Abstract
The present research analyzed the elements of thalassemia which affect the patient’s perceived quality of life. Three hundred patients with Thalassemia Major (males = 165, 55%; females = 135, 45%; Mage = 36.13, standard deviation = 8.54) were the sample. Analysis of multiple mediations revealed a direct effect of self-efficacy on the Satisfaction with Life Scale that is mediated only by social support.The findings suggest a need to accentuate help and support to patients with Thalassemia Major.
Keywords: life engagement, proactive personality, quality of life, social support, well-being
Introduction
During the past decades, there has been an increasing predominance of chronic disorders, which, in turn, lead to a large number of people living with chronic diseases that can adversely affect their quality of life. Thalassemia is a chronic disease that can have an impact on the patient’s social behavior and psychological functioning. Depending on the type of the hemoglobin involved, there are two distinct forms of thalassemia: beta-thalassemia and alpha-thalassemia. The patients suffering from the most severe form of this disease need to have continuous blood transfusions.
The World Health Organization (WHO) (1958) defines health as not the merely absence of disease or infirmity, but a state of complete psychical, mental, and social well-being. According to the WHO, Thalassemia is defined as “rare”; nevertheless, due to the migration flows and the lack of prevention measures, it has recently become an issue of great concern.
According to WHO (1996), Quality of Life is defined as an individual’s perceptions of their position, specifically in terms of culture and systems of values in which the persons live and in relation to their goals, expectations, standards, and concerns.
Devins et al. (1983) claim that any chronic disease negatively impacts the patients’ life and their psychosocial well-being. Specifically, recent research found that the self-image of young adults with thalassemia was characterized by the inability to engage with daily goals (Messina et al., 2008). In those circumstances, it is important to talk about global assistance toward the patients, in order for them to achieve an improvement in the quality of their life and social integration; that would also allow them to coexist in a more peaceful way with their pathological condition (Hadi et al., 2009).
The following research originates from a collaboration with the Italian League for the Fight against Childhood-Cancer and Blood Disorders; it came from the recognition of a discrepancy between the actual quality of life of patients with hemoglobinopathies and their search for a better future, together with their lack of planning and projection in the future.
Theoretical background
Among the variables that contribute to determine the quality of life in people with chronic illness, the WHO identified the following factors: physical health, psychological well-being, level of independence, social relations, and relationship with important features of the environment (WHO, 1993a, 1993b). Several studies indicated that personal and psychosocial factors can affect the perception of quality of life in those patients (e.g. Brow et al., 2007; Thomason et al., 2007). According to this, the following factors have been considered in the present study: Social Support, Satisfaction with Quality of Life, Proactive Personality, Self-Efficacy, and Life Engagement.
As for the social support, Shumaker and Brownell (1984) defined it as “an exchange of resources between two individuals perceived by the provider or the recipient to be intended to enhance the well-being of the recipient” (p. 1).
Social support can have three functions: an emotional function, which promotes the feelings of comfort; a cognitive function, which involves the acquisition of information and knowledge; a material function, which offers instrumental support. Furthermore, social support is able to decrease stress levels and may also influence the physical symptoms related with the disease (Gerhardt, 1991; Jacobson, 1986; Rook, 2014; Rook and Underwood, 2000). With regard to the satisfaction with the quality of life, it can be defined as a current and future life’s condition which the individual identifies himself with (Diener et al., 1985); quality of life is an important outcome variable for the patient’s health monitoring and for evaluating the effectiveness of health interventions. The concept of “proactive personality” according to Bateman and Crant (1993) concerns the ability of individuals to change and manipulate their surroundings. The authors stated that people with high pro-activity are able to handle with and resolve their problems and to seek new opportunities in obtaining a positive change about their welfare. A proactive attitude a patient might have toward their own life, means not to be overwhelmed by everyday adversity but to be able to achieve their life goals and going beyond the illness itself (Aspinwall, 2011; Cunningham and De La Rosa, 2008; Justice, 1998). Personal actions such as health promotion behaviors have also been recognized as having an important influence on quality of life (Blumenthal and Gullette, 2002; Kahana and Kahana, 1996; Marquez et al., 2009).
