Abstract
Recent studies have indicated the existence of an endogenous sulfur dioxide (SO2)-generating system in the cardiovascular system. The present study aimed to discuss the function and regulatory mechanism of gaseous signal molecule SO2 in inhibiting apoptosis and endoplasmic reticulum stress (ERS) via the Hippo-MST signaling pathway to improve myocardial fibrosis of diabetic rats. A total of 40 male Sprague-Dawley rats were randomly divided into four groups (10 rats per group): Normal control group (control group), diabetic rats group [streptozotocin (STZ) group], SO2 intervention group (STZ+SO2 group) and diabetes mellitus rats treated with L-Aspartic acid β-hydroxamate (HDX) group (HDX group). Diabetic rats models were established by intra-peritoneal injection of STZ (40 mg/kg) Following model establishment, intra-peritoneal injection of Na2SO3/NaHSO3 solution (0.54 mmol/kg) was administered in the STZ+SO2 group, and HDX solution (25 mg/kg/week) was administered in the HDX group. A total of 4 weeks later, echocardiography was performed to evaluate rats' cardiac function; Masson staining, terminal deoxynucleotidyl transferase dUTP nick end labeling staining and transmission electron microscopy examinations were performed to observe myocardial morphological changes. ELISA was employed to determine the SO2 content. Western blot analysis was performed to detect the expression of proteins associated with apoptosis, ERS and the Hippo-MST signalling pathway. Compared with the control group, the STZ group and HDX group had a disordered arrangement of myocardial cells with apparent myocardial fibrosis, and echocardiography indicated that the cardiac function was lowered, there was an obvious increase of apoptosis in myocardial tissue, the expression levels of apoptosis-associated protein B-cell lymphoma associated protein X, caspase-3 and caspase-9 were upregulated, and Bcl-2 expression was downregulated. The expression of ERS and Hippo-MST pathway-associated proteins, including CHOP, GRP94, MST1 and MST2, were significantly upregulated. By contrast, these above-mentioned changes were reversed by SO2 treatment. Compared with STZ group, the HDX group had a further increase of myocardial fibrosis and apoptosis, while there were no statistically significant differences in the expression of Bax/Bcl-2, caspase-3, caspase-9 and ERS and Hippo-MST pathway-associated proteins. The results of the present study demonstrated that the gaseous signal molecule SO2 can effectively improve the myocardial fibrosis of diabetic rats, and its mechanism may be associated with reduced apoptosis and ERS by downregulated Hippo-MST pathway.
Keywords: sulfur dioxide, myocardial fibrosis, Hippo-MST pathway, endoplasmic reticulum stress, apoptosis
Introduction
With the continuous change in modern lifestyles, the incidence rate of diabetes is on the rise (1). Diabetic cardiomyopathy (DC) is a chronic complication of diabetes, a specific myocardial lesion independent from valvular heart disease, coronary heart disease, congenital heart disease and other diseases. Such disease is one of the major causes of death among diabetic patients (2). The pathological changes of DC are mainly characterised by cardiomyocyte hypertrophy, apoptosis and necrosis as well as progressive myocardial interstitial fibrosis (3). Myocardial fibrosis is an important marker of the myocardial remodelling of DC and the major cause of left ventricular dysfunction. Moreover, the mechanism involved is considerably complicated. Evidence shows that the pathogenesis of myocardial fibrosis is associated with oxidative stress, endoplasmic reticulum stress (ERS), apoptosis (4–8). However, the specific regulatory mechanism remains unclear.
Sulfur dioxide (SO2) is a poisonous, small-molecule gas. However, recent studies have found the existence of an endogenous SO2-generating system in the cardiovascular system. As a new gaseous signalling molecule following the discovery of NO, CO and hydrogen sulfide (H2S), endogenous SO2 performs the following functions: Vasodilation, suppression of inflammation and improvement of vascular collagen remodelling in the cardiovascular system (9). However, whether SO2 takes part in the occurrence and development of DC and its internal mechanism remains an open issue.
As one of the prevalent cell signalling mechanisms of pathological and physiological processes in animals, the Hippo-MST signalling pathway participates in the regulation of cell proliferation and apoptosis (10–12). The components of the Hippo-MST pathway mainly include MST1/2, Sav, LATS1/2 and MOBI. MST1/2 is a protein kinase of the STE20 family and could phosphorylate the core members of the Hippo-MST pathway-Sav1, LATS1/2 and MOBI. At present, MST has been proven to play a role in regulating apoptosis in some animal models in the presence of cardiovascular diseases. It can also induce cell death by activating LATS. The upregulation of MST1 expression or its specific overexpression has been confirmed to induce the apoptosis of myocardial cells. The Hippo-MST pathway is also known to participate in the regulatory mechanism of myocardial fibrosis, and the overexpression of MST1 may result in myocardial fibrosis. However, the role of the Hippo-MST pathway in diabetic myocardial fibrosis and its mechanism of action remain unclear.
In the present research, we propose to establish an streptozotocin (STZ)-induced model of diabetic rats with intervention by a SO2 donor and endogenous SO2 synthase inhibitor L-Aspartic acid β-hydroxamate (HDX) so as to explore the role of the gaseous signalling molecule SO2 in inhibiting apoptosis by regulating the Hippo-MST pathway and improving ERS and myocardial fibrosis of diabetic rats.
Materials and methods
Experimental animals
Adult male Sprague-Dawley (SD) rats (240±20 g) were obtained from the Animal Experiment Centre of South China University. Prior to the experiments, the SD rats were fed with standard rat chow and normal water ad libitum. The rats were housed and separated by treatment group under a 12 h light-dark cycle at a temperature of 23±1°C and humidity of 60%. The rats were fed according to institutional policies, and all the experiments were carried out with the approval of the University Committee on the Use and Care of Animals of South China University.
Chemicals and reagents
Na2SO3, NaHSO3 and HDX were purchased from Sigma-Aldrich (St. Louis, MO, USA). STZ was purchased from MP Biomedicals, LLC (Santa Ana, CA, USA). The antibodies for matrix metalloproteinase (MMP)9, MMP24, tissue inhibitor of metalloproteinase (TIMP)1 and GAPDH were purchased from Wuhan Boster Biological Technology, Ltd. (Wuhan, China). The dilution rate of these antibodies was 1:400. Furthermore, the antibodies for MST1, MST2, MOB1, LATS1, BIP, PDI and ERO1-L were purchased from Cell Signalling Technology (Danfoss, MA, USA). The antibodies for Bcl-2, Bax, caspase-3, caspase-9, CHOP, GRP94, eIF2α and GOT1 were purchased from Proteintech Group, Inc. (Chicago, IL, USA). The dilution rate of these antibodies was 1:1,000. Anti-rabbit secondary antibody and anti-rat secondary antibody were also purchased from Proteintech Group, Inc. The cell lysis buffer for western blot analysis, Bicinchoninic Acid (BCA) Protein Assay kit, Enhanced Chemiluminescence Reagent kit and SDS-PAGE Gel Preparation kit were obtained from Beyotime Institute of Biotechnology (Shanghai, China). The ELISA kit of SO2 was obtained from Mlbio Co. (Shanghai, China).
