Abstract
Background:
Involvement in road traffic accidents (RTAs) may put individuals at increased risk for a wide range of psychiatric disorders, among which posttraumatic stress disorder (PTSD) presents a public health issue. However, a great disparity was observed among studies exploring the prevalence of PTSD among RTA survivors. This meta-analysis aimed to explore the pooled prevalence of PTSD among RTA survivors.
Methods:
Electronic databases of PubMed, Embase, Web of Science, PsycARTICLES, PsycINFO, and CINAHL were searched to identify relevant studies. Study selection and data extraction were conducted independently by 2 investigators, and a meta-analysis was performed to synthesize the data. Heterogeneity among studies was evaluated using the Cochran Q test and quantified using the I2 statistic. Subgroup analyses were performed to identify the source of the heterogeneity. The possibility of publication bias was assessed using Egger linear test.
Results:
Fifteen eligible studies containing 6804 RTA survivors were identified in this meta-analysis, of which 1489 were identified with PTSD. The pooled prevalence of PTSD among RTA survivors was 22.25% (95% confidence interval: 16.71%–28.33%). A high degree of heterogeneity was observed across studies (I2 = 97.1%, P < .001), with reported PTSD prevalence ranging from 6.3% to 58.3%. Subgroup analyses found that the prevalence of PTSD among RTA survivors varied significantly across studies in relation to the instrument used to assess PTSD, country, race, gender, and education level (P < .05).
Conclusion:
The high pooled prevalence of PTSD among RTA survivors found in this study significantly underscores the need for providing timely and effective intervention strategies for RTA survivors.
Keywords: meta-analysis, posttraumatic stress disorder, prevalence, road traffic accident
1. Introduction
Over 50 million people worldwide experience trauma through road traffic accidents (RTAs) yearly, and by the year 2020, the injury caused by RTA will be the 3rd-leading cause of disability.[1] Accumulated evidence has shown that involvement in RTA may put individuals at increased risk for a wide range of psychiatric disorders, including posttraumatic stress disorder (PTSD), depression, anxiety, etc.[2–4] In particular, PTSD presents a public health issue in RTA-related population.[5,6]
PTSD is characterized by intrusion, avoidance, hyper-arousal, and negative alterations in cognition and mood according to the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders-V.[7] PTSD can lead to not only physical and psychological impairment but also high healthcare costs.[8–10] For example, Landolt et al[11] found that early PTSD symptoms could have negative influence on health-related quality of life among injured children and adolescents following RTA, and Bartoli et al[12] found that individuals with PTSD have a greater risk of metabolic syndrome and obesity.[13] Furthermore, Chan et al[14] interviewed 391 RTA survivors in South Australia at about 9 months after the accident and found that compared with those without PTSD, individuals with PTSD incurred higher healthcare costs. In this regard, a reliable estimate of the prevalence of PTSD among RTA survivors is of great importance, as it may help the service providers to predict the number of RTA survivors who may develop PTSD, and thus providing timely and effective intervention strategies.
However, a great disparity was observed across studies exploring the prevalence of PTSD among RTA survivors, ranging from 6% to 50%,[15,16] indicating the necessity to estimate the pooled prevalence. Therefore, this meta-analysis aimed to explore the pooled prevalence of PTSD among RTA survivors.
2. Methods
2.1. Ethical approval
Ethical approval was not required for this meta-analysis since this meta-analysis utilized published data which were already ethically approved.
2.2. Search strategy
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Electronic databases of PubMed, Embase, Web of Science, PsycARTICLES, PsycINFO, and CINAHL were searched from their inception to September 2017. Instead of using “key words,” this study used “title” or “abstract,” to enroll more relevant articles. For example, search terms for the database of PubMed was “(((posttraumatic stress disorder[Title/Abstract]) OR post traumatic stress disorder[Title/Abstract]) OR PTSD[Title/Abstract]) AND ((((road traffic accident[Title/Abstract]) OR road traffic crash[Title/Abstract]) OR motor vehicle accident[Title/Abstract]) OR motor vehicle crash[Title/Abstract])”. The reference lists for full articles were also identified in this study.
2.3. Eligibility criteria
The inclusion criteria for this meta-analysis were: observational studies focusing on RTA survivors; sample size ≥200; examined PTSD with specific reference to RTA at least 1 month after the accident; provided a clear definition of the diagnosis of PTSD; reported a binary outcome for PTSD with “Yes” or “No”; and provided information about the sample size and the prevalence of PTSD among RTA survivors. The exclusion criteria were: full article not written in English; and reviews, comments, or case reports. Besides, if repeated data were observed across studies with the same follow-up period, only the earlier publication was included.
