Abstract
Objective
According to the EAU Guidelines, transurethral resection of the prostate (TURP) has so far still been considered as the gold standard for surgical treatment for patients with obstructing clinical benign prostate hyperplasia (BPH). However, its relatively high rate of complications and postoperative recurrence necessitates further modification and innovation on the surgery technique. We reported the patient outcomes with our technique.
Methods
We retrospectively analyzed 52 patients with obstructing clinical BPH who underwent bipolar transurethral enucleation and resection of the prostate (B-TUERP) between March 2015 and September 2015. Pre- and perioperative parameters were obtained from medical charts. Postoperative follow-ups were administrated at 1, 3, 6, 12 and 24 month(s) after surgery, respectively.
Results
All the operations were performed successfully with a mean operative time of 43.1 min and an average tissue removal rate of 74.7%. Qmax was significantly improved immediately after surgery, followed by a continuous improvement throughout the follow-ups. Following a steep decrease in mean prostate specific antigen (PSA) and post void residual (PVR) observed within the first half year after surgery, the serum PSA was then maintained at a constant level of 0.61 ng/mL. Temporary urinary retention was found in four cases (7.7%). Stress urinary incontinence occurred in five patients (9.6%), with the condition resolved in 1–2 weeks without extra treatment. Urethral strictures and bladder neck contractures, as the most commonly observed long-term complications, developed in four patients (7.7%). No recurrence was found during 2 years of follow-ups. An improvement in International Index of Erectile Function (IIEF-5) scores was witnessed in 17 patients preoperatively with normal sexual function during the first 6 months after surgery, and sustained throughout the 24-month period.
Conclusions
Enucleation reflects an improvement on surgical technique in many ways with a need for surgical equipment that can be broadly accessible in clinical practice. Currently, bipolar resection is a commonly employed procedure in clinical settings, and its similarity shared with bipolar enucleation technique warrants a quick learning of B-TUERP by urologists. Based on these findings, we believe that the substitution of TURP by TUERP as the gold standard for prostate endoscopic procedure can be expected in the future.
Keywords: Benign prostatic hyperplasia, TURP, Enucleation, Bipolar, Endoscopic surgery
1. Introduction
Lower urinary tract symptoms (LUTS) represent one of the most common clinical complaints in adult men. LUTS can be classified as storage, voiding, and post-micturition symptoms, and are mostly related to clinical benign prostatic hyperplasia (BPH) [1]. Transurethral resection of the prostate (TURP), so far still regarded as the gold standard for surgical treatment for symptomatic BPH, is characterized by immediate removal of the intravesical obstruction and a long-lasting improvement on the symptoms and voiding parameters.
Disadvantages of classical TURP, such as heating of deeper tissue, nerves or muscle stimulation, as well as possible malfunction of cardiac pacemakers, have been broadly recognized by urologists [2]. Absorption of hypoosmotic irrigation fluid adds to another potential risk for monopolar TURP due to the possibility of causing TUR syndrome [3]. New devices such as the plasmakinetic (PK) system [4] and the transurethral resection in saline (TURis) system [5] invented to overcome these severe complications have shown improved surgical efficiency as compared with conventional TURP, from which patients have benefited a lot as demonstrated by significantly reduced complications, shorter convalescence and satisfactory symptom scores and voiding parameters in the follow-ups.
However, despite of the improvement made for TURP surgical equipment, the principle of this endoscopic surgery and some of the subsequent complications such as the high rate of postoperative recurrence remain unchanged, calling for a substantial innovation on the surgical technique. Under this background, another alternative of TURP, the endoscopic enucleation, was developed in an attempt to overcome these problems.
2. Materials and methods
We retrospectively analyzed 52 patients with symptomatic BPH who underwent bipolar transurethral enucleation and resection of the prostate (B-TUERP) between March 2015 and September 2015 in our institution. All operations were performed by a single surgeon (C. Liu). All patients were evaluated preoperatively by physical examination, digital rectal examination and prostate specific antigen (PSA) measurement. The inclusion criteria for operation were established as patients aging from 50 to 80 years old who were diagnosed with clinical BPH, with a PSA level ranging from 0 to 4 ng/mL and a prostate volume from 40 to 160 mL (by transrectal ultrasound: 0.52 × longitudinal diameter × transversal diameter × vertical diameter). All included patients were identified having at least one of the following conditions: 1) International Prostate Symptom Score (IPSS) ≥12, and the quality of life (QoL) ≥4; 2) Qmax ≤15mL/s (voided volume ≥150 mL); 3) Poor response to drug treatment; 4) Recurrent urinary retention; and 5) The Schafer grade ≥2 [6].