Model establishment and grouping
Forty experimental rats were randomly divided into four groups: Normal group (control group), diabetes mellitus rats (STZ 40 mg/kg) group (STZ group), diabetes mellitus rats (STZ 40 mg/kg) treated with SO2 (STZ+SO2 group) and diabetes mellitus rats (STZ 40 mg/kg) treated with HDX group (HDX group). Each rat in the STZ group, STZ+SO2 group and HDX group were made diabetic via a single intraperitoneal injection of 40 mg/kg body weight STZ. At the same time, the rats of the control group were treated with saline once (i.p.). Blood glucose from the rat tail vein was detected with a blood glucose monitor. The rats were considered diabetic when the concentration of glucose was higher than 16.7 mmol/l 3 days after STZ injection. Then, SO2 donor (Na2SO3/NaHSO3) was administered to the rats of the STZ+SO2 group. Na2SO3/NaHSO3 was freshly dissolved in saline at 0.54:0.18 mmol/kg before injection. The HDX group was treated with HDX (25 mg/kg, i.p.) once a week. The control group and STZ group were intraperitoneally injected with physiological saline every day. The experiment lasted for four weeks.
Specimen collection and processing
After 4 weeks, the rats were weighed and subjected to echocardiography. They were then anesthetised with chloral hydrate (350 mg/kg). The hearts of the rats were lavaged with ice-cold normal saline before they were removed and weighed. Parts of the heart tissues were preserved at −80°C for the experiment. The remaining heart tissues were fixed in 4% paraformaldehyde in phosphate-buffered saline and then embedded in paraffin.
Echocardiography analysis
After 4 weeks, the mice were anesthetised with chloral hydrate (350 mg/kg, i.p.). We used transthoracic echocardiography to test left ventricular function. The left ventricular end-diastolic dimension (LVEDD), left ventricular end-systolic diameter (LVESD), left ventricular ejection fraction (LVEF) and left ventricular fraction shortening (LVFS) were measured to evaluate heart function.
Histopathology analysis of myocardial fibres
After 4 weeks, the animals that survived were sacrificed. Their hearts were removed immediately and then fixed in 4% paraformaldehyde. Each heart was embedded in paraffin, dewatered with alcohol, embedded in paraffin again and sliced up in 5 µm sections. These sections were stained using a Masson staining kit and observed under an optical microscope.
SO2 content assay
Myocardial SO2 content was assayed by ELISA. The ELISA kit of SO2 was obtained from Mlbio Co. The steps were taken following the manufacturer's instructions.
TUNEL assay
The myocardial tissue of each rat was fixed in 10% formalin and embedded in paraffin. It was then processed for TUNEL assay. The slides were treated with H2O2 and incubated with a reaction mixture containing TdT and digoxigenin-conjugated dUTP for 1 h at 37°C. Labelled DNA was visualised with a peroxidase-conjugated anti-digoxigenin antibody using 3,3′-diaminobenzidine (DAB) as the chromogen. Rat testicular tissue was used as positive control in the TUNEL assay.
Transmission electron microscopy (TEM)
The left ventricular tissues in each group were cut into small pieces on the ice and then immersion-fixed in 2.5% glutaraldehyde, post-fixed in 1% osmium tetroxide and dehydrated in a series of graded ethanol solutions. Ultrathin sections were cut and stained with uranyl acetate and lead citrate. Ultrathin sections were observed via electron microscopy.
Western blot analysis
Total proteins were extracted in ice-cold radioimmunoprecipitation assay buffer containing protease inhibitors (Beyotime Institute of Biotechnology) and then quantified using a BCA protein assay kit. Proteins were denatured, separated by SDS-PAGE electrophoresis and transferred to a PVDF membrane via wet transfer method. The membranes were blocked with 5% skimmed milk in Tris-buffered saline with Tween-20 (TBST) for 2 h at room temperature. The membranes were incubated with a blocking solution containing primary antibodies (anti-GAPDH, 1:400; anti-MMP9, 1:400; anti-MMP24, 1:400; anti-TIMP1, 1:400; anti-Bax, 1:1,000; anti-Bcl-2, 1:1,000; anti-caspase-3, 1:1,000; anti-caspase-9, 1:1,000; anti-GOT1, 1:1,000; anti-CHOP, 1:1,000; anti-GRP94, 1:1,000; anti-eIF2α, 1:1,000; anti-BIP, 1:1,000; anti-PDI, 1:1,000; anti-ERO1-L, 1:1,000; anti-MST1, 1:1,000; anti-MST2, 1:1,000; anti-MOB1, 1:1,000; anti-LATS1, 1:1,000) overnight at 4°C. After washing three times with TBST, the membranes were incubated with horseradish peroxidase-conjugated secondary antibody (1:2,000) for 1 h at room temperature. Next, the membrane was washed in TBST buffer thrice. Finally, these membranes were subjected to chemiluminescence detection assay. The bands were analysed with a Molecular Imager VersaDoc MP 5000 system (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
Data were expressed as mean ± standard deviation. The statistical differences among the groups were assessed via one-way analysis of variance with SPSS 18.0 (SPSS, Inc., Chicago, IL, USA). Comparisons between two groups were made using the Student-Newman-Keuls test. A P-value of <0.05 was considered statistically significant.
Results
SO2 improves myocardial fibrosis in diabetic rats
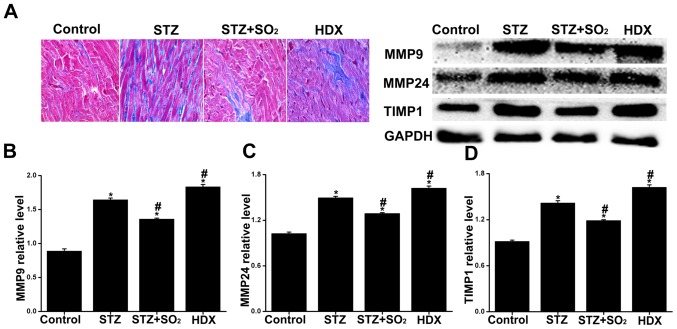
Four weeks later, there were 10, 7, 9, 7 mice that had survived in the control group, STZ group, STZ+SO2 and HDX group respectively. In evaluating the deposition of collagen fibres in the myocardium, Masson staining was carried out at the end of the experiment. The result revealed the deposition of the collagen fibres. Blue staining demonstrated the intensity of myocardial fibrosis. As indicated by the result of Masson staining (Fig. 1A), myocardial fibrosis was barely observed in the control group. In the STZ group, the myocardial cells showed a disorderly arrangement, and myocardial fibres significantly increased. Unlike in the STZ group, the myocardial fibrosis was obviously alleviated in the STZ+SO2 group. Moreover, the myocardial fibrosis was more serious in the HDX group than in the STZ group. On the whole, these results above suggest that treatment with the SO2, decreases diabetes-induced myocardial fibrosis. Therefore, it indicates that SO2 improves myocardial fibrosis in diabetic rats.
