Abstract
The present study evaluated the effect of anagliptin on intimal hyperplasia following carotid artery injury in Sprague-Dawley rats. Sprague-Dawley rats weighing 280–300 g were injured using a 2F Fogarty balloon embolectomy catheter. The rats were divided into injury-(saline) and anagliptin-(10 mg/kg/day) treated groups. vascular injuries were induced in the left carotid artery, followed by evaluation of neointima formation at 28 days. The right and left carotid arteries were harvested and evaluated with histological evaluation, and the plasma activity of glucagon-like peptide 1 receptor (GLP-1), stromal cell-derived factor (SDF)-1α, interleukin (IL)-6, IL-1β and tumor necrosis factor (TNF)-α were detected by ELISA analysis. Treatment with anagliptin decreased balloon injury-induced neointima formation, compared with the injury group (P<0.01). Body weight and food consumption did not alter following treatment with anagliptin. Anagliptin caused an increase in the serum active GLP-1 concentration, compared with the injury group. In addition, serum SDF-1α was significantly decreased by treatment with anagliptin (P<0.001). Anagliptin altered the serum activity of IL-6, IL-1β and TNF-α (P<0.01). The results of the present study demonstrated that anagliptin appeared to attenuate neointimal formation by inhibiting inflammatory cytokines and chemokines following balloon injury, and that treatment with a dipeptidyl peptidase 4 inhibitor may be useful for future preclinical studies and potentially for the inhibition of thrombosis formation following percutaneous coronary intervention.
Keywords: artery injury, intimal hyperplasia, dipeptidyl peptidase 4 inhibitor, anagliptin
Introduction
Balloon angioplasty, stenting and coronary arterial bypass grafting (CABG) are common interventions for the treatment of coronary artery disease (CAD), which is the leading cause of death globally and is expected to account for 14.2% of all deaths by 2030 (1). However, these interventions are not always successful, due to the development of stent thrombosis and excessive intimal hyperplasia formation, narrowing the lumen (2). Iatrogenic trauma and damage that occurs in the vascular endothelium during angioplasty, stenting and bypass graft surgery causes the development of remodeling, which leads to the migration of proliferated smooth muscle cells (SMCs) from media to intima and connective tissue accumulation in the vasculature (3).
Endothelial cell (EC) injury is considered to be the first step towards postoperative intimal hyperplasia formation. The injured site is less capable of producing antiproliferative products and the regulation of vascular homeostasis in the vessel wall is further disturbed. The damaged area is coated with platelets and macrophages which release thrombotic factors (fibrinogen and von Willebrand factor) and growth factors (platelet-derived growth factor and transforming growth factor) (4). According to the response-to-injury theory, the mechanism that initiates intimal thickening is that the growth factors which are released from platelets and ECs adhering to the damaged vessel wall stimulate the proliferation of SMCs within the first 24 h (5), and subsequently induce the proliferated SMCs in the medial layer to migrate to the intima during the 3rd and 4th days, ultimately leading to intimal hyperplasia. A previous study demonstrated that acute injury to the intima and media may produce hyperplasia and SMC proliferation, which occur at a rate proportional to the degree of injury (6). It has been additionally observed that intimal hyperplasia forms around the injury sites following balloon angioplasty (7).
Dipeptidyl peptidase 4 (DPP-4), also termed CD26, is a widely-expressed serine peptidase that exists on the surface of various cell types, although its expression level differs among cells (8). However, in different organs and tissues, including the lung, muscle and heart, approximately all tissue DPP-4 activity is due to its presence in the microvasculature (9). In the immune system, DPP-4 is associated with T-cell signal transduction as a co-stimulatory molecule.
Anagliptin, a specific DPP-4 inhibitor, is a novel oral anti-hyperglycemic agent which has been used to treat type 2 diabetes mellitus by improving glycemic control (10). A previous study suggested that anagliptin may exert anti-atherosclerotic effects by suppressing inflammatory reactions of monocytes and stimulating the mobilization of endothelial progenitor cells (EPCs) (11). An additional study demonstrated that anagliptin may suppress plaque formation in coronary arteries with a marked reduction in macrophage accumulation, likely via its anti-inflammatory properties, while not affecting body weight (12). However, whether or not anagliptin has the effect of suppressing intimal hyperplasia following balloon injury remains to be elucidated.
The present study aimed to investigate the effects of anagliptin on the formation of intimal hyperplasia following surgical procedures performed on the left carotid artery of Sprague-Dawley rats, using the method of balloon injury.
Materials and methods
Carotid balloon injury model
Male Sprague-Dawley rats weighing 280–300 g (age, 10 weeks; n=20.) were obtained from the Animal Center of The Second Affiliated Hospital of Harbin Medical University (Harbin, China), and were maintained in groups of five animals per cage. Rats had free access to water and food and were housed with a 14-h light and 10-h dark cycle under controlled conditions (23±1°C and 55±5% humidity). Rats were randomized to the injury group (n=10) and the anagliptin group (n=10). The experimental protocol was designed in accordance with Institutional Laboratory Animal Care and Use Committee standards, and all experimental procedures performed in studies involving animals were approved by the Institutional Animal Care and Use Committee of Harbin Medical University. Animals were anesthetized by intraperitoneal injection of chloral hydrate (4%). The left common carotid artery was exposed and a 2F Fogarty balloon embolectomy catheter (Edwards Lifesciences, Irvine, CA, USA) was inserted via an external carotid arteriotomy incision. The catheter was advanced to the aortic arch, inflated with 0.2 ml air, and drawn back to the arteriotomy three times. When the catheter had been withdrawn, the proximal external carotid artery was ligated and blood flow was restored. The surgical incision was closed and the rats were allowed to recover from anesthesia. The right uninjured artery was used as control tissue.