Patients with neurogenic bladder, history of lower urinary tract surgery, urethral stricture or prostate/bladder cancer were excluded. Poor general condition of the patient also was classified as one of the exclusion criteria. As for those with an elevated PSA, negative biopsy results before surgery were required for inclusion. The perioperative parameters, including operative time, weight of resected prostatic tissue, catheterization time, and hospital stay, were obtained from medical charts (Table 1). Postoperative follow-ups were carried out at 1, 3, 6, 12 and 24 month(s) after the surgery, respectively, with a thorough record for all the postoperative surgical complications that believed to be associated with the procedure.
Table 1.
Perioperative data of the patients (n = 52) (mean ± SD).
| Characteristic | Value |
|---|---|
| Age, year | 67.9 ± 6.4 |
| PV, mL | 72.4 ± 10.2 |
| PSA, ng/mL | 2.35 ± 0.92 |
| Operation time, min | 43.1 ± 4.0 |
| Enucleation time, min | 39.9 ± 3.9 |
| Enucleation weight, g | 54.2 ± 8.1 |
| Tissue removal rate, % | 74.7 ± 2.6 |
| Decrease in sodium, mmol/L | 0.790 ± 0.380 |
| Postoperative irrigation, h | 18.4 ± 2.4 |
| Duration of catheterization, h | 40.0 ± 6.1 |
| Postoperative hospital stay, h | 66.7 ± 6.3 |
2.1. Surgical procedure
The procedure was performed using the Scanmed Plasmakinetic System (Scanmed, Zhuhai, China) with Plasma electrodes as well as a power of 160 W for the cutting and 80 W for coagulating. As described in our previous reports [7], [8], the enucleation procedure usually started from the prostatic apex, the boundary between the adenoma and external sphincter [9] (Fig. 1, Supplement file 1), rather than the verumontanum which is a mark but not a boundary. Blunt dissection was conducted clockwise and counterclockwise to separate the surgical capsule from the gland via the beak of the resectoscope sheath, and the detachment area was extended laterally and forward to completely peel the adenomatous tissues off the surgical capsule (Fig. 2). Four tricks during the procedure were emphasized by the author, including: be sure to identify the correct plane of surgical capsule; enucleate the gland tissues along the surgical capsule with proficient skills; preserve the physiological curvature of the bladder neck at the 6 o'clock position; and preserve partial of the urethral valve at the 12 o'clock position to avoid sphincter injury (Fig. 3).
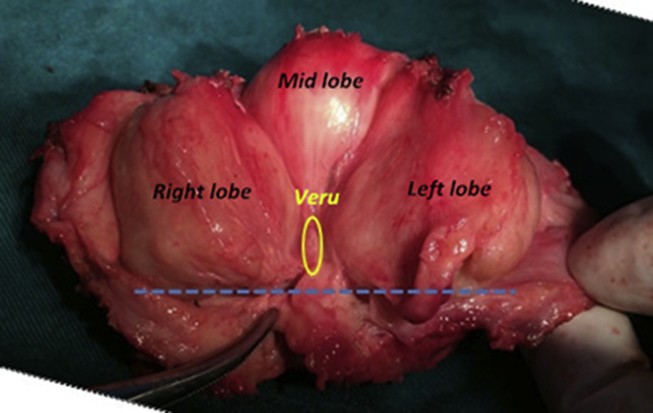
Figure 1.
Boundary of verumontanum and hyperplasia gland. A prostate specimen from a prostate cancer patient which showed that the apical portions of the adenoma were more than 1 cm distal to the verumontanum. The yellow circle represent verumontanum, and the blue dotted line on behalf of distal boundary of hyperplasia gland.
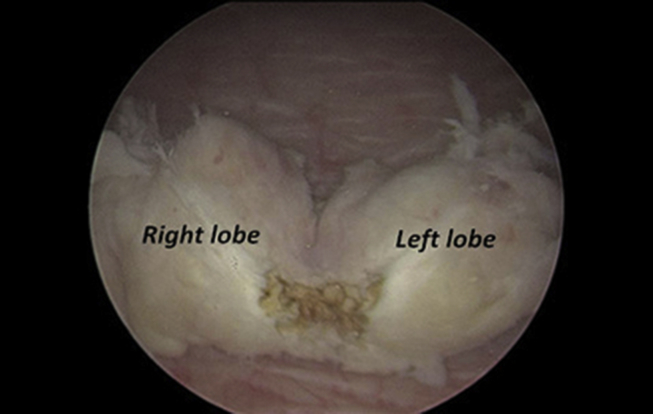
Figure 2.