Figure 1.
SO2 improves myocardial fibrosis in diabetic rats. (A) Morphological changes in myocardium assessed by Masson staining. Images were acquired at ×400 magnification. Expression levels of (B) MMP9, (C) MMP24 and (D) TIMP1 in each group. Date are expressed as mean ± standard deviation (n=3). *P<0.05 vs. control group; #P<0.05 vs. STZ group. SO2, sulfur dioxide; MMP, matrix metalloproteinase; TIMP, tissue inhibitor of metalloproteinase; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
Effects of SO2 on MMP9, MMP24 and TIMP1 expression in diabetic rats
The balance of MMPs/TIMPs determines the ratio of collagen synthesis and degradation. Therefore, we determined the expressions of MMP9 (Fig. 1B), MMP24 (Fig. 1C) and TIMP1 (Fig. 1D) to reflect fibrosis to some degree. Compared with the control group, the expression levels of MMP9, MMP24 and TIMP1 in STZ group, STZ+SO2 group and HDX group were significantly increased. Compared with STZ group, the myocardial expression levels of MMP9, MMP24 and TIMP1 were significantly reduced in STZ+SO2 group, meanwhile, the expression levels of MMP9, MMP24 and TIMP1 were obviously increased in HDX group.
SO2 improves cardiac function in diabetic rats
In this study, the parameters of cardiac function evaluated via echocardiography, namely, LVEDD, LVESD, ejection fraction (EF) and fractional shortening (FS), were measured to evaluate left ventricular function. Compared with the control group, LVEDD and LVESD increased more significantly in the STZ group and HDX group EF and FS decreased more significantly (by 17.32 and 13.5%, respectively) in the STZ group and (by 21.55 and 15.92%, respectively) HDX group. Compared with STZ group, the EF and FS increased more significantly in the STZ+SO2 group, while the LVEDD and LVESD obviously decreased in the STZ+SO2 group. Moreover, compared with STZ group, EF and FS slightly decreased in the HDX group, while the LVEDD and LVESD slightly increased in the HDX group, but there were not statistically significant (Table I). Taken together, our results indicate that SO2 improves diabetic-induced the decrease of cardiac function.
Table I.
SO2 improves cardiac function in diabetic rats. Effects of SO2 on LVEDD, LVESD, EF and FS% in diabetic rats.
| Group | control group | STZ group | STZ+SO2 group | HDX group |
|---|---|---|---|---|
| LVEDD (mm) | 4.77±0.59 | 6.27±0.32a | 5.26±0.31b | 6.50±0.42a |
| LVESD (mm) | 2.50±0.18 | 4.17±0.21a | 3.10±0.26b | 4.56±0.71a |
| EF (%) | 85.35±2.27 | 68.03±0.90a | 79.40±1.56b | 63.80±3.68a |
| FS (%) | 46.27±2.73 | 32.77±1.46a | 41.57±1.43b | 30.35±2.62a |
Values are expressed as mean ± standard deviation (n=7).
P<0.05 vs. control group
P<0.05 vs. STZ group. SO2, sulfur dioxide; LVEDD, left ventricular end-diastolic dimension; LVESD, left ventricular end-systolic diameter; EF, ejection fraction; FS, fractional shortening; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
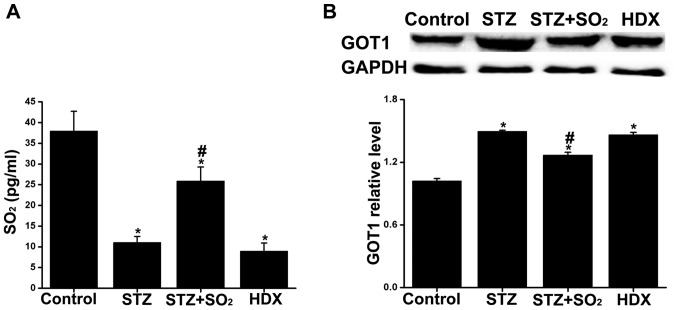
SO2 content in each group
To determine whether diabetes-induced myocardium damage was related to the decreased generation of endogenous SO2, we assayed SO2 content via ELISA. In comparison with those in the control group, the expression levels of SO2 in the STZ group and HDX group were significantly decreased. In comparison with that in the STZ group, the myocardial expression of SO2 was significantly increased in the STZ+SO2 group. Nevertheless, no significant changes were observed in the HDX group in comparison with the STZ group (Fig. 2A). The results demonstrate that the content of SO2 in diabetic rats were significantly decreased.
Figure 2.
(A) Quantification of myocardial SO2 content in rats from each group and SO2 synthase aspartate aminotransferase (GOT1) protein expressions in each group (B) Data are expressed as mean ± standard deviation (n=3). *P<0.05 vs. control group; #P<0.05 vs. STZ group. SO2, sulfur dioxide; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
GOT1 protein expressions in each group
The expressions of SO2 synthase aspartate aminotransferase (GOT1) protein in myocardium tissues were measured by western blot analysis. In comparison with that in the control group, the expression levels of GOT1 in the STZ group, STZ+SO2 group, and HDX group were significantly increased. In comparison with the STZ group, the myocardial expression of GOT1 was significantly decreased in the STZ+SO2 group. Nevertheless, no significant changes were observed in the HDX group in comparison with the STZ group (Fig. 2B).
