Abstract
Diabetic kidney disease (DKD) is a common complication of diabetes, which is characterized by albuminuria, impaired glomerular filtration rate or a combination of the two. The aim of the present study was to identify the potential key genes involved in DKD progression and to subsequently investigate the underlying mechanism involved in DKD development. The array data of GSE30528 including 9 DKD and 13 control samples was downloaded from the Gene Expression Omnibus database. The differentially expressed genes (DEGs) in DKD glomerular and tubular kidney biopsy tissues were compared with normal tissues, and were analyzed using the limma package. Gene Ontology (GO) annotation and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses were performed for DEGs using the GO Function software in Bioconductor. The protein-protein interaction (PPI) network was then constructed using Cytoscape software. A total of 426 genes (115 up- and 311 downregulated) were differentially expressed between the DKD and normal tissue samples. The PPI network was constructed with 184 nodes and 335 edges. Vascular endothelial growth factor A (VEGFA), α-actinin-4 (ACTN4), proto-oncogene, Src family tyrosine kinase (FYN), collagen, type 1, α2 (COL1A2) and insulin-like growth factor 1 (IGF1) were hub proteins. Major histocompatibility complex, class II, DP α1 (HLA-DPA1) was the common gene enriched in the rheumatoid arthritis and systemic lupus erythematosus pathways, and the immune response was a GO term enriched in module A. VEGFA, ACTN4, FYN, COL1A2, IGF1 and HLA-DPA1 may be potential key genes associated with the progression of DKD, and immune mechanisms may serve a part in DKD development.
Keywords: diabetic kidney disease, differentially expressed genes, Kyoto Encyclopedia of Genes and Genomes pathway, protein-protein interaction network, key genes
Introduction
Diabetic kidney disease (DKD) is a common complication of diabetes, which is characterized by albuminuria, an impaired glomerular filtration rate (GFR) or a combination of the two (1,2). DKD accounts for ~50% of all cases of end-stage renal disease (ESRD) in the United States and the US ESRD program is a large medical expense/economic burden and costs a great amount of money to run. However, a number of genes closely associated with DKD development have yet to be identified despite many years of intensive study (3). Therefore, the identification of genes associated with DKD development is urgently required, as well as the subsequent elucidation of its molecular mechanism.
Some advancements have been made in the elucidation of the pathological mechanism involved in the development of DKD. The loss of podocytes is an early feature of DKD (4). The levels of almost all podocyte-specific genes including genes for congenital nephrotic syndrome of the finish type (NPHS1), glomerular podocin (NPHS2), the Wilm's tumor gene (WT1) and vascular endothelial growth factor (VEGF) are all severely reduced in DKD (3). Some other studies have also demonstrated that NPHS1 (5,6), NPHS2 (7), bone morphogenetic protein 7 (8), WT1 (4) and VEGF (9,10) are decreased in DKD. In addition, tubulointerstitial fibrosis is a prominent feature of progressive DKD and is likely to be one of the final common pathways leading to the development of ESRD, with patients subsequently requiring dialysis or transplantation (11,12). A previous study revealed that using angiotensin-converting-enzyme-inhibitors and angiotensin II receptor antagonists in patients with diabetes mellitus can respectively improve mortality and delay the progression of DKD (13). In addition, a human genetic study highlighted that the complement system potentially serves a role in low-grade inflammation and the development of DKD (14). Therefore, the aim of the present study was to identify the key genes associated with the development of DKD and elucidate its underlying mechanism.
In the present study, the microarray data of GSE30528 was downloaded the from Gene Expression Omnibus database (GEO; www.ncbi.nlm.nih.gov/geo/). The gene expression profiles in DKD were analyzed and functional analysis was performed for differentially expressed genes (DEGs) in DKD glomerular and tubular kidney biopsy tissues in comparison with normal tissues. In addition, the protein-protein interaction (PPI) network was also constructed. These results were used to discover the key genes associated with DKD development and to clarify the underlying mechanism.
Materials and methods
Affymetrix microarray data
The array data for GSE30528 was downloaded from the GEO database, which was first recorded by Woroniecka et al (3) and was based on the GPL571 platform (Affymetrix Human Genome U133A 2.0 Array; Affymetrix, Inc.; Thermo Fisher Scientific, Inc., Waltham, MA, USA). A total of 44 samples were used to develop the original array data, and of these 9 DKD [age, 64±13.56 years; 5 females, 4 males; body mass index (BMI), 32.74±7.9 kg/m2] and 13 healthy, disease-free control samples (age, 51.38±12.01 years; 5 females, 8 males; BMI, 29.59±9.08 kg/m2) were selected for analysis in the present study.
Data processing and DEG analysis
The raw expression data was preprocessed using the robust multiarray average algorithm (15) and the Affy package in Bioconductor (bioconductor.org/packages/release/bioc/html/affy.html); the expression levels of the probes were then obtained. If several probes mapped to one gene symbol, then the mean value was set as the final expression value of this gene. The DEGs in DKD glomerular and tubular kidney biopsy tissues where then compared with normal tissues using the limma package (16). |logFC| >1 and P<0.05 were considered as the cutoff criterion.