En bloc gland is peeled off from the surgical capsule and pushed to the bladder which could be treated by morcellator.
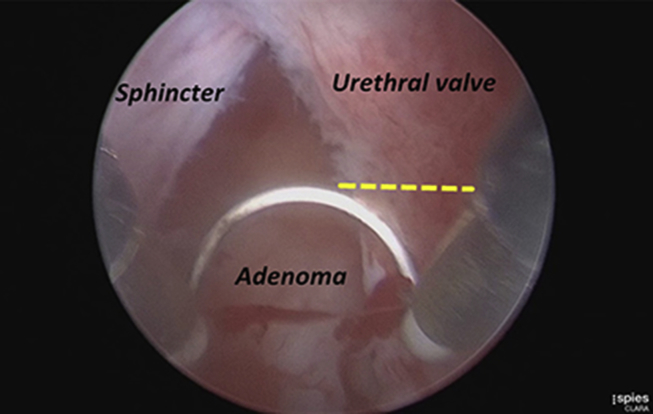
Figure 3.
Treatment of 12 o'clock. Use brief cutting instead of blunt dissection without cutting beyond the yellow line to preserve partial urethral valve at 12 o'clock, that avoiding injury of the sphincter.
Potential intraoperative urethral sphincter injury was examined using “Micturition Experiment” (Supplement file 2) immediately after the surgery by instilling appropriate saline into the bladder to simulate the urinary storage period. The urine coming out under the pressing on the suprapubic area and ceasing when the pressing stopped can lead to a preliminary judgment that the urethral sphincter is undamaged [10], [11], [12].
2.2. Statistical analysis
The data were presented by mean ± SD and analyzed with SPSS, version 19.0 (IBM Corp., Armonk, IL, USA). Mean PSA, Qmax, postvoid residual (PVR), IPSS and QoL score were compared with preoperative values using the paired Student's t-test. Statistical significance was considered at p < 0.05 for all analyses.
3. Results
All the operations were completed successfully, with a mean operative time of 43.1 min, of which the enucleation time accounted for 92.4%. The average tissue removal rate in our group was 74.7% according to the calculation by resected prostatic tissues/prostate volume, much higher as compared to the results in traditional TURP [13]. The duration of catheterization was approximately 40.0 h. A significant improvement was observed in Qmax immediately after the surgery and also during the follow-up period. Mean PSA and PVR showed a steep decrease in the first half year postoperative, while serum PSA maintained at a constant level of 0.61 ng/mL thereafter (Table 2).
Table 2.
Follow-up data.
| Pre | 1 m post | 3 m post | 6 m post | 12 m post | 24 m post | |
|---|---|---|---|---|---|---|
| Qmax (mL/s) | 9.18 ± 2.88 | 21.60 ± 5.32 | 22.90 ± 4.55 | 25.50 ± 4.79 | 27.70 ± 5.01 | 27.50 ± 4.94 |
| PVR (mL)# | 66.30 ± 103.00 | 12.40 ± 8.75 | 9.30 ± 7.24 | 7.10 ± 5.46 | 5.40 ± 4.75 | 5.00 ± 3.34 |
| IPSS | 22.10 ± 3.20 | 7.48 ± 0.66 | 5.83 ± 0.73 | 4.06 ± 0.72 | 2.23 ± 0.70 | 1.83 ± 0.64 |
| QoL | 4.69 ± 1.12 | 3.23 ± 0.50 | 2.46 ± 0.63 | 1.85 ± 0.63 | 1.50 ± 0.57 | 0.62 ± 0.59 |
| PSA (ng/mL) | 2.35 ± 0.92 | – | 0.76 ± 0.53 | – | 0.64 ± 0.38 | 0.61 ± 0.48 |
| IIEF-5 (n = 17) | 19.80 ± 0.94 | – | – | 20.30 ± 1.03 | 20.10 ± 0.67* | 21.00 ± 0.76** |
∗n = 11, **n = 7.
#Postvoid residual of uroschesis patients is calculated according to bladder capacity.