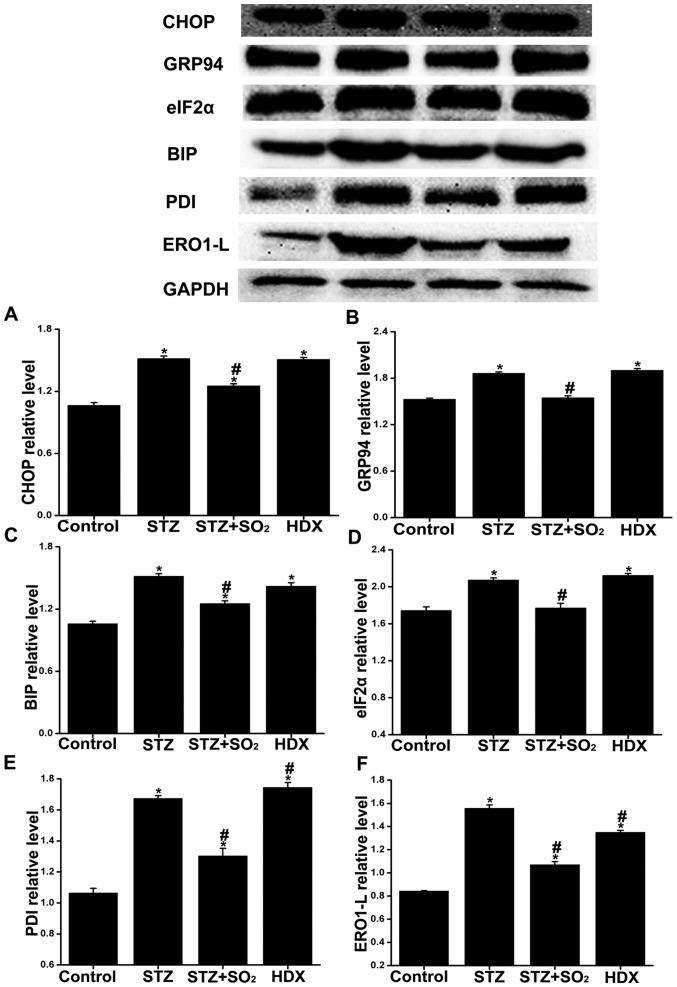
SO2 can reduce ERS in diabetic rats
By performing western blot analysis, we determined the expressions of CHOP (Fig. 3A), GRP94 (Fig. 3B), BIP (Fig. 3C), eIF2α (Fig. 3D), PDI (Fig. 3E) and ERO1-L (Fig. 3F) to observe ERS in the myocardium and to assess whether SO2 protects against ERS. Unlike those in the control group, the expressions of CHOP, eIF2α, GRP94, BIP, PDI and ERO1-L were significantly increased in the STZ group and HDX group. In comparison with those in the STZ group, the expression levels of CHOP, eIF2α, GRP94, BIP, PDI and ERO1-L in the STZ+SO2 group significantly decreased. The expression levels of some ERS protein markers slightly increased in the HDX group, but the change was not statistically significant. Our data thus indicate that SO2 inhibits the expression of proteins associated with ERS in diabetic rats.
Figure 3.
SO2 can reduce endoplasmic reticulum stress in diabetic rats. Expression levels of (A) CHOP, (B) GRP94, (C) BIP, (D) eIF2α, (E) PDI and (F) ERO1-L in each group. Data are expressed as mean ± standard deviation (n=3). *P<0.05 vs. control group; #P<0.05 vs. STZ group. SO2, sulfur dioxide; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
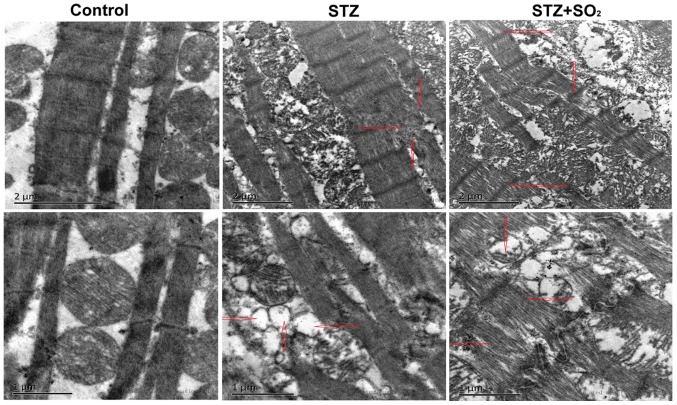
Effects of SO2 on myocardial ultrastructure in diabetic rats
To investigate the internal mechanism underlying the SO2-elicited beneficial effects against diabetes, we performed TEM in our observation of the endoplasmic reticulum and myocardial fibres. As indicated by the TEM results, the myocardial fibres were arranged normally, and the endoplasmic reticulum was normal and showed no swelling in the control group. In some myocardial tissues from the STZ group, the myocardial fibres were arranged disorderly and were dropsical, and focal cytolysis necrosis was observed. Swelling and vesiculation of the endoplasmic reticulum were also observed in the STZ group. These changes in the STZ group obviously improved in the STZ+SO2 group. Additionally, the myocardial ultrastructural changes in the HDX group were similar to those in the STZ group (Fig. 4). These results above indicates that SO2 improves the injury of myocardial ultrastructure in diabetic rats.
Figure 4.
SO2-alleviated myocardial ultrastructural disorder and swelling of the endoplasmic reticulum in diabetic rats. Transmission electron micrographs at bars of 1 and 2 µm. SO2, sulfur dioxide; STZ, streptozotocin.
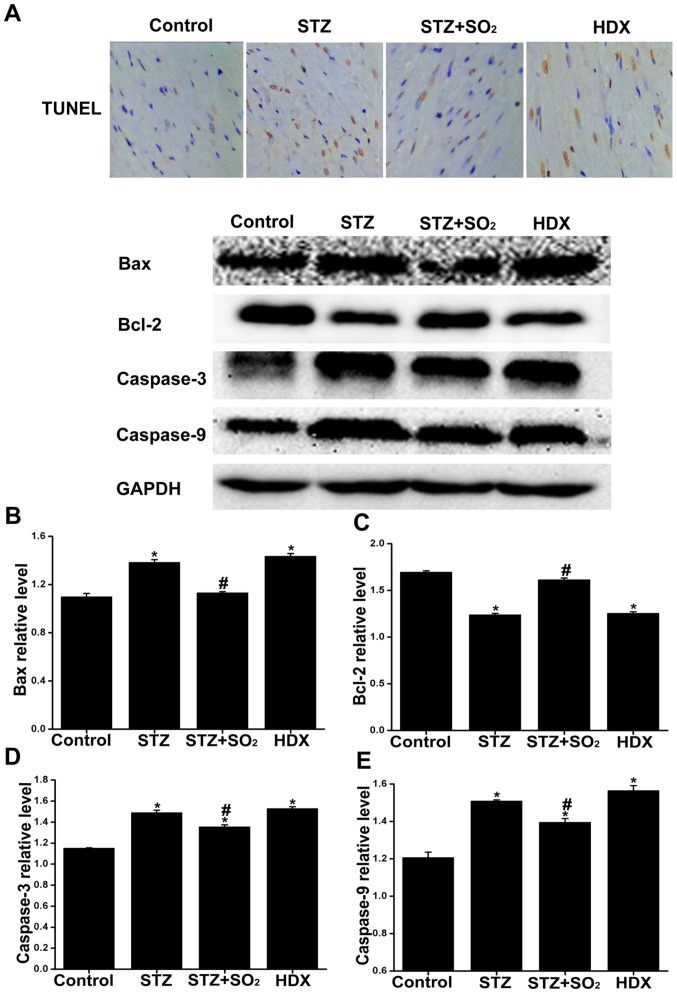
SO2 can reduce cardiomyocyte apoptosis in diabetic rats
In this experiment, we used TUNEL assay to detect apoptosis in heart tissue. The number of apoptotic cells increased more obviously in the STZ group than in the control group. We also found that under SO2 treatment, the number of TUNEL-positive cells decreased obviously in the STZ+SO2 group. In comparison with those in the STZ group, the apoptotic cells in the HDX group obviously increased (Fig. 5A). These results indicate that SO2 suppresses diabetic-induced cell apoptosis indiabetic rats.