The concept of self-efficacy in the patient with thalassemia is also important, and it is related to the capability to achieve some important goals together with their psychological well-being (Moghadam et al., 2000). Self-efficacy is defined as those beliefs concerning the individual capability to do what will help them in obtaining their goals or purposes. Patients with higher self-efficacy and a greater belief in their ability to handle with their daily tasks are more likely to perform better in terms of achieved goals (Huang et al., 2013). Patients suffering from chronic disease are generally more likely to overcome social, psychological, and physical barriers if they have a high level of self-efficacy. Consequently, this has also an impact on the effectiveness of the therapies carried out (Adegbola, 2007; Lorig et al., 2001; Mechanic, 1995). The engagement with life is another factor to be taken into consideration; it is defined as the degree to which a person engages in activities that are meaningful to them by pursuing valued goals, and it enables them to see life as purposeful (Scheier et al., 2006). Life engagement reflects experiences that have affected a person in a positive way. The perception of satisfaction or dissatisfaction can influence the subjective well-being, as “this quality of life can be associated with life engagement which is also an important aspect of mental health” (Shahnaz and Karim, 2014: 276). Investigating which are the factors that most affect the perception of quality of life may offer interesting insights to understand the patient’s reaction to the illness (in terms of psychological impact) and their ability to rely on their internal resources, which can also help when deciding future treatments.
Research questions
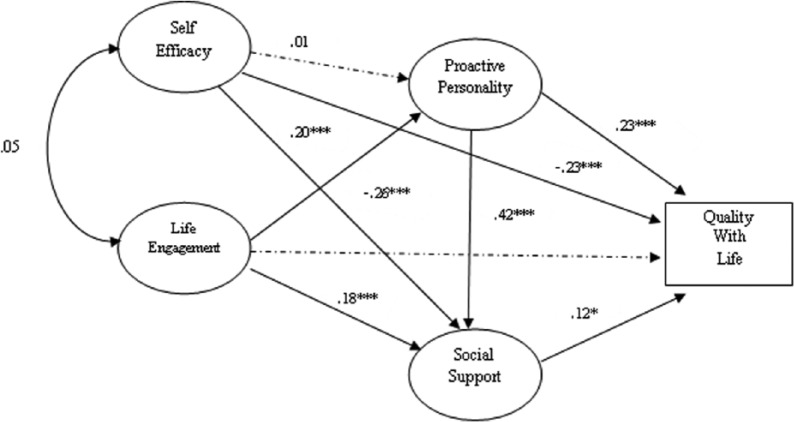
Based on the previous literature, the aim of the present study is to explore the impact the above variables can have on patients with thalassemia; it is plausible to assume that the perception of the quality of life of the individual may be affected by some psychosocial variables. A first hypothesis is that social support can be an important mediator in the relationship between life engagement and satisfaction with quality of life. A second hypothesis is that proactive personality can mediate the relationship between self-efficacy and quality of life (Figure 1).
Figure 1.
Conceptual model showing directed and mediating effect of proactive personality and social support on the relationship between self-efficacy and quality of life and life engagement.
Method
Participants and procedure
The present research involved 300 patients with Thalassemia Major (males = 165, 55%; females = 135, 45%; Mage = 36.13, standard deviation (SD) = 8.54), belonging to 12 associations located within the Region of Sicily. The data collection process took place within the associations with the help of social workers and psychologists who have received instruction and training on how to prepare the setting. For the educational level of the sample, percentages were as follows: middle school = 18 % high school = 52 % bachelor degree = 22 % post-graduate degree = 8 percent. Data were collected during the period between September 2015 and March 2016. The time to read and fill in the test ranged from 15 and 20 minutes. The participation to this study-research was completely voluntary, data were collected anonymously, and the participants could revoke their participation at any moment.
Measures
The Satisfaction with Life Scale
The SWLS is a five-item scale answered on a 7-point Likert scale (1 = “low satisfaction,” 7 = “high satisfaction”) (Diener et al., 1985). Each item assessed ideal life. The scale reported good internal reliability, 2-month test–retest reliability, and moderate correlations (.50 to .60) with a large number of subjective well-being scales. The SWLS is used in our study as a general, global, subjective quality of life measure. In our study, Cronbach’s coefficient alpha was .92. Examples of items are “I am satisfied with my life,” “In most ways, my life is close to my ideal.”
The Multidimensional Scale of Perceived Social Support
The Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet et al., 1988) assessed perceptions of support from three different sources: family, friends, and a significant other. The scale contains a total of 12 items, with 4 items for each subscale and it has been translated into different languages. The MSPSS scale has demonstrated good internal and test–retest reliability; specifically for the Significant Other, Family, and Friends subscales values were .91, .87, and .95, respectively. Examples of items are “There is a special person who is around when I am in need” and “I can talk about my problems with my family.” The reliability for the total scale was .88. For each item, participants expressed their opinion on a 7-point Likert scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Cronbach’s alpha for each subscale was as follows: Significant Other = .86, Family = .92, Friends = .89; total scale = .90.
