Abstract
Atopic dermatitis (AD) is characterized by a defective skin barrier, which increases the penetration of allergens and pathogens through the skin. The role of interleukin (IL)-17, a pro-inflammatory cytokine, in the pathogenesis of AD remains to be elucidated. The present study aimed to examine the effects of IL-17 on skin barrier proteins in the HaCaT cell line. The expression levels of filaggrin (FLG) and involucrin (IVL) were evaluated by reverse transcription-quantitative polymerase chain reaction and western blot analyses of the HaCaT cells following IL-17 simulation. The role of IL-17 was further examined by using small molecule inhibitors of extracellular signal-regulated kinase (ERK) and P38. Treatment of the HaCaT cells with IL-17 resulted in reduced expression levels of FLG and IVL at the mRNA and protein levels. In addition, the gene expression levels of FLG and IVL were significantly reduced in the HaCaT cells by IL-4. Treatment with the mitogen-activated protein kinase (MAPK) inhibitors, SB203580 and PD98059, significantly inhibited the effects of IL-17 on the gene and protein expression levels of FLG and IVL. Finally, the protein levels of phosphorylated ERK and P38 were significantly increased following IL-17 stimulation. Taken together, the results revealed that IL-17 reduced the expression of FLG and IVL in HaCaT cells, and this effect involved the P38/ERK MAPK signaling pathways.
Keywords: atopic dermatitis, filaggrin, involucrin, interleukin-17, skin barrier
Introduction
Atopic dermatitis (AD) is a chronic, relapsing inflammatory skin disease, which affects ~10–20% and 1–3% of children and adults, respectively, in Western populations (1). Impaired epidermal barrier and immune function defects are common in patients with AD (2,3).
AD is also characterized by a T helper type 2 (Th2) dominance, mediated by pro-Th2 cytokines, thymic stromal lymphopoietin and interleukin (IL)-33, which polarize dendritic cells and promote Th2 responses (4). CD4+ T cells are the primary mediators of cellular immunity and are found in the cell infiltrate of the skin of patients with AD (5). Th17 cells, a distinct lineage of CD4+ helper T cells, are important in the host defense against extracellular fungal and bacterial pathogens, and the pathogenesis of inflammatory and autoimmune disorders (6). IL-17, also known as IL-17A, is the primary effector cytokine of Th17 cells and regulates the functions of multiple cell types (7), including the stimulation of keratinocytes to produce cytokines, chemokines and vascular endothelial growth factor (6).
Another important component in AD is skin integrity (8,9). Of note, skin barrier dysfunction in patients with AD is associated with abnormal protein expression of filaggrin (FLG), loricrin (LOR) and involucrin (IVL), which result in skin impermeability by cross-linking (10,11). FLG is a major structural protein in the stratum corneum of the epidermis, with reduced levels altering the shape of skin corneocytes (12). LOR comprises 80% of the total protein mass in the cornified layer (13), whereas IVL functions as a scaffold to other cross-linked proteins (14). Patients with AD with an acquired defect in the expression of FLG exhibit an atopic inflammatory response (15). Therefore, it is hypothesized that FLG and IVL can be regulated by AD-associated cytokines, including IL-17, as the expression of IL-17 is enhanced in acute lesions in AD skin, compared with that in normal skin, with increased numbers of Th17 cells in the peripheral blood in acute AD (16). IL-17 activates mitogen-activated protein kinases (MAPKs), and the P38/extracellular signal-regulated kinase (ERK) MAPK signaling pathways are involved in the pathogenesis of inflammatory skin diseases, including psoriasis (17). The present study aimed to examine the effects of IL-17 on the expression of FLG and IVL in human HaCaT keratinocytes, and investigate the regulatory mechanism.
Materials and methods
Cell culture
The HaCaT cells (JennioBioech Co., Ltd., Guangzhou, China), a human keratinocyte cell line, were cultured in DMEM (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.) and 100 U/ml of penicillin/streptomycin (Gibco; Thermo Fisher Scientific, Inc.), at 37°C in a humid environment containing 5% CO2. To examine the effects of cytokines on the expression of FLG and IVL, the keratinocytes were differentiated for 5 days by treatment with CaCl2 at 1.3 mmol/l. Cells seeded at 1×105 cells/ml were allowed to grow to 70–80% confluence and were stimulated with medium containing IL-4 (100 ng/ml) or different concentrations of IL-17 (50, 100 and 200 ng/ml) for 24 h at 37°C. IL-4 and IL-17 were purchased from PeproTech, Inc. (Rocky Hill, USA). Following treatment, the cells were harvested for protein extraction. Cells in passages 2–5 were used for all experiments.