Figure 5.
SO2 reduces cardiomyocyte apoptosis in diabetic rats. (A) Representative photomicrographs of heart tissues showing TUNEL-positive (apoptotic) myocardiocytes. Images were acquired at ×400 magnification. Expression levels of (B) Bax, (C) Bcl-2, (D) caspase-3 and (E) caspase-9 in each group. Data are expressed as mean ± standard deviation (n=3). *P<0.05 vs. control group; #P<0.05 vs. STZ group. SO2, sulfur dioxide; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
SO2 can reduce myocardial apoptosis in diabetic rats
To expound the molecular basis of the increased myocardial apoptosis in the diabetic rats, we examined the expression levels of Bax (Fig. 5B), Bcl-2 (Fig. 5C), caspase-3 (Fig. 5D) and caspase-9 (Fig. 5E) via western blot analysis. The expressions of Bax, caspase-3 and caspase-9 expression increased, and the expression of Bcl-2 decreased in the STZ group in comparison with the control group. However, under SO2 treatment, the expression of Bcl-2 increased, and those of Bax, caspase-3 and caspase-9 decreased in the STZ+SO2 group in comparison with the STZ group. These results indicated that diabetes-induced apoptosis was likely mediated, at least in part, by the Bcl-2/Bax-mediated caspase-3 and caspase-9 activation pathway in the heart. Our results thus indicate that SO2 can reduce myocardial apoptosis in diabetic rats.
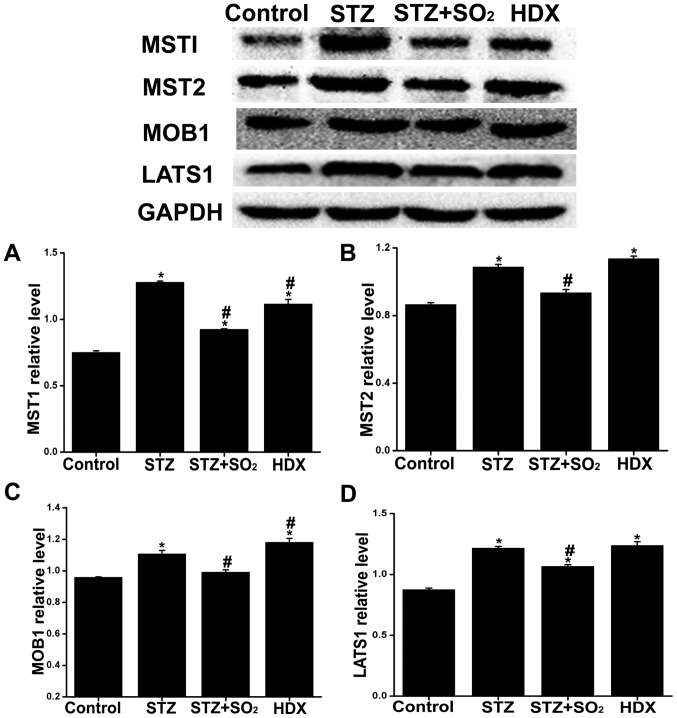
Effects of SO2 on diabetes-induced change in the Hippo-MST signalling pathway
To demonstrate the Hippo-MST signalling pathway involved in the development of DC, we detected the expression of proteins related to the Hippo-MST signalling pathway via western blot analysis. In comparison with those in the control group, the expressions of MST1 (Fig. 6A), MST2 (Fig. 6B), MOB1 (Fig. 6C), and LATS1 (Fig. 6D) in the STZ group and HDX group significantly increased. In comparison with those in the STZ group, the expressions of MST1, MST2, MOB1 and LATS1 in STZ+SO2 group significantly decreased. Taken together, our results indicate that high glucose induced the activation of Hippo-MST signalling pathway and SO2 can downregulate the expression of proteins associated with Hippo-MST signalling pathway in diabetic rats.
Figure 6.
Effects of SO2 on diabetes-induced change in Hippo-MST signalling pathway. Expression levels of (A) MST1, (B) MST2, (C) MOB1 and (D) LATS1 in each group. Data are expressed as mean ± standard deviation (n=3). *P<0.05 vs. control group; #P<0.05 vs. STZ group. SO2, sulfur dioxide; STZ, streptozotocin; HDX, L-Aspartic acid β-hydroxamate.
Discussion
Diabetic mellitus (DM) is a global health issue that has attracted significant attention. As one of the major complications of DM, DC imposes a severe threat on human health (13). The crucial pathological changes of myocardial fibrosis in relation to the occurrence and development of DM are also an important cause of myocardial remodelling and heart failure. In this research, a model of diabetic rats was built with the intraperitoneal injection of STZ. Masson staining and TEM revealed that collagen deposition obviously increased in the myocardial tissue of the diabetic rats, and the western blot analysis indicated the significant maladjustment of MMPs/TIMPs in the myocardial tissue of the diabetic rats. The results suggest an obvious interstitial fibrosis in the myocardial tissue of the diabetic rats. Echocardiography also further confirmed the decline of cardiac function of the diabetic rats. Myocardial fibrosis participates in the mechanism of the occurrence and development of DC, and it is closely associated with the poor prognosis of diabetic patients. However, the mechanism of diabetic myocardial fibrosis has not been completely understood. Some studies have shown a close correlation between diabetic myocardial fibrosis and oxidative stress, ERS, apoptosis.
Currently, apoptosis is known to take part in the occurrence and development of DC (14,15). When the body is under common apoptosis-promoting stimulations of diabetes, such as high glucose, oxidative stress and metabolic disorders, the caspase cascade pathways in the myocardial tissue are activated one by one, thus inducing the occurrence of apoptosis. The activation of caspase-3 is a key link in the apoptosis signalling pathway (16), and Bcl-2 has been proven to block the activation of caspase and inhibit cell apoptosis (17). The result of TUNEL staining revealed that the number of apoptotic cells in the myocardial tissues of the diabetic rats increased more remarkably relative to the control group. At the same time, the expressions of the pro-apoptotic proteins caspase-3, caspase-9 and Bax in the myocardial tissue was significantly upregulated, and the expression of the anti-apoptotic protein Bcl-2 was obviously downregulated. ERS has been also found to take part in the occurrence mechanism of DC, and it serves as the initial common channel of oxidative stress and other cell stress reactions. However, sustained or extremely strong ERS may result in cell apoptosis. ERS in diabetics may be induced by numerous factors, including hyperglycemia, oxidative stress, activation of RAS system and lipid metabolism. Some studies have found that ERS in myocardial cells is excessively activated (18,19). The current research found that the ERS-associated proteins of DC, such as CHOP, GRP94, BIP and eIF2α, were obviously upregulated. Furthermore, TEM showed that swelling occurred in the endoplasmic reticulum of the myocardial cells and that the volume increased, thereby suggesting excessively activated ERS in the myocardial tissue as well as endoplasmic reticulum damage. ERS may activate CHOP, and the upregulation of CHOP may inhibit Bcl-2 expression, thus inducing ERS-associated apoptosis. In the present work, we found that the endoplasmic reticulum was obviously activated in the myocardial tissues of the diabetic rats and that CHOP expression was upregulated, thereby suggesting that ERS participated in the occurrence mechanism of apoptosis in the process of diabetic myocardial fibrosis.