Proactive Personality Scale
The Proactive Personality Scale (PPS; Seibert et al., 2001; it. adapt., Trifiletti et al., 2009) evaluates the inclination to take action and change the environment to realize one’s goals. The present study used a shorter version, made of 10 items (Trifiletti et al., 2009). Participants answered the following measures using a 7-point Likert scale ranging from 1 (“absolutely false”) to 7 (“absolutely true”). Examples of items are “If I see something I don’t like, I fix it” and “I am constantly on the lookout for new ways to improve my life.”
The scale is a one-dimensional measure and it showed good internal and test–retest reliability. Cronbach’s alpha was .92.
The Life Engagement Test
Life Engagement Test (LET; Scheier et al., 2006) is a scale composed of six items (three items framed in a positive direction and three items framed in a negative direction). For each item, participants expressed their evaluation on a 5-point Likert scale ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). That scale assessed the purpose in life, defined in terms of the extent to which a person engages in activities that are personally valued. The intent of the scale is to provide an index of purpose in life by assessing the extent to which a person considers his or her activities to be valuable and important. Example of item is “I have lots of reasons for living.” Cronbach’s alpha of the scale was .87.
The General Self-Efficacy Scale
The general self-efficacy scale is aimed to assess a broad and stable sense of personal competence to deal efficiently with a variety of stressful situations. The first version of the scale was originally developed with 20 items and later reduced to a 10-item version (Jerusalem and Schwarzer, 1986, 1992; Schwarzer, 2002; Schwarzer and Jerusalem, 1995). Responses are made on a 4-point Likert scale, from 1 (“not at all true”) to 4 (“exactly true”). The scale showed good convergent and discriminant validity. Example of item is “I can always manage to solve difficult problems if I try hard enough.” Cronbach’s alpha in the present study was .97.
Data analysis
Linear structural equations models were calibrated to test the hypothesized model with AMOS 21.0 (Arbuckle and Wothke, 1999). First, a confirmatory factor analysis (CFA) was used to test the fit of the measurement model (Byrne, 2001). AMOS provides several goodness-of-fit indexes, including the chi-square (χ2), the comparative fit index (CFI), the Tucker–Lewis index (TLI) (also called the non-normed fit index or NNFI), the CFI, the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR). Akaike Information Criterion (AIC) was also presented (lower values indicate better fit). The chi-square tests the null hypothesis that the covariance matrix and mean vector in the population are equal to the model-implied covariance matrix and mean vector (Geiser, 2013). A significant chi-square value leads to the rejection of the null hypothesis that the model fits in the population. Because the χ2 is highly sensitive to sample size (the larger the sample size, the more likely to reject the model), the ratio chi-square/degrees of freedom (df) is frequently analyzed. Kline (2005) recommended that a χ2/df greater than 3 represents inadequate fit. The CFI provides an evaluation of the difference between an independent model and the specified model. According to Hu and Bentler (1999), a CFI < .95 can indicate a good model fit. The TLI, for which the same cut-off values as for the CFI apply, compares the fit of the target model to the fit of the independent model. The RMSEA is a measure of approximate model fit. According to Browne and Cudeck (1993), a RMSEA < .09 is still an indicator of a reasonable error of approximation in smaller samples. In fact, in small sample sizes (n ≤ 300), even a CFI ≥ .90 can indicate an acceptable fit (Bentler, 1990; Hu and Bentler, 1999). Finally, the SRMR coefficient is a standardized measure for the evaluation of the model residuals.
Values range from 0 to 1.0, with well fitting models obtaining values less than .05 (Byrne, 2001); however, values as high as .08 are also acceptable (Hu and Bentler, 1999). The SEM approach was then used to test the mediation model shown in Figure 1, following James et al.’s (2006) recommendations and Shrout and Bolger’s (2002) logic with regard to expected proximal and distal effects.1 Other well-known analytical tools, such as correlations, were also used, implemented using SPSS 20.0. In order to optimize the sample size, missing values for the relevant items were estimated using Expectation Maximization method. None of the items had more than 5 percent missing values, indicating that this option was appropriate for use (Tabachnick and Fidell, 2007).
Results
Descriptive statistics and multivariate normality
In SEM, one of the main concerns about data is whether the sample has a multivariate normal distribution, because that determines which estimation method will be used and to what extent the estimates obtained from the most common methods are trust worthy (Child, 2006). Each observed variable has minimum, maximum, skewness, and kurtosis values. Critical values that exceed +2.00 or that are smaller than −2.00 indicate statistically significant degrees of non-normality. The descriptive statistics in Table 1 show that data were normally distributed, with acceptable skewness and kurtosis values.
Table 1.