2.4. Data extraction
Two investigators (WL and MX) independently identified the eligibility of articles and extracted data from eligible articles. Any discrepancies between them were resolved by consensus. Data extracted from eligible articles for this study were: first author, year of publication, country, study design, time point of PTSD assessment, injury severity, instrument used to assess PTSD, number of survivors with PTSD, sample size, prevalence of PTSD, and quality of study. Besides, if necessary, data on race, gender, marital status, education level, and position in vehicle were also extracted to perform subgroup analyses.
2.5. Quality assessment
The Agency for Healthcare Research and Quality was used to assess the quality of eligible articles.[17,18] It consists of 11 items, each with 3 possible answers “Yes” or “No” or “Unclear.” The response of “Yes” for each item is scored “1,” and the response of “No” or “Unclear” is scored “0.” Therefore, the total score of this instrument ranges from 0 to 11, with 0 to 3, 4 to 7, and 8 to 11 indicating low, moderate, and high quality, respectively.
2.6. Statistical analysis
Statistical analyses for this study were conducted using the R statistical software version 3.2.0. Heterogeneity across studies was evaluated using χ2 test for Cochran Q statistic and quantified with the I2 statistic, with I2 ≥25%, ≥50%, and ≥75% indicating low, moderate, and high heterogeneity, respectively.[19] The pooled prevalence of PTSD among RTA survivors was combined using Freeman–Tukey double arcsine method by a fixed effects model if the P value of χ2 test for Cochran Q statistic was at least 0.05. Otherwise, a random effects model was used.[20] Sensitivity was assessed by the effect of low-quality articles on the stability of the pooled prevalence.[21,22] Publication bias was evaluated using the Egger linear test and a funnel plot for asymmetry was presented.[23] Besides, if necessary, subgroup analyses according to the time point of PTSD assessment, instrument used to assess PTSD, country, race, gender, marital status, education level, and position in vehicle were performed to identify the source of the heterogeneity. The χ2 tests were used to compare the difference within each subgroup and the significance level was set at P < .05.
3. Results
3.1. Search results
A total of 616 articles were yielded by the search strategy of this study. After removing duplicates, 432 articles were screened for eligibility. After abstracts screening, 69 full articles were shortlisted for eligibility. Among the 69 articles, 16 were excluded for neither reporting the prevalence of PTSD among RTA survivors nor reporting a binary outcome (“Yes” or “No”) of PTSD, 34 were excluded for having a sample size of less than 200, and 4 were excluded for repeated data. Finally, 15 eligible articles were included in this meta-analysis (Fig. 1).
Figure 1.
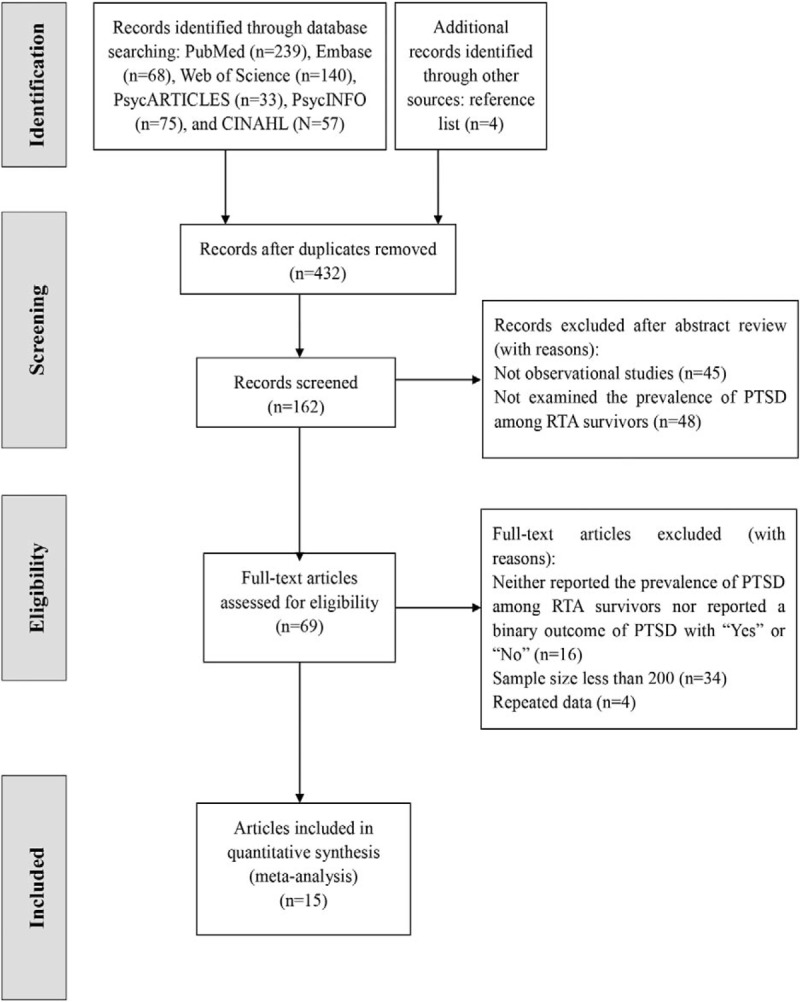
Flow chart of study identification and selection.