As one of the prevalent cell signalling mechanisms of pathological and physiological processes in animals, the Hippo-MST signalling pathway participates in the regulation of cell proliferation and apoptosis, tissue repair and other processes (20). Such pathway mainly includes MST, MOB, LATS and other signalling molecules. As a key transcription factor of this pathway, MST1 plays an important role in promoting cell apoptosis and proliferation (21,22). Activated MST may enter the cell nucleus to promote apoptosis, inhibit cell growth and proliferation and associate with the phosphorylation of FOXO. LATS may be activated by the phosphorylation of MST, enter its own phosphorylation cycle and become activated continuously. MST and LATS can also interact with each other to create a positive feedback circuit and thus promote the pro-apoptotic effect. Some studies have shown that MST1 overexpression may promote myocardial apoptosis and that the inhibition of MTS1 expression may improve apoptosis as well as myocardial remodelling and cardiac dysfunction caused by destructive stimuli, such as apoptosis and ischaemia-reperfusion injury (23–26). The latest research shows that the abnormal activation of MST1 is closely associated with the occurrence mechanism of diabetes and that it participates in the occurrence of myocardial fibrosis (27,28). In the current research, we found obvious myocardial fibrosis in the diabetic rats and a remarkably upregulated expression of the Hippo-MST pathway-associated proteins. Such finding suggests the possible participation of the Hippo-MST pathway in the occurrence of myocardial fibrosis in the diabetic rats. MST1/2 may phosphorylate the core members of Hippo signalling, namely, Sav1, LATS1/2 and MOB1. Therefore, the upregulation of MST1/2 may promote apoptosis. In the present research, we found that the expressions of MST1/2 and its downstream pathway proteins MOB and LATS were obviously upregulated. The expressions of MST1/2 and its downstream pathway proteins MOB and LATS may participate in apoptosis regulation under oxidative stress and ERS in diabetics. Hence, the Hippo-MST signalling pathway maintains the balance between tissue injury and repair and participates in the occurrence mechanism of diabetic myocardial fibrosis by regulating cell apoptosis and maintaining proliferation.
After the discovery of NO, CO and H2S in recent years, some studies have shown that SO2 may be a novel gaseous signalling molecule (29). As the research on sulfurous gases continue, an endogenous SO2-generating system has been found in the cardiovascular system. Sulfur-containing amino acids may generate H2S and SO2 via in vivo metabolism (30,31). Thus far, H2S is known to exhibit a myocardial protective effect in the presence of oxidative stress and hypoxic-ischaemic injury and improve myocardial fibrosis. Both H2S and SO2 are metabolites of sulfur-containing amino acids, and their pathological actions closely correlated with each other. Recent studies have found that SO2 improved the ISO-induced myocardial apoptosis of the rats (32). Some studies have shown that SO2 gas performs many biological functions, such as vasodilation, improvement of vascular and collagen remodelling; it also inhibits inflammation and autoxidation and exerts an important protective effect on vascular diseases (33–36), such as pulmonary arterial hypertension, myocardial ischaemia-reperfusion injury, myocardial hypertrophy, spontaneous hypertension and acute lung injury (37–40). However, the role of SO2 in diabetic myocardial fibrosis and the relevant regulatory mechanism have not been studied yet. The result of the present research indicated that after the intervention with SO2 donor, collagen deposition was obviously decreased in the myocardial interstitium of the diabetic rats and that the dysregulation of MMPs/TIMPs obviously improved, thus suggesting that exogenous SO2 could improve the myocardial fibrosis of diabetic rats. The ERS level in the myocardial tissue of the diabetic rats obviously decreased after the intervention with SO2. The result showed that the expressions of ERS-associated proteins CHOP, GRP94, eIF2α, BIP, PDI and ER01-L were obviously downregulated. Furthermore, after the intervention with SO2, cell apoptosis obviously decreased in the myocardial cells of the diabetic rats. At the same time, the expressions of the pro-apoptotic proteins caspase-3 and caspase-9 were obviously downregulated, and the expression of the anti-apoptotic protein Bcl-2 was obviously upregulated. Such findings indicate that exogenous SO2 can improve ERS and inhibit cell apoptosis, which may be associated with its role in improving myocardial fibrosis.
Existing studies have found that the role of SO2 in inhibiting cell apoptosis may be correlated with its mechanism of regulating the Hippo-MST signalling pathway. The expressions of the Hippo-MST signalling pathway proteins (MST1, Sav1, LATS1 and MOB1) in the myocardial tissues of the rats in the SO2 intervention group were obviously downregulated in comparison with those in the diabetic group. Hence, exogenous SO2 may inhibit the Hippo-MST signalling pathway to reduce ERS and cell apoptosis as well as the resulting diabetic myocardial fibrosis. On the contrary, after the intervention with the SO2-generating enzyme inhibitor HDX, the myocardial fibrosis of the diabetic rats became severe in Masson staining, but he myocardial ultrastructural changes in the HDX group were similar to those in the STZ group, It is likely to have some factors that was difficult to control, because we can not make sure the myocardial tissues were obtained from the identical parts in the heart and there may be some differences between Masson staining and TEM in the steps of making myocardium specimens, we need to evaluate the difference of myocardial fibrosis between STZ group and HDX group in multiple aspects. For example, compared with STZ group, the expression levels of MMP9, MMP24 and TIMP1 were obviously increased and the cardiac function was even worse in HDX group, these results remind us that the myocardial fibrosis may become severe in HDX group, thus suggesting that endogenous SO2 may take part in the regulatory mechanism of myocardial fibrosis in diabetic rats. Unlike that in the diabetics group, the intervention with HDX led to no statistically significant changes in the Hippo-MST signalling pathway, ERS and apoptosis in the myocardial tissues of the diabetic rats. Hence, the aforementioned changes in diabetic myocardial tissue may be related to the downregulated generation of endogenous SO2 and its signal regulation.