Descriptive statistics (range (minimum/maximum), mean (M), including standard error (SE), standard deviation (SD), skewness, and kurtosis).
| N | Min | Max | M | SE | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|---|
| Proactive Personality | 300 | 1.50 | 5.90 | 3.77 | .048 | .83 | −.19 | −.51 |
| Life Engagement | 300 | 1.00 | 5.00 | 3.99 | .039 | .667 | −.99 | 1.65 |
| Quality with Life | 300 | 1.00 | 7.00 | 4.35 | .072 | 1.25 | −.23 | −.45 |
| Self-Efficacy | 300 | 2.00 | 4.00 | 2.93 | .028 | .49 | .18 | −.58 |
| Social Support | 300 | 1.00 | 7.00 | 5.48 | .059 | 1.03 | −.99 | 1.17 |
| Family | 300 | 1.00 | 7.00 | 5.68 | .067 | 1.17 | −1.01 | .71 |
| Friends | 300 | 1.00 | 7.00 | 5.46 | .064 | 1.12 | −.73 | .35 |
| Other | 300 | 1.00 | 7.00 | 5.29 | .065 | 1.12 | −.72 | .56 |
CFA confirmatory of the model’s variables
CFAs were performed using robust maximum likelihood estimation to examine the structure of latent variables (social support and proactive personality). At first, we decided to test a model with four factors, where all the variables were considered as unidimensional except for the social support, which was organized in three sub-factors (Significant Others, Family, and Friends). This model produced poor fit to the data (χ2(51, N = 300) = 198.26, p < .001, χ2/df = 3.88, RMSEA = .09, CFI = .93, TLI = .91, SRMR = .08, AIC = 252.263). Given that Model 1 with seven factors (three factors for social support, one for Proactive Personality, one for Life Engagement, one for Satisfaction with Life Scale and one for Self-Efficacy) did not represent a good fit to the data, a new model with five factors (Model 2, with one factor for each variable considered in the study) was evaluated. In this case, the fit indices improved (χ2(35, N = 300) = 91.68, p < .001, χ2/df = 2.62, RMSEA = .06, CFI = .93, TLI = .95, SRMR = .07, AIC = 183.536); moreover, all factor loadings were significant (p < .001). A next step to test hypothesized model of analysis and to verify the relationship between the variables was to conduct a structural equation model, using the maximum likelihood estimation method. All the variables studied were measured from the same source, and therefore, common method bias may have occurred. We conducted a CFA according to Harman’s single-factor test to diagnose the extent to which common method variance was a problem (Harman, 1960). If common method variance is largely responsible for the relationship among the variables, the one-factor CFA model should fit the data well (Korsgaard and Roberson, 1995; Mossholder et al., 1998). Significant common method variance would result in one general factor accounting for the majority of covariance in the variables. A comparison between the hypothesized model (Model 2) and a model with one factor (with all items loading on a unique factor, Model 3) revealed that the former provided a better fit for the data in all the CFA fit measures (one-factor model: χ2(186) = 443.87, p < .001, CFI = .93, TLI = .91, GFI = .92, SRMR = not possible to estimate, RMSEA = .06, and AIC = 133.172)), and the variance of the single factor was 18 percent (Podsakoff et al., 2003). The differences were significant according to a comparison of the models’ χ2 values and degrees of freedom: Δχ2(186) = 2734.04 (p < .001). According to these results, we found no evidence for common method bias in the data.
Correlations between the main variables are presented in Table 2. Results demonstrated they are all significant, with the exception of “self-efficacy” with “proactive personality” and “self-efficacy” with “life engagement.”
Table 2.
Correlations between Proactive Personality, Life Engagement, Quality with Life, Self-Efficacy and Social Support.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Proactive Personality | − | .20** | .29** | .02 | .47** |
| 2. Life Engagement | − | .18* | .05 | .25** | |
| 3. Quality with Life | − | −.26** | .31** | ||
| 4. Self-Efficacy | − | −.25** | |||
| 5. Social Support | − |
p < .05, **p < .01, ***p < .001.
Multiple mediation analysis
Multiple mediation analysis was conducted using AMOS software, version 21.0 (Arbuckle and Wothke, 1999). The effects of multiple mediator variables can be tested individually and simultaneously. The advantage of simultaneous testing is the ability to learn whether the effect of a mediator and other mediator is independent (Chen and Hung, 2016). Quality of life was therefore entered as the dependent variables, while self-efficacy and life engagement are independent variables; social support and proactive personality were entered as mediators. All variables were entered as latent variables, with the exception of Quality of Life which was entered as an observed variable. The bootstrapping method (2000 samples) was used with bias corrected (BC) confidence intervals in order to obtain more powerful confidence interval limits for indirect effects (95% CI, Preacher and Hayes, 2008).