Gene Ontology (GO) and pathway enrichment analysis
GO is used for the unification of biology, collecting defined, structured and controlled vocabulary for gene annotation, which mainly includes the following 3 categories: Molecular function, biological process and cellular component (17). The Kyoto Encyclopedia of Genes and Genomes (KEGG) is a database for the classification of relevant gene sets into their respective pathways (18).
In order to analyze the DEGs on a functional level, GO annotation and KEGG pathway enrichment analyses were performed for DEGs using GO Function version 1.24.0 (19) software in Bioconductor version 3.5 (www.bioconductor.org/packages/release/bioc/html/GOFunction.html), and gene annotation information was obtained from the org. Hs. eg. db and GO. db package. P<0.05 and gene counts >2 were set as the cut off values.
PPI network analysis
The Search Tool for the Retrieval of Interacting Genes (STRING) database provides the experimental and predicted interaction information of proteins (20). Protein pair interactions in STRING were presented with a combined score. The DEGs were mapped into PPIs and a combined score of >0.7 was identified as the cutoff standard for the important protein pairs. The PPI network was constructed using Cytoscape software version 2.8.2 (www.cytoscape.org/) (21).
Module analysis
ClusterONE version 1.0 (www.paccanarolab.org/cluster-one/) in the Cytoscape software package was used to analyze the PPI network modules with a minimum size of 3 and a minimum density of 0.5. Modules with P<0.01 were set as significant clustering modules.
Results
Data processing and DEGs analysis
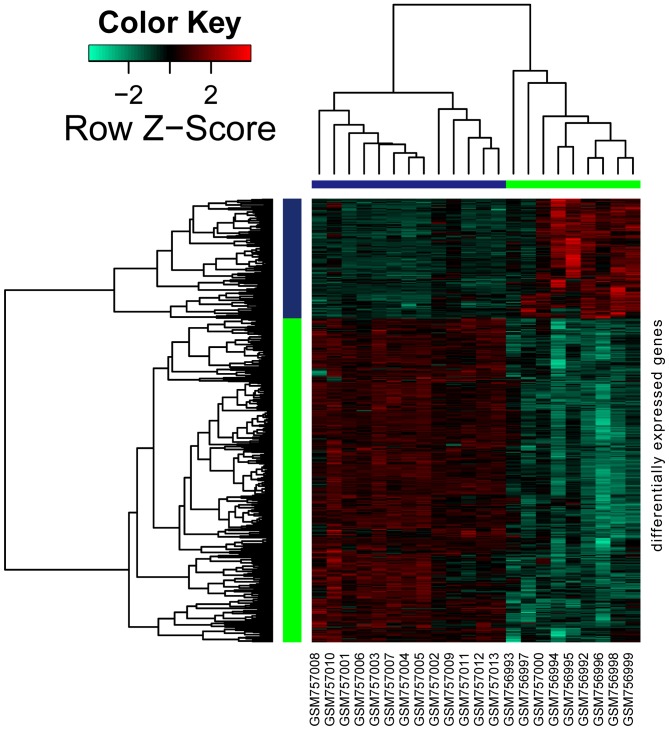
As shown in Fig. 1, a total of 426 genes were differentially expressed in DKD samples when compared with normal samples, amongst which 115 genes were upregulated and 311 were downregulated.
Figure 1.
A heat map of the differentially expressed genes identified. Horizontal band with the tree at the top: blue, normal samples; green, diabetes samples; vertical band with the tree on the side: blue, upregulated genes; green, downregulated genes.
GO and pathway enrichment analysis
GO and KEGG pathway analyses were performed for upregulated and downregulated DEGs. The top 5 GO terms are shown in Table I. The overrepresented GO terms of upregulated DEGs were primarily associated with extracellular region, antigen binding, extracellular space, the defense response, the immune response and peptidase regulator activity (Table IA). The downregulated DEGs were mainly involved in cardiovascular system development, circulatory system development, actin cytoskeleton, cell junction, cytoskeletal protein binding and integrin binding (Table IB).
Table I.