Drug administration
Anagliptin (10 mg/kg per day; MedChem Express China, Shanghai, China) or vehicle (saline) was administered by oral injection twice daily to the rats for 28 days. The body weight of each group was measured at baseline. Food consumption was monitored daily, and treatment was begun 1 day prior to surgery, and continued for 28 days following surgery.
Tissue preparation and histological evaluation
A total of 28 days post-injury, rats were euthanized by a sodium pentobarbital overdose. The left and right carotid arteries were removed. Tissues were fixed in 4% paraformaldehyde for 30 min at 4°C, embedded in paraffin and then four sections (5 µm) were cut at multiple levels. Tissues were then dewaxed with xylene, rehydrated with decreasing concentrations of ethanol and washed with tap water. The sections were stained with hematoxylin-eosin (hematoxylin, 3 min; eosin, 3 min) and elastic van Gieson stain (Weigert, 3 min; van Gieson, 3 min; cat. no. 4033–4037; Muto Pure Chemicals Co., Ltd., Tokyo, Japan) at room temperature. Following staining, the sections were dehydrated with increasing concentrations of ethanol and xylene. Sections were examined microscopically (magnification, ×200) with an optical microscope (Olympus Corporation, Tokyo, Japan), and the cross-sectional areas of the lumen, neointima and media were determined using digital microscopy with SPOT Advanced software v5.3 (SPOT Imaging; Diagnostic Instruments, Inc., Sterling Heights, MI, USA). Intimal hyperplasia was defined as the formation of a neointimal layer medial to the internal elastic lamina. The medial area represents the area between the external elastic lamina and the internal elastic lamina. The intima-to-media ratio was calculated as the intimal area divided by the media area.
ELISA analysis
Blood samples were collected in anticoagulant-free tubes pre-operatively, and at 1, 7, 14, 21 and 28 days post-surgery in the control and anagliptin groups. Plasma was separated by centrifugation at 1,000 × g and 4°C for 10 min and was stored at −20°C for a maximum period of 1 month according to the manufacturers' protocols for the ELISA kits. Glucagon-like peptide 1 receptor (GLP-1; cat. no. ZK-R3375; Shenzhen Ziker Biological Technology Co., Ltd., Shenzhen, Guangdong, China) and stromal cell-derived factor (SDF)-1α (cat. no. ZK-R3591, Shenzhen Ziker Biological Technology Co., Ltd.) activity in plasma was measured using a double-antibody sandwich ELISA method. Interleukin (IL)-1β (cat. no. SEA563Ra), IL-6 (cat. no. SER079Ra), tumor necrosis factor (TNF)-α (cat. no. SEA133Ra) in serum were determined using commercial ELISA kits (Uscn Life Sciences, Inc., Wuhan, China). Blood samples (100 µl) were added to a 96-well plate, which was covered with an adhesive strip and incubated for 2 h at room temperature on a horizontal orbital microplate shaker. Each well was washed three times with wash buffer. A total of 200 µl GLP-1, IL-1β, IL-6, TNF-α and SDF-1α conjugate was added to each well, covered with a fresh adhesive strip, and incubated for 2 h at room temperature on the shaker. The washing steps were repeated, and 200 µl substrate solution was added to each well and incubated for 30 min at room temperature in the dark. Stop solution (50 µl) was added to each well and the optical density of each well was determined within 30 min using an Infinite 200PRO microplate spectrophotometer (Tecan Group, Ltd., Mannedorf, Switzerland) set at 450 nm. All samples were run in duplicate.
Statistics
Obtained data are expressed as the mean ± standard deviation. Data were assessed using SPSS 15.0 (SPSS, Inc., Chicago, IL, USA) by one-way analysis of variance with post hoc Bonferroni test for multiple comparisons. P<0.01 was considered to indicate a statistically significant difference. Results are expressed as the mean ± standard error of the mean.
Results
Neointima formation following balloon injury
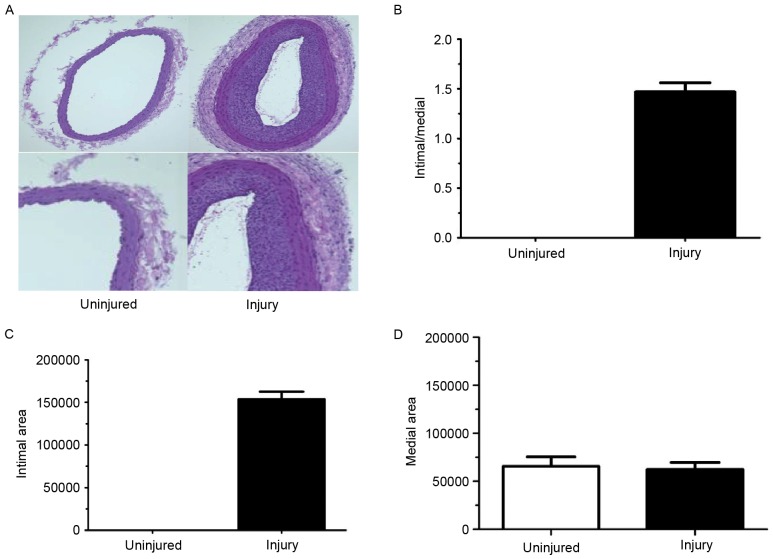
For these experiments, the right common carotid artery did not undergo balloon injury procedures, which meant the intimal/media ratio and the intimal area were equal to 0. Thus, the right common carotid artery served as the loading control. Rat left carotid artery injuries were performed and neointima formation was evaluated at 28 days post-surgery. The left carotid artery was injured and exhibited a decreased lumen area (Fig. 1A and B) which corresponded to increased intimal thickening. The intima/media ratio was also increased in the left arteries compared with right arteries (Fig. 1C). However, there was no difference in the medial area between left and right carotid arteries (Fig. 1D).
Figure 1.