In the present research, the downregulated generation of endogenous SO2 wasobserved in DC. This result corresponded to the compensatory upregulation of the expression of the endogenous SO2-generating enzyme GOT1, thereby suggesting that the insufficient endogenous generation of the gaseous signalling molecule SO2 may contribute to the occurrence mechanism of myocardial interstitial fibrosis in diabetic rats and that the internal mechanism by which SO2 improves myocardial fibrosis may be associated with its inhibition of the Hippo-MST signalling pathway to improve cell apoptosis and ERS. The above results would provide new evidence for the further discussion on the occurrence mechanism of DC and offer a new target for the treatment and prevention of diabetic myocardial fibrosis. However, the specific molecular mechanism by which endogenous SO2 regulates the Hippo-MST signalling pathway and improves cell fate still need further discussion because of the limitations of present data, We planed to do further research about the specific molecular mechanism by which endogenous SO2 regulates the Hippo-MST signalling pathway and improves cell fate on the basis of present results in the next research, such as adding the SO2 treatment group on normal rats and MST inhibitor treatment group on STZ-induced diabetic rats and useing cell culture to explore the role of Hippo-MST signalling pathway in high glucose-induced cardiomyocyte injury and whether SO2 protects cardiomyocytes against high glucose-induced injury by Hippo-MST signalling pathway by. In order to discuss the specific relation among ERS, apoptosis and Hippo-MST signalling pathway, it is important to conduct enzymatic activity assays and reporter gene assays. Meanwhile, we intended to use Mst1-knockout mice to investigate Mst1-knockout whether can alleviate the myocardial fibrosis in DC. We hope the further research to make more contributions to the treatment of DC.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant no. 81202830) and the Natural Science Foundation of Hunan Province, China (grant no. 2017JJ3271).
Glossary
Abbreviations
- SO2
sulfur dioxide
- ERS
endoplasmic reticulum stress
- HDX
L-Aspartic acid β-hydroxamate
- TEM
transmission electron microscopy
- DC
diabetic cardiomyopathy
- DM
diabetic mellitus
- H2S
hydrogen sulfide
- MMP
matrix metalloproteinase
- TIMP
tissue inhibitor of metalloproteinase
- LVEDD
left ventricular end-diastolic dimension
- LVESD
left ventricular end-systolic diameter
- EF
ejection fraction
- FS
fractional shortening
References
- 1.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 2.Jia G, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat Rev Endocrinol. 2016;12:144–153. doi: 10.1038/nrendo.2015.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mizushige K, Yao L, Noma T, Kiyomoto H, Yu Y, Hosomi N, Ohmori K, Matsuo H. Alteration in left ventricular diastolic filling and accumulation of myocardial collagen at insulin-resistant prediabetic stage of a type II diabetic rat model. Circulation. 2000;101:899–907. doi: 10.1161/01.CIR.101.8.899. [DOI] [PubMed] [Google Scholar]
- 4.Varga ZV, Giricz Z, Liaudet L, Haskó G, Ferdinandy P, Pacher P. Interplay of oxidative, nitrosative/nitrative stress, inflammation, cell death and autophagy in diabetic cardiomyopathy. Biochim Biophys Acta. 2015;1852:232–242. doi: 10.1016/j.bbadis.2014.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang JS, Hou YL, Lu WW, Ni XQ, Lin F, Yu YR, Tang CS, Qi YF. Intermedin1-53 protects against myocardial fibrosis by inhibiting endoplasmic reticulum stress and inflammation induced by homocysteine in apolipoprotein E-deficient mice. J AtherosclerThromb. 2016;23:1294–1306. doi: 10.5551/jat.34082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li F, Luo J, Wu Z, Xiao T, Zeng O, Li L, Li Y, Yang J. Hydrogen sulfide exhibits cardioprotective effects by decreasing endoplasmic reticulum stressin a diabetic cardiomyopathy rat model. Mol Med Rep. 2016;14:865–873. doi: 10.3892/mmr.2016.5289. [DOI] [PubMed] [Google Scholar]
- 7.Bugger H, Abel ED. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia. 2014;57:660–671. doi: 10.1007/s00125-014-3171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nerheim P, Krishnan SC, Olshansky B. Apoptosis in the genesis of cardiac rhythm disorders. Cardiology clinics. 2001;19:155–163. doi: 10.1016/S0733-8651(05)70201-0. [DOI] [PubMed] [Google Scholar]
- 9.Huang Y, Tang C, Du J, Jin H. Endogenous sulfur dioxide: A new member of gasotransmitter family in the cardiovascular system. Oxid Med Cell Longev. 2016;2016:8961951. doi: 10.1155/2016/8961951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan D. The hippo signaling pathway in development and cancer. Dev Cell. 2010;19:491–505. doi: 10.1016/j.devcel.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Radu M, Chernoff J. The DeMSTification of mammalian Ste20 kinases. Curr Bio. 2009;19:R421–R425. doi: 10.1016/j.cub.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 12.Lin J, Zhang L, Zhang M, Hu J, Wang T, Duan Y, Man W, Wu B, Feng J, Sun L, et al. Mst1 inhibits CMECs autophagy and participates in the development of diabetic coronary microvascular dysfunction. Sci Rep. 2016;6:34199. doi: 10.1038/srep34199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Y, Du J, Zhao YT, Zhang L, Lv G, Zhuang S, Qin G, Zhao TC. Histone deacetylase (HDAC) inhibition improves myocardial function and prevents cardiac remodeling in diabetic mice. Cardiovasc Diabetol. 2015;14:99. doi: 10.1186/s12933-015-0262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Ding WY, Wang ZH, Tang MX, Wang F, Li Y, Zhong M, Zhang Y, Zhang W. Erratum to: Early administration of trimetazidine attenuates diabetic cardiomyopathy in rats by alleviating fibrosis, reducing apoptosis and enhancing autophagy. J Transl Med. 2016;14:309. doi: 10.1186/s12967-016-0849-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang B, Shen Q, Chen Y, Pan R, Kuang S, Liu G, Sun G, Sun X. Myricitrin alleviates oxidative stress-induced inflammation and apoptosis and protects mice against diabetic cardiomyopathy. Sci Rep. 2017;7:44239. doi: 10.1038/srep44239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu W, Zha W, Guo S, Cheng H, Wu J, Liu C. Flos puerariae extract prevents myocardial apoptosis via attenuation oxidative stress in streptozotocin-induced diabetic mice. PLoS One. 2014;9:e98044. doi: 10.1371/journal.pone.0098044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou W, Yang J, Zhang DI, Li F, Li G, Gu Y, Luo M. Role of Bcl-2/adenovirus E1B 19 kDa-interacting protein 3 in myocardial cells in diabetes. Exp Ther Med. 2015;10:67–73. doi: 10.3892/etm.2015.2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biden TJ, Boslem E, Chu KY, Sue N. Lipotoxic endoplasmic reticulum stress, β cell failure and type 2 diabetes mellitus. Trends Endocrinol Metab. 2014;25:389–398. doi: 10.1016/j.tem.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Tang C, Koulajian K, Schuiki I, Zhang L, Desai T, Ivovic A, Wang P, Robson-Doucette C, Wheeler MB, Minassian B, et al. Glucose-induced beta cell dysfunction in vivo in rats: Link between oxidative stress and endoplasmic reticulum stress. Diabetologia. 2012;55:1366–1379. doi: 10.1007/s00125-012-2474-8. [DOI] [PubMed] [Google Scholar]