Pathological examination revealed BPH in 49 cases and prostatic intraepithelial neoplasia (PIN) in three cases. No severe complications were observed in any of the patients. Other events included a need for postoperative blood transfusion for one patient (1.9%), temporary urinary retention in four patients (7.7%) due to removal of the catheter as early as at 6 h after the surgery, transient urinary incontinence occurred in five cases (9.6%) with the condition resolved within 1–2 weeks without further treatment, as well as retrograde ejaculation that was found in 20 patients. As for long-term complications, urethral strictures and bladder neck contractures, as the most common adverse events, were noticed in four patients (7.7%). These cases were managed successfully by routine urethral dilation or laser internal urethrotomy, with no recurrence during the 2-year follow-ups.
An improvement in IIEF-5 scores was seen in 17 patients preoperatively with normal sexual function during the first 6 months and throughout the 24-month period after the operation (Table 2).
4. Discussion
In 1989, Hiraoka and Akimoto [14] first proposed the concept of transurethral enucleation for benign prostatic adenomatous hyperplasia, which was conducted with a detaching blade mimicking the index finger at open prostatectomy, and therefore minimized the potential risk of capsular perforation compared to standard TURP.
Later on, Gilling et al. [15] pioneered holmium laser nucleation of the prostate (HoLEP), and made this technique widely recognized as an effective and safe procedure for clinical BPH of any size [16]. The improvement in clinical outcomes gained by HoLEP was durable, accompanied by a low complication and reoperation rate [17]. The subsequent introduction of bipolar plasmakinetic energy into the same endoscopic enucleation procedure by this team [18] further demonstrated that plasmakinetic enucleation was also a safe and technically feasible alternative for enucleation of prostatic adenomata.
In 2003, Liu et al. [19] performed a totally retrograde B-TUERP, which, although shares some similarities with HoLEP, also presents differences besides the equipment employed in the procedure, specifically in the following aspects: Gilling started enucleation from bladder neck while Liu preferred prostate apex as the starting point; Gilling used laser energy for exploration through the adenoma to find the surgical capsule, in contrast to blunt dissection employed by Liu; and Liu would like to use the beak of resectoscope sheath for enucleation, instead of the radio frequency that played a critical role in Gilling's surgeries. However, since the two procedures were based on the same principles, the outcomes were found to be similarly satisfying [7], [17]. Laser enucleation is thought to be superior in terms of less potential risk of hemorrhage, reduced bladder irrigation and catheterization time. In contrast, bipolar enucleation has its own advantage in that the equipment is easily accessible and highly cost-efficient [8], [20], [21]. In general, the two procedures are believed to be in the similar position considering their aims of a high efficiency in removing the prostate adenomatous tissues as well as relieving the obstruction and lower urinary tract symptoms.
4.1. Enucleation and efficacy
Voiding dysfunction associated with clinical BPH adversely affects patients' QoL and could significantly interfere with their daily activities [1]. Meanwhile, storage symptoms are also troubling for patients with BPH. The recovery of detrusor function after a surgical procedure for clinical BPH may be influenced by the degree of de-obstruction [22]. TURP is often not extended down to the fibre of the capsule for fear of capsular perforation and severe venous bleeding, therefore amass of adenoma tissues remains after TURP, usually leading to a high postoperative recurrence rate [9]. In this study, 74.7% tissue was removed after enucleation, which is much higher than that in traditional TURP, and contributes to a significant improvement in postoperative IPSS, QoL and Qmax.
4.2. Enucleation and PSA
The raised PSA level seen in clinical BPH is related to the size of the adenoma in the transitional zone. Hence, a dramatic decrease in the PSA level should be observed in cases with complete resection of the adenoma [23], which has been proven by a randomized trial with a similar reduction of the PSA level and postoperative prostate volume in the enucleation group as compared to the open surgery group during 1-year follow-ups [24].
According to Palaniappan et al. [25], the enucleation group possessed a significantly lower postoperative PSA level than the TURP group (1.2 ng/mL vs. 1.9 ng/mL, p = 0.01), accompanied by a more remarkable reduction in the mean PSA level (88.8% vs. 71.6%). These findings, together with the similar results reported by other studies, suggest that a lower PSA level and higher peak urinary flow may be considered as the surrogate markers of a more complete adenoma removal [24], [26], [27], [28].
In addition, long-term follow-up data indicate that the patients who received TUERP in the authors' institution mostly had a stable PSA level ranging from 0.41 to 1.08, and a hypothesis currently under study also suggests that an abnormal increase of the PSA level should arouse vigilance for the potential risk of prostate cancer in the residual prostate gland. Therefore, PSA level after prostate enucleation is considered not only an indicator of the completeness of adenoma removal, but also a tool for early warning of prostate cancer if a continued elevation is observed.