Gene Ontology analysis for differentially expressed genes.
| A, Upregulated | |||
|---|---|---|---|
| Term | Description | Counts (n) | P-valuea |
| GO-BP terms | |||
| GO:0006952 | Defense response | 44 | <0.0005 |
| GO:0006955 | Immune response | 41 | 2.22×10−16 |
| GO:0002376 | Immune system process | 50 | 3.00×10−15 |
| GO:0001775 | Cell activation | 31 | 1.37×10−14 |
| GO:0045321 | Leukocyte activation | 26 | 1.76×10−13 |
| GO-CC terms | |||
| GO:0005576 | Extracellular region | 63 | 2.06×10−12 |
| GO:0005615 | Extracellular space | 32 | 4.37×10−12 |
| GO:0031982 | Vesicle | 53 | 9.90×10−11 |
| GO:0031988 | Membrane-bounded vesicle | 52 | 1.13×10−10 |
| GO:0044421 | Extracellular region part | 53 | 3.50×10−10 |
| GO-MF terms | |||
| GO:0003823 | Antigen binding | 8 | 2.97×10−07 |
| GO:0061134 | Peptidase regulator activity | 10 | 6.67×10−07 |
| GO:0005539 | Glycosaminoglycan binding | 9 | 2.84×10−07 |
| GO:0004866 | Endopeptidase inhibitor activity | 8 | |
| 8092×10−06 | |||
| GO:0061135 | Endopeptidase regulator activity | 8 | 1.11×10−05 |
| B, Downregulated | |||
| Term | Description | Counts (n) | P-valuea |
| GO-BP terms | |||
| GO:0072358 | Cardiovascular system development | 50 | 3.77×10−15 |
| GO:0072359 | Circulatory system development | 50 | 3.77×10−15 |
| GO:0009653 | Anatomical structure morphogenesis | 91 | 4.66×10−15 |
| GO:0048731 | System development | 121 | 3.40×10−14 |
| GO:0032502 | Developmental process | 147 | 5.66×10−14 |
| GO-CC terms | |||
| GO:0015629 | Actin cytoskeleton | 31 | 1.79×10−12 |
| GO:0030054 | Cell junction | 47 | 6.04×10−10 |
| GO:0070161 | Anchoring junction | 28 | 1.82×10−09 |
| GO:0005912 | Adherens junction | 27 | 3.39×10−09 |
| GO:0044421 | Extracellular region part | 98 | 3.00×10−08 |
| GO-MF terms | |||
| GO:0008092 | Cytoskeletal protein binding | 40 | 9.40×10−11 |
| GO:0005178 | Integrin binding | 12 | 1.23×10−07 |
| GO:0032403 | Protein complex binding | 35 | 4.24×10−07 |
| GO:0050839 | Cell adhesion molecule binding | 14 | 8.04×10−07 |
| GO:0003779 | Actin binding | 21 | 1.40×10−06 |
P<0.00001 vs. normal matched tissues. GO, Gene Ontology; BP, biological process; CC, cellular component; MF, molecular function; Term, the identification number of GO; Description, the name of the GO term; Counts, the number of genes enriched in the GO term.
The upregulated DEGs were mainly enriched in 17 KEGG pathways, including primary immunodeficiency, extracellular matrix-receptor interactions, rheumatoid arthritis and systemic lupus erythematosus (Table IIA). In addition, major histocompatibility complex, class II, DP α1 (HLA-DPA1) was the common gene in the rheumatoid arthritis and systemic lupus erythematosus pathways. The downregulated DEGs were mainly enriched in 16 KEGG pathways, such as tight junction and adherens junction.
Table II.
Kyoto Encyclopedia of Genes and Genomes pathway enrichment analysis of the top 10 DEGs.
| A, Upregulated | |||
|---|---|---|---|
| Term | Description | Counts (n) | P-value |
| 5150 | Staphylococcus aureus infection | 5 | 1.89×10−04c |
| 5020 | Prion diseases | 4 | 3.58×10−04c |
| 5340 | Primary immunodeficiency | 4 | 3.58×10−04c |
| 4512 | Extracellular matrix-receptor interaction | 5 | 1.42×10−03b |
| 5323 | Rheumatoid arthritis | 5 | 1.92×10−03b |
| 5142 | Chagas disease (American trypanosomiasis) | 5 | 3.45×10−03b |
| 4610 | Complement and coagulation cascades | 4 | 4.61×10−03b |
| 4974 | Protein digestion and absorption | 4 | 8.12×10−03b |
| 5322 | Systemic lupus erythematosus | 5 | 1.06×10−02a |
| 4640 | Hematopoietic cell lineage | 4 | 1.08×10−02a |
| B, Downregulated | |||
| Term | Description | Counts (n) | P-value |
| 4520 | Adherens junction | 8 | 3.85×10−05d |
| 4510 | Focal adhesion | 13 | 4.51×10−05d |
| 4810 | Regulation of actin cytoskeleton | 13 | 8.65×10−05d |
| 4530 | Tight junction | 9 | 5.06×10−04c |
| 5410 | Hypertrophic cardiomyopathy | 7 | 6.17×10−04c |
| 5414 | Dilated cardiomyopathy | 7 | 1.00×10−03b |
| 5412 | Arrhythmogenic right ventricular cardiomyopathy | 6 | 1.87×10−03b |
| 4610 | Complement and coagulation cascades | 5 | 7.26×10−03b |
| 4360 | Axon guidance | 7 | 7.65×10−03b |
| 5200 | Pathways in cancer | 12 | 1.21×10−02a |
P<0.05
P<0.01
P<0.001
P<0.0001 vs. normal matched tissues. KEGG, Kyoto Encyclopedia of Genes and Genomes; Term, the identification number of the KEGG pathway; Description, the name of the KEGG pathway; Counts, the number of genes enriched in the KEGG pathway.
