence, young adulthood, and adulthood.
While this investigation suggests exposure to substance use and/or poor mental health are associated with food insecurity, there are potentially multiple directions of association among these variables. As previously indicated in the introduction, relationships among food insecurity, mental health, and substance use (Fig 1) may be due to independent or synergistic effects of various nutrition, mental health, and behavioural pathways [9, 45]. Structural level drivers that include ecological (e.g., food environments), economic (e.g., income), and social factors (e.g., stigma) may intersect with these pathways [46]. The trajectories and final outcomes depend on one’s coping and resilience [7, 47, 48]. For example, food insecurity can contribute to over nutrition (overweight, obesity), and under nutrition (protein and energy deficiencies), nutrient excesses and disproportions, eating disturbances, micronutrient deficiencies, and alterations in the gut-microbiota-brain axis [49–52] which can compromise nutritional and mental health [4]. Nutritional status may be further undermined due to drug (e.g., substance, psychiatric medication) and nutrition interactions, [29, 53], eating disturbances (e.g., fasting to heighten drug effects) [54, 55], and imbalances in metabolic responses [56, 57]. Conversely, mental health pathways such as diathesis–stress may explain how predispositional vulnerability to poor mental health may be triggered by environmental influences (e.g., stressors such as food insecurity) [58] leading to subsequent substance use. Furthermore, mental ill health may heighten a substance’s effects due to “supersensitivity” [59] and lead to sustained drug use as mental health problems persist with continued substance use and continued substance use alleviate psychiatric symptoms [37]. To explore this investigation’s findings further, relevant literature related to the five substances studied is highlighted.
Effect modification: Mood disorder and substances
Effect modification between mood disorder and cannabis may be explained by the self medication hypothesis. Cannabinoid effects include euphoria and therefore may be used as a means to control symptoms of a mood disorder. However, experimental studies have shown association between the psychoactive component delta-9-tetrahydrocannabinol, psychosis and schizophrenia-like symptoms [60, 61]. Evidence from prospective studies suggest a causal link between cannabis use and psychosis in some individuals that are genetically vulnerable [62, 63].
Cannabis use stimulates appetite and can increase caloric intake by 40% [64]. This creates greater demands for food intake which can heighten food insecurity. Hallucinogens, such as LSD and PCP, and stimulants such as MDMA can produce substantial anorexia which may change the perception of hunger [65]. In other words, the conditions leading to food insecurity may not have changed, but the altered state brought on by the substance has changed an individual’s perception of this state. The use of hallucinogens may trigger onset of psychosis [37] and worsen mental health [66] through mechanisms such as altered glutamatergic neurotransmission [67] which may perpetuate substance use. Some individuals that use MDMA heavily experience long-lasting depression [68].
Independent effects: Crack/cocaine or speed (methamphetamine)
Cocaine suppresses appetite and contributes to eating disturbances [37]. ‘Drug binges’–patterns of intense drug use often lasting for days at a time during which food, sleep, and basic hygiene are neglected–are common among users of stimulant drugs and significantly affect dietary intake [69, 70]. Cocaine use is associated with alterations in food cues, eating disorders, and compulsive overeating [71]; all factors that impact on food security. For those who inject cocaine, elevated risks of infectious diseases, violence, victimization, overdose, mental health problems, poverty, incarceration, and sex trade involvement [72] have been found; all of these factors also interfere with stable access to food.
The findings that speed and mood disorders did not have significant interaction effects were surprising. Among regular amphetamine users, high rates of mental health problems such as psychosis have been found [73] and studies have shown bi-directional association. There may be a peripheral association between amphetamine use and food insecurity as some methamphetamine users lose their teeth from a condition known as meth mouth [74, 75]. This is a result of drug-induced psychological and physiological changes that lead to xerostomia, poor oral hygiene, frequent consumption of high-calorie, carbonated beverages, as well as teeth grinding and clenching [76] which can present barriers to healthy food intake.
