Supplemental Digital Content is available in the text
Keywords: balloon block and support technique, coronary bifurcation intervention, side branch wiring
Abstract
Background:
Despite advancements in the devices and techniques used for percutaneous coronary intervention, side branch (SB) wiring remains highly challenging in certain complex bifurcation intervention cases.
Methods and Results:
In this report, we demonstrate the efficacy and safety of the balloon block and support technique (BBST), which comprises inflation of an appropriately sized balloon 1–2 mm distal from the carina in the distal main branch to facilitate wire access to the SB. Between June 2012 and July 2017, we utilized the BBST as a bail-out strategy for six bifurcation cases with difficult SB wiring. In this report, we present in detail the oldest and the most recent of those cases to illustrate the use of the BBST. As a bail-out strategy, the BBST successfully facilitated SB wiring. No BBST-related complications were observed.
Conclusions:
The BBST may be an efficient and safe method for facilitating SB wiring in complex bifurcation intervention cases and could be used as a bail-out technique.
1. Introduction
Successful guide wire placement in the side branch (SB) is essential for coronary bifurcation intervention. Despite advancements in the devices and techniques used for percutaneous coronary intervention,[1–4] SB wiring remains highly challenging in certain complex cases. The factors that affect SB wiring include severe curvature, heavy plaque burden and significant stenosis in the proximal main branch (PMB), and extremely angulated SB (greater than 90°).
2. Methods
In cases with significant angulation (greater than 90°) between the SB and distal main branch (DMB), the guide wire is always advanced into the DMB instead of the SB. An uninflated balloon (B) is placed in the DMB at 1–2 mm from the carina. Once the tip of the guide wire reaches the level of the SB ostium (SBO), the balloon is inflated to block (B) the DMB pathway and provide upward support (S) for the guide wire. This facilitates advancement of the guide wire into the SB. The acronym created for this technique (T) is balloon block and support technique (BBST).
Additionally, in cases with heavy plaque burden in the PMB at the origin of the SB, the preshaped guide wire tip becomes straightened due to the severe stenosis near the SBO. This causes the guide wire to slip into the DMB when it is further advanced. To prevent this, a balloon is inflated to block the DMB pathway and provide additional upward support for the SB guide wire.
All procedures performed in this study involving human participants were conducted in accordance with the standards of the Ethics Committee of the Guangzhou Red Cross Hospital and with fully informed consent.
3. Results
Between June 2012 and July 2017, we utilized the BBST as a bail-out strategy for six bifurcation cases with difficult SB wiring. These included four cases of Medina 1,1,1 and two cases of Medina 1,0,1. The bifurcation characteristics and procedural details of the six cases treated with the BBST are shown in Table 1. Of these cases, two were described in detail below.
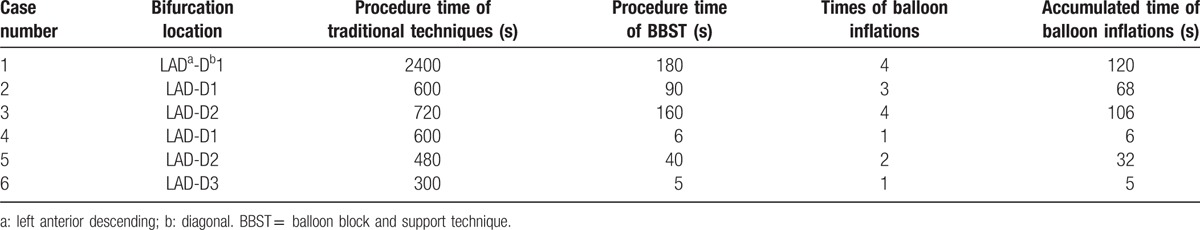
Table 1.
Bifurcation characteristics and procedural details for the six cases treated with the balloon block and support technique.
3.1. Case 1
A 55-year-old man was admitted to the hospital complaining of chest pain lasting for 1 month. Coronary angiography (CAG) showed a left anterior descending artery (LAD) and the first diagonal artery (D1) bifurcation lesion. The angle between the LAD and D1 was approximately 70°, which was enlarged to over 90° by the plaque in the SBO (Figure 1A–C). We successfully advanced a BMW UNIVERSAL guide wire (ABBOTT VASCULAR) into the distal LAD. However, we failed to advance a Rinato guide wire (ASAHI) into the D1 despite using different techniques, including switching to a Runthrough NS Floppy guide wire (TERUMO) and a Pilot50 guide wire (MEDAKO INDIA), reshaping the guide wires, and predilating the PMB. We then placed a Sprinter Legend 2.5 × 15 mm balloon (MEDTRONIC) in the distal LAD (2 mm from the carina) and advanced a preshaped Rinato guide wire to the carina. Next, we inflated the balloon at 8 atm while inserting the guide wire and directing the tip toward the SBO (Figure 1D). After three attempts, the guide wire advanced into the SB with support from the inflated balloon (Figure 1E, Supplemental Video 1 which demonstrates the BBST procedure in case 1). The subsequent intervention was successfully completed.