- 20.Avruch J, Zhou D, Fitamant J, Bardeesy N, Mou F, Barrufet LR. Protein kinases of the Hippo pathway: Regulation and substrates. Semin Cell Dev Biol. 2012;23:770–784. doi: 10.1016/j.semcdb.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meng Z, Moroishi T, Guan KL. Mechanisms of Hippo pathway regulation. Genes Dev. 2016;30:1–17. doi: 10.1101/gad.274027.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Praskova M, Xia F, Avruch J. MOBKL1A/MOBKL1B phosphorylation by MST1 and MST2 inhibits cell proliferation. Curr Biol. 2008;18:311–321. doi: 10.1016/j.cub.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakamura M, Zhai P, Del Re DP, Maejima Y, Sadoshima J. Mst1-mediated phosphorylation of Bcl-xL is required for myocardial reperfusion injury. JCI Insight. 2016;1:e86217. doi: 10.1172/jci.insight.86217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee GJ, Yan L, Vatner DE, Vatner SF. Mst1 inhibition rescues β1-adrenergic cardiomyopathy by reducing myocyte necrosis and non-myocyte apoptosis ratherthan myocyte apoptosis. Basic Res Cardiol. 2015;110:7. doi: 10.1007/s00395-015-0461-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu J, Man W, Shen M, Zhang M, Lin J, Wang T, Duan Y, Li C, Zhang R, Gao E, et al. Luteolin alleviates post-infarction cardiac dysfunction by up-regulating autophagy through Mst1 inhibition. J Cell Mol Med. 2016;20:147–156. doi: 10.1111/jcmm.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamamoto S, Yang G, Zablocki D, Liu J, Hong C, Kim SJ, Soler S, Odashima M, Thaisz J, Yehia G, et al. Activation of Mst1 causes dilated cardiomyopathy by stimulating apoptosis without compensatory ventricular myocyte hypertrophy. J Clin Invest. 2003;111:1463–1474. doi: 10.1172/JCI17459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang M, Zhang L, Hu J, Lin J, Wang T, Duan Y, Man W, Feng J, Sun L, Jia H, et al. MST1 coordinately regulates autophagy and apoptosis in in mice. Diabetologia. 2016;59:2435–2447. doi: 10.1007/s00125-016-4070-9. [DOI] [PubMed] [Google Scholar]
- 28.Ardestani A, Maedler K. MST1: A promising therapeutic target to restore functional beta cell mass in diabetes. Diabetologia. 2016;59:1843–1849. doi: 10.1007/s00125-016-3892-9. [DOI] [PubMed] [Google Scholar]
- 29.Shen Y, Shen Z, Luo S, Guo W, Zhu YZ. The cardioprotective effects of hydrogen sulfide in heart diseases: From molecular mechanisms to therapeutic potential. Oxid Med Cell Longev. 2015;2015:925167. doi: 10.1155/2015/925167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stipanuk MH. Sulfur amino acid metabolism: Pathways for production and removal of homocysteine and cysteine. Annu Rev Nutr. 2004;24:539–577. doi: 10.1146/annurev.nutr.24.012003.132418. [DOI] [PubMed] [Google Scholar]
- 31.Singer TP, Kearney EB. Intermediary metabolism of L-cysteinesulfinic acid in animal tissues. Arch Biochem Biophys. 1956;61:397–409. doi: 10.1016/0003-9861(56)90363-0. [DOI] [PubMed] [Google Scholar]
- 32.Jin H, Liu AD, Holmberg L, Zhao M, Chen S, Yang J, Sun Y, Chen S, Tang C, Du J. The role of sulfur dioxide in the regulation of mitochondrion-related cardiomyocyte apoptosis in ratswith isopropylarterenol-induced myocardial injury. Int J Mol Sci. 2013;14:10465–10482. doi: 10.3390/ijms140510465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang Y, Shen Z, Chen Q, Huang P, Zhang H, Du S, Geng B, Zhang C, Li K, Tang C, et al. Endogenous sulfur dioxide alleviates collagen remodeling via inhibiting TGF-β/Smad pathway invascular smooth muscle cells. Sci Rep. 2016;6:19503. doi: 10.1038/srep19503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang H, Huang Y, Bu D, Chen S, Tang C, Wang G, Du J, Jin H. Endogenous sulfur dioxide isa novel adipocyte-derived inflammatory inhibitor. Sci Rep. 2016;6:27026. doi: 10.1038/srep27026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu D, Huang Y, Bu D, Liu AD, Holmberg L, Jia Y, Tang C, Du J, Jin H. Sulfur dioxide inhibits vascular smooth muscle cell proliferation via suppressing the Erk/MAP kinasepathway mediated by cAMP/PKA signaling. Cell Death Dis. 2014;5:e1251. doi: 10.1038/cddis.2014.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang XB, Jin HF, Tang CS, Du JB. The biological effect of endogenous sulfur dioxide in the cardiovascular system. Eur J Pharmacol. 2011;670:1–6. doi: 10.1016/j.ejphar.2011.08.031. [DOI] [PubMed] [Google Scholar]
- 37.Huang P, Sun Y, Yang J, Chen S, Liu AD, Holmberg L, Huang X, Tang C, Du J, Jin H. The ERK1/2 signaling pathway is involved in sulfur dioxide preconditioning-induced protection against cardiac dysfunction in isolated perfused rat heart subjected tomyocardial ischemia/reperfusion. Int J Mol Sci. 2013;14:22190–22201. doi: 10.3390/ijms141122190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu W, Liu D, Liang C, Ochs T, Chen S, Chen S, Du S, Tang C, Huang Y, Du J, Jin H. Sulfur dioxide protects against collagen accumulation in pulmonary artery in association with downregulation of the transforming growth factor β1/smad pathway in pulmonary hypertensive rats. J Am Heart Assoc. 2016;5:e003910. doi: 10.1161/JAHA.116.003910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen Q, Zhang L, Chen S, Huang Y, Li K, Yu X, Wu H, Tian X, Zhang C, Tang C, et al. Downregulated endogenous sulfur dioxide/aspartate aminotransferase pathway is involved inangiotensin II-stimulated cardiomyocyte autophagy and myocardial hypertrophy in mice. Int J Cardiol. 2016;225:392–401. doi: 10.1016/j.ijcard.2016.09.111. [DOI] [PubMed] [Google Scholar]
- 40.Liu J, Huang Y, Chen S, Tang C, Jin H, Du J. Role of endogenous sulfur dioxide in regulating vascular structural remodeling in hypertension. Oxid Med Cell Longev. 2016;2016:4529060. doi: 10.1155/2016/4529060. [DOI] [PMC free article] [PubMed] [Google Scholar]