Neointimal hyperplasia formation following balloon injury. (A) Tissues were evaluated by hematoxylin and eosin staining (magnification, ×200) at 28 days subsequent to balloon injury. The (B) ratio of intima/media (normalized to the uninjured tissue), (C) area of the intima and (D) area of the media were calculated and between the right and left carotid artery in the balloon injury group. Data are presented as the mean ± standard error of the mean.
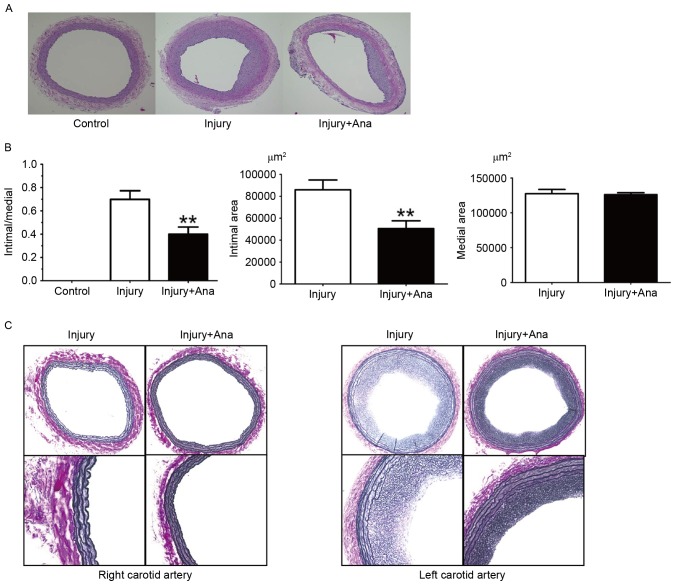
Effect of anagliptin on the degree of neointimal thickness following balloon injury
In the histological sections obtained from the rats which were given anagliptin (10 mg/kg) twice daily, compared with the injury group, no significant differences between the right carotid arteries were observed. It was observed that the lumen area, intimal area and intima/media ratio was decreased at 28 days compared with the injury group (Fig. 2A). Notably, the medial area in the left carotid artery of both groups was same (Fig. 2B).
Figure 2.
Anagliptin attenuates neointimal hyperplasia following balloon injury. (A) Tissues were evaluated by hematoxylin and eosin staining (magnification, ×200) at 28 days following the commencement of treatment with anagliptin. (B) The intima/media ratio (normalized to injury), and the area of the intima and media were calculated in the injury and anagliptin groups. (C) Histological sections of injured and anagliptin-treated arteries were stained with elastic van Gieson (magnification, ×200). **P<0.01 vs. injury. Data are presented as the mean ± standard error of the mean. Ana, anagliptin.
It has been hypothesized that the structural integrity of the IEL may be essential in the internal elastic lamina (IEL) rupture mechanism, in order to minimize intimal hyperplasia following vascular injury. The right carotid artery did not undergo vascular injury, and hence no intimal hyperplasia or IEL rupture was detected in the right carotid arteries of the injury and anagliptin groups. IEL rupture was subsequently analyzed in rat left carotid arteries, which were subjected to balloon injury in each group. Notably, balloon injury using the 2F Fogarty catheter did not result in any fractures in the whole IEL circumference, although intimal hyperplasia was still observed in the two groups (Fig. 2C). Intimal hyperplasia was decreased in the anagliptin group (Fig. 2C). The results of the present study indicated that there was no association between IEL rupture and intimal hyperplasia following balloon injury.
Effect of food consumption and body weight following balloon injury
In order to examine the systemic influence of anagliptin on metabolism, the food consumption and body weight of all the animals were determined at different time points. Following surgery, the body weight of both groups decreased at 4 days, and gradually recovered from 12 days until normal body weight was attained 28 days in the two groups (Fig. 3A). Daily analyses of food consumption illustrated decreased food intake at 4 days subsequent to balloon injury and recovery at 12 days, and this phenomenon was accordance with the loss of body weight observed in the groups (Fig. 3B). The results of the present study indicated that anagliptin attenuated neointima formation, independent of the glucose-lowering effect and body weight reduction among the groups.
Figure 3.
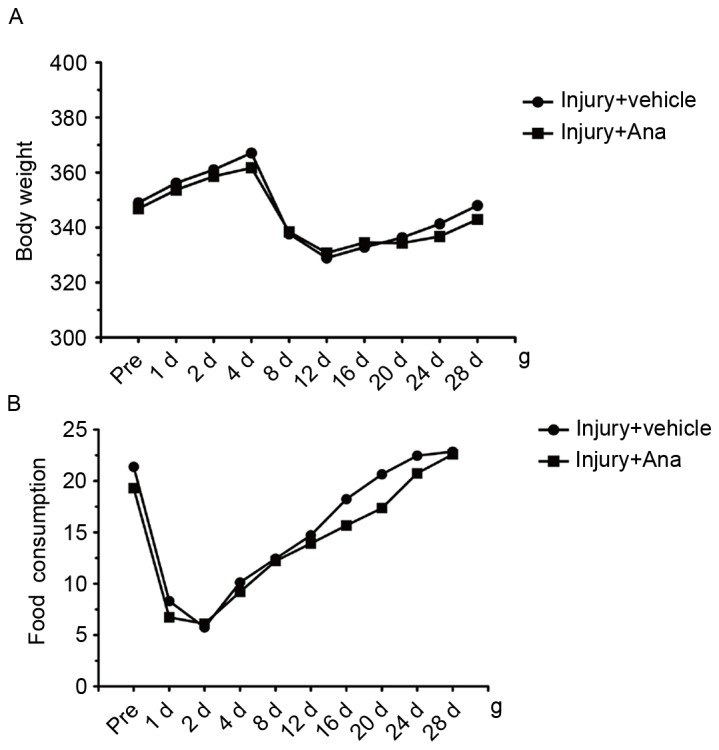
Comparison of the differences in (A) body weight and (B) food consumption in the injury group and the anagliptin-treated group. Data are presented as the mean ± standard error of the mean. Ana, anagliptin.
