Abstract
We assessed the frailty status of inpatients and analyzed the factors influencing frailty status to explore the reasons for frailty and identify feasible intervention strategies.
A total of 1494 geriatric patients aged ≥60 years were recruited as subjects. All patients were hospitalized between September 2014 and August 2015 in the internal medicine units of 3 hospitals in Chongqing and Zunyi in the southwestern area of China. Patients’ frailty status was evaluated using the Phenotype of Frailty scale, via face-to-face interviews coupled with physical examinations using simple equipment.
Of the 1494 cases, 1400 (93.71%) were eligible for analysis. Participants’ mean age was 75.52 ± 9.28 years. The overall prevalence of frailty was 18.0%, and was higher for frail females (9.4%) than males (8.6%). Increasing age and body mass index, low income (<1000 Ren Min Bi for per month), poor self-rated health, cognitive impairment, depression, polypharmacy (≥5 medications), disability, and a history of fall in the past 1 year were independently significantly correlated with frailty (P < .05 for each comparison).
Numerous factors were associated with frailty. As treatment for frailty is focused on prevention in this study, intervention strategies should target a comprehensive list of physiological and psychological aspects of the older people.
Keywords: evaluation, frailty, hospital, influencing factors, old people
1. Introduction
The global population is rapidly aging, the number of the elderly people in the world has reached 629 million. Increasing age and aging are related to body function decline and the risk of adverse outcomes. It is difficult to distinguish the difference “disease and health,” and the older adults are often in the status “neither disability nor health.” How to realize and prevent the adverse events as early as possible? The concept of frailty increasingly attracts the attention of the researchers and clinical workers in recent years, is becoming a hot point in the field of gerontology. The academic community has not settled on a unified clinical definition for frailty.[1] While frailty can be narrowly defined as “physiological function decrease,” this merely provides a 1-dimensional understanding of the condition; a more general and multidimensional definition of frailty would help emphasize its impacts on the overall body. Accordingly, one can define it as a decline in the reserve capacity of multiple body systems and physical degeneration.[2]
Frailty can occur as the result of a range of chronic diseases and acute reactions or medical conditions, and is not synonymous with any specific pathological state or disability; frailty could be reversed through intervention. Indeed, the term “frailty” is often used to describe the chronic health problems experienced by elderly adults aged 65 years old or older, and it is particularly common among those over the age of 80.[3,4] Frailty can severely affect work and quality of life, as well as increase social and family burden.
International scholars have recently begun focusing on the development of a frailty theory. In December 2012, the concept of frailty was “re-opened” for discussion.[5] The experts concluded at that time that frailty is a complex medical syndrome with multiple causes and contributors that is mainly characterized by reduced strength and endurance, reduced physiological function that increases an individual's vulnerability for developing increased dependency and/or death, and can be reversed or attenuated through appropriate intervention. It is recommended that all elderly aged 70 years old and above be routinely assessed for frailty.
As a result of research on frailty and its related influencing factors, some evaluation tools with better validity and reliability have been developed, for example, Phenotype of Frailty (FP)[6,7]; Study of Osteoporotic Fractures[8,9]; Frailty Index[10,11]; Frailty Instrument of the Survey of Health, Ageing and Retirement in Europe[12,13]; Tilburg Frailty Index[14,15]; Groningen Frailty Indicator [16,17]; etc.
In comparison to other developed countries, frailty research commenced at a later stage, the subjects of few studies were mainly community-dwelling geriatric populations in China.[18–22] This study was to focus on the frailty status of inpatients aged 60 years old or over and analyze the influencing factors and reasons of frailty by FP instrument.
2. Materials and methods
2.1. Data and participants
The study received approval from the Human Research Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University, Chongqing, China (No. 71, 2014). All recruited patients signed an informed consent.
This was a cross-sectional study, and stratified random samples were used to recruit geriatric inpatients from the internal medicine units of 3 general hospitals in Chongqing and Zunyi from September 2014 to August 2015. These hospitals were the Second Affiliated Hospital of Chongqing Medical University, the First People's Hospital of Zunyi, and the Aerospace Hospital of Guizhou in southwestern area of China.
Geriatric patients who met the following criteria were included in this study: ≥60 years old; able to communicate and did not have severe cognitive impairment or psychiatric illness; had the consent of themselves and their families; and voluntarily agreed to participate. A total of 1494 patients (aged ≥60 years old) were recruited. After excluding those who refused participation (n = 32, 2.14%), who had communication impairments or seriously illness (n = 20, 1.34%), and who had missing data (n = 42, 2.81%), a total of 1400 patients were ultimately recruited and analyzed (valid response rate: 93.71%; Fig. 1).
Figure 1.