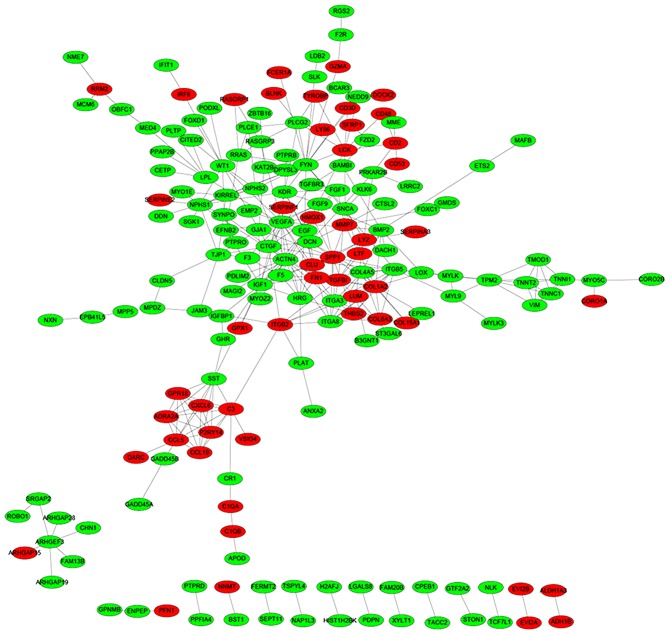
PPI network analysis
Based on the STRING database, a total of 335 protein pairs with a combined score of >0.7 were obtained. As presented in Fig. 2, the PPI network was constructed with 335 edges and 184 nodes. The nodes of VEGFA (degree score, 19), α-actinin-4 (ACTN4; degree score, 17), proto-oncogene, Src family tyrosine kinase (FYN; degree score, 17), collagen, type 1, α2 (COL1A2; degree score, 15) and insulin-like growth factor 1 (IGF1; degree score, 15) were hub proteins in the network.
Figure 2.
Protein-protein interaction networks of differentially expressed genes. The red nodes represent the upregulated genes and the green nodes represent the downregulated genes.
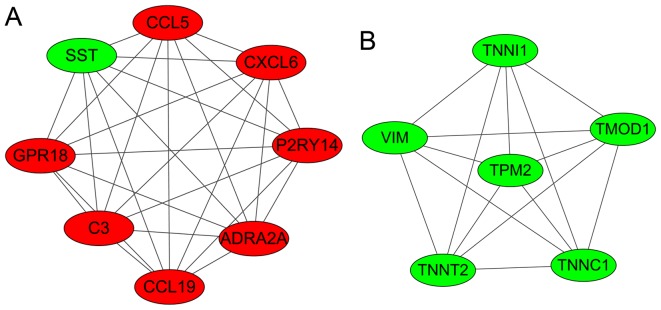
Modules analysis
Two significant clustering modules were obtained using ClusterONE software (Fig. 3). A total of 8 and 6 nodes were enriched in modules A and B, respectively. As shown in Table III, nodes in module A (density, 1.0; quality, 0.800; P=1.606×10−4) were mainly enriched in GO: G-protein coupled receptor protein signaling pathway, cell surface receptor linked signal transduction, the immune response, the chemokine signaling pathway and the cytokine-cytokine receptor interaction pathway. Nodes in module B (density, 1.0; quality, 0.789; P=0.001) were mainly enriched in GO: regulation of ATPase activity, regulation of system process and regulation of hydrolase activity.
Figure 3.
Two significant clustering modules (modules A and B) that were identified in the PPI networks. The red nodes represent the upregulated genes and the green nodes represent the downregulated genes. SST, somatostatin precursor; CCL5, chemokine C-C motif ligand 5; CXCL6, chemokine C-X-C motif ligand 6; P2RY14, P2Y purinoceptor 14; ADRA2A, adrenoceptor α2A; C3, complement component 3; GPR18, G-protein-coupled receptor 18; VIM, vimentin; TNNI1, troponin I1; TMOD1, tropomodulin 1; TNNC1, troponin C1; TNNT2, troponin T2; TPM2, tropomyosin 2β.
Table III.