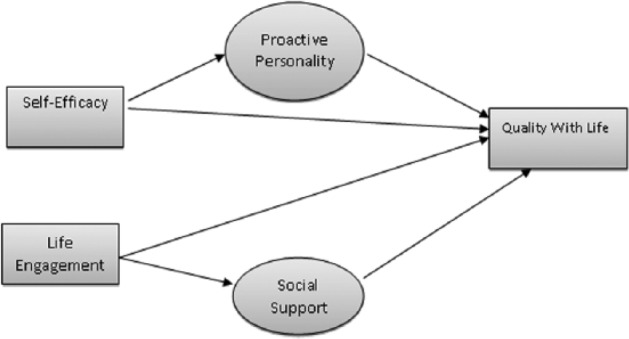
Direct effects
The results revealed that there is a direct effect for self-efficacy on quality of life (β = .23, p < .001), whereas on the other hand there is no significant connection between self-efficacy and proactive personality. In addition, there is a direct effect of self-efficacy on social support (β = .20, p < .001) and, in line with the assumptions, there is a direct effect of life engagement on social support (β = .18, p < .001) and proactive personality (β = . 20, p < .001) (Figure 2).
Figure 2.
Standardized coefficients for the mediating role of proactive personality and social support in association between self-efficacy, life engagement, and quality with life. Solid lines represent significant direct effects while dotted lines represent non-significant direct effect.
Indirect effects
In line with our hypotheses, the relationship between Quality of Life and Engagement with Life is mediated by both social support and proactive personality, whereas the relationship between self-efficacy and quality of life is mediated only by social support. Finally, interesting to note that the relationship between life engagement and social support is mediated by proactive personality (Table 3).
Table 3.
Standardized indirect effects from Self-Efficacy, Life Engagement to Quality with Life through Social Support, and Proactive Personality.
| Predictor | Mediator | Outcome | Estimate | SE | BC 95% CI |
|
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Life Engagement | Social Support | Quality with Life | .07*** | .02 | .032 | .130 |
| Life Engagement | Proactive Personality | Quality with Life | .06*** | .02 | .022 | .105 |
| Self-Efficacy | Social Support | Quality with Life | −.06*** | .02 | −.107 | −.026 |
| Self-Efficacy | Proactive Personality | Quality with Life | .004 | .02 | −.031 | .040 |
| Proactive Personality | Social Support | Quality with Life | .09*** | .03 | .036 | .167 |
| Self-Efficacy | Proactive Personality | Social Support | .01 | .03 | −.052 | .060 |
| Life Engagement | Proactive Personality | Social Support | .08*** | .03 | .038 | .140 |
p < .05; ***p < .001.
Discussion
Although there has been little research conducted on adults with thalassemia, there are numerous studies in the literature that deal with the quality of life in patients with various chronic diseases (Kitaoka et al., 2016; Lam and Lauder, 2000; Megari, 2013). The awareness of suffering from a chronic disorder might result for the patients in a series of possible reactions, first of all the belief of not being able to have control over their lives. Most studies agree, regardless of the nature and severity of the chronic disorder, that the more patients feel supported, the better they will be able to develop appropriate coping activities and to improve the levels of self-efficacy, self-esteem, their commitment to achieve specific goals in life, and the perception of their quality of life. Moreover, some psychological traits (like optimism, sense of coherence, life engagement, sense of control, and challenge) and an internal locus of control are linked to lower levels of emotional stress and generally still improve all psychosocial adjustment indexes (Buscemi et al., 2016; De Sanctis et al., 2013; Masera et al., 1990). Other studies have shown that social support, known in its three basic forms (cognitive, affective, and instrumental), is not only able to support the individuals with chronic illness, but it can protect them from the negative effects related with health problems and negative life events (Greenglass et al., 2006); moreover, social support showed to positively influence the psychosocial adjustment and the daily management of the chronic disease (Gallant, Bodenheimer et al., 2002).
The present study aimed to investigate the influence of some psychosocial factors on the perception of quality of life in patients with thalassemia. The factors being considered are as follows: proactive personality, defined as an attitude to realize the purpose of life; self-efficacy, intended as a general provision to have the resources to overcome the difficulties and achieve the objective; quality of life, namely the perception of subjective well-being that the individual thinks he has reached (Diener et al., 2002, 2003). More factors that have been taken into consideration in the present study are related with the objective and subjective reactions of the individuals to the life demands; life engagement, namely a commitment that persons are willing to make in order to achieve their goals (in terms of well-being) and social support, which is the variable that more than others is able to influence the relationship between the patients’ desire to be satisfied with their life and the conditions that will enable or help them to do so.