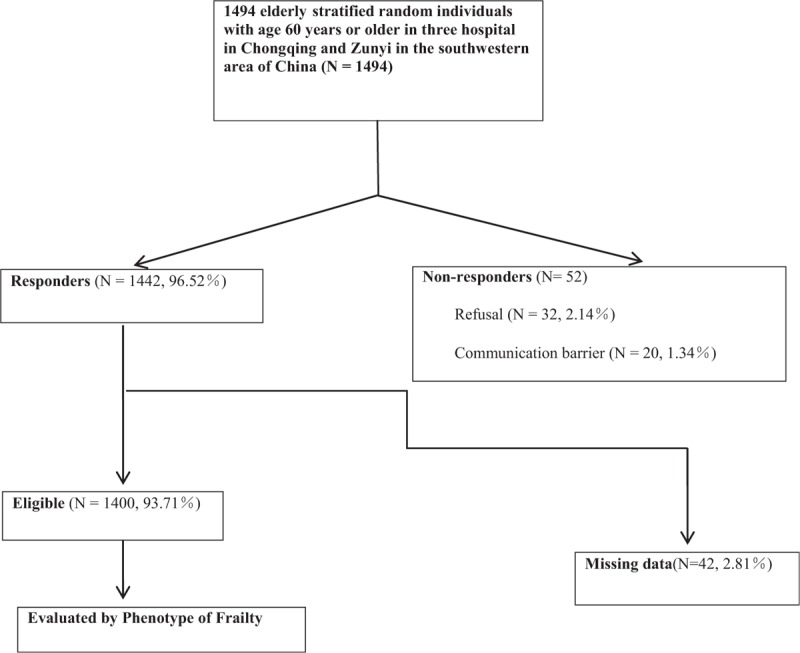
Flowchart for patient survey.
2.2. Study design
The evaluation instrument of frailty was the FP scale. Patients’ frailty status was assessed using a questionnaire administered in a face-to-face interview by trained staffs in the first 48 h of inpatients admission, along with a physical examination (which included measurements of blood pressure, heart rate, height, and weight) using simple detection equipment.
2.3. Baseline characteristics
The questionnaire included general demographic information (e.g., age, sex, educational level, marital status), degree of family and social support (e.g., whether one is living alone, relationship status with family, main monthly income, main social activities), disease status (e.g., main diseases, medication compliance, types of taking medications), and personal habits (e.g., smoking history, drinking history, etc.).
We then entered factors that might be related to frailty into a univariate analysis. The specific indicators included gender, education level, marital status, income level, smoking, drinking, history of hospitalization, and a fall in the past 1 year, duration of hospitalization, cognitive impairment, depression, disability, comorbidity, polypharmacy, poor self-rated health, age, and body mass index (BMI) (note that these latter 2 variables were treated as continuous variables; see Table 1 for details).
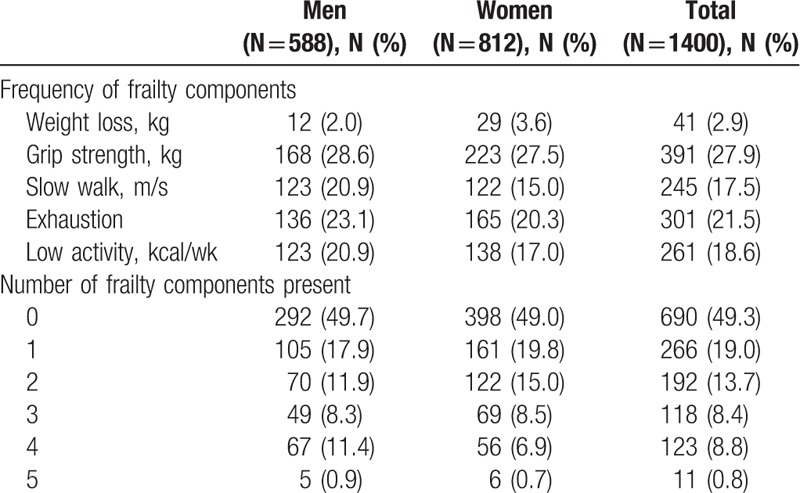
Table 1.
Prevalence of phenotype of frailty components in percentages.
2.4. Frailty assessment tool
FP was proposed by Fried et al,[6] the scale contained 5 items, the presence of 3 or more of the following components in the frailty scale was classified as frail, 1 or 2 criteria was considered as intermediate frailty status or prefrail, no criteria as nonfrail.
Weight loss was defined as self-reported unintentional weight loss >4.5 kg or >5% of body weight in prior year (by direct measurement of weight).