Treatment with MAPK inhibitors
The MAPK inhibitors directed against P38 (SB203580; 5 µM), ERK (PD98059; 20 µM), or c-Jun N-terminal kinase (SP600125, 1 µM), respectively, were added to the media for treatment of the HaCaT cells 1 h prior to the addition of IL-17 (100 ng/ml) at 37°C. The cells were cultured for 24 h prior to harvest for mRNA and protein extraction.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis for quantitation of mRNA expression
Total RNA was extracted from the HaCaT cells using the RNeasy Mini kit (Qiagen, Inc., Valencia, CA, USA), according to the manufacturer's protocol. cDNA was reverse transcribed from total RNA using TaqMan RT reagents (Applied Biosystems; Thermo Fisher Scientific, Inc.). The mRNA levels were assessed using the SYBR® Green ER™ qPCR Reagent system (Invitrogen; Thermo Fisher Scientific, Inc.) on an ABI PRISM 7000 sequence detection system (Applied Biosystems; Thermo Fisher Scientific, Inc.). The primers used for RT-qPCR were as follows: FLG forward, 5′-TGAAGCCTATGACACCACTGA-3′ and reverse, 5′-TCCCCTACGCTTTCTTGTCCT-3′; IVL forward, 5′-ACAAGGGAAGAGAGAGCCACTG-3′ and reverse, 5′-TGTAGAGGGACAGAGTCAAGTTCA-3′. The GAPDH gene was used as endogenous control with the following sequences: Forward, 5′-ATCAAGAAGGTGGTGAAGCAGGC-3′ and reverse, 5′-TCAAAGGTGGAGGAGTGGGTGTC-3′. The cycling conditions were as follows: 95°C for 2 min; followed by 45 cycles of denaturation at 95°C for 5 sec, annealing at 60°C for 10 sec and extension at 72°C for 15 sec. Each PCR assay was run in triplicate. The relative gene expression levels were analyzed using the 2−ΔΔCq method (18).
Western blot analysis
The cells were washed three times with cold 1X phosphate-buffered saline and harvested with radioimmunoprecipitation buffer comprising 50 mM Tris-HCl (pH 8.0), 150 mM NaCl, 1% (v/v) Nonidet P-40, 0.5% (w/v) deoxycholate and 0.1% (w/v) SDS, a protease inhibitor cocktail (1:100; Roche Applied Science, Penzberg, Germany) and a phosphatase inhibitor (sodium orthovanadate, 0.5 mg/ml; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany). Protein concentrations were measured using a bicinchoninic Protein Assay kit (Pierce; Thermo Fisher Scientific, Inc.). The proteins (20–40 mg) were first resolved by 12.5% SDS-PAGE, and transferred onto an Immobilon-P1 transfer membrane (Merck KGaA). The membrane was then blocked in 5% milk in Tris-buffered saline-Tween TBST for 30 min at room temperature. Following blocking, the membrane was incubated overnight at 4°C with anti-FLG, anti-IVL, anti-ERK, anti-phosphorylated (p)-ERK (1:500; cat. nos. SC30229, SC28557, SC135900 and SCSC7383, respectively) from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA), anti-p38, anti p-p38 (diluted 1:500; cat. nos. AB7952 and AB4822, respectively) from Abcam (Cambridge, MA, USA), or anti-GAPDH (1:1,000; cat. no. 10494-1-AP; ProteinTech Group, Inc., Chicago, IL, USA) antibodies. The membranes were washed 3 times (5 min each) with PBS containing 0.1% Tween-20 and incubated with horseradish peroxidase-conjugated secondary antibody (cat. no. p0448; Dako; Agilent Technologies, Inc., Santa Clara, CA, USA) at dilution of 1:5,000 in TBST for 1 h at room temperature. The blots were quantified by densitometry using Quantity One software (version 4.6.2; Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
Statistical analyses are presented as the mean ± standard deviation of the mean. Data were analyzed using GraphPad Prism software (version 4.03; GraphPad Software, Inc., La Jolla, CA, USA). Differences among multiple groups were determined using one-way analysis of variance; differences between two groups were assessed using the Tukey-Kramer test. P<0.05 was considered to indicate a statistically significant difference.