Functional enrichment analysis of protein-protein interaction network clustering modules.
| Term | Description | Counts (n) | P-value |
|---|---|---|---|
| Module A | |||
| GO_BP:0007186 | G-protein coupled receptor protein signaling pathway | 8 | 2.67×10−08a |
| GO_BP:0007166 | Cell surface receptor linked signal transduction | 8 | 9.06×10−07a |
| GO_BP:0006955 | Immune response | 5 | 2.08×10−04b |
| KEGG_ hsa04062 | Chemokine signaling pathway | 3 | 1.25×10−02c |
| KEGG_ hsa04060 | Cytokine-cytokine receptor interaction | 3 | 2.38×10−02c |
| Module B | |||
| GO_BP:0043462 | Regulation of ATPase activity | 3 | 1.31×10−05d |
| GO_BP:0044057 | Regulation of system process | 3 | 4.97×10−03e |
| GO_BP:0051336 | Regulation of hydrolase activity | 3 | 5.89×10−03f |
| KEGG_ hsa04260 | Cardiac muscle contraction | 2 | 2.32×10−04b |
| KEGG_ hsa05410 | Hypertrophic cardiomyopathy | 3 | 2.76×10−04b |
| KEGG_ hsa05414 | Dilated cardiomyopathy | 2 | 3.24×10−04b |
P<0.00001
P<0.0005
P<0.05
P<0.0001
P<0.005
P<0.01vs. normal matched tissues. GO, Gene Ontology; KEGG, KEGG, Kyoto Encyclopedia of Genes and Genomes; Term, the identification number of GO-Biological Process or KEGG pathway; Description, the name of the GO- Biological Process or KEGG pathway; Counts, the number of genes enriched in GO- Biological Process or KEGG pathway.
Discussion
In the present study, using the gene expression patterns downloaded from the GEO database, 426 DEGs in DKD glomerular and tubular kidney biopsy tissues were obtained and compared with matched normal tissues, identifying 115 upregulated genes and 311 downregulated DEGs. The results demonstrated that HLA-DPA1 was the common gene enriched in the rheumatoid arthritis and systemic lupus erythematosus pathways, and the immune response was a significant GO term enriched in module A. In addition, VEGFA, ACTN4, FYN, COL1A2 and IGF1 had higher degrees and were established as hub nodes in the PPI network; they may therefore contribute to the progression of DKD.
A previous study suggested that cells in the immune system may be involved in the progression of DKD (22). Immune cells take part in vascular injury under DKD-associated conditions (23). Other previous studies have also indicated that the immune system is associated with DKD development (24–26). Primary immunodeficiency (27), rheumatoid arthritis (28) and systemic lupus erythematosus (29) are associated with the immune system. In the present study, primary immunodeficiency, rheumatoid arthritis and systemic lupus erythematosus were 3 significantly enriched pathways, and the immune response was a GO term enriched in module A. Thus, the results of the present study are in agreement with previous findings, and therefore indicate that immune mechanisms may serve a role in DKD development.
The work of Woroniecka et al (3) suggested that HLA-DPA1 was a differentially expressed transcript in the tubulointerstitium of patients with DKD when compared with normal samples. Previous studies revealed that HLA-DPA1, which is the closest centromeric gene expressed to HLA-DOα, may contribute to the differences in the associated risks of diabetes (30,31), including DKD, which is a complication of diabetes. In the present study, HLA-DPA1 was the common gene enriched in the rheumatoid arthritis and systemic lupus erythematosus pathways. Therefore, these results are in line with previous findings and suggest that HLA-DPA1 may contribute to DKD development.
In addition, VEGFA, ACTN4, FYN, COL1A2 and IGF1 were identified as hub proteins in the PPI network. VEGFA is an important angiogenic growth factor that regulates endothelial cells' permeability and vasculogenesis (32). It is also important for the differentiation, proliferation, survival and migration of endothelial cells within the glomerulus (33). Previous studies have suggested that VEGFA may serve a significant role in retaining glomerular endothelial cell function as a reduction in VEGFA levels induced abnormal remodeling of glomerular capillaries (34,35). VEGF may also serve a role in the pathogenesis of DKD (36) and the dysregulation of VEGFA may serve a pathogenic role in inducing glomerular injury (37). In DKD, VEGFA has reduced mRNA expression and may be a potential factor that can lead to the development of DKD by inducing microvascular rarefaction and tubular atrophy (9). In addition, neoangiogenesis, which is caused by overexpression of VEGFA, may stimulate the development of DKD and therefore blocking VEGFA or its signaling may ameliorate DKD (38). These findings indicate that VEGFA may serve a role in DKD progression.
ACTNs are actin-binding proteins that are critical in cell adhesion and in the organization of the cytoskeleton (39). Increasing evidence has revealed that in diabetes, there are cytoskeletal changes in podocytes. For instance, advanced glycosylation end products and high glucose can decrease the expression of ACTN4 (40), and a reduced expression of ACTN4 may lead to proteinuria (a symptom of DKD) (41). In addition, FYN is a tyrosine-specific phospho-transferase that belongs to the Src family of tyrosine protein kinases (42). FYN phosphorylation is transiently stimulated by high glucose levels (43). Src/FYN kinase inhibitors disrupt signaling molecules in the VEGF signal transduction pathway (44), and as mentioned above, VEGF may be associated with DKD; thus, FYN may in turn be involved in DKD. In addition, the accumulation of extracellular matrix proteins such as COL1A2 is a key feature of DKD (45). A previous report demonstrated that some key microRNAs (miR) act as effectors of transforming growth factor (TGF)-β and the actions of high glucose in DKD (46). In mesangial cells and the kidney, experimental diabetes was associated with the increased expression of COL1A2, and miR-192 was increased by TGF-β treatment (45). IGF1 as a growth factor receptor has been associated with type 1 DKD (47). In addition, IGF-1 has the capacity to mediate the histological changes characteristic of DKD (48). These previous studies all indicate that these proteins are associated with DKD. Therefore, the results of the present study are in agreement with these findings and provide further evidence that VEGFA, ACTN4, FYN, COL1A2 and IGF1 may serve important roles in DKD development directly or indirectly.