Exhaustion was indicated by a self-response as “a moderate amount the time” or “most of the time in the previous week” to either of the following 2 statements: “I felt everything I did was an effort” or “I could not get going” from the Center for Epidemiological Studies—Depression Scale.[23]
Low physical activity level was defined by gender-specific low weekly energy expenditure measured by Minnesota Questionnaire Assessment Scale,[24] and <383 kcal/wk for males and <270 kcal/wk for females were considered as “low physical activity.”
Slow walking speed and low grip strength were analyzed according to elderly Chinese people pace and grip strength standard,[25] <0.65 m/s for males, <0.60 m/s for females; <22 kg for males and <14 kg for females were indicated slow walking speed and low grip strength, respectively. Pace speed was measured by normal walking 6 m on level road; maximal handgrip strength was measured using a handheld dynamometer (CAMRY MODEL EH101, Guang Dong, China), Participants performed 2 trials on each side, the mean value of the best side was used.
2.5. Definition of indicators
2.5.1. Cognitive impairment
Subjects’ mental state was assessed using the Mini-Mental State Examination.[26] This comprises a total of 30 questions; each question that is correctly answered is awarded 1 point, whereas incorrect answers or no answers are awarded 0 points. The total score ranged from 0 to 30 points. A score of ≥24 was considered normal.
2.5.2. Depression
The Geriatric Depression Scale (GDS) was adopted to determine whether subjects exhibited depression.[27] The GDS comprises a total of 30 items, with a total score ranging from 0 to 30. Scores of ≥11 were considered as depression.
2.5.3. Barthel index
This instrument was used to evaluate Basic Activities of Daily Living (BADL),[28] including eating, bathing, grooming, dressing, bowel control, bladder control, assistance required for bed-to-chair movement or going to the bathroom, walking (45 m), and climbing and descending the stairs.
2.5.4. Instrumental Activities of Daily Living (IADL) (7 variables)
These 7 variables reflected individuals’ ability to perform the following activities, including shopping, going out, cooking, household chores, telephone use, taking medication, and financial management.[29]
2.5.5. Disability
The ≥1 item of BADL or IADL need assistance to finish or cannot even finish was considered to have a disability.[30]
2.5.6. Comorbidity
Comorbidity was defined as having 2 or more age-related health conditions or diseases through medical charts diagnosis.[31]
We defined subjects as smoking if they reported currently smoking or had smoked ≥100 cigarettes in a lifetime; subjects who had never smoked or had smoked <100 cigarettes in a lifetime were considered as nonsmoking.[32] Drinking alcohol referred to subjects who were still drinking, while those who never drank or occasionally drank were considered as nondrinking.
Participants were deemed as polypharmacy if they took ≥5 medications on a regular basis.
“Married” indicated that the spouse was still alive and lived together, whereas “live alone” included divorcees, single individuals, or widows but without lived with their family members.
2.6. Statistical analysis
The chi-squared test was used to compare categorical data, which were expressed as numbers and percentages. Continuous data were analyzed using 1-way analysis of variance and were expressed as means and standard deviations. We then entered above indicators into a univariate analysis. Those factors that were significantly related to frailty in the univariate analysis were then included in a multinomial logistic regression analysis to clarify the independent influencing factors of frailty status. (Using frailty as a dependent variable, variables with preliminary statistical significance from the univariate analysis were converted into independent variables.) Significance level was set at P < .05. The statistical analysis was carried out using SPSS 18.0 software (SPSS Inc., Chicago, IL).
3. Results
3.1. General subjects data
The overall recruited patients were aged between 60 and 99 years old (75.52 ± 9.28 years), with males (n = 588, 42%) ranging from 60 to 99 years old (76.11 ± 9.76 years) and females (n = 812, 58%) ranging from 60 to 97 years old (75.10 ± 8.90 years). The mean duration of hospitalization was 11.82 ± 4.65 days.
A total of 1400 individuals were identified. The most prevalent criterion was low handgrip strength (27.9%), followed by exhaustion (21.5%), low physical activity (18.6%), low gait speed (17.5%), and weight loss (2.9%) (Table 1).
The over prevalence of frailty in this study was 18.0% (n = 252), while the prevalence rates of intermediate and nonfrail were 32.7% (n = 458) and 49.3% (n = 690), respectively; and prevalence of frailty for frail female patients was 9.4% (n = 131) and male patients was 8.6% (n = 121) (Table 2).
Table 2.
The association of baseline indicators with different frailty level in percentages by univariate analysis.