Detection of the activity of plasma GLP-1 and SDF-1α in α balloon injury model following treatment with anagliptin
GLP-1 is one of the substrates of DPP-4 in vivo which is rapidly degraded by the enzyme DPP-4 under normal conditions. Therefore, the concentration of GLP-1 may reflect the activity of DPP-4. ELISA analysis was employed for the detection of serum GLP-1 content which was collected from injury and anagliptin rats at the chosen time points (pre-operatively, and at 1, 7, 14, 21 and 28 days). The results demonstrated that serum GLP-1 content in anagliptin group was significantly increased compared with the control group and peaked at 28 days (Fig. 4A) which suggested the activity of DPP-4 was decreased.
Figure 4.
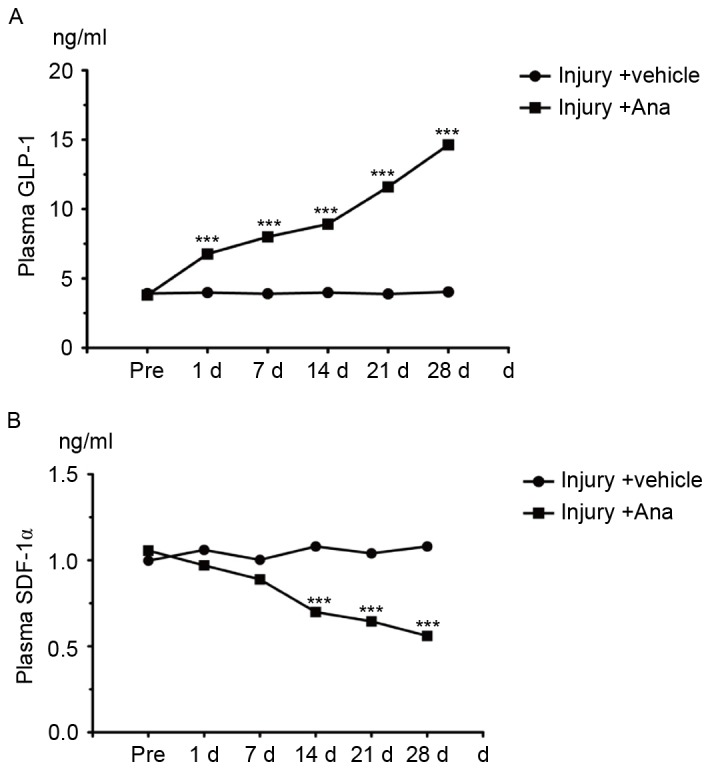
Measurement of the serum concentration of GLP-1 and SDF-1α following treatment with anagliptin. (A) The serum concentration of GLP-1 in the injury and anagliptin groups. (B) Serum level of SDF-1α in the injury and Anagliptin groups. ***P<0.001 vs. Injury + vehicle group. Data are presented as the mean ± standard error of the mean. Ana, anagliptin; GLP-1, glucagon-like peptide 1 receptor; SDF-1α, stromal cell-derived factor 1α.
SDF-1α, one of the DPP-4 substrates that is degraded by DPP-4 through its cleavage, is a chemokine which induces EPCs to differentiate into ECs in order to protect the injured artery. Therefore, the serum SDF-1α concentration was measured. Anagliptin decreased the serum SDF-1α level (Fig. 4B). These data suggested that anagliptin increased the serum active GLP-1 concentration, and altered serum factors associated with EPC migration.
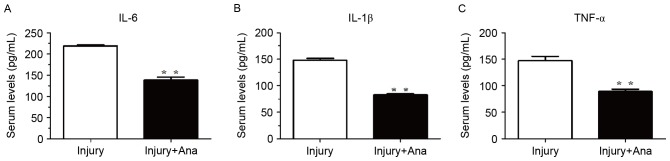
Detection of the serum activity of inflammatory cytokines following administration of anagliptin
Inflammatory cytokines are among the most important accelerators of intimal hyperplasia. Therefore, the present study assessed the inflammatory response following balloon injury. The serum levels of IL-1β, IL-6 and TNF-α were measured using ELISA analysis. The serum levels of IL-6, IL-1β, and TNF-α in the injury group were significantly increased compared with the group treated with anagliptin at 7 days (Fig. 5).
Figure 5.
Measurement of the serum activity of inflammatory cytokines following treatment with anagliptin. At 7 days post-injury, anagliptin decreased the serum activity of (A) IL-6, (B) IL-1β and (C) TNF-α. **P<0.01 vs. injury group. Data are presented as the mean ± standard error of the mean obtained from five independent experiments. Ana, anagliptin; IL, interleukin; TNF-α, tumor necrosis factor.
Discussion
CAD is the leading cause of mortality and morbidity in the developed world (13). Numerous improvements have been made in coronary angioplasty, including balloon angioplasty, stenting and CABG, although a metallic scaffold device, alone or in combination with drug eluting stents (DESs) is considered to be the most effective method of treating CAD (14). However, studies have suggested that DESs delay re-endothelialization, which is important for the prevention of restenosis and stent thrombosis. Intimal hyperplasia develops as a result of SMC migration and proliferation, and the accumulation of the extracellular matrix, which is a normal adaptive response in arteries against hemodynamic stress and is a characteristic feature of arterial injury healing (15,16).
ECs regulate vascular physiology by producing a variety of small molecules which have been identified, and regulate vascular homeostasis, including inhibiting the formation of thrombosis, coagulation, vasomotor tone and blood flow (17). It has been demonstrated that defects in endothelial integrity and dysfunction may be the initial steps leading to the adhesion of phagocytic cells (18) and proliferation of SMCs (19) in an injured artery, and may further induce atherosclerotic lesion and neointima formation (20). Therefore, EC loss is a factor that is a primary contributor to remodeling (21), and strategies to protect the endothelium and/or stimulate its repair following injury have been sought to reduce intimal hyperplasia formation.