Study limitations
This study provided the opportunity to analyze a large representative population sample and present novel findings related to independent and synergistic associations between mood disorders and substance use in relation to food insecurity. However the findings are limited by the use of a cross-sectional design, insufficient details about substance use (e.g., dose, frequency, drug purity, routes of administration, period of life when substance used) and the measurement of household level food insecurity which cannot account for intra-household variations. Some households with food insecurity, which can include poor access to healthy foods even if they have access to enough food for energy and satiety needs, may have been screened out which could lead to underestimation of food insecurity. Although measuring for substances such as solvents, steroids and heroin and accounting for polysubstance use would have also been informative, the frequencies were too low in this sample to enable these types of analyses. Furthermore, caution must be used to avoid conflating being diagnosed with a mood disorder with having a mood disorder, as undiagnosed mental health problems may be very common. The results are specific to the province of British Columbia but may not be generalizeable to other settings (including populations in British Columbia not included in the sample). All data collected were self-reported and vulnerable to biases such as recall and social desirability. Finally, any other potentially important confounders could not be controlled for.
Conclusions
The results of this study suggest that substance use and poor mental health are potential independent or interdependent factors that contribute to food insecurity. By tailoring prevention and intervention efforts, such as screening for the significant correlates reported in this study, strides may be made to alleviate the preventable public health issue of food insecurity. The results of some of the associations with food insecurity are difficult to interpret (e.g., potential potective effect of lifetime substance use related to food insecurity) and require further study. The conceptual framework (Fig 1) suggests that coping and resilience are underlying features that warrant further investigation as potential explanatory mechanisms that could mediate or moderate food insecurity, substance use, and mental ill health in the context of different macro-level drivers and mental health, nutrition, and behavioural pathways. Longitudinal research and further investigations of coping and resilience may discern explanatory mechanisms that could mediate or moderate substance use, poor mental health, and food insecurity. Finally, customized intervention research can help determine effective ways to reduce substance use, poor mental health, and food insecurity.
Acknowledgments
This study was part of Karen Davison’s postdoctoral work funded by the Canadian Institues for Health Research’s Intersections of Mental Health Perspectives in Addictions Research Training Program. Gratitude is extended to Catherine (Katie) Goldie, Brittany Bingham, and Alina Sotskova for their early work on this project that included submitting the proposal to Statistics Canada and initial data analysis.
Data Availability
Data is secured by Statistics Canada and permission to share data publicly cannot be granted as it might compromise patient confidentiality or participant privacy. The Canadian Community Health Survey data for this analysis was collected by Statistics Canada (third party data). Details about how to access Statistics Canada data are available at: https://www.statcan.gc.ca/eng/rdc/index. Researchers who have been sworn in as "deemed employees" of Statistics Canada can access the confidential microdata files for approved projects through Statistics Canada’s Research Data Centres (RDCs). The confidential microdata files contain information collected during the survey, derived variables, and the Bootstrap weights used to calculate the exact variance.
Funding Statement
KMD's work was supported by a Canadian Institutes of Health Research Intersections of Mental Health Perspectives in Addictions Research Training (IMPART) postdoctoral fellowship.
References
- 1.Davis B, Tarasuk V. Hunger in Canada. Agriculture and Human Values 1994;11(4):50–57. [Google Scholar]