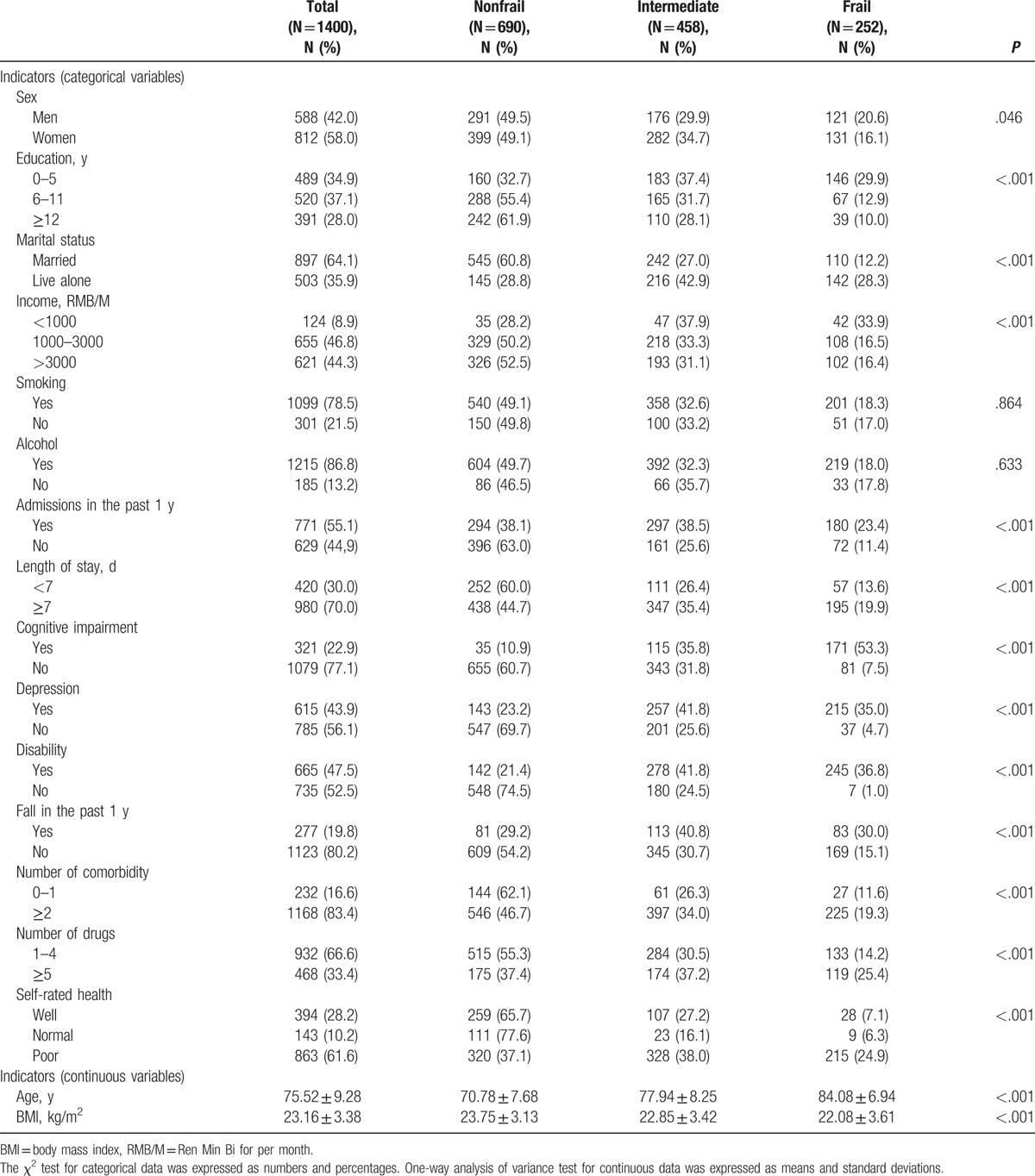
3.2. Univariate analysis results
In the univariate analysis, except for smoking and drinking, frailty was more common among patients with a low education level (≤5 years), low income (<1000 Ren Min Bi for per month [RMB/M]), live alone, and poor self-report health, frailty was also more likely to develop among patients with comorbidity, disability, cognitive impairment and depression, as well as those who had longer durations of hospitalization (≥7 days) and polypharmacy, a history of hospitalization and a fall in the previous year; notably, the proportion of frailty increased with increasing age and BMI (P < .05 for each comparison; Table 2).