Figure 1.
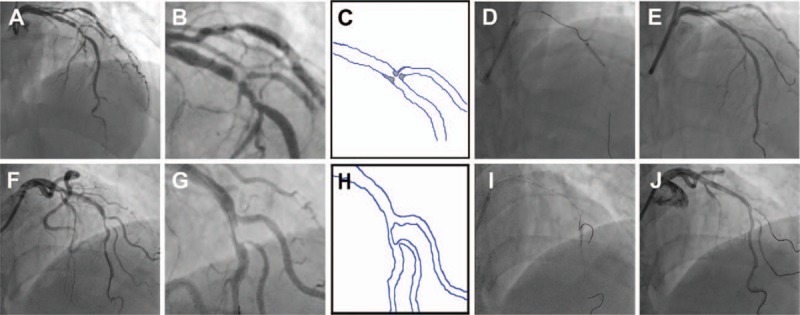
Bifurcation characteristics and the balloon block and support technique (BBST) procedure in case 1 and 2. A, B: Baseline angiography showed left anterior descending-first diagonal (LAD-D1) bifurcation lesions. C: Schematic diagram showing much more rapid LAD-D1 angulation than that apparent by visual estimation. D, E: Fluoroscopy showing that inflation of a balloon in the distal main branch facilitates side branch wiring. F, G: Baseline angiography showing left anterior descending-third diagonal (LAD-D3) bifurcation lesions and an extremely angulated D3. H: Schematic diagram depicting heavy plaque burden in the proximal main branch and rapid LAD-D3 angulation. I, J: Details of the BBST procedure.
3.2. Case 2
A 76-year-old male with intermittent chest pain for a 2-year duration presented with aggravated resting angina lasting for 1 week and was admitted to our hospital. As shown in Figure 1F–H, CAG showed a severe stenosis in the mid-LAD. The ostia of the second diagonal artery (D2) and the third diagonal artery (D3) were involved. We advanced a BMW UNIVERSAL guide wire into the distal LAD and a Rinato guide wire into the D2, but failed to advance a Runthrough NS Floppy guide wire into the D3 by modifying the PMB plaque or using a microcatheter. A Sprinter Legend 2.0 × 12 mm balloon was then placed in the distal LAD (1–2 mm from the carina). After the Runthrough NS Floppy guide wire reached the carina, the balloon was inflated at 8 atm while directing the guide wire toward the SBO and advancing it further. After only one attempt, the guide wire was advanced and placed into the D3 successfully within 5 min (Figure 1I,J, Supplemental Video 2, which demonstrates the BBST procedure in case 2). Finally, a drug-eluting stent was deployed in the LAD as a provisional strategy.
4. Discussion
The success rate for SB wiring has dramatically improved with the development of advanced techniques. The success of traditional techniques depends on bifurcation angle, lesion type, and availability of special devices (e.g., venture-catheter and microcatheter). Additionally, there is concern that some of those techniques may have higher complication rates. For example, plaque modification in the PMB may cause complete occlusion of the SB. Herein, we proposed a novel maneuver that facilitates SB wiring during bifurcation intervention; we named this maneuver the BBST.
The following features differentiate the BBST from other techniques: (1) It does not utilize additional devices, except a balloon, which is the key device. (2) It can be performed effectively with little risk. (3) It can be performed with a variety of soft guide wires, such as the BMW UNIVERSAL, Rinato, and Runthrough NS floppy guide wires in our cases.
As shown in Figure 2, the BBST is applicable for SB wiring in cases with the following lesion characteristics: (1) large angle (greater than 70°) of the SB (Figure 2A); (2) PMB lesion bifurcations of Medina 1,1,1, 1,0,1, and 1,0,0 (Figure 2B); and (3) DMB wiring in Medina 1,1,1 with balloon placement in the SB (Figure 2C).
Figure 2.