3.2. Study characteristics
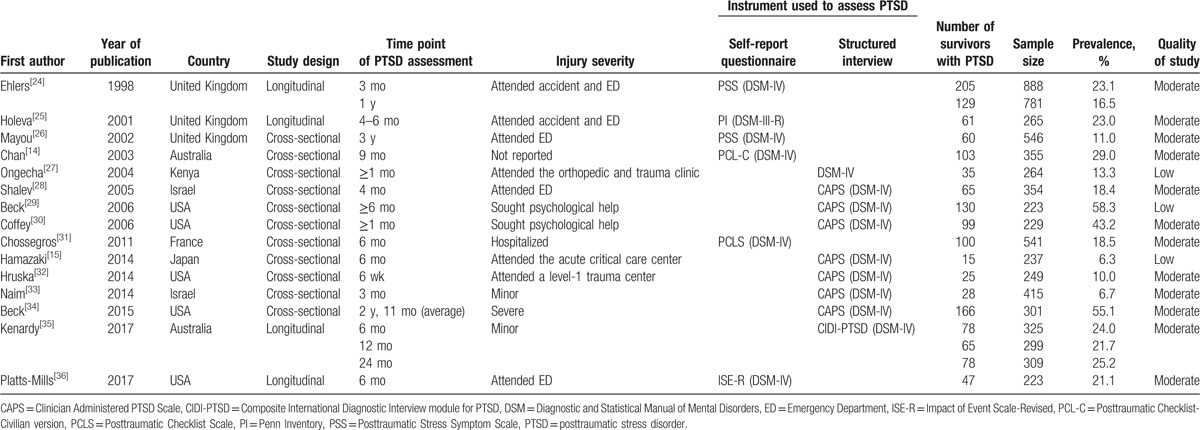
Table 1 shows the characteristics of eligible studies. Fifteen studies conducted in 7 countries were included. A total of 6804 RTA survivors were assessed, of which 1489 were identified with PTSD. Among the 15 eligible studies, 4 were longitudinal and 11 were cross-sectional. Besides, 6 used self-report questionnaire to assess PTSD and 9 used structured interview. The time points of PTSD assessment among these studies ranged from 1 month to 37 years after RTA. Additionally, according to the Agency for Healthcare Research and Quality assessment, 3 were considered low quality and 12 were considered moderate quality.
Table 1.
Characteristics of eligible studies included in this meta-analysis.
3.3. Pooled prevalence of PTSD among RTA survivors
A high degree of heterogeneity was observed across studies (I2 = 97.1%, P < .001), with the reported prevalence of PTSD ranging from 6.3%[15] to 58.3%.[29] The pooled prevalence of PTSD among RTA survivors was 22.25% (95% confidence interval [CI]: 16.71%–28.33%) by a random effects model. Figure 2 presents the details.
Figure 2.
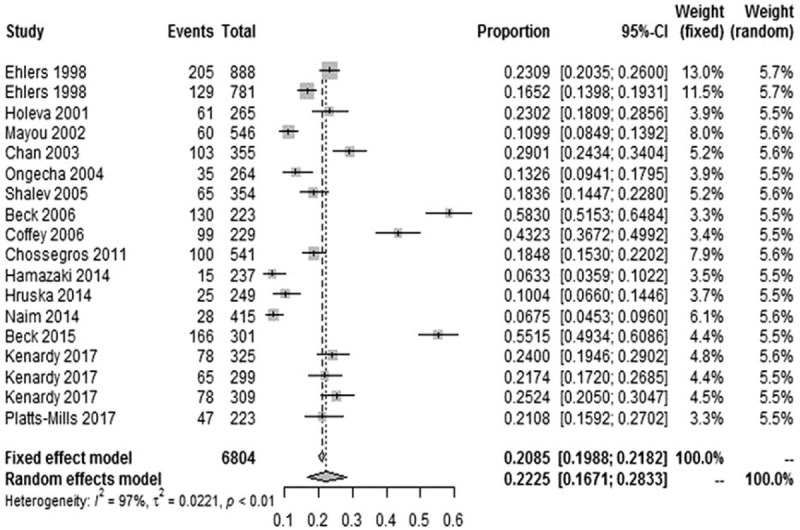
Forest plot presenting the prevalence of PTSD among RTA survivors. PTSD = posttraumatic stress disorder, RTA = road traffic accident.