In conclusion, the results of the present study indicated that in addition to VEGFA, ACTN4, FYN, COL1A2, IGF1 and HLA-DPA1, immune mechanisms may also serve an important role in the development of DKD. These genes may serve as target genes for the treatment of DKD in future clinical practice. However, this conclusion has no experimental verification; therefore, further evaluation of the potential applications in clinical practice is required.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant nos. 81070578 and 81270809).
References
- 1.Association AD. Standards of medical care in diabetes-2010. Diabetes care. 2010;33(Suppl):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levin A, Rocco M. KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am J Kidney Dis. 2007;49(2 Suppl 2):S12–S154. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Woroniecka KI, Park AS, Mohtat D, Thomas DB, Pullman JM, Susztak K. Transcriptome analysis of human diabetic kidney disease. Diabetes. 2011;60:2354–2369. doi: 10.2337/db10-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Susztak K, Raff AC, Schiffer M, Böttinger EP. Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy. Diabetes. 2006;55:225–233. doi: 10.2337/diabetes.55.01.06.db05-0894. [DOI] [PubMed] [Google Scholar]
- 5.Langham RG, Kelly DJ, Cox AJ, Thomson NM, Holthöfer H, Zaoui P, Pinel N, Cordonnier DJ, Gilbert RE. Proteinuria and the expression of the podocyte slit diaphragm protein, nephrin, in diabetic nephropathy: Effects of angiotensin converting enzyme inhibition. Diabetologia. 2002;45:1572–1576. doi: 10.1007/s00125-002-0946-y. [DOI] [PubMed] [Google Scholar]
- 6.Doublier S, Salvidio G, Lupia E, Ruotsalainen V, Verzola D, Deferrari G, Camussi G. Nephrin expression is reduced in human diabetic nephropathy: Evidence for a distinct role for glycated albumin and angiotensin II. Diabetes. 2003;52:1023–1030. doi: 10.2337/diabetes.52.4.1023. [DOI] [PubMed] [Google Scholar]
- 7.Koop K, Eikmans M, Baelde HJ, Kawachi H, de Heer E, Paul LC, Bruijn JA. Expression of podocyte-associated molecules in acquired human kidney diseases. J Am Soc Nephrol. 2003;14:2063–2071. doi: 10.1097/01.ASN.0000078803.53165.C9. [DOI] [PubMed] [Google Scholar]
- 8.Turk T, Leeuwis JW, Gray J, Torti SV, Lyons KM, Nguyen TQ, Goldschmeding R. BMP signaling and podocyte markers are decreased in human diabetic nephropathy in association with CTGF overexpression. J Histochem Cytochem. 2009;57:623–631. doi: 10.1369/jhc.2009.953224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindenmeyer MT, Kretzler M, Boucherot A, Berra S, Yasuda Y, Henger A, Eichinger F, Gaiser S, Schmid H, Rastaldi MP, et al. Interstitial vascular rarefaction and reduced VEGF-A expression in human diabetic nephropathy. J Am Soc Nephrol. 2007;18:1765–1776. doi: 10.1681/ASN.2006121304. [DOI] [PubMed] [Google Scholar]
- 10.Hohenstein B, Hausknecht B, Boehmer K, Riess R, Brekken RA, Hugo CP. Local VEGF activity but not VEGF expression is tightly regulated during diabetic nephropathy in man. Kidney Int. 2006;69:1654–1661. doi: 10.1038/sj.ki.5000294. [DOI] [PubMed] [Google Scholar]
- 11.Nath KA. The tubulointerstitium in progressive renal disease. Kidney Int. 1998;54:992–994. doi: 10.1046/j.1523-1755.1998.00079.x. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert RE, Cooper ME. The tubulointerstitium in progressive diabetic kidney disease: More than an aftermath of glomerular injury? Kidney Int. 1999;56:1627–1637. doi: 10.1046/j.1523-1755.1999.00721.x. [DOI] [PubMed] [Google Scholar]
- 13.Strippoli GF, Craig M, Deeks JJ, Schena FP, Craig JC. Effects of angiotensin converting enzyme inhibitors and angiotensin II receptor antagonists on mortality and renal outcomes in diabetic nephropathy: Systematic review. BMJ. 2004;329:828. doi: 10.1136/bmj.38237.585000.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen TK, Forsblom C, Saraheimo M, Thorn L, Wadén J, Høyem P, Østergaard J, Flyvbjerg A, Groop PH, FinnDiane Study Group Association between mannose-binding lectin, high-sensitivity C-reactive protein and the progression of diabetic nephropathy in type 1 diabetes. Diabetologia. 2010;53:1517–1524. doi: 10.1007/s00125-010-1742-8. [DOI] [PubMed] [Google Scholar]