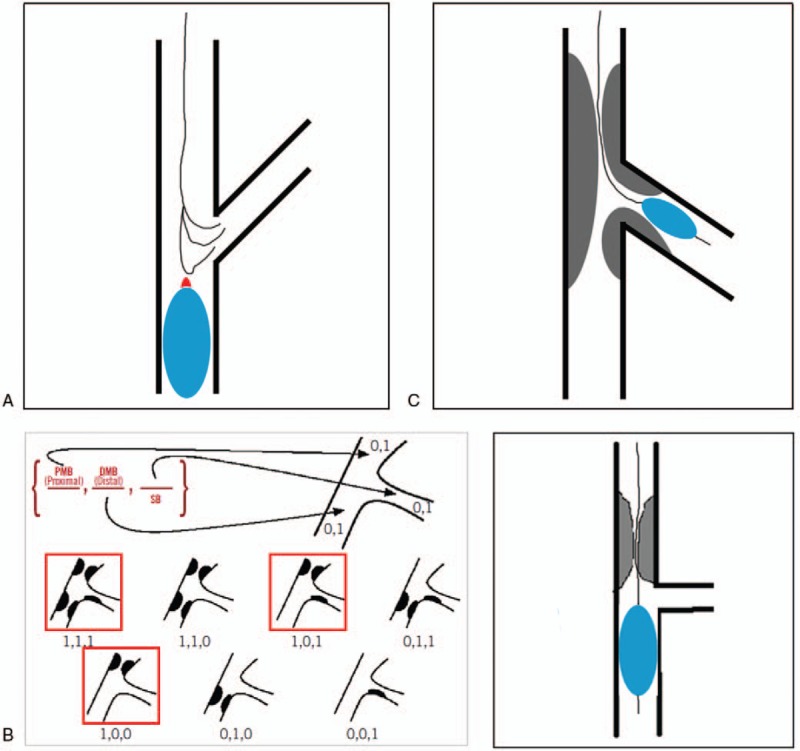
Mechanisms and theoretical indications of the balloon block and support technique (BBST). A, B: In cases with severe angulation of greater than 70° between the distal main branch (DMB) and side branch (SB) (A), and cases with heavy plaque burden or significant stenosis in the proximal main branch (PMB) near the SB ostium (SBO) (B), balloon inflation provides upward support for the guide wire by blocking the DMB pathway and facilitating guide wire advancement into the SB. C: DMB wiring in Medina 1,1,1 with the balloon placed in the SB.
The following aspects of the BBST should be noted: (1) The balloon diameter to DMB ratio should be 0.75:1. (2) The balloon should be inflated at a low pressure (8–10 atm). (3) The inflation of the balloon should not cause any ischemic symptoms. For the six cases presented here, the longest balloon inflation time was 60 s, and no BBST-related complications were observed (Table 1). (4) The balloon should be placed 1–2 mm distal from the carina in the DMB to help provide adequate space for the guide wire to be advanced toward the SB. (5) The balloon should remain inflated, while the guide wire is advanced through the proximal SB and then deflated when the guide wire reaches the mid-SB.
5. Study limitations
There are some limitations to our study. First, this was a single-center study. More experiences are required to confirm the clinical effectiveness of this new technique and generalize this technique as a bail-out strategy for SB wiring.
6. Conclusions
The presented cases highlight the efficacy and safety of the BBST for facilitating SB wiring in complex bifurcation lesions independent of additional devices. The BBST shows promise as a bail-out technique after unsuccessful attempts at SB wiring using routine maneuvers.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: BBST = balloon block and support technique, CAG = coronary angiography, D1 = the first diagonal artery, D2 = the second diagonal artery, D3 = the third diagonal artery, DMB = distal main branch, LAD = left anterior descending artery, PCI = percutaneous coronary intervention, PMB = proximal main branch, SB = side branch, SBO = SB ostium.
This work was supported by the Natural Science Foundation of Guangdong Province [grant number 2016A030313430]; the Scientific and Technological Program of Guangzhou City [grant number 201510010024]; the Natural Science Foundation of Guangdong Province [grant number 2014A030310049].
The authors report no relationships that could be construed as a conflict of interest.
Supplemental Digital Content is available for this article.
References
- [1].Burzotta F, De Vita M, Sgueglia G, et al. How to solve difficult side branch access? Euro Intervention 2010;6:J72–80. [DOI] [PubMed] [Google Scholar]
- [2].Ojeda S, Pan M, Mazuelos F, et al. Use of the venture wire-control catheter for accessing side branches during provisional stenting: an option for bifurcations with an unfavorable anatomy. Rev Esp Cardiol 2010;63:1487–91. [DOI] [PubMed] [Google Scholar]
- [3].Nomura T, Kikai M, Hori Y, et al. Tips of the dual-lumen microcatheter-facilitated reverse wire technique in percutaneous coronary interventions for markedly angulated bifurcated lesions. Cardiovasc Interv Ther 2017;Epub Ahead of Print. [DOI] [PubMed] [Google Scholar]
- [4].Nomura T, Higuchi Y, Kato T. Successful percutaneous coronary intervention for complex bifurcated lesions with combination of “Reverse wire technique” and “Reverse bent wiring with the crusade catheter” novel wire manipulation technique. Catheter Cardiovasc Interv 2016;87:920–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