3.4. Sensitivity analysis and publication bias
After excluding 3 articles with low quality, the pooled prevalence of PTSD among RTA survivors decreased slightly from 22.25% (95% CI: 16.71%–28.33%) to 22.12% (95% CI: 16.84%–27.88%), suggesting low sensitivity of this meta-analysis.
Publication bias was not observed in this meta-analysis, with P value for the Egger linear test being 0.289 (t = 1.097). Consistent with the result of Egger linear test, the funnel plot was symmetrical (Fig. 3).
Figure 3.
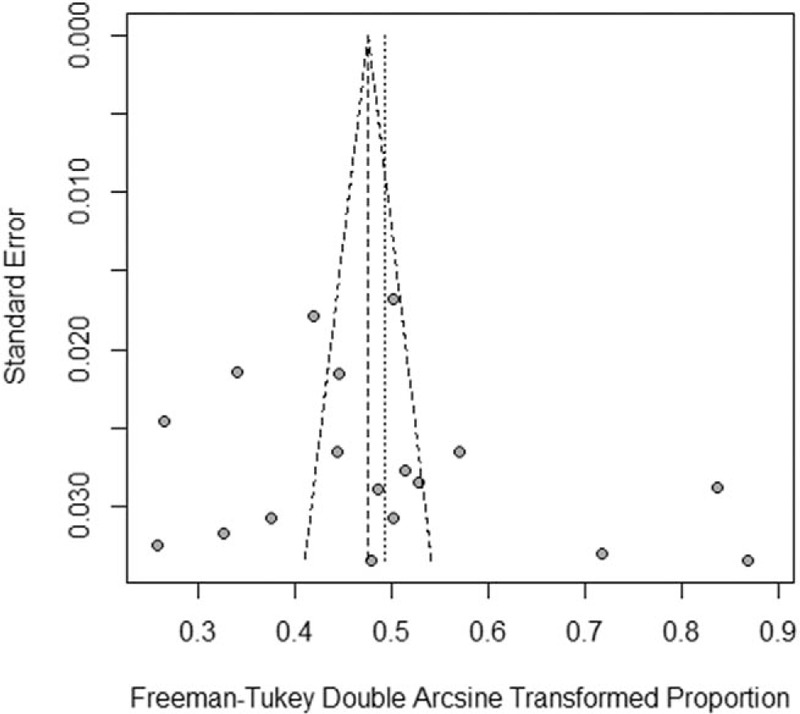
Funnel plot of the 15 studies included in this meta-analysis.
3.5. Subgroup analyses
Table 2 displays the results of subgroup analyses. The pooled prevalence of PTSD assessed at less than 1 year and at 1 year or more after RTA was 17.33% (95%CI: 12.71%–22.50%) and 18.14% (95%CI: 12.57%–24.46%), respectively. The pooled prevalence of PTSD assessed using structured interview and self-report questionnaire was 23.76% (95%CI: 14.15%–34.95%) and 19.92% (95%CI: 15.76%–24.44%), respectively. In addition, the pooled prevalence of PTSD among female and male RTA survivors was 27.61% (95%CI: 17.44%–39.08%) and 20.49% (95%CI: 12.37%–30.00%), respectively.
Table 2.
Subgroup analyses of posttraumatic stress disorder among road traffic accident survivors.