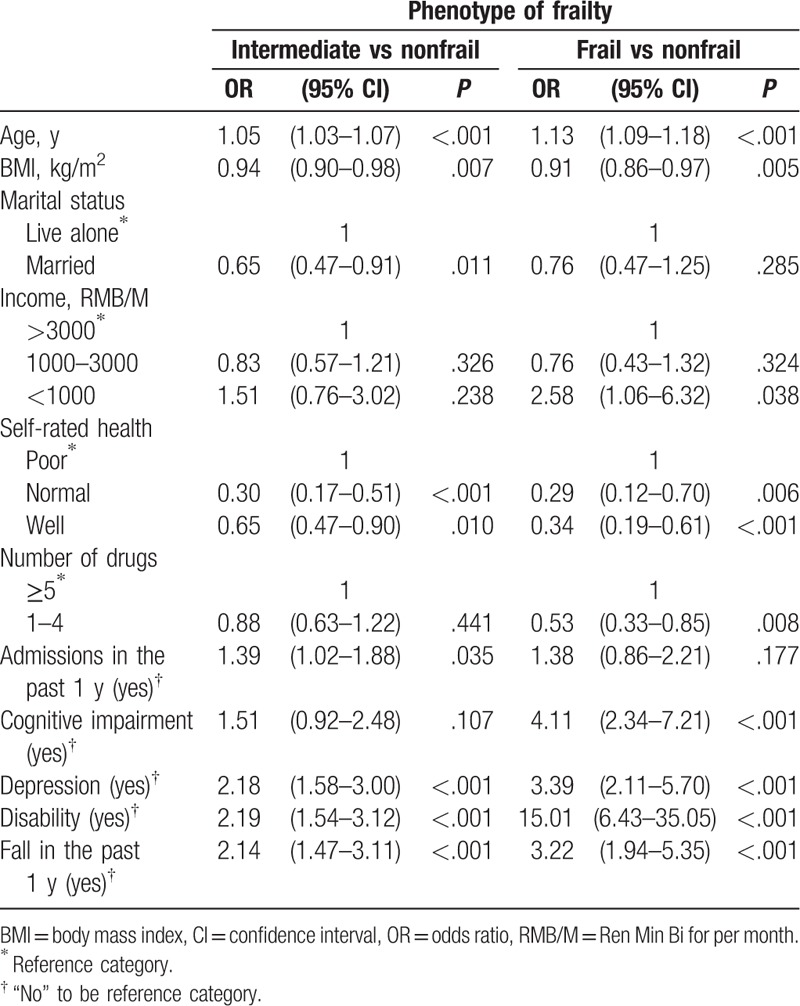
3.3. Multinomial logistic regression analysis results
The above significant variables were then incorporated into a multinomial logistic regression analysis. There were various risk factors in different frailty level. Table 3 shows that increasing age and BMI, disability, cognitive impairment and depression, polypharmacy, low income (<1000 RMB/M), poor self-rated health, and a fall history in the past 1 year were independently positively correlated with frail state (P < .05 for each comparison). Except for income, cognitive impairment, and polypharmacy, the other variables in Table 3 also independently correlated with frail intermediate status (P < .05 for each comparison).
Table 3.
The association between positively variables and different frailty levels by multinomial logistic regression analysis.
4. Discussion
The overall prevalence of frailty among 1400 patients aged ≥60 years old was 18.0%. Furthermore, the prevalence of intermediate frail was 32.7%. Currently, there is no consensus about the prevalence of frailty worldwide.[33] This is because of the diversity of instruments, research subjects, and ages focused on; as such, rates have ranged from 6.9% to 32%.[34–37] The results of this study were within this scope. Generally, the prevalence rate of frailty among older inpatients is higher than that among community-dwelling elderly,[38] in a systematic review of frailty status of multiple groups of a total of 61,500 community-dwelling participants aged ≥65 years old, the mean prevalence of frailty was 10.7%, with a range of 4.0% to 59.1%, the prefrailty prevalence rate was 41.6%.[33] Dent et al[39] applied different evaluation tools to measure the frailty prevalence among a total of 172 geriatric inpatients aged ≥70 years old, and found that the rates ranged from 24% to 94%. The prevalence of frailty in our study was below these ranges, which might be due to the relatively younger ages of the recruited subjects (≥60 years old). Notably, we found that a higher prevalence of frailty for frail female patients (9.4%) compared with male patients (8.6%), similar results have been reported previously,[18,19,33,40,41] which might be related to the former's lower BMI and muscle strength.[42]
Because all the subjects were hospitalized patients, we included “duration of hospitalization” and “history of hospitalization in the past 1 year” as variables, both of them had no independently correlated with frailty according to the regression analysis, 1 possible reason might be that longer hospital stay was an outcome of frailty rather than the etiologic risk factor.[34] Some positive indicators in the univariate analysis in our study were similar to the results from Taiwan of China.[21]
There were 9 independent risks factors related to frailty, including increasing age and BMI, disability, cognitive impairment and depression, polypharmacy, low income (<1000 RMB/M), poor self-rated health, and a fall history in the past 1 year. Age was an independent risk factor, a numerous of studies have showed that the prevalence of frailty increased with increasing age.[19,20,22,33,40] Some scholars have explored that frailty can increase the risks of hospitalization, fall, and disability.[7,8,43] The other researches have proposed that polypharmacy was the one of presence of frailty syndrome.[44,45]
A regression analysis further explored that intermediate frail and frail had different risk factors, the strength of the correlations of these variables was dissimilar in different frail levels. As shown in Table 3, for example, when the frail compared with nonfrail groups, the odds ratio (OR) of disability was 15.01 (95% confidence interval [CI] was 6.43–35.05, P < .001). In comparison with nonfrail groups, the intermediate group had an OR of 2.19 (95% CI [1.54–3.12], P < .001). Disability was thus regarded as strong risk factors in this study.