- 15.Gautier L, Cope L, Bolstad BM, Irizarry RA. affy-analysis of Affymetrix GeneChip data at the probe level. Bioinformatics. 2004;20:307–315. doi: 10.1093/bioinformatics/btg405. [DOI] [PubMed] [Google Scholar]
- 16.Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, Smyth GK. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, et al. Gene ontology: Tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altermann E, Klaenhammer TR. PathwayVoyager: Pathway mapping using the Kyoto Encyclopedia of Genes and Genomes (KEGG) database. BMC Genomics. 2005;6:60. doi: 10.1186/1471-2164-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J, Zhou X, Zhu J, Gu Y, Zhao W, Zou J, Guo Z. GO-function: Deriving biologically relevant functions from statistically significant functions. Brief Bioinform. 2012;13:216–227. doi: 10.1093/bib/bbr041. [DOI] [PubMed] [Google Scholar]
- 20.Szklarczyk D, Franceschini A, Kuhn M, Simonovic M, Roth A, Minguez P, Doerks T, Stark M, Muller J, Bork P, et al. The STRING database in 2011: Functional interaction networks of proteins, globally integrated and scored. Nucleic Acids Res. 2011;39:D561–D568. doi: 10.1093/nar/gkq973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kohl M, Wiese S, Warscheid B. Cytoscape: Software for visualization and analysis of biological networks. Methods Mol Biol. 2011;696:291–303. doi: 10.1007/978-1-60761-987-1_18. [DOI] [PubMed] [Google Scholar]
- 22.Ichinose K, Kawasaki E, Eguchi K. Recent advancement of understanding pathogenesis of type 1 diabetes and potential relevance to diabetic nephropathy. Am J Nephrol. 2007;27:554–564. doi: 10.1159/000107758. [DOI] [PubMed] [Google Scholar]
- 23.Galkina E, Ley K. Leukocyte recruitment and vascular injury in diabetic nephropathy. J Am Soc Nephrol. 2006;17:368–377. doi: 10.1681/ASN.2005080859. [DOI] [PubMed] [Google Scholar]
- 24.Chow F, Ozols E, Nikolic-Paterson DJ, Atkins RC, Tesch GH. Macrophages in mouse type 2 diabetic nephropathy: Correlation with diabetic state and progressive renal injury. Kidney Int. 2004;65:116–128. doi: 10.1111/j.1523-1755.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- 25.Tuttle KR. Linking metabolism and immunology: Diabetic nephropathy is an inflammatory disease. J Am Soc Nephrol. 2005;16:1537–1538. doi: 10.1681/ASN.2005040393. [DOI] [PubMed] [Google Scholar]
- 26.Mora C, Navarro JF. Inflammation and diabetic nephropathy. Curr Diab Rep. 2006;6:463–468. doi: 10.1007/s11892-006-0080-1. [DOI] [PubMed] [Google Scholar]
- 27.Johnston SL, Virgo PF, Unsworth DJ. Type 1 diabetes mellitus masking primary antibody deficiency. J Clin Pathol. 2000;53:236–237. doi: 10.1136/jcp.53.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prevoo ML, Van't Hof MA, Kuper HH, Van Leeuwen MA, Van de Putte LB, Van Riel PL. Modified disease activity scores that include twenty-eight-joint counts, development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 29.Feng PH. Systemic lupus erythematosus: the face of Asia. Ann N Y Acad Sci. 2007;1108:114–120. doi: 10.1196/annals.1422.013. [DOI] [PubMed] [Google Scholar]
- 30.Varney MD, Valdes AM, Carlson JA, Noble JA, Tait BD, Bonella P, Lavant E, Fear AL, Louey A, Moonsamy P, et al. HLA DPA1, DPB1 alleles and haplotypes contribute to the risk associated with type 1 diabetes: Analysis of the type 1 diabetes genetics consortium families. Diabetes. 2010;59:2055–2062. doi: 10.2337/db09-0680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Santin I, Castellanos-Rubio A, Aransay AM, Gutierrez G, Gaztambide S, Rica I, Vicario JL, Noble JA, Castaño L, Bilbao JR. Exploring the diabetogenicity of the HLA-B18-DR3 CEH: Independent association with T1D genetic risk close to HLA-DOA. Genes Immun. 2009;10:596–600. doi: 10.1038/gene.2009.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dvorak HF, Brown LF, Detmar M, Dvorak AM. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol. 1995;146:1029–1039. [PMC free article] [PubMed] [Google Scholar]