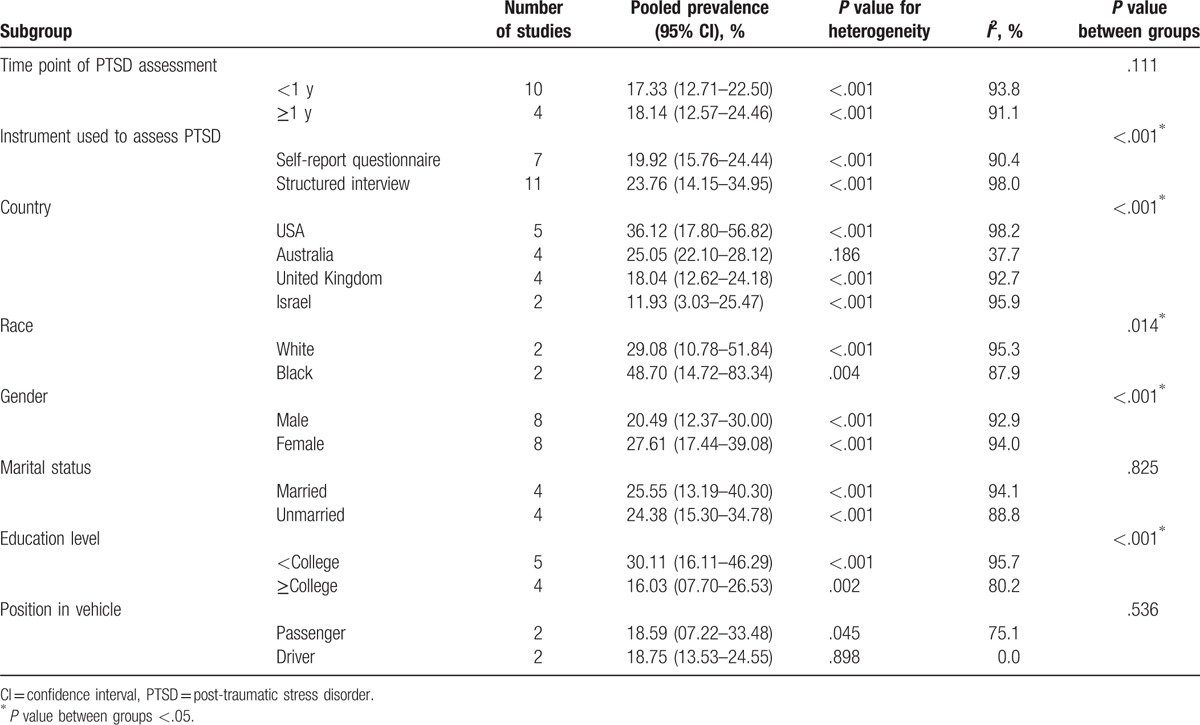
The heterogeneity was high within most subgroups. However, the heterogeneity was quite low when estimating the pooled prevalence of PTSD among RTA survivors in Australia (I2 = 37.7%, P = .186) and those who occupied the position of driver in a vehicle (I2 = 0.0%, P = .898). Subgroup analyses also indicated that the prevalence of PTSD among RTA survivors varied significantly across studies in relation to the instrument used to assess PTSD, country, race, gender, and education level (P < .05).
4. Discussion
This meta-analysis included 15 eligible articles conducted in 7 countries with a total of 6804 participants, of which 1489 were identified with PTSD. The reported prevalence of PTSD among RTA survivors ranged from 6.3%[15] to 58.3%[29] among eligible studies, and the pooled prevalence was 22.25% (95% CI: 16.71%–28.33%). To the best of our knowledge, this is the 1st meta-analysis to estimate the pooled prevalence of PTSD among RTA survivors.
The pooled prevalence of PTSD among RTA survivors found in this study (22.25%, 95% CI: 16.71%–28.33%) was lower than that among earthquake survivors (23.66%, 95% CI: 19.34–28.27%).[21] However, this rate was higher than that among flood survivors (15.74%, 95% CI: 11.25%–20.82%) and survivors of stroke and transient ischemic attack (13%, 95% CI: 11%–16%) found in previous meta-analyses.[37,38] The difference in the severity of trauma may account for the difference in the pooled prevalence observed among these studies.[21] Notably, many countries have witnessed a rapid increase in the number of motor vehicles over the past few decades, which may contribute a lot to the rapid increase in the occurrence of RTA.[27] Therefore, more psychological resources should be allocated to RTA survivors, and early assessment of PTSD symptoms in this population needs to be implemented urgently.
Subgroup analyses showed that the pooled prevalence of PTSD identified at less than 1 year after RTA was slightly lower than that identified at 1 year or more after RTA (17.33% vs 18.14%), but the difference was not significant. This finding was inconsistent with previous meta-analyses. Dai et al[21] found that the pooled prevalence of PTSD identified at 9 months or less after earthquake was significantly higher than that assessed at more than 9 months after earthquake (28.76% vs 19.48%). The same tendency of PTSD prevalence over time was also found in a meta-analysis focusing on survivors of stroke and transient ischemic attack.[38] One possible reason for the contradictory results found between this study and previous related studies may be the fact that the heterogeneity across studies included in the subgroup of time point of PTSD assessment in this meta-analysis was high. Specifically, the I2 statistics for studies exploring the prevalence of PTSD identified at less than 1 year after RTA was 93.8%, while for studies exploring the prevalence of PTSD identified at 1 year or more after RTA, the I2 statistics was 91.1%.