Results
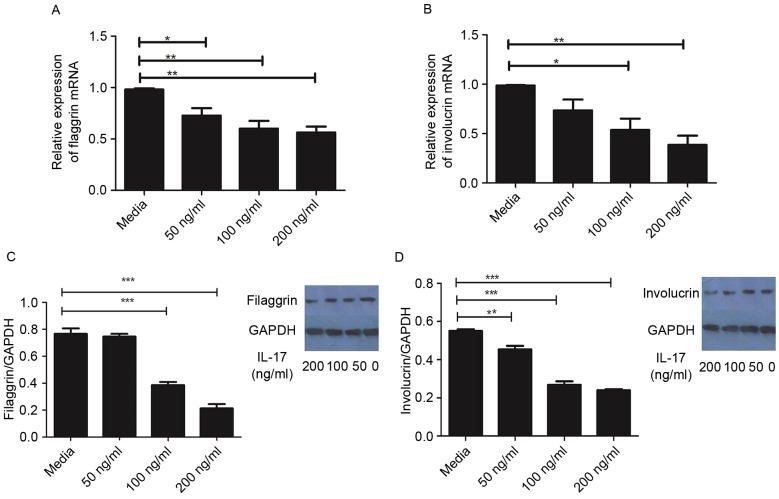
Effect of IL-17 on expression levels of FLG and IVL in HaCaT cells
As demonstrated in Fig. 1A, the mRNA levels of FLG were significantly reduced following treatment with IL-17, compared with that in the control group. Similarly, the gene expression of IVL was significantly reduced by IL-17 at concentrations ≥100 ng/ml, compared with that in the control group (Fig. 1B). In agreement, the protein levels of FLG and IVL were significantly reduced following treatment with IL-17, as determined using western blot analysis (Fig. 1C and D).
Figure 1.
Human HaCaT keratinocytes were treated with various concentrations of IL-17 for 24 h. Gene expression levels of (A) FLG and (B) IVL; protein levels of (C) FLG and (D) IVL. *P<0.05; **P<0.01; ***P<0.001 (n=4). FLG, filaggrin; IVL, involucrin; IL-17, interleukin-17.
IL-17 is similar to Th2 cytokines in regulating skin-barrier proteins
Th2 cytokines can downregulate the expression of FLG, LOR and IVL (15). Therefore, the present study comparatively assessed the effects of IL-4, a Th2 cytokine, and IL-17 on the expression levels of FLG and IVL in the HaCaT cells. In this experiment, cells were treated with 100 ng/ml IL-4 or IL-17 for 24 h, and the gene expression levels of FLG and IVL were evaluated. As exhibited in Fig. 2, the mRNA levels of FLG and IVL were significantly decreased in the HaCaT cells treated with IL-4 or IL-17, compared with the levels in the untreated HaCaT cells (P<0.05). However, no significant differences were found between IL-4 and IL-17 in terms of their ability to reduce the expression of FLG and IVL (Fig. 2A and B).
Figure 2.
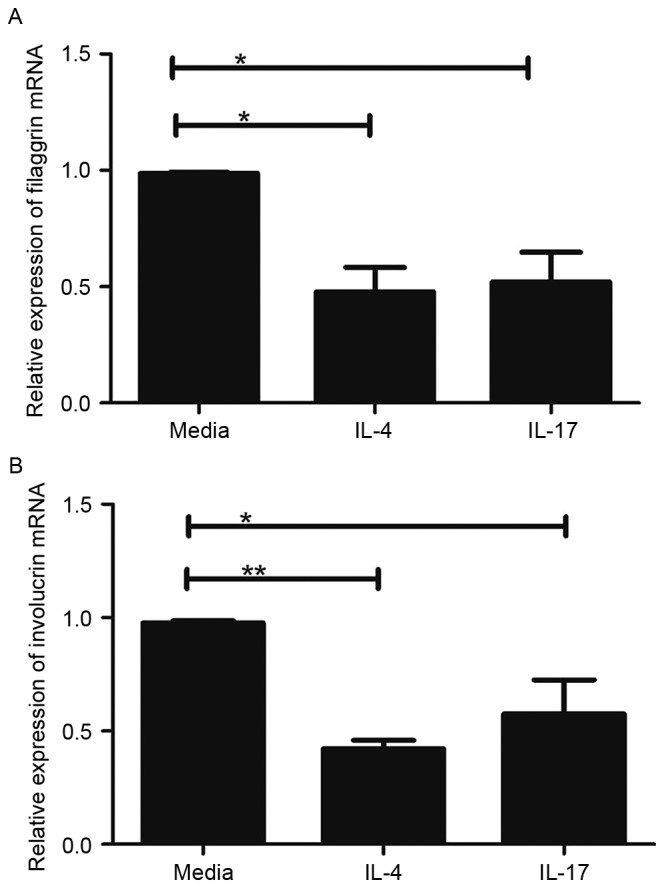
Effects of the IL-4 and IL-17 cytokines on the gene expression levels of (A) FLG and (B) IVL. *P<0.05; **P<0.01 (n=4). FLG, filaggrin; IVL, involucrin; IL, interleukin.