- 33.Schrijvers BF, Flyvbjerg A, De Vriese AS. The role of vascular endothelial growth factor (VEGF) in renal pathophysiology. Kidney Int. 2004;65:2003–2017. doi: 10.1111/j.1523-1755.2004.00621.x. [DOI] [PubMed] [Google Scholar]
- 34.Baelde HJ, Eikmans M, Doran PP, Lappin DW, de Heer E, Bruijn JA. Gene expression profiling in glomeruli from human kidneys with diabetic nephropathy. Am J Kidney Dis. 2004;43:636–650. doi: 10.1053/j.ajkd.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 35.Bortoloso E, Del Prete D, Vestra M Dalla, Gambaro G, Saller A, Antonucci F, Baggio B, Anglani F, Fioretto P. Quantitave and qualitative changes in vascular endothelial growth factor gene expression in glomeruli of patients with type 2 diabetes. Eur J Endocrinol. 2004;150:799–807. doi: 10.1530/eje.0.1500799. [DOI] [PubMed] [Google Scholar]
- 36.Cha DR, Kim NH, Yoon JW, Jo SK, Cho WY, Kim HK, Won NH. Role of vascular endothelial growth factor in diabetic nephropathy. Kidney Int Suppl. 2000;77:S104–S112. doi: 10.1046/j.1523-1755.2000.07717.x. [DOI] [PubMed] [Google Scholar]
- 37.Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, Gerber HP, Kikkawa Y, Miner JH, Quaggin SE. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003;111:707–716. doi: 10.1172/JCI17423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caldwell RB, Bartoli M, Behzadian MA, El-Remessy AE, Al-Shabrawey M, Platt DH, Caldwell RW. Vascular endothelial growth factor and diabetic retinopathy: Pathophysiological mechanisms and treatment perspectives. Diabetes Metab Res Rev. 2003;19:442–455. doi: 10.1002/dmrr.415. [DOI] [PubMed] [Google Scholar]
- 39.Nikolopoulos SN, Spengler BA, Kisselbach K, Evans AE, Biedler JL, Ross RA. The human non-muscle alpha-actinin protein encoded by the ACTN4 gene suppresses tumorigenicity of human neuroblastoma cells. Oncogene. 2000;19:380–386. doi: 10.1038/sj.onc.1203310. [DOI] [PubMed] [Google Scholar]
- 40.HA TS. High glucose and advanced glycosylated end-products affect the expression of alpha-actinin-4 in glomerular epithelial cells. Nephrology (Carlton) 2006;11:435–441. doi: 10.1111/j.1440-1797.2006.00668.x. [DOI] [PubMed] [Google Scholar]
- 41.Jefferson JA, Shankland SJ, Pichler RH. Proteinuria in diabetic kidney disease: A mechanistic viewpoint. Kidney Int. 2008;74:22–36. doi: 10.1038/ki.2008.128. [DOI] [PubMed] [Google Scholar]
- 42.Resh MD. Fyn, a Src family tyrosine kinase. Int J Biochem Cell Biol. 1998;30:1159–1162. doi: 10.1016/S1357-2725(98)00089-2. [DOI] [PubMed] [Google Scholar]
- 43.Taniguchi K, Xia L, Goldberg HJ, Lee KW, Shah A, Stavar L, Masson EA, Momen A, Shikatani EA, John R, et al. Inhibition of Src kinase blocks high glucose-induced EGFR transactivation and collagen synthesis in mesangial cells and prevents diabetic nephropathy in Mice. Diabetes. 2013;62:3874–3886. doi: 10.2337/db12-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van Nieuw Amerongen GP, van Hinsbergh VW. Targets for pharmacological intervention of endothelial hyperpermeability and barrier function. Vascular pharmacol. 2002;39:257–272. doi: 10.1016/S1537-1891(03)00014-4. [DOI] [PubMed] [Google Scholar]
- 45.Kato M, Zhang J, Wang M, Lanting L, Yuan H, Rossi JJ, Natarajan R. MicroRNA-192 in diabetic kidney glomeruli and its function in TGF-beta-induced collagen expression via inhibition of E-box repressors; Proc Natl Acad Sci USA; 2007; pp. 3432–3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kato M, Arce L, Natarajan R. MicroRNAs and their role in progressive kidney diseases. Clin J Am Soc Nephrol. 2009;4:1255–1266. doi: 10.2215/CJN.00520109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ewens KG, George RA, Sharma K, Ziyadeh FN, Spielman RS. Assessment of 115 candidate genes for diabetic nephropathy by transmission/disequilibrium test. Diabetes. 2005;54:3305–3318. doi: 10.2337/diabetes.54.11.3305. [DOI] [PubMed] [Google Scholar]
- 48.Schreiber B, Hughes M, Groggel G. Insulin-like growth factor-1 stimulates production of mesangial cell matrix components. Clin Nephrol. 1995;43:368–374. [PubMed] [Google Scholar]