Excessive intimal hyperplasia causes a decrease in blood flow, narrowing of the lumen and thrombosis formation by impairing the release of anticoagulants from ECs. A number of studies have been conducted using drugs to prevent intimal hyperplasia following balloon injury or stenting (22,23). Various mechanisms, including growth factors, inflammation, metabolic disorders and blood flow disturbances may cause intimal hyperplasia (24). Studies about the use of anagliptin for preventing intimal hyperplasia are novel and have not been published previously, however, positive results were obtained in the present study by using anagliptin in the prevention of intimal hyperplasia.
The intimal/medial ratio of the left carotid artery and the intimal area where the artery was injured were thicker compared with the right carotid artery in the injury group, although the medial area was the same. These results indicated that the model system used in the present study was successful and stable. In a previous study, it was observed that intimal hyperplasia began to form within 5 days following balloon injury and continued to thicken for 8 weeks until a maximum intima/media ratio was attained (25). From these observations, it is likely that the time course of intimal hyperplasia formation following balloon injury is complex and may involve a number of signaling pathways, although the beginning of intimal hyperplasia formation following injury may be reproducible. In the group treated with anagliptin, the intimal/medial ratio and intimal area were decreased compared with the group in which saline was used. Anagliptin alleviated the intimal hyperplasia on the injured side and decreased the intimal area. However, in the present study it was observed that anagliptin exerted no effect on medial area compared with the control group. The results of the present study only exhibited the intimal/medial ratio at 28 days following balloon injury whether.
A previous study indicated that the IEL may act as a physical barrier to SMC migration or inhibit paracrine communication between cells of the intima and media, and that IEL may disrupt the development of intimal hyperplasia (26). In support of this, elastic van Gieson staining was used in the present study to detect the rupture of the IEL in the model and anagliptin groups. Notably, the IEL remained intact in the two groups, meaning that the effect of anagliptin inhibiting intimal hyperplasia following balloon injury may not be mediated by maintenance of the IEL.
DPP-4 inhibitors, including anagliptin, are a novel class of drug which were introduced in the treatment of type 2 diabetes mellitus. DPP-4 inhibitors decrease blood glucose levels through inhibition of the degradation of GLP-1, which results in reduced secretion of glucagon and increased secretion of insulin (27). A previous study demonstrated that sitagliptin, a DPP-4 inhibitor, has protective properties against restenosis following carotid injury in an animal model of type 2 diabetes and in vascular cell lines, indicating that sitagliptin may be a novel agent for the treatment of macrovascular-related complications in patients with type 2 diabetes (28). With the results of the histological analysis performed in the present study, it may be demonstrated that anagliptin inhibited intimal hyperplasia in vivo. However, the present study sought to elucidate whether the effect of anagliptin on neointimal hyperplasia was mediated by a decrease in the activity of DPP-4. Therefore, the plasma concentration of GLP-1, which may reflect the plasma activity of DPP-4, was measured. Serum GLP-1 concentrations rose with anagliptin treatment at the different time points indicating that anagliptin may inhibit the plasma activity of DPP-4 in vivo, with no difference being observed in the model group. Although the plasma levels of DPP-4 and GLP-1 were altered, body weight and food intake were not markedly different in the two groups. Notably, the active GLP-1 levels tended to increase in the anagliptin group compared with the injury group, although there was no significant difference preoperatively. A previous report indicated that the daily glucose levels of rats that were fasted for 4 h were similar in a group treated with vildagliptin compared with the control group, although they significantly decreased between week 2 and week 5 (29); it was hypothesized that this may be associated with tissue or circulating DPP-4 enzyme activity (30). The DPP-4 expression and enzyme activity in other tissues remain unknown and its role requires future investigation. It may be that there exist other pathways which control the process of intimal hyperplasia apart from the metabolic pathway.
The C-X-C chemokine SDF-1α, which is important for cell mobilization/homing (31), is highly expressed in human atherosclerotic plaques and effectively activates platelets in vitro (32). There are two SDF-1 isoforms which are derived from a single SDF-1 gene that is encoded and produced by alternative splicing (33). The two SDF-1 isoforms are cleaved by soluble or cellular DPP-4, which has been demonstrated to inactivate their antiviral and chemotactic properties in cell-based assays in vitro (34). SDF-1α is constitutively expressed in a number of tissues and has been observed to be a chemoattractant for many types of cell. In the present study, it was observed that serum levels of SDF-1α did not notably fluctuate in the model group. However, SDF-1α expression significantly decreased at 1 day post-balloon injury and peaked at 28 days following treatment with anagliptin. The results of the present study were in contrast to those of a previous study which reported an increase in plasma SDF-1α within 24 h following vascular injury in mice (35). A previous study demonstrated that anagliptin did not increase the serum SDF-1α level within atherosclerotic lesions in apolipoprotein E-deficient mice (36). DPP-4 is a membrane-bound exopeptidase that rapidly degrades GLP-1. A previous study demonstrated that a soluble form of DPP-4 (s-DPP-4) that lacks the short intracellular tail and the transmembrane regions is present in serum and other bodily fluids which exhibit DPP-4 enzyme activity (37). High serum levels of s-DPP-4 have been described in various conditions (38). It may therefore be hypothesized that anagliptin may only inhibit the activity of s-DPP-4, whilst preserving the function of DPP-4 in the membrane. However, the underlying mechanism of this action remains unknown. A previous study demonstrated that systemic treatment of mice with a SDF-1α blocking antibody reduced injury-induced neointima formation (39). Therefore, neutralizing SDF-1α may have the effect of diminishing plaque formation and reducing smooth muscle progenitor cell recruitment and neointima formation following vascular injury (40). In the present study, following treatment of the balloon injury model with anagliptin, the intimal area and intimal/medial ratio was reduced. Notably, the plasma level of SDF-1α was decreased. This indicated that SDF-1α may serve an important role in the process of vascular remodeling, particularly the formation of intimal hyperplasia. The major new insight provided by the results of the present study in terms of mechanism is that administering anagliptin may reduce the level of SDF-1α, which is associated with inhibition of the formation of intimal hyperplasia. It may be hypothesized that reducing the plasma level of SDF-1α may promote leukocyte adhesion and migration, and hence stimulate migration and proliferation of ECs from the adjacent non-injured endothelium via additional factors released from the site of injury. These factors may drive vascular re-endothelialization, which may inhibit platelet aggregation and adhesion, and recovery of the function of the injured artery.