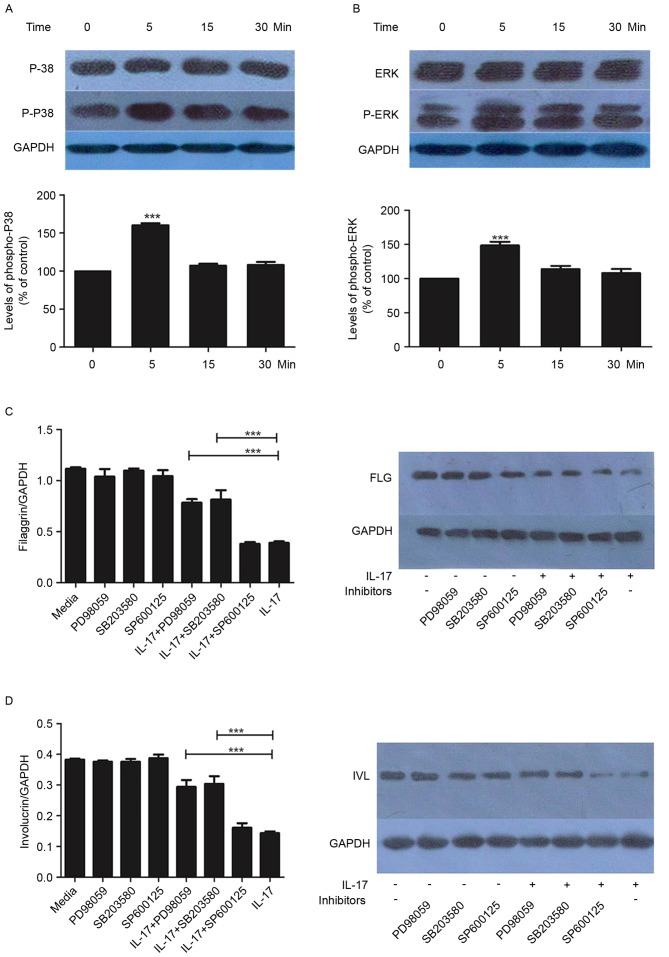
P38/ERK MAPK signaling is upregulated by IL-17
Subsequently, the present study examined the effects of IL-17 (100 ng/ml) on the activation of P38/ERK MAPK effectors p38 and ERK. The phosphorylation of p38 and ERK was increased by IL-17, with statistical significance at the 5-min time point (Fig. 3A and B). This effect was not observed at later time points (15 and 30 min).
Figure 3.
P38 and ERK inhibitors inhibit the IL-17-mediated reduction of FLG and IVL. Phosphorylation levels of (A) P38 and (B) ERK were assessed using western blot analysis following treatment with IL-17 (100 ng/ml). (C) IL-17-induced reduction in the expression of FLG was partially inhibited by P38 and ERK inhibitors at the gene and protein levels. (D) IL-17-induced reduction in the expression of IVL was partially inhibited by P38 and ERK inhibitors. These results are representative of three experiments performed in triplicate. Band intensities were quantified and data are presented as the mean ± standard deviation. ***P<0.001, compared with the control group. FLG, filaggrin; IVL, involucrin; IL-17, interleukin-17; ERK, extracellular signal-regulated kinase; P-/phospho-, phosphorylated.