Our initial hypothesis was therefore to determine whether there is a relationship between life engagement and self-efficacy, and whether this effect may be mediated by social support and proactive personality. Through a series of mediation analyses (Baron and Kenny, 1986), the results have indicated that the perception of the patient’s quality of life affects their self-efficacy and life engagement, and that this is mediated by proactive personality and social support. The results showed some interesting elements on which it is worthy to reflect on. There is a direct link between self-efficacy and quality of life, but not between life engagement and quality of life. Moreover, there is an indirect effect of social support on proactive personality.
Ultimately, our results showed how patients with thalassemia are more likely to achieve their objectives when there is a personal disposition to do so, namely when there is a proactive personality, and when they perceive a sufficient support from the others.
The present study also suggests some practical implications to improve and invest on social support, to increase and strengthen the network of help and assistance around the patient and not to underestimate the psychosocial aspects of those suffering from a chronic illness. In developed countries, thanks to the combination of medical care and psychosocial support, those individuals are better integrated in society, by making an increasing number of patients with thalassemia end school, establish a steady relationship with peers, find a job, get married, and have a family (Lorig et al., 2001; Ratip and Modell, 1996).
The main limitation of the present study is that it considered only patients with diagnosis of Thalassemia Major; would be interesting also to consider other samples and to compare patients with different diagnosis of thalassemia (e.g. major and intermediate forms of thalassemia).
Acknowledgments
The authors thank Italian League against Hematological Illnesses and Federation of Sicilian Associations for Childhood-Cancer and Thalassemia and SCD (FASTED) and their field staff for conducting the survey and data collection. None played a role in study design, analysis, or preparation of this article, nor in the decision to submit the article for publication.
Hoyle and Kenny define a proximal mediator as a being greater than b (all variables standardized) and a distal mediator as b being greater than.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The survey was approved by the Ethical Commission of Catania University.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Participation in the study was completely voluntary, the data were collected anonymously, and the participants could refuse to participate further at any moment.
References
- Adegbola M. (2007). The relationship among spirituality, self-efficacy, and quality of life in adults with sickle cell disease. Doctoral Dissertation (ProQuest Digital Dissertation, AAT 3289109), The University of Texas at Arlington, Arlington, TX. [Google Scholar]
- Arbuckle JL, Wothke W. (1999) AMOS 4.0 User’s Guide. Chicago, IL: SmallWaters. [Google Scholar]
- Aspinwall LG. (2011) Future-oriented thinking, proactive coping, and the management of threats to health and well-being. In: Folkman S, Nathan P. (eds) The Oxford Handbook of Stress, Health, and Coping. New York: Oxford University Press; pp. 334–365. [Google Scholar]
- Baron RM, Kenny DA. (1986) The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology 51: 1173–1182. [DOI] [PubMed] [Google Scholar]
- Bateman TS, Crant JM. (1993) The proactive component of organizational behavior. Journal of Organizational Behavior 14(2): 103–118. [Google Scholar]
- Bentler PM. (1990) Comparative fit indexes in structural models. Psychological Bulletin 107(2): 238–246. [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Gullette ECD. (2002) Exercise interventions and aging: Psychological and physical health benefits in older adults. In: Schaie KW, Leventhal H, Willis SL. (eds) Effective Health Behavior in Older Adults. New York: Springer. [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, et al. (2002) Patient self-management of chronic disease in primary care. Journal of the American Medical Association 288(19): 2469–2475. [DOI] [PubMed] [Google Scholar]
- Brow JP, McGee HM, O’Boyle CA. (2007) Conceptual approaches to the assessment of quality of life. Psychology & Health 12: 737–751. [Google Scholar]
- Browne MW, Cudeck R. (1993) Alternative ways of assessing model fit. In: Bollen KA, Long (eds) Testing Structural Equation Models. Newbury Park, CA: SAGE, pp. 136–162. [Google Scholar]
- Buscemi A, Rapisarda A, Platania S, et al. (2016) The woman in pregnancy: Body care by knowing of alternative medicine. Acta Medica Mediterranea 32(4): 953–958. [Google Scholar]