A previous study demonstrated that another DPP-4 inhibitor, alogliptin, was able to inhibit intimal hyperplasia in rats by inhibiting inflammation (20 mg/kg/day for 14 days; oral injection) (41). Although this previous study and the present study used the same source drug (alogliptin vs. anagliptin) and obtained the same results (inhibition of intimal hyperplasia), there remain certain differences: i) The two types of animal model may reflect the different pathological processes of intimal hyperplasia, although the balloon injury model is considered to be a priority in the study of arterial restenosis following mechanical injury [which is the primary complication of percutaneous luminal coronary angioplasty (PTCA)]; and ii) the balloon injury model may be useful for the discovery of drugs which have the ability to inhibit the formation of intimal hyperplasia. However, it is thought that inhibiting the activity of DPP-4 may be a potential therapy to inhibit the process of intimal hyperplasia, and thus, this may also be a novel therapy for inhibiting restenosis following PTCA. A previous study reported that DPP-4 is released as an adipokine from visceral fat, and stimulates vascular (V) SMC proliferation through extracellular signal-regulated kinase/mitogen-activated protein kinase phosphorylation in VSMCs (40). Other DPP-4 substrates, including BNP (42), were not measured in the present study due to sample limitation. It was not possible to investigate all the mechanisms through which anagliptin may attenuate neointima formation following vascular injury. Further studies are required to clarify the vasculoprotective effect of anagliptin and to detect other DPP-4 substrates.
In conclusion, the results of the present study demonstrated that anagliptin was able to inhibit intimal hyperplasia by reducing the plasma level of SDF-1α, rather than by altering the process of metabolism. It was hypothesized that the potential mechanism involves decreasing the plasma level of SDF-1α to inhibit leukocyte adhesion and the migration of SMCs, and hence stimulate the migration and proliferation of ECs from the adjacent non-injured endothelium via additional factors released from the site of balloon injury. Future studies in the field of vascular biology following injury may positively affect the quality of life of patients who have undergone cardiovascular surgery by providing an improved understanding of endothelial functioning and recovery from injury, which is primarily responsible for intimal hyperplasia. The prevention of the intimal hyperplasia response may be effective in increasing lifespan following vascular reconstructive interventions, including surgical graft bypass or balloon angioplasty.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant no. 81500209), the University Nursing Program for Young Scholars with Creative Talents in Heilongjiang Province (grant no. 2016050) and Heilongjiang Postdoctoral Financial Assistance (grant no. LBH-Z14215).
References
- 1.Molina JA, Heng BH. Global trends in cardiology and cardiothoracic surgery-an opportunity or a threat? Ann Acad Med Singapore. 2009;38:541–545. [PubMed] [Google Scholar]
- 2.Uchida Y, Uchida Y, Matsuyama A, Koga A, Kanai M, Sakurai T. Formation of web- and membrane-like structures on the edges of bare-metal coronary stents. Circ J. 2010;74:1830–1836. doi: 10.1253/circj.CJ-10-0093. [DOI] [PubMed] [Google Scholar]
- 3.Pauletto P, Sartore S, Pessina AC. Smooth-muscle-cell proliferation and differentiation in neointima formation and vascular restenosis. Clin Sci (Lond) 1994;87:467–479. doi: 10.1042/cs0870467. [DOI] [PubMed] [Google Scholar]
- 4.Delafontaine P. Growth factors and vascular smooth muscle cell growth responses. Eur Heart J. 1998;19(Suppl G):G18–G22. [PubMed] [Google Scholar]
- 5.Ross R. Cell biology of atherosclerosis. Annu Rev Physiol. 1995;57:791–804. doi: 10.1146/annurev.ph.57.030195.004043. [DOI] [PubMed] [Google Scholar]
- 6.Chervu A, Moore WS. An overview of intimal hyperplasia. Surg Gynecol Obstet. 1990;171:433–447. [PubMed] [Google Scholar]
- 7.Allaire E, Clowes AW. Endothelial cell injury in cardiovascular surgery: The intimal hyperplastic response. Ann Thorac Surg. 1997;63:582–591. doi: 10.1016/s0003-4975(96)01045-4. [DOI] [PubMed] [Google Scholar]
- 8.Hong WJ, Petell JK, Swank D, Sanford J, Hixson DC, Doyle D. Expression of dipeptidyl peptidase IV in rat tissues is mainly regulated at the mRNA levels. Exp Cell Res. 1989;182:256–266. doi: 10.1016/0014-4827(89)90296-6. [DOI] [PubMed] [Google Scholar]
- 9.Matheeussen V, Baerts L, de Meyer G, de Keulenaer G, van der Veken P, Augustyns K, Dubois V, Scharpé S, De Meestre I. Expression and spatial heterogeneity of dipeptidyl peptidases in endothelial cells of conduct vessels and capillaries. Biol Chem. 2011;392:189–198. doi: 10.1515/bc.2011.002. [DOI] [PubMed] [Google Scholar]