- 2.Strike C, Rudzinski K, Patterson J, Millson M. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health. 2012;12:1058 doi: 10.1186/1471-2458-12-1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weaver LJ, Hadley C. Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr. 2009;48(4): 263–284. doi: 10.1080/03670240903001167 [DOI] [PubMed] [Google Scholar]
- 4.Davison KM, Kaplan BJ. Food insecurity in adults with mood disorders: prevalence estimates and associations with nutritional and psychological health. Ann Gen Psychiatry. 2015;14: 21 doi: 10.1186/s12991-015-0059-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davison KM, Marshall-Fabien GL, Tecson A. Association of moderate and severe food insecurity with suicidal ideation in adults: national survey data from three Canadian provinces. Soc Psychiatry Psychiatr Epidemiol. 2015;50(6):963–972. doi: 10.1007/s00127-015-1018-1 [DOI] [PubMed] [Google Scholar]
- 6.Slopen N, Fitzmaurice G, Williams DR, Gilman SE. Poverty, food insecurity, and the behavior for childhood internalizing and externalizing disorders. J Am Acad Child Adolesc Psychiatry. 2010;49(5):444–452. [DOI] [PubMed] [Google Scholar]
- 7.Huddleston-Casas C, Charigo R, Simmons LA. Food insecurity and maternal depression in rural, low-income families: A longitudinal investigation. Public Health Nutr. 2008;12(8): 1133–1140. doi: 10.1017/S1368980008003650 [DOI] [PubMed] [Google Scholar]
- 8.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, et al. Household food insecurity is associated with adult health status. J Nutr. 2004;134:2330–2335. [DOI] [PubMed] [Google Scholar]
- 9.Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):S1729–S1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melchior M, Caspi A, Howard LM, Ambler AP, Bolton H, Mountain N, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124(4):e564–e572. doi: 10.1542/peds.2009-0583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chilton M, Booth S. Hunger of the body and hunger of the mind: African American women's perceptions of food insecurity, health and violence. J Nutr Educ Behav. 2007;39:116–125. doi: 10.1016/j.jneb.2006.11.005 [DOI] [PubMed] [Google Scholar]
- 12.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171–86. doi: 10.1177/002214650404500204 [DOI] [PubMed] [Google Scholar]
- 13.Hamelin AM, Hamel D. Food insufficiency in currently or formerly homeless persons is associated with poorer health. Can J Urban Res. 2009;18:1–24. [Google Scholar]
- 14.Hendricks KM, Erzen HD, Wanke CA, Tang AM. Nutrition issues in the HIV-infected injection drug user: findings from the nutrition for healthy living cohort. J Am Coll Nutr. 2010;29:136–143. [DOI] [PubMed] [Google Scholar]
- 15.Saeland M, Haugen M, Eriksen FL, Wandel M, Smehaugen A, Böhmer T, et al. High sugar consumption and poor nutrient intake among drug addicts in Oslo, Norway. Br J Nutr. 2011;105:618–624. doi: 10.1017/S0007114510003971 [DOI] [PubMed] [Google Scholar]
- 16.Tang AM, Bhatnagar T, Ramachandran R, Dong K, Skinner S, Kumar MS, et al. Malnutrition in a population of HIV-positive and HIV-negative drug users living in Chennai, South India. Drug Alcohol Depend. 2011;118:73–77. doi: 10.1016/j.drugalcdep.2011.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang AM, Forrester JE, Spiegelman D, Flanigan T, Dobs A, Skinner S, et al. Heavy injection drug use is associated with lower percent body fat in a multi-ethnic cohort of HIV-positive and HIV-negative drug users from three U.S. cities. Am J Drug Alcohol Abuse. 2010;36:78–86. doi: 10.3109/00952990903544851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vogenthaler NS, Hadley C, Lewis SJ, Rodriguez AE, Metsch LR, del Rio C. Food insufficiency among HIV-infected crack-cocaine users in Atlanta and Miami. Public Health Nutr. 2010;13:1478–1484. doi: 10.1017/S1368980009993181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawrelak JA, Myers SP. The causes of intestinal dysbiosis: A review. Altern Med Review. 2004;9:180–197. [PubMed] [Google Scholar]
- 20.Gelberg L, Stein JA, Neumann CG. Determinants of undernutrition among homeless adults. Public Health Rep. 1995;110:448–54. [PMC free article] [PubMed] [Google Scholar]