Effect of MAPK inhibitors on the expression of FLG and IVL
To further examine the mechanisms underlying the regulation of FLG and IVL by IL-17, the HaCaT cells were treated with SP600125, SB203580 or PD98059 in the presence or absence of IL-17. As demonstrated in Fig. 3C and D, SB203580 and PD98059 had significant inhibitory effects on the IL-17-mediated reduction in the expression of FLG and IVL. This was observed at the gene and protein levels (Fig. 3C and D).
Discussion
The present study demonstrated that IL-17 reduced the levels of two skin barrier proteins, FLG and IVL, and that this effect was partially inhibited by the addition of ERK and P38 inhibitors. Therefore, the downregulation of skin barrier proteins by IL-17 may contribute to the pathogenesis of AD.
AD is a genetic disease caused by defects in skin barrier proteins. The disruption of the skin barrier results in contact between epidermal immune cells and antigens from the external environment, leading to intense itching, scratching and inflammation (19). FLG and IVL are proteins belonging to the epidermal differentiation complex, encoded by a cluster of genes on chromosome 1q21, which includes a number of genes important for barrier function (20). The protein levels of FLG and IVL in the skin of patients with AD are reduced (21), suggesting that patients with AD have defects in these two proteins, which are important in skin barrier function.
The IL-17 cytokine family, including IL-17A-F (22), is involved in acute and chronic inflammatory responses (23). IL-17 is the most potent Th17 cytokine, which stimulates the production of chemokines, cytokines and other mediators by upregulating various genes associated with inflammation in target cells, including keratinocytes (24). The number of Th17 cells has been reported to be increased in the peripheral blood and skin tissue samples from patients with AD and psoriasis (16). It is known that keratinocytes are pivotal in skin barrier formation and maintenance (25). IL-17 affects the expression of genes associated with cellular adhesion between keratinocytes, resulting in skin barrier disruption (26), and skin barrier disruption increases the penetration of allergens and the atopic inflammatory response (27,28). In turn, the enhanced atopic immune responses can worsen skin barrier defects in AD. IL-17 has been shown to downregulate FLG and other genes involved in cellular adhesion, with positive effects on the expression of IVL in primary keratinocytes (26,29). In the present study, following treatment of primary keratinocytes with IL-17, reduced mRNA and protein levels of FLG and IVL were observed. The skin in patients with AD at the acute phase is characterized by the overexpression of Th2 cytokines IL-4 and IL-13, which can further downregulate the expression of IVL and LOR through signal transducer and activator of transcription-6 (21). Taken together, the results of the present study and others (26) suggest that IL-17 is important in the skin barrier dysfunction present in patients with AD.
IL-17 is known to activate MAPKs, and P38/ERK MAPK signaling is involved in the pathogenesis of inflammatory skin diseases (17). As described above, increased phosphorylation levels of the ERK and P38 proteins were observed following IL-17 treatment, and this effect was alleviated by MAPK inhibitors. These findings suggested that IL-17 regulated FLG and IVL through the P38 and ERK pathways. Therefore, inhibiting the activity of IL-17 may be a treatment option for patients with chronic inflammatory diseases (30), including AD, restoring barrier function (31). Other cytokines, including the IL-27, IL-21 and IL-10 cytokines, are important factors in the counter regulatory mechanism, which eliminates the immune response and protects from excessive immune responses (32). In addition, previous data revealed the importance of the histamine 4-receptor for the treatment of itching symptoms, suggesting that a multifaceted approach may assist in AD therapy (33).
In conclusion, the present study demonstrated that IL-17 is important in the pathogenesis of AD. Inhibiting the downstream effectors of IL-17 offers a potential therapeutic strategy for AD.
Acknowledgements
This study was supported by Natural Science Foundation Project of CQ CSTC (grant no. cstc2012jjA10017).