- Byrne BM. (2001) Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Chen LJ, Hung HC. (2016) The indirect effect in multiple mediators model by structural equation modeling. European Journal of Business, Economics and Accountancy 4(3): 36–43. Available at: http://www.idpublications.org/ejbea-vol-4-no-3-2016/ [Google Scholar]
- Child D. (2006) The Essentials of Factor Analysis (3rd edn). New York: Continuum International Publishing Group. [Google Scholar]
- Cunningham CJL, De La Rosa GM. (2008) The interactive effects of proactive personality and work-family interference on well-being. Journal of Occupational Health Psychology 13: 271–282. [DOI] [PubMed] [Google Scholar]
- De Sanctis V, Zani B, Basile D, et al. (2013) Come vincere la sfida della talassemia. Resilienza e qualità di vita. Bologna: Persiani Editore. [Google Scholar]
- Devins GM, Binik YM, Hutchinson TA, et al. (1983) The emotional impact of end-stage renal disease: Importance of patients’ perceptions of intrusiveness and control. International Journal of Psychiatry in Medicine 13: 327–343. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, et al. (1985) The Satisfaction with Life Scale. Journal of Personality Assessment 49: 71–75. [DOI] [PubMed] [Google Scholar]
- Diener E, Oishi S, Lucas RE. (2002) Subjective well-being: The science of happiness and life satisfaction. In: Snyder CR, Lopez SJ. (eds) The Handbook of Positive Psychology. New York: Oxford University Press, pp. 63–73. [Google Scholar]
- Diener E, Oishi S, Lucas RE. (2003) Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annual Review of Psychology 54: 403–425. [DOI] [PubMed] [Google Scholar]
- Geiser C. (2013) Data Analysis with Mplus (Methodology in the Social Sciences). New York: Guilford Press. [Google Scholar]
- Gerhardt U. (1991) Stress and stigma explanations of illness. In: Gerhardt U, Wadsworth MEJ. (eds) Stress and Stigma. New York: St. Martin’s Press, pp. 161–204. [Google Scholar]
- Greenglass E, Fiksenbaum L, Eaton J. (2006) The relationship between coping, social support, functional disability and depression in the elderly. Anxiety, Stress and Coping 19(1): 15–31. [Google Scholar]
- Hadi N, Karami D, Montazeri A. (2009) Health-related quality of life in major thalassemic patients. Payesh 8(4): 387–393. [Google Scholar]
- Harman HH. (1960) Modern Factor Analysis. Chicago, IL: University of Chicago Press. [Google Scholar]
- Hu LT, Bentler PM. (1999) Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling 6(1): 1–55. [Google Scholar]
- Huang L, Li L, Zhang Y, et al. (2013) Self-efficacy, medication adherence, and quality of life among people living with HIV in Hunan Province of China: A questionnaire survey. Journal of the Association of Nurses in AIDS Care 24(2): 145–153. [DOI] [PubMed] [Google Scholar]
- Jacobson DE. (1986) Types and timing of social support. Journal of Health and Social Behavior 27: 250–264. Available at: http://www.jstor.org/stable/2136745 [PubMed] [Google Scholar]
- James LR, Mulaik SA, Brett JM. (2006) A tale of two methods. Organizational Research Methods 9: 233–244. [Google Scholar]
- Jerusalem M, Schwarzer R. (1986) Selbstwirksamkeit (Self-efficacy). In: Schwarzer R. (ed.) Skalen zur Befindlichkeit und Persönlichkeit. Berlin: Institut für Psychologie, Freie Universität, pp. 15–28. [Google Scholar]
- Jerusalem M, Schwarzer R. (1992) Self-efficacy as a resource factor in stress appraisal processes. In: Schwarzer R. (ed.) Self-efficacy: Thought Control of Action. Washington, DC: Hemisphere Publishing, pp. 195–213. [Google Scholar]
- Justice B. (1998) A Different Kind of Health: Finding Well-being Despite Illness. Houston, TX: Peak Press. [Google Scholar]
- Kahana E, Kahana B. (1996) Conceptual and empirical advances in understanding well-being through proactive adaptation. In: Bengtson V. (ed.) Adulthood and Aging: Research on Continuities and Discontinuities. New York: Springer, pp. 18–41. [Google Scholar]
- Kitaoka M, Mitoma J, Asakura H, et al. (2016) The relationship between hypertension and health-related quality of life: Adjusted by chronic pain, chronic diseases, and life habits in the general middle-aged population in Japan. Environmental Health and Preventive Medicine 21(4): 193–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. (2005) Principle and Practice of Structural Equation Modeling. New York: Guilford Press. [Google Scholar]
- Korsgaard MA, Roberson L. (1995) Procedural justice in performance evaluation: The role of instrumental and non-instrumental voice in performance appraisal discussions. Journal of Management 21: 657–669. [Google Scholar]
- Lam CLK, Lauder IJ. (2000) The impact of chronic disease on the health related quality of life (HRQOL) of Chinese patients in primary care. Family Practice 17: 159–166. [DOI] [PubMed] [Google Scholar]