- 21.Kraybill K, Zerger S. Providing Treatment for Homeless People With Substance Use Disorders: Case Studies of Six Programs. Nashville, USA: National Care for the Homeless Council, 2003. [Google Scholar]
- 22.Santolaria-Fernández FJ, Gómez-Sirvent JL, González-Reimers CE, Batista-López JN, Jorge-Hernández JA, Rodríguez-Moreno F, et al. Nutritional assessment of drug addicts. Drug Alcohol Depend. 1995;38(1):11–18. [DOI] [PubMed] [Google Scholar]
- 23.Wiecha JL, Dwyer JT, Dunn-Strohecker M. Nutrition and health services needs among the homeless. Public Health Rep. 1991;106:364–74. [PMC free article] [PubMed] [Google Scholar]
- 24.Heslin KC, Andersen RM, Gelberg L. Case management and access to services for homeless women. J Health Care Poor Underserved. 2003;14:34–51. [PubMed] [Google Scholar]
- 25.Coelho JS, Polivy J, Herman CP. Selective carbohydrate or protein restriction: effects on subsequent food intake and cravings. Appetite 2006;47:352–360. doi: 10.1016/j.appet.2006.05.015 [DOI] [PubMed] [Google Scholar]
- 26.Heller J, Edelmann RJ. Compliance with a low calorie diet for two weeks and concurrent and subsequent mood changes. Appetite. 1991;17:23–28. [DOI] [PubMed] [Google Scholar]
- 27.Liu X, Tein JY. Life events, psychopathology, and suicidal behavior in Chinese adolescents. J Affect Dis. 2005;86:195–203. doi: 10.1016/j.jad.2005.01.016 [DOI] [PubMed] [Google Scholar]
- 28.Polivy J. Psychological consequences of food restriction. J Am Diet Assoc. 1996;96: 589–592. doi: 10.1016/S0002-8223(96)00161-7 [DOI] [PubMed] [Google Scholar]
- 29.Davison KM, Cairns J, Selly C, Ng E, Chandrasekera U, Sengmueller E, et al. The Role of Nutrition Care for Mental Health Conditions (Paper 2). Toronto, Canada: Dietitians of Canada, 2012. [Google Scholar]
- 30.Heflin CM, Siefert K, Williams DR. Food insufficiency and women's mental health: Findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005;61(9):1971–1982. doi: 10.1016/j.socscimed.2005.04.014 [DOI] [PubMed] [Google Scholar]
- 31.Runnels VE, Kristjansson E, Calhoun M. An investigation of adults' everyday experiences and effects of food insecurity in an urban area in Canada. Can J Commun Ment Health. 2011;30(1):157–172. [Google Scholar]
- 32.Tarasuk V, Fitzpatrick S, Ward H. (2010) Nutrition inequities in Canada. Appl Physiol Nutr Metab. 35(2): 172–179. doi: 10.1139/H10-002 [DOI] [PubMed] [Google Scholar]
- 33.Broussard CA. Research regarding low-income single mothers' mental and physical health: a decade in review. J Poverty. 2010;14(4):443–51. [Google Scholar]
- 34.Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophrenia Bulletin. 2000;26:105–118. [DOI] [PubMed] [Google Scholar]
- 35.Canadian Centre on Substance Abuse. Substance abuse in Canada: concurrent disorders. Ottawa, Canada: Canadian Centre on Substance Abuse, 2009. [Google Scholar]
- 36.Alaimo K, Olson CM, Frongillo EA Jr. Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. J Nutr. 2002;132:719–725. [DOI] [PubMed] [Google Scholar]
- 37.Gregg L, Barrowclough C, Haddock G. Reasons for increased substance use in psychosis. Clin Psychol Rev. 2007;27(4):494–510. doi: 10.1016/j.cpr.2006.09.004 [DOI] [PubMed] [Google Scholar]
- 38.Statistics Canada, Health Statistics Division. Canadian community health survey, cycle 4.1, 2007 Synthetic edition Ottawa, Canada: Statistics Canada, 2008. http://data.library.utoronto.ca/microdata/canadian-community-health-survey-cycle-41-2007-synthetic-edition. Accessed July 2015 [Google Scholar]
- 39.Health Canada. The Household Food Security Survey Module (HFSSM). Ottawa, Canada: Health Canada, 2012. http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/insecurit/hfssm-mesam-eng.php. Accessed July 2015 [Google Scholar]
- 40.Statistics Canada, Health Statistics Division. Canadian community health survey, cycle 4.1, 2007 Synthetic edition Ottawa, Canada: Statistics Canada, 2008. http://data.library.utoronto.ca/microdata/canadian-community-health-survey-cycle-41-2007-synthetic-edition. Accessed July 2015 [Google Scholar]
- 41.StataCorp. Stata Statistical Software: Release 11. College Station, USA: StataCorp LP, 2009. [Google Scholar]
- 42.Statistics Canada. Canadian Community Health Survey—Annual Component (CCHS). Ottawa, Canada: Statistics Canada, 2015. http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226. Accessed July 2015 [Google Scholar]