Glossary
Abbreviations
- AD
atopic dermatitis
- FLG
filaggrin
- GAPDH
glyceraldehydes-3-phosphate dehydrogenase
- IL
interleukin
- IVL
involucrin
- LOR
loricrin
- MAPK
mitogen-activated protein kinase
- RT-qPCR
reverse transcription-quantitative polymerase chain reaction
- Th2
T helper type 2
References
- 1.Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol. 2006;118:209–213. doi: 10.1016/j.jaci.2006.04.043. [DOI] [PubMed] [Google Scholar]
- 2.Flohr C, England K, Radulovic S, McLean WH, Campbel LE, Barker J, Perkin M, Lack G. Filaggrin loss-of-function mutations are associated with early-onset eczema, eczema severity and transepidermal water loss at 3 months of age. Br J Dermatol. 2010;163:1333–1336. doi: 10.1111/j.1365-2133.2010.10068.x. [DOI] [PubMed] [Google Scholar]
- 3.Zhang H, Guo Y, Wang W, Shi M, Chen X, Yao Z. Mutations in the filaggrin gene in Han Chinese patients with atopic dermatitis. Allergy. 2011;66:420–427. doi: 10.1111/j.1398-9995.2010.02493.x. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd CM, Hessel EM. Functions of T cells in asthma: More than just T (H)2 cells. Nat Rev Immunol. 2010;10:838–848. doi: 10.1038/nri2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai HC, Velichko S, Hung LY, Wu R. IL-17A and Th17 cells in lung inflammation: An update on the role of Th17 cell differentiation and IL-17R signaling in host defense against infection. Clin Dev Immunol. 2013;2013:267971. doi: 10.1155/2013/267971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koga C, Kabashima K, Shiraishi N, Kobayashi M, Tokura Y. Possible pathogenic role of Th17 cells for atopic dermatitis. J Invest Dermatol. 2008;128:2625–2630. doi: 10.1038/jid.2008.111. [DOI] [PubMed] [Google Scholar]
- 7.Nograles KE, Zaba LC, Guttman-Yassky E, Fuentes-Duculan J, Suárez-Fariñas M, Cardinale I, Khatcherian A, Gonzalez J, Pierson KC, White TR, et al. Th17 cytokines interleukin (IL)-17 and IL-22 modulate distinct inflammatory and keratinocyte-response pathways. Br J Dermatol. 2008;159:1092–1102. doi: 10.1111/j.1365-2133.2008.08769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boguniewicz M, Leung DY. Atopic dermatitis: A disease of altered skin barrier and immune dysregulation. Immunol Rev. 2011;242:233–246. doi: 10.1111/j.1600-065X.2011.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung DY. New insights into atopic dermatitis: Role of skin barrier and immune dysregulation. Allergol Int. 2013;62:151–161. doi: 10.2332/allergolint.13-RAI-0564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Candi E, Schmidt R, Melino G. The cornified envelope: A model of cell death in the skin. Nat Rev Mol Cell Biol. 2005;6:328–340. doi: 10.1038/nrm1619. [DOI] [PubMed] [Google Scholar]
- 11.Noh M, Yeo H, Ko J, Kim HK, Lee CH. MAP17 is associated with the T-helper cell cytokine-induced down-regulation of filaggrin transcription in human keratinocytes. Exp Dermatol. 2010;19:355–362. doi: 10.1111/j.1600-0625.2009.00902.x. [DOI] [PubMed] [Google Scholar]
- 12.Elias PM, Hatano Y, Williams ML. Basis for the barrier abnormality in atopic dermatitis: Outside-inside-outside pathogenic mechanisms. J Allergy Clin Immunol. 2008;121:1337–1343. doi: 10.1016/j.jaci.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steven AC, Bisher ME, Roop DR, Steinert PM. Biosynthetic pathways of filaggrin and loricrin-two major proteins expressed by terminally differentiated epidermal keratinocytes. J Struct Biol. 1990;104:150–162. doi: 10.1016/1047-8477(90)90071-J. [DOI] [PubMed] [Google Scholar]
- 14.Kalinin A, Marekov LN, Steinert PM. Assembly of the epidermal cornified cell envelope. J Cell Sci. 2001;114:3069–3070. doi: 10.1242/jcs.114.17.3069. [DOI] [PubMed] [Google Scholar]
- 15.Howell MD, Kim BE, Gao P, Grant AV, Boguniewicz M, DeBenedetto A, Schneider L, Beck LA, Barnes KC, Leung DY. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 2009;124(3 Suppl 2):R7–R12. doi: 10.1016/j.jaci.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Ma L, Xue HB, Guan XH, Shu CM, Wang F, Zhang JH, An RZ. The Imbalance of Th17 cells and CD4 (+) CD25 (high) Foxp3 (+) Treg cells in patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2014;28:1079–1086. doi: 10.1111/jdv.12288. [DOI] [PubMed] [Google Scholar]