- 10.Shinjo T, Nakatsu Y, Iwashita M, Sano T, Sakoda H, Ishihara H, Kushiyama A, Fujishiro M, Nishimura F, Asano T. High-fat diet feeding significantly attenuates anagliptin-induced regeneration of islets of Langerhans in streptozotocin-induced diabetic mice. Diabetol Metab Syndr. 2015;7:50. doi: 10.1186/s13098-015-0047-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ervinna N, Mita T, Yasunari E, Azuma K, Tanaka R, Fujimura S, Sukmawati D, Nomiyama T, Kanazawa A, Kawamori R, et al. Anagliptin, a DPP-4 inhibitor, suppresses proliferation of vascular smooth muscles and monocyte inflammatory reaction and attenuates atherosclerosis in male apo E-deficient mice. Endocrinology. 2013;154:1260–1270. doi: 10.1210/en.2012-1855. [DOI] [PubMed] [Google Scholar]
- 12.Hirano T, Yamashita S, Takahashi M, Hashimoto H, Mori Y, Goto M. Anagliptin, a dipeptidyl peptidase-4 inhibitor, decreases macrophage infiltration and suppresses atherosclerosis in aortic and coronary arteries in cholesterol-fed rabbits. Metabolism. 2016;65:893–903. doi: 10.1016/j.metabol.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Indolfi C, Pavia M, Angelillo IF. Drug-eluting stents versus bare metal stents in percutaneous coronary interventions (a meta-analysis) Am J Cardiol. 2005;95:1146–1152. doi: 10.1016/j.amjcard.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 14.Cassess S, Hoppmann P, Kufner S, Byrne RA, Wiebe J, Colleran R, Giacoppo D, Harada Y, Laugwitz KL, Schunkert H, et al. Intraindividual comparison of everolimus eluting bioresorbable vascular scaffolds versus drug eluting metallic stent. Circ Cardiovasc Interv. 2016;9:pii: e003698. doi: 10.1161/CIRCINTERVENTIONS.116.003698. [DOI] [PubMed] [Google Scholar]
- 15.Allagnat F, Dubuis C, Lambelet M, Le Gal L, Alonso F, Corpataux JM, Déglise S, Haefliger JA. Connexin37 reduces smooth muscle cell proliferation and intimal hyperplasia in a mouse model of carotid artery ligation. Cardiovasc Res. 2017;113:805–816. doi: 10.1093/cvr/cvx079. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, He X, Chen X, Ma H, Liu D, Luo J, Du Z, Jin Y, Xiong Y, He J, et al. Enhanced external counterpulsation inhibits intimal hyperplasia by modifing shear stress responsive gene expression in hypercholesterolemic pigs. Circulation. 2007;116:526–534. doi: 10.1161/CIRCULATIONAHA.106.647248. [DOI] [PubMed] [Google Scholar]
- 17.Davies MG, Hagen PO. The vascular endothelium. A new horizon. Ann Surg. 1993;218:593–609. doi: 10.1097/00000658-199321850-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kibos A, Campeanu A, Tintoiu I. Pathophysiology of coronary artery in-stent restenosis. Acute Card Care. 2007;9:111–119. doi: 10.1080/17482940701263285. [DOI] [PubMed] [Google Scholar]
- 19.Yoneda S, Abe S, Kanaya T, Oda K, Nishino S, Kageyama M, Taguchi I, Masawa N, Inoue T. Late-phase inflammatory response as a feature of in-stent restenosis after drug-eluting stent implantation. Coron Artery Dis. 2013;24:368–373. doi: 10.1097/MCA.0b013e32836222ec. [DOI] [PubMed] [Google Scholar]
- 20.McDonald RA, Halliday CA, Miller AM, Diver LA, Dakin RS, Montgomery J, McBride MW, Kennedy S, McClure JD, Robertson KE, et al. Reducing in-stent restenosis: Therapeutic manipulation of miRNA in vascular remodeling and inflammation. J Am Coll Cardiol. 2015;65:2314–2327. doi: 10.1016/j.jacc.2015.03.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paneghetti L, Ng YS. A novel endothelial-derived anti-inflammatory activity significantly inhibits spontaneous choroidal neovascularisation in a mouse model. Vasc Cell. 2016;8:2. doi: 10.1186/s13221-016-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang W, Zheng B, Zhang XH, Yue LY, Liu C, Ma D, Yang Z, Wen JK. Tongxinluo inhibits neointimal formation by regulationg the expression and post-translational modification of KLF5 in macrophages. Am J Transl Res. 2016;8:4778–4790. [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang YQ, Tian F, Zhou Y, Chen YD, Li B, Ma Q, Zhang Y. Nicorandil attenuates carotid intimal hyperplasia after balloon catheter injury in diabetic rats. Cardiovasc Diabetol. 2016;15:62. doi: 10.1186/s12933-016-0377-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grus T, Lambert L, Matěcha J, Grusová G, Špaček M, Mlček M. The ratio of diameters between the target artery and the bypass modifies hemodynamic parameters related to intimal hyperplasia in the distal end to side anastomosis. Physiol Res. 2016;65:901–908. doi: 10.33549/physiolres.933297. [DOI] [PubMed] [Google Scholar]
- 25.Honda Y, Kitano T, Fukuya F, Sato Y, Iwama S, Morie T, Notake M. A novel alphavbeta3 integrin antagonist suppresses neointima formation for more than 4 weeks after balloon injury in rats. Arterioscler Thromb Vasc Biol. 2005;25:1376–1382. doi: 10.1161/01.ATV.0000168902.18672.2f. [DOI] [PubMed] [Google Scholar]