- 43.Hammond RA, Dubé L. A systems science perspective and transdisciplinary models for food and nutrition security. Proc Natl Acad Sci U S A. 2012; 109(31):12356–63. doi: 10.1073/pnas.0913003109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pryor L, Lioret S, van der Waerden J, Fombonne É, Falissard B, Melchior M. Food insecurity and mental health problems among a community sample of young adults. Soc Psychiatry Psychiatr Epidemiol. 2016; 51(8):1073–81. doi: 10.1007/s00127-016-1249-9 [DOI] [PubMed] [Google Scholar]
- 45.Hadley C, Crooks DL. Coping and the biosocial consequences of food insecurity in the 21st century. Am J Phys Anthropol. 2012;149 Suppl 55:72–94. [DOI] [PubMed] [Google Scholar]
- 46.Logan AC, Jacka FN. Nutritional psychiatry research: an emerging discipline and its intersection with global urbanization, environmental challenges and the evolutionary mismatch. J Physiol Anthropol. 2014;33:22 doi: 10.1186/1880-6805-33-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tarasuk V, Mah C. Household Food Insecurity in Canada—An Update From the PROOF Research Project. Ottawa, Canada: Food Secure Canada, 2012. http://foodsecurecanada.org/resources-news/webinars-podcasts/household-food-insecurity-canada#sthash.Az9XgAka.dpuf. Accessed July 2015 [Google Scholar]
- 48.Brown DR, Brewster LG. (2015) The food environment is a complex social network. Soc Sci Med. 133: 202–204. doi: 10.1016/j.socscimed.2015.03.058 [DOI] [PubMed] [Google Scholar]
- 49.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. [DOI] [PubMed] [Google Scholar]
- 50.Bove CF, Olson CM. Obesity in low-income rural women: qualitative insights about physical activity and eating patterns. Women Health. 2006;44(1):57–78. doi: 10.1300/J013v44n01_04 [DOI] [PubMed] [Google Scholar]
- 51.Petra AI, Panagiotidou S, Hatziagelaki E, Stewart JM, Conti P, Theoharides TC. Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther. 2015;37(5):984–995. doi: 10.1016/j.clinthera.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davison KM, Kaplan BJ. Vitamin and mineral intakes in adults with mood disorders: Comparisons to nutrition standards and associations with sociodemographic and clinical variables. J Am Coll Nutr. 2011;30(6):547–558. [DOI] [PubMed] [Google Scholar]
- 53.Davison KM, Kaplan BJ. Nutrient- and non-nutrient-based natural health product (NHP) use in adults with mood disorders: prevalence, characteristics and potential for exposure to adverse events. BMC Complement Altern Med. 2013;13:80 doi: 10.1186/1472-6882-13-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hatcher AS. Nutrition and Addictions: A Guide for Professionals. Chicago, USA: American Dietetic Association, 2008. [Google Scholar]
- 55.Davison KM, Marshall-Fabien GL, Gondara L. Sex differences and eating disorder risk among psychiatric conditions, compulsive behaviors and substance use in a screened Canadian national sample. Gen Hosp Psychiatry. 2014;36(4):411–414. doi: 10.1016/j.genhosppsych.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 56.Maes M, Kubera M, Leunis JC, Berk M, Geffard M, Bosmans E. In depression, bacterial translocation may drive inflammatory responses, oxidative and nitrosative stress (O&NS), and autoimmune responses directed against O&NS-damaged neoepitopes. Acta Psychiatr Scand. 2013;127(5): 344–354. doi: 10.1111/j.1600-0447.2012.01908.x [DOI] [PubMed] [Google Scholar]
- 57.Volpe GE, Ward H, Mwamburi M, Dinh D, Bhalchandra S, Wanke C, et al. Associations of cocaine use and HIV infection with the intestinal microbiota, microbial translocation, and inflammation. J Stud Alcohol Drugs. 2014;75(2):347–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ingram RE, Luxton D. Vulnerability-stress models In: Hankin BL & Abela JRZ (Eds.). Development of psychopathology: A vulnerability-stress perspective. New York, USA: Sage, 2005. [Google Scholar]
- 59.Agrawal A, Lynskey MT. Are there genetic influences on addiction: evidence from family, adoption and twin studies. Addiction. 2008;103(7):1069–1081. doi: 10.1111/j.1360-0443.2008.02213.x [DOI] [PubMed] [Google Scholar]