- 17.Johansen C, Kragballe K, Westergaard M, Henningsen J, Kristiansen K, Iversen L. The mitogen-activated protein kinases p38 and ERK1/2 are increased in lesional psoriatic skin. Br J Dermatol. 2005;152:37–42. doi: 10.1111/j.1365-2133.2004.06304.x. [DOI] [PubMed] [Google Scholar]
- 18.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 19.Maintz L, Novak N. Getting more and more complex: The pathophysiology of atopic eczema. Eur J Dermatol. 2007;17:267–283. doi: 10.1684/ejd.2007.0200. [DOI] [PubMed] [Google Scholar]
- 20.de Guzman Strong C, Conlan S, Deming CB, Cheng J, Sears KE, Segre JA. A milieu of regulatory elements in the epidermal differentiation complex syntenic block: Implications for atopic dermatitis and psoriasis. Hum Mol Genet. 2010;19:1453–1460. doi: 10.1093/hmg/ddq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim BE, Leung DY, Boguniewicz M, Howell MD. Loricrin and involucrin expression is down-regulated by Th2 cytokines through STAT-6. Clin Immunol. 2008;126:332–337. doi: 10.1016/j.clim.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aggarwal S, Gurney AL. IL-17: Prototype member of an emerging cytokine family. J Leukoc Biol. 2002;71:1–8. [PubMed] [Google Scholar]
- 23.Iwakura Y, Ishigame H, Saijo S, Nakae S. Functional specialization of interleukin-17 family members. Immunity. 2011;34:149–162. doi: 10.1016/j.immuni.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Kirkham BW, Kavanaugh A, Reich K. Interleukin-17A: A unique pathway in immune-mediated diseases: Psoriasis, psoriatic arthritis and rheumatoid arthritis. Immunology. 2014;141:133–142. doi: 10.1111/imm.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feingold KR, Elias PM. Role of lipids in the formation and maintenance of the cutaneous permeability barrier. Biochim Biophys Acta. 2014;1841:280–294. doi: 10.1016/j.bbalip.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Gutowska-Owsiak D, Schaupp AL, Salimi M, Selvakumar TA, McPherson T, Taylor S, Ogg GS. IL-17 downregulates filaggrin and affects keratinocyte expression of genes associated with cellular adhesion. Exp Dermatol. 2012;21:104–110. doi: 10.1111/j.1600-0625.2011.01412.x. [DOI] [PubMed] [Google Scholar]
- 27.Spergel JM, Mizoguchi E, Brewer JP, Martin TR, Bhan AK, Geha RS. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 1998;101:1614–1622. doi: 10.1172/JCI1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Benedetto A, Rafaels NM, McGirt LY, Ivanov AI, Georas SN, Cheadle C, Berger AE, Zhang K, Vidyasagar S, Yoshida T, et al. Tight junction defects in patients with atopic dermatitis. J Allergy Clin Immunol. 2011;127:773–786. e1-e7. doi: 10.1016/j.jaci.2010.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen JQ, Man XY, Li W, Zhou J, Landeck L, Cai SQ, Zheng M. Regulation of involucrin in psoriatic epidermal keratinocytes: The roles of ERK1/2 and GSK-3β. Cell Biochem Biophys. 2013;66:523–528. doi: 10.1007/s12013-012-9499-y. [DOI] [PubMed] [Google Scholar]
- 30.Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic inflammation. Nat Rev Drug Discov. 2012;11:763–776. doi: 10.1038/nrd3794. [DOI] [PubMed] [Google Scholar]
- 31.Simon D, Lang K Kernland. Atopic dermatitis: From new pathogenic insights toward a barrier-restoring and anti-inflammatory therapy. Curr Opin Pediatr. 2011;23:647–652. doi: 10.1097/MOP.0b013e32834cad0a. [DOI] [PubMed] [Google Scholar]
- 32.Noh G, Lee J. Atopic dermatitis and cytokines: The immunoregulatory and therapeutic implications of cytokines in atopic dermatitis-part II: Negative regulation and cytokine therapy in atopic dermatitis. Recent Pat Inflamm Allergy Drug Discov. 2012;6:248–261. doi: 10.2174/187221312802652802. [DOI] [PubMed] [Google Scholar]
- 33.Roesner LM, Werfel T, Heratizadeh A. The adaptive immune system in atopic dermatitis and implications on therapy. Expert Rev Clin Immunol. 2016;12:787–796. doi: 10.1586/1744666X.2016.1165093. [DOI] [PubMed] [Google Scholar]