- Lorig K, Sobel D, Ritter P, et al. (2001) Effect of a self-management program for patients with chronic disease. Effective Clinical Practice 4(6): 256–262. [PubMed] [Google Scholar]
- Marquez DX, Bustamante EE, Blissmer BJ, et al. (2009) Health promotion for successful aging. American Journal of Lifestyle Medicine 3(1): 12–19. [Google Scholar]
- Masera G, Monguzzi W, Tornotti G, et al. (1990) Psychosocial support in thalassemia major: Monza center’s experience. Haematologica 75(5): 181–90. [PubMed] [Google Scholar]
- Mechanic D. (1995) Sociological dimensions of illness behavior. Social Problems 41: 1207–1216. [DOI] [PubMed] [Google Scholar]
- Megari K. (2013) Quality of life in chronic disease patients. Health Psychology Research 1(3): 141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina G, Colombo E, Cassinerio E, et al. (2008) Psychosocial aspects and psychiatric disorders in young adult with thalassemia major. Internal and Emergency Medicine 3(4): 339–343. [DOI] [PubMed] [Google Scholar]
- Moghadam MP, Nourisancho H, Shahdadi H, et al. (2000) Effects of home-care training on the self-efficacy of patients with beta thalassemia major. Mater Socio-Medica 28(5): 357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossholder KW, Bennett N, Kemery ER, et al. (1998) Relationships between bases of power and work reactions: The mediational role of procedural justice. Journal of Management 24: 533–552. [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee J-Y, et al. (2003) Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology 88(5): 879–903. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40: 879–891. [DOI] [PubMed] [Google Scholar]
- Ratip S, Modell B. (1996) Psychological and sociological aspects of the thalassemias. Seminars in Hematology 33(1): 53–65. [PubMed] [Google Scholar]
- Rook KS. (2014) The health effects of negative social exchanges in later life. Generations: Journal of the American Society on Aging 38(1): 15–23. Available at: http://gateway.webofknowledge.com/ [Google Scholar]
- Rook KS, Underwood LG. (2000) Social support measurement and interventions: Comments and future directions. In: Cohen S, Gottlieb BH, Underwood LG. (eds) Social Support Measurement and Interventions: A Guide for Health and Social Scientists. New York: Oxford University Press, pp. 311–334. [Google Scholar]
- Scheier MF, Wrosch C, Baum A, et al. (2006) The life engagement test: Assessing purpose in life. Journal of Behavioral Medicine 29(3): 291–298. [DOI] [PubMed] [Google Scholar]
- Schwarzer R. (2002) The general self-efficacy scale (GSE). Available at: http://userpage.fu-berlin.de/~health/engscal.htm
- Schwarzer R, Jerusalem M. (1995) Causal and Control Beliefs: Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M. (eds) Measures in Health Psychology: A User’s Portfolio. Windsor: NFER–Nelson, pp. 35–37. [Google Scholar]
- Seibert SE, Kraimer ML, Crant JM. (2001) What do proactive people do? A longitudinal model linking proactive personality and career success. Personnel Psychology 54: 845–874. [Google Scholar]
- Shahnaz I, Karim R. (2014) The impact of Internet addiction on life satisfaction and life engagement in young adults. Universal Journal of Psychology 2(9): 273–284. [Google Scholar]
- Shrout PE, Bolger N. (2002) Mediation in experimental and non experimental studies: New procedures and recommendations. Psychological Methods 7(4): 422–445. [PubMed] [Google Scholar]
- Shumaker SA, Brownell A. (1984) Toward a theory of social support: Closing conceptual gaps. Journal of Social Issues 40: 11–36. [Google Scholar]
- Tabachnick BG, Fidell LS. (2007) Using Multivariate Statistics (5th edn). Boston, MA: Allyn & Bacon. [Google Scholar]
- Thomason B, Jones G, McClure J, et al. (2007) Psychosocial co-factors in HIV illness: An empirically-based model. Psychology & Health 11(3): 385–393. [Google Scholar]
- Trifiletti E, Capozza D, Pasin A, et al. (2009) A validation of the Proactive Personality Scale. TPM—Testing, Psychometrics, Methodology in Applied Psychology 16: 77–93. [Google Scholar]
- World Health Organization (WHO) (1958) The first ten years of the Health Organization. Geneva: WHO. [Google Scholar]
- World Health Organization (WHO) (1993. a) Report of WHOQOL Focus Group Work (MNH/PSF/934). Geneva: WHO. [Google Scholar]
- World Health Organization (WHO) (1993. b) WHOQOL Study Protocol (MNH/PSF/939). Geneva: WHO. [Google Scholar]
- World Health Organization (WHO) (1996) Programme on Mental Health. Geneva: WHO. [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, et al. (1988) The multidimensional scale of perceived social support. Journal of Personality Assessment 52: 30–41. [Google Scholar]