- 60.Cortes-Briones JA, Cahill JD, Skosnik PD, Mathalon DH, Williams A, Sewell RA, et al. The psychosis-like effects of delta-9-tetrahydrocannabinol are associated with increased cortical noise in healthy humans. Biol Psychiatry. 2015;78:805–13. doi: 10.1016/j.biopsych.2015.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weiser M, Noy S. Interpreting the association between cannabis use and increased risk for schizophrenia. Dialogues Clin Neurosci. 2005;7:81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pelayo-Terán JM, Pérez-Iglesias R, Mata I, Carrasco-Marín E, Vázquez-Barquero JL, Crespo-Facorro B. Catechol-O-Methyltransferase (COMT) Val158Met variations and cannabis use in first-episode non-affective psychosis: clinical-onset implications. Psychiatry Res. 2010;179;291–296. doi: 10.1016/j.psychres.2009.08.022 [DOI] [PubMed] [Google Scholar]
- 63.Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry. 2005;57:1117–1127. doi: 10.1016/j.biopsych.2005.01.026 [DOI] [PubMed] [Google Scholar]
- 64.Foltin RW, Fischman MW, Byrne MF. Effects of smoked marijuana on food intake and body weight of humans living in a residential laboratory. Appetite. 1988;11(1):1–14. [DOI] [PubMed] [Google Scholar]
- 65.Yago KB, Pitts FN Jr, Burgoyne RW, Aniline O, Yago LS, Pitts AF. The urban epidemic of phencyclidine (PCP) use: Clinical and laboratory evidence from a public psychiatric hospital emergency service. J Clin Psychiatry. 1981;42:193–196. [PubMed] [Google Scholar]
- 66.Baker A, Lee NK, Claire M, Lewin TJ, Grant T, Pohlman S, et al. Drug use patterns and mental health of regular amphetamine users during a reported 'heroin drought'. Addiction. 2004;99(7):875–84. doi: 10.1111/j.1360-0443.2004.00741.x [DOI] [PubMed] [Google Scholar]
- 67.Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62:63–77. doi: 10.1016/j.neuropharm.2011.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tracy JI., Josiassen RC, Bellack AS. Neuropsychology of dual diagnosis: Understanding the combined effects of schizophrenia and substance use disorders. Clin Psychol Rev. 1995;15:67–97. [Google Scholar]
- 69.Cornish JW, O'Brien CP. Crack cocaine abuse: an epidemic with many public health consequences. Annu Rev Public Health. 1996;17:259–273. doi: 10.1146/annurev.pu.17.050196.001355 [DOI] [PubMed] [Google Scholar]
- 70.Tomasi D, Wang GJ, Wang R, Caparelli EC, Logan J, Volkow ND. Overlapping patterns of brain activation to food and cocaine cues in cocaine abusers: association to striatal D2/D3 receptors. Hum Brain Mapp 2015;36:120–136. doi: 10.1002/hbm.22617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.American Dietetic Association & Dietitians of Canada. Manual of Clinical Dietetics. Chicago, USA: Author, 2000. [Google Scholar]
- 72.Anema A, Wood E, Weiser SD, Qi J, Montaner JS, Kerr T. Hunger and associated harms among injection drug users in an urban Canadian setting. Subst Abus Treat Prev Policy. 2010;5:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hart CL, Marvin CB, Silver R, Smith EE. Is cognitive functioning impaired in methamphetamine users? A critical review. Neuropsychopharmacology 2012;37(3):586–608. doi: 10.1038/npp.2011.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hussain F, Frare RW, Py Berrios KL. Drug abuse identification and pain management in dental patients: a case study and literature review. Gen Dent. 2012;60:334–345. [PubMed] [Google Scholar]
- 75.Muirhead V, Quiñonez C, Figueiredo R, Locker D. Oral health disparities and food insecurity in working poor Canadians. Community Dent Oral Epidemiol. 2009;7:294–304. [DOI] [PubMed] [Google Scholar]
- 76.American Dental Association. Methamphetamine Use (Meth Mouth). Chicago, IL: American Dental Association, 2008. http://web.archive.org/web/20080601035323/http://www.ada.org/prof/resources/topics/methmouth.asp. Accessed July 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is secured by Statistics Canada and permission to share data publicly cannot be granted as it might compromise patient confidentiality or participant privacy. The Canadian Community Health Survey data for this analysis was collected by Statistics Canada (third party data). Details about how to access Statistics Canada data are available at: https://www.statcan.gc.ca/eng/rdc/index. Researchers who have been sworn in as "deemed employees" of Statistics Canada can access the confidential microdata files for approved projects through Statistics Canada’s Research Data Centres (RDCs). The confidential microdata files contain information collected during the survey, derived variables, and the Bootstrap weights used to calculate the exact variance.