Additionally, subgroup analyses found that the prevalence of PTSD assessed using structured interview was significantly higher than that assessed using self-report questionnaire. Numerous studies have indicated that compared with the structured interview, self-report questionnaires, such as the posttraumatic checklist and posttraumatic stress symptom scale, have high specificity and sensitivity.[30,39] The difference in the PTSD prevalence found across studies using self-report questionnaire and the structured interview could be explained by the difference in sample sources. In general, studies using the structured interview were more likely to enroll participants in clinic-based venues with severe injury, while studies using the self-report questionnaires were more likely to enroll participants in population-based venues with minor injury.
Moreover, subgroup analyses indicated that the prevalence of PTSD among RTA survivors differed significantly by country and race, which may be explained by the difference in social, cultural, and biological characteristics. For example, it has been indicated that compared with the white population, African Americans were more likely to experience race-related discrimination and were also more likely to experience violent assault.[40,41] Additionally, ethnic difference in the frequency of genetic polymorphisms may lead to different prevalence of PTSD.[42–44]
Subgroup analyses also indicated that the prevalence of PTSD among RTA survivors differed significantly across gender and education levels. Specifically, female RTA survivors and less than college level of education RTA survivors were more likely to develop PTSD than their counterparts. Gender difference in PTSD could be largely attributed to gender difference in coping strategies when facing trauma, as well as gender difference in interpretation of trauma.[45–47] For example, it has been well-established that female subjects interpret trauma more negatively than their male counterparts.[45] Similarly, coping strategies for individuals with low education level were poorer than for those with high education level, thus affecting PTSD status.[48–50]
Certain limitations should be acknowledged in this study. First, this meta-analysis included 15 eligible articles with none of them considered high quality. However, the inclusion of studies with a sample size of at least 200 would enhance the representability of the samples in the included studies, thus adding more confidence when estimating the pooled prevalence. Second, the heterogeneity was high within most subgroups. Though several studies found that smoking status, previous psychiatric illness, and posttraumatic amnesia may be associated with the prevalence of PTSD among RTA survivors,[15,27,31] subgroup analyses according to these factors were unable to conduct, since very few studies have reported relevant information. Therefore, future studies need to explore more factors associated with PTSD among RTA survivors. Third, though injury severity, an important predictive factor of PTSD following RTA, was reported in many eligible articles,[26,31] it was not possible to pool studies according to injury severity since the measurement of injury severity was inconsistent and mostly based on the authors’ description of injury severity. Therefore, future studies should use standard measurements to assess injury severity, such as the New Injury Severity Score.[31]
Despite the preceding limitations, this study has several strengths. First, to the best of our knowledge, this is the first meta-analysis estimating the pooled prevalence of PTSD among RTA survivors. A reliable estimate of the prevalence of PTSD among RTA survivors may help the service providers to predict the number of survivors who may develop PTSD, thus providing timely and effective intervention strategies. Second, different prevalence found in the subgroup analyses will be helpful to identify factors associated with PTSD. Finally, low sensitivity and no risk of publication bias identified in this meta-analysis significantly add confidence when interpreting the results of this study.
5. Conclusions
The pooled prevalence of PTSD among RTA survivors was 22.25% (95% CI: 16.71%–28.33%). The prevalence of PTSD among RTA survivors varied significantly across studies in relation to the instrument used to assess PTSD, country, race, gender, and education level. The findings of this study significantly underscore the need for providing timely and effective intervention strategies for RTA survivors.
Acknowledgments
The authors thank to all authors of the eligible articles included in this meta-analysis.
Footnotes
Abbreviations: CI = confidence interval, PTSD = posttraumatic stress disorder, RTA = road traffic accident.
The authors have no funding and conflicts of interest to disclose.