Based on the results of this study, a timely assessment of frailty status should be given to recently admitted inpatients (especially during their prefrail or frail state). The “Silver Book” is an intercollegiate publication focusing on good care during the first 24 h of an older person's admission to hospital,[45] it recommends that all patients are assessed for depression, falls, continence, dementia, nutrition, and activities of daily living, etc.; this is especially necessary for inpatients with high-risk factors. There is currently no effective treatment for frailty, the emphasis is on prevention. Good education can improve cognitive function.[46] A timely medical care or treatment might be a result of good economic support from higher income. Exercise can improve the central nervous, endocrine, immune system, and function of skeletal system; improve the body function and mobility[47–53] as well as reverse or attenuate sarcopenia,[54]; reduce falls, disability, and its complications; and also can improve cognitive function and emotion.[55]
A meta-analysis by Kelaiditi et al showed that exercise and nutritional therapy can improve frailty state and delay the decline in function.[56] The current guidelines from the US Department of Health and Human Services (www.health.gov/paguidelines/guidelines/default.aspx) suggested that all adults over 65 years should participate in 150 min (2 h and 30 min) of moderate aerobic exercise per week, and encouraged frail older adults to start with an aerobic activity such as walking, as it is more accessible, if possible, resistance exercise training should be added, depending on the frailty level. Morley was also to demonstrate the role of resistance exercise in frailty management.[57] Majority of the evidence have showed that regular physical activity or exercise was beneficial for older adults who were frail or at high risk of frailty.[58]
5. Conclusions
We assessed the frailty status of geriatric inpatients using FP instrument; in our data, the overall prevalence of frailty was 18.0%, the prevalence of prefrailty was 32.7%, and multidimensional factors were independently positively associated with frailty. The emphasis is on prevention, interventions would need to be comprehensive, targeting physiology and psychology aspects of geriatric patients. The effective strategies would alleviate or reverse frailty status.
China has a rapidly aging population, how to face the challenges of health care for the elderly? To our knowledge, above of, timely evaluation of frailty status for newly admitted to the hospital patients is one of methods, last but not least, a diverse health management model is urgently needed to prevent and treat frailty for the older adults. Furthermore, we will take specific interventions measures for frail patients in future research.
This study had several limitations: first, we recruited only inpatients, meaning that the results cannot represent community-dwelling elderly. Second, some data were based on self-reports, which might mean that they are subject to recall bias. Third, because this was a cross-sectional study, we could not follow-up on patients’ health status, particularly those with poor health outcomes (e.g., mortality). These factors should be further studied.
Acknowledgment
The authors would like to thank the patients who participated in the study.
Footnotes
Abbreviations: BADL = Basic Activities of Daily Living, BMI = body mass index, CI = confidence interval, FP = Phenotype of Frailty, IADL = Instrumental Activities of Daily Living, OR = odds ratio, RMB/M = Ren Min Bi for per month.
Fan Yang performed the study, interpreted the patient data, and wrote the paper. Qing-Wei Chen revised the article. All authors read and approved the final article.
This work was supported by the following grants: Science and Technology Bureau of Zunyi, Gui Zhou Province, China (No. 04, 2015).
The authors have no conflicts of interest to disclose.