- 26.Touchard AG, Schwartz RS. Preclinical restenosis models: Challenges and successes. Toxicol Pathol. 2006;34:11–18. doi: 10.1080/01926230500499407. [DOI] [PubMed] [Google Scholar]
- 27.Shinjo T, Nakatus Y, Iwashita M, Sano T, Sakoda H, Ishihara H, Kushiyama A, Fujishiro M, Nishimura F, Asano T. High-fat diet feeding significantly attenuates anagliptin-induced regeneration of islets of Langerhans in streptozotocin-induced diabetic mice. Diabetol Metab Syndr. 2015;7:50. doi: 10.1186/s13098-015-0047-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lim S, Choi SH, Shin H, Cho BJ, Park HS, Ahn BY, Kang SM, Yoon JW, Jang HC, Kim YB, Park KS. Effect of a dipeptidyl peptidase-IV inhibitor, des-fluoro-sitagliptin, on neointimal formation after balloon injury in rats. PLoS One. 2012;7:e35007. doi: 10.1371/journal.pone.0035007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eom YS, Gwon AR, Kwak KM, Kim JY, Yu SH, Lee S, Kim YS, Park IB, Kim KW, Lee K, Kim BJ. Protective effects of vildagliptin against pioglitazone induced bone loss in type 2 diabetic rat. PLoS One. 2016;11:e0168569. doi: 10.1371/journal.pone.0168569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mentlein R. Dipeptidyl peptidase IV (CD26)-role in the inactivation of regulatory peptides. Regul Pept. 1999;85:9–24. doi: 10.1016/S0167-0115(99)00089-0. [DOI] [PubMed] [Google Scholar]
- 31.Tachibana K, Hirota S, Iizasa H, Yoshida H, Kawabata K, Kataoka Y, Kitamura Y, Matsushima K, Yoshida N, Nishikawa S, et al. The chemokine receptor CXCR4 is essential for vascularization of the gastrointestinal tract. Nature. 1998;393:591–594. doi: 10.1038/31261. [DOI] [PubMed] [Google Scholar]
- 32.Abi-Younes S, Sauty A, Mach F, Sukhova GK, Libby P, Luster AD. The stromal cell-derived factor-1 chemokine is a potent platelet agonist highly expressed in atherosclerotic plaques. Circ Res. 2000;86:131–138. doi: 10.1161/01.RES.86.2.131. [DOI] [PubMed] [Google Scholar]
- 33.Shirozu M, Nakano T, Inazawa J, Tashiro K, Tada H, Shinohara T, Honji T. Structure and chromosomal localization of the human stromal cell-derived factor 1 (SDF1) gene. Genomics. 1995;28:495–500. doi: 10.1006/geno.1995.1180. [DOI] [PubMed] [Google Scholar]
- 34.Shioda T, Kato H, Ohnishi Y, Tashiro K, Ikegawa M, Nakayama EE, Hu H, Kato A, Sakai Y, Liu H, et al. Anti-HIV-1 and chemotactic activities of human stromal cell-derived factor 1alpha (SDF-1alpha) and SDF-1beta are abolished by CD26/dipeptidyl peptidase IV-mediated cleavage; Proc Natl Acad Sci USA; 1998; pp. 6331–6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schober A, Knarren S, Lietz M, Lin EA, Weber C. Crucial role of stromal cell-derived factor-1alpha in neointima formation after vascular injury in apolipoprotein E-deficient mice. Circulation. 2003;108:2491–2497. doi: 10.1161/01.CIR.0000099508.76665.9A. [DOI] [PubMed] [Google Scholar]
- 36.Ervinna N, Mita T, Yasunari E, Azuma K, Tanaka R, Fujimura S, Sukmawati D, Nomiyama T, Kanazawa A, Kawamori R, et al. Anagliptin, a DPP-4 inhibitor, suppresses proliferation of vascular smooth muscles and monocyte inflammatory reaction and attenuates atherosclerosis in male apo E-deficient mice. Endocrinology. 2013;153:1260–1270. doi: 10.1210/en.2012-1855. [DOI] [PubMed] [Google Scholar]
- 37.Lambeir AM, Durinx C, Scharpe S, De Meester I. Dipeptidyl-peptidase IV from bench to bedside: An update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit Rev Clin Lab Sci. 2003;40:209–294. doi: 10.1080/713609354. [DOI] [PubMed] [Google Scholar]
- 38.Gorrell MD, Gysbers V, McCaughan GW. CD26: A multifunctional integral membrane and secreted protein of activated lymphocytes. Scand J Immunol. 2001;54:249–264. doi: 10.1046/j.1365-3083.2001.00984.x. [DOI] [PubMed] [Google Scholar]
- 39.Zernecke A, Schober A, Bot I, Von Hundelshausen P, Liehn EA, Möpps B, Mericskay M, Gierschik P, Biessen EA, Weber C. SDF-1alpha/CXCR4 axis is instrumental in neointimal hyperplasia and recruitment of smooth muscle progenitor cells. Circ Res. 2005;96:784–791. doi: 10.1161/01.RES.0000162100.52009.38. [DOI] [PubMed] [Google Scholar]
- 40.Akita K, Isoda K, Shimada K, Daida H. Dipeptidyl-Peptidase-4 inhibitor, alogliptin, attenuates arterial inflammation and neointimal formation after injury in low-density lipoprotein (LDL) receptor-deficient mice. J Am Heart Assoc. 2015;4:e001469. doi: 10.1161/JAHA.114.001469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lamers D, Famulla S, Wronkowitz N, Hartwig S, Lehr S, Ouwens DM, Eckardt K, Kaufman JM, Ryden M, Müller S, et al. Dipeptidyl peptidase 4 is a novel adipokine potentially linking obesity to the metabolic syndrome. Diabetes. 2011;60:1917–1925. doi: 10.2337/db10-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murohara T. Dipeptidyl peptidase-4 inhibitor: Another player for cardiovascular protection. J Am Coll Cardiol. 2012;59:277–279. doi: 10.1016/j.jacc.2011.09.050. [DOI] [PubMed] [Google Scholar]