References
- [1].World Health Organization, 2013. WHO global status report on road safety 2013: supporting a decade of action. World Health Organization. [Google Scholar]
- [2].Asuquo JE, Edet BE, Abang IE, et al. Depression and posttraumatic stress disorder among road traffic accident victims managed in a Tertiary hospital in Southern Nigeria. Niger J Clin Pract 2017;20:170–5. [DOI] [PubMed] [Google Scholar]
- [3].Smith B, Mackenzie-Ross S, Scragg P. Prevalence of poor psychological morbidity following a minor road traffic accident (RTA): the clinical implications of a prospective longitudinal study. Counsell Psychol Q 2007;20:149–55. [Google Scholar]
- [4].Seethalakshmi R, Dhavale HS, Gawande S, et al. Psychiatric morbidity following motor vehicle crashes: a pilot study from India. J Psychiatr Pract 2006;12:415–8. [DOI] [PubMed] [Google Scholar]
- [5].Hamanaka S, Asukai N, Kamijo Y, et al. Acute stress disorder and posttraumatic stress disorder symptoms among patients severely injured in motor vehicle accidents in Japan. Gen Hosp Psychiatry 2006;28:234–41. [DOI] [PubMed] [Google Scholar]
- [6].Ozaltin M, Kaptanoglu C, Aksaray G. Acute stress disorder and posttraumatic stress disorder after motor vehicle accidents. Turk J Psychiatry 2004;15:16–25. [PubMed] [Google Scholar]
- [7].American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 5th ed.Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- [8].Walker EA, Katon W, Russo J, et al. Health care costs associated with posttraumatic stress disorder symptoms in women. Arch Gen Psychiatry 2003;60:369–74. [DOI] [PubMed] [Google Scholar]
- [9].O’Donnell ML, Creamer M, Elliott P, et al. Health costs following motor vehicle accidents: the role of posttraumatic stress disorder. J Trauma Stress 2005;18:557–61. [DOI] [PubMed] [Google Scholar]
- [10].Dai W, Kaminga AC, Tan H, et al. Comorbidity of post-traumatic stress disorder and anxiety in flood survivors: prevalence and shared risk factors. Medicine 2017;96:e7994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Landolt MA, Vollrath ME, Gnehm HE, et al. Post-traumatic stress impacts on quality of life in children after road traffic accidents: prospective study. Aust N Z J Psychiatry 2009;43:746–53. [DOI] [PubMed] [Google Scholar]
- [12].Bartoli F, Carra G, Crocamo C, et al. Metabolic syndrome in people suffering from posttraumatic stress disorder: a systematic review and meta-analysis. Metab Syndr Relat Disord 2013;11:301–8. [DOI] [PubMed] [Google Scholar]
- [13].Bartoli F, Crocamo C, Alamia A, et al. Posttraumatic stress disorder and risk of obesity: systematic review and meta-analysis. J Clin Psychiatry 2015;76:e1253–61. [DOI] [PubMed] [Google Scholar]
- [14].Chan AO, Medicine M, Air TM, et al. Posttraumatic stress disorder and its impact on the economic and health costs of motor vehicle accidents in South Australia. J Clin Psychiatry 2003;64:175–81. [DOI] [PubMed] [Google Scholar]
- [15].Hamazaki K, Nishi D, Yonemoto N, et al. The role of high-density lipoprotein cholesterol in risk for posttraumatic stress disorder: taking a nutritional approach toward universal prevention. Eur Psychiatry 2014;29:408–13. [DOI] [PubMed] [Google Scholar]
- [16].Kupchik M, Strous RD, Erez R, et al. Demographic and clinical characteristics of motor vehicle accident victims in the community general health outpatient clinic: a comparison of PTSD and non-PTSD subjects. Depress Anxiety 2007;24:244–50. [DOI] [PubMed] [Google Scholar]
- [17].Yang LS, Zhang ZH, Sun L, et al. Prevalence of suicide attempts among college students in China: a meta-analysis. PloS One 2015;10:e0116303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hu J, Dong Y, Chen X, et al. Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry 2015;61:78–89. [DOI] [PubMed] [Google Scholar]
- [19].Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646–54. [DOI] [PubMed] [Google Scholar]
- [20].Li X, Wang J, Zhou J, et al. The association between post-traumatic stress disorder and shorter telomere length: a systematic review and meta-analysis. J Affect Disord 2017;218:322–6. [DOI] [PubMed] [Google Scholar]
- [21].Dai W, Chen L, Lai Z, et al. The incidence of post-traumatic stress disorder among survivors after earthquakes:a systematic review and meta-analysis. BMC Psychiatry 2016;16:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Dai W, Ye L, Liu A, et al. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: a meta-analysis. Medicine 2017;96:e8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [24].Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. J Abnorm Psychol 1998;107:508–19. [DOI] [PubMed] [Google Scholar]
- [25].Holeva V, Tarrier N, Wells A. Prevalence and predictors of acute stress disorder and PTSD following road traffic accidents: thought control strategies and social support. Behav Ther 2001;32:65–83. [Google Scholar]
- [26].Mayou RA, Ehlers A, Bryant B. Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behav Res Ther 2002;40:665–75. [DOI] [PubMed] [Google Scholar]