References
- [1].Hamerman D. Toward an understanding of frailty. Ann Intern Med 1999;130:945–50. [DOI] [PubMed] [Google Scholar]
- [2].Whitson HE, Purser JL, Cohen HJ. Frailty thy name is ... Phrailty? J Gerontol A Biol Sci Med Sci 2007;62:728–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bowsher J, Bramlett M, Burnside IM, et al. Methodological considerations in the study of frail elderly people. J Adv Nurs 1993;18:873–9. [DOI] [PubMed] [Google Scholar]
- [4].Bales CW, Ritchie CS. Sarcopenia, weight loss, and nutritional frailty in the elderly. Annu Rev Nutr 2002;22:309–23. [DOI] [PubMed] [Google Scholar]
- [5].Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56. [DOI] [PubMed] [Google Scholar]
- [7].Bandeen RK, Xue QL, Ferrucci L, et al. Phenotype of frailty: characterization in the women's health and aging studies. J Gerontol A Biol Sci Med Sci 2006;61:262–6. [DOI] [PubMed] [Google Scholar]
- [8].Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 2008;168:382–9. [DOI] [PubMed] [Google Scholar]
- [9].Kiely DK, Cupples LA, Lipsitz LA. Validation and comparison of two frailty indexes: the MOBILIZE Boston Study. J Am Geriatr Soc 2009;57:1532–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Rockwood K, Abeysundera MJ, Mitnitski A. How should we grade frailty in nursing home patients? J Am Med Dir Assoc 2007;8:595–603. [DOI] [PubMed] [Google Scholar]
- [11].Rockwood K, Mitnitski A, Song X, et al. Long-term risks of death and institutionalization of elderly people in relation to deficit accumulation at age 70. J Am Geriatr Soc 2006;54:975–9. [DOI] [PubMed] [Google Scholar]
- [12].Romero-Ortuno R. The Frailty Instrument of the Survey of Health, Ageing and Retirement in Europe (SHARE-FI) predicts mortality beyond age, comorbidities, disability, self-rated health, education and depression. Eur Geriatr Med 2011;2:323–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Romero-Ortuno R, Walsh CD, Lawlor BA, et al. A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). BMC Geriatr 2010;10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gobbens RJ, van Assen MA, Luijkx KG, et al. The Tilberg frailty indicator: psychometric properties. J Am Med Dir Assoc 2010;11:344–55. [DOI] [PubMed] [Google Scholar]
- [15].Gobbens RJ, van Assen MA, Luijkx KG, et al. Determinants of frailty. J Am Med Dir Assoc 2010;11:356–64. [DOI] [PubMed] [Google Scholar]
- [16].Peters LL, Boter H, Buskens E, et al. Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J Am Med Dir Assoc 2012;13:546–51. [DOI] [PubMed] [Google Scholar]
- [17].Hoogendijk EO, van Hout HP. Investigating measurement properties of the Groningen Frailty Indicator: a more systematic approach is needed. J Am Med Dir Assoc 2012;13:757. [DOI] [PubMed] [Google Scholar]
- [18].Woo J, Goggins W, Sham A, et al. Public health significance of the frailty index. Disabil Rehabil 2006;28:515–21. [DOI] [PubMed] [Google Scholar]
- [19].Shi J, Song X, Yu P, et al. Analysis of frailty and survival from late middle age in the Beijing Longitudinal Study of Aging. BMC Geriatr 2011;11:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Dupre ME, Gu D, Warner DF, et al. Frailty and type of death among older adults in China: prospective cohort study. BMJ 2009;338:b1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chang CI, Chan DC, Kuo KN, et al. Prevalence and correlates of geriatric frailty in a northern Taiwan community. J Formos Med Assoc 2011;110:247–57. [DOI] [PubMed] [Google Scholar]
- [22].Ma L, Zhang L, Tang Z, et al. Use of the frailty index in evaluating the prognosis of older people in Beijing: a cohort study with an 8-year follow-up. Arch Gerontol Geriat 2016;64:172–7. [DOI] [PubMed] [Google Scholar]
- [23].Orme J, Reis J, Herz E. Factorial and discriminate validity of the Center for Epidemiological Studies depression (CES-D) scale. J Clin Psychol 1986;42:28–33. [DOI] [PubMed] [Google Scholar]
- [24].Taylor HL, Jacobs DR, Jr, Schucker B, et al. A questionnaire for the assessment of leisure time physical activities. J Chron Dis 1978;31:741–55. [DOI] [PubMed] [Google Scholar]
- [25].Liu Y, Jian Z. The evaluation of frailty in older adults. Health Manag 2014;9:40–3. [Google Scholar]
- [26].Magni E, Binetti G, Bianchetti A, et al. Mini-Mental State Examination: a normative study in an Italian elderly population. Eur J Neurol 1996;3:198–202. [DOI] [PubMed] [Google Scholar]
- [27].Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17:37–49. [DOI] [PubMed] [Google Scholar]
- [28].Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index: reliability study. Md State Med J 1965;14:61–5. [PubMed] [Google Scholar]