- [27].Ongecha-Owuor FA, Kathuku DM, Othieno CJ, et al. Post traumatic stress disorder among motor vehicle accident survivors attending the orthopaedic and trauma clinic at Kenyatta National Hospital, Nairobi. East Afr Med J 2004;81:362–6. [DOI] [PubMed] [Google Scholar]
- [28].Shalev AY, Freedman S. PTSD following terrorist attacks: a prospective evaluation. Am J Psychiatry 2005;162:1188–91. [DOI] [PubMed] [Google Scholar]
- [29].Beck JG, Palyo SA, Canna MA, et al. What factors are associated with the maintenance of PTSD after a motor vehicle accident? The role of sex differences in a help-seeking population. J Behav Ther Exp Psychiatry 2006;37:256–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Coffey SF, Gudmundsdottir B, Beck JG, et al. Screening for PTSD in motor vehicle accident survivors using the PSS-SR and IES. J Trauma Stress 2006;19:119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chossegros L, Hours M, Charnay P, et al. Predictive factors of chronic post-traumatic stress disorder 6 months after a road traffic accident. Accid Anal Prev 2011;43:471–7. [DOI] [PubMed] [Google Scholar]
- [32].Hruska B, Irish LA, Pacella ML, et al. PTSD symptom severity and psychiatric comorbidity in recent motor vehicle accident victims: a latent class analysis. J Anxiety Disord 2014;28:644–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Naim R, Wald I, Lior A, et al. Perturbed threat monitoring following a traumatic event predicts risk for post-traumatic stress disorder. Psychol Med 2014;44:2077–84. [DOI] [PubMed] [Google Scholar]
- [34].Beck JG, Jones JM, Reich CM, et al. Understanding the role of dysfunctional post-trauma cognitions in the co-occurrence of Posttraumatic Stress Disorder and Generalized Anxiety Disorder: two trauma samples. Behav Res Ther 2015;70:23–31. [DOI] [PubMed] [Google Scholar]
- [35].Kenardy J, Heron-Delaney M, Hendrikz J, et al. Recovery trajectories for long-term health-related quality of life following a road traffic crash injury: results from the UQ SuPPORT study. J Affect Disord 2017;214:8–14. [DOI] [PubMed] [Google Scholar]
- [36].Platts-Mills TF, Nebolisa BC, Flannigan SA, et al. Post-traumatic stress disorder among older adults experiencing motor vehicle collision: a multicenter prospective cohort study. Am J Geriatr Psychiatry 2017;25:953–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chen L, Liu A. The incidence of posttraumatic stress disorder after floods: a meta-analysis. Disaster Med Public Health Prep 2015;9:329–33. [DOI] [PubMed] [Google Scholar]
- [38].Edmondson D, Richardson S, Fausett JK, et al. Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. PloS One 2013;8:e66435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Karstoft KI, Andersen SB, Bertelsen M, et al. Diagnostic accuracy of the posttraumatic stress disorder checklist-civilian version in a representative military sample. Psychol Assess 2014;26:321–5. [DOI] [PubMed] [Google Scholar]
- [40].Schwartz AC, Bradley RL, Sexton M, et al. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatr Serv 2005;56:212–5. [DOI] [PubMed] [Google Scholar]
- [41].Breslau N, Chilcoat HD, Kessler RC, et al. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry 1999;156:902–7. [DOI] [PubMed] [Google Scholar]
- [42].Garakani A, Mathew SJ, Charney DS. Neurobiology of anxiety disorders and implications for treatment. Mt Sinai J Med 2006;73:941–9. [PubMed] [Google Scholar]
- [43].Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol 2009;5:374–81. [DOI] [PubMed] [Google Scholar]
- [44].Dai W, Kaminga AC, Wu X, et al. Brain-derived neurotropic factor Val66Met polymorphism and posttraumatic stress disorder among survivors of the 1998 Dongting Lake Flood in China. Biomed Res Int 2017;2017:4569698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Muldoon OT. Perceptions of stressful life events in Northern Irish school children: a longitudinal study. J Child Psychol Psychiatry 2003;44:193–201. [DOI] [PubMed] [Google Scholar]
- [46].Dai W, Kaminga AC, Tan H, et al. Long-term psychological outcomes of flood survivors of hard-hit areas of the 1998 Dongting Lake flood in China: prevalence and risk factors. PloS One 2017;12:e0171557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Dai W, Wang J, Kaminga AC, et al. Predictors of recovery from post-traumatic stress disorder after the dongting lake flood in China: a 13-14 year follow-up study. BMC Psychiatry 2016;16:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Lilly MM, Pole N, Best SR, et al. Gender and PTSD: what can we learn from female police officers? J Anxiety Disord 2009;23:767–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Priebe S, Grappasonni I, Mari M, et al. Posttraumatic stress disorder six months after an earthquake: findings from a community sample in a rural region in Italy. Soc Psychiatry Psychiatr Epidemiol 2009;44:393–7. [DOI] [PubMed] [Google Scholar]
- [50].Dai W, Chen L, Tan H, et al. Association between social support and recovery from post-traumatic stress disorder after flood: a 13-14 year follow-up study in Hunan, China. BMC Public Health 2016;16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]