- [29].Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J 2001;1:323–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kane RL, Shamliyan T, Talley K, et al. The association between geriatric syndromes and survival. Am Geriatr Soc 2012;60:896–904. [DOI] [PubMed] [Google Scholar]
- [31].Yancik R, Ershler W, Satariano W, et al. Report of the National Institute on Aging Task Force on Comorbidity. J Gerontol A Biol Sci Med Sci 2007;62A:275–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lin CC, Li CI, Chang CK, et al. Reduced health-related quality of life in elders with frailty: a cross-sectional study of community-dwelling elders in Taiwan. PLoS ONE 2011;6:e21841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Collard RM, Boter H, Schoevers RA, et al. Prevalence of frailty in community dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487–92. [DOI] [PubMed] [Google Scholar]
- [34].Puts MT, Lips P, Deeg DJ. Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol 2005;58:1188–98. [DOI] [PubMed] [Google Scholar]
- [35].Schuurmans H, Steverink N, Lindenberg S, et al. Old or frail: what tells us more? J Gerontol A Biol Sci Med Sci 2004;59:M962–5. [DOI] [PubMed] [Google Scholar]
- [36].Purser JL, Kuchibhatla MN, Fillenbaum GG, et al. Identifying frailty in hospitalized older adults with significant coronary artery disease. J Am Geriatr Soc 2006;54:1674–81. [DOI] [PubMed] [Google Scholar]
- [37].Khandelwal D, Goel A, Kumar U, et al. Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging 2012;16:732–5. [DOI] [PubMed] [Google Scholar]
- [38].Parker SG, Fadayevatan R, Lee SD. Acute hospital care for frail older people. Age Ageing 2006;35:551–2. [DOI] [PubMed] [Google Scholar]
- [39].Dent E, Chapman I, Howell S, et al. Frailty and functional decline indices predict poor outcomes in hospitalised older people. Age Ageing 2014;43:477–84. [DOI] [PubMed] [Google Scholar]
- [40].Gu D, Dupre ME, Sautter J, et al. Frailty and mortality among Chinese at advanced ages. J Gerontol B Psychol Sci Soc Sci 2009;64B:279–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Mitnitski A, Song X, Skoog I, et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc 2005;53:2184–5189. [DOI] [PubMed] [Google Scholar]
- [42].Morley JE. Diabetes, sarcopenia, and frailty. Clin Geriatr Med 2008;24:455–69. [DOI] [PubMed] [Google Scholar]
- [43].Rockwood K, Howlett SE, MacKnight C, et al. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci 2004;59:1310–7. [DOI] [PubMed] [Google Scholar]
- [44].British Journal of Hospital Medicine. Assessment of frailty in the inpatient setting. Br J Hosp Med 2016;77:29–31. [DOI] [PubMed] [Google Scholar]
- [45].Turner G, Clegg A. British Geriatrics Society. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing 2014;43:744–7. [DOI] [PubMed] [Google Scholar]
- [46].van Kan GA, Rolland Y, Bergman H, et al. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging 2008;12:29–37. [DOI] [PubMed] [Google Scholar]
- [47].Van Praag H. Exercise and the brain: something to chew on. Trends Neurosci 2009;32:283–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Barber SE, Clegg AP, Young JB. Is there a role for physical activity in preventing cognitive decline in people with mild cognitive impairment? Age Ageing 2012;41:5–8. [DOI] [PubMed] [Google Scholar]
- [49].Gleeson M, McFarlin B, Flynn M. Exercise and toll-like receptors. Exerc Immunol Rev 2006;12:34–53. [PubMed] [Google Scholar]
- [50].Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature 2008;454:463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].De Vries NM, van Ravensberg CD, Hobbelen JS, et al. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing Res Rev 2012;11:136–49. [DOI] [PubMed] [Google Scholar]
- [52].Theou O, Stathokostas L, Roland KP, et al. The effectiveness of exercise interventions for the management of frailty: a systematic review. J Aging Res 2011;2011:569194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Clegg A, Barber S, Young J, et al. Do home-based exercise interventions improve outcomes for frail older people? Findings from a systematic review. Rev Clin Gerontol 2012;22:68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Tarazona-Santabalbina FJ, Gómez-Cabrera MC, Pérez-Ros P, et al. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: a randomized clinical trial. JAMDA 2016;17:426–33. [DOI] [PubMed] [Google Scholar]
- [56].Kelaiditi E, Van Kan GA, Cesari M. Frailty: role of nutrition and exercise. Curr Opin Clin Nutr Metab Care 2014;17:32–9. [DOI] [PubMed] [Google Scholar]
- [57].Morley JE. Frailty: diagnosis and management. J Nutr Health Aging 2011;15:667–70. [DOI] [PubMed] [Google Scholar]
- [58].Fiatarone MA, O’neill EF, Ryan ND, et al. Training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med 1994;330:1769–75. [DOI] [PubMed] [Google Scholar]