4.3. Enucleation and complications
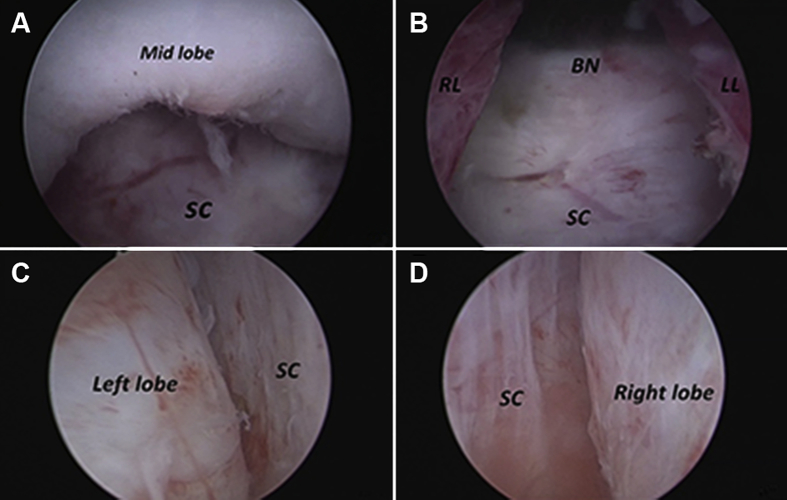
Capsular perforation or undermining of the bladder neck that was reported in 8% of patients undergoing endoscopic resection with bipolar energy [13] did not occur in this study, which was believed to be associated with the selected procedure by which the enucleation was performed along the natural plane between the gland and surgical capsule (Fig. 4C and 4D). The vascular network running on the inner surface of the surgical capsule and its perforating vessels given out to the prostatic adenoma (Fig. 4) [7], [8] make hemostasis an easy work under endoscopic monitoring. Meanwhile, precisely positioned surgical plane is beneficial for preserving the physiological gradient of the bladder neck, and therefore will contribute to uncompromised postoperative sexual and urinary functions (Fig. 4B).
Figure 4.
Enucleation based on the surgical capsule. (A) Enucleation of the middle lobe; (B) Preserving the physiological gradient of the bladder neck (after enucleation of the middle lobe); (C) Enucleation of the left lobe; (D) Enucleation of the right lobe; SC, surgical capsule; BN, bladder neck; RL, right lobe; LL, left lobe.
Temporary urinary retention was noted in 7.7%, and transient urinary incontinence, which was correlated to a variety of factors such as urinary tract infection and overactive bladder, was found in 9.4% of the patients within 1 month after surgery. These postoperative complications were resolved without receiving extra treatment, with most cases recovered from temporary incontinence or urge incontinence within 3 months. Bladder neck contracture and urethral stricture, occurred at the similar rate (7.7%) with endoscopic resection, were managed by routine urethral dilation and/or urethrotomy.
4.4. Enucleation and sexual function
Sexual function after prostate operation is also related to some local factors including intraoperative blood loss and thermal damage [29] in addition to age, general condition, and psychological state of the patients.
Analysis of the available data has revealed that TURP has no adverse effect on sexual function in patients receiving the surgery, and a 12-year follow-up study by Mishriki et al. [30] even demonstrated a long-lasting improvement on the pre-operative erectile dysfunction by TURP. Similar results were also obtained by Capogrosso et al. [31] in patients undergoing enucleation procedure.
According to current data, TURP showed no statistically significant difference in the recovery of sexual function after surgery as compared with enucleation. Moreover, the sexual satisfaction was found to be positively correlated with the improvement of LUTS [32].
Retrograde ejaculation has been recognized worldwide with a high incidence of up to 50% in patients after TURP, and speculated as a potential cause for sexual dysfunction given its adverse effects both psychologically and physiologically on the patients. In this regard, many scholars believe that theoretically, enucleation may result in more severe adverse effects associated with sexual functions, as the glandular tissues are removed more completely in enucleation than in resection (TURP). However, the authors argue to the contrary for the following reasons:
-
(i)
Enucleation maximally decreases the strain of surgical capsule and releases the mechanical pressure of the hypertrophic gland on the erectile nerves, leading to an improvement in the hemodynamic parameters of erectile function, which is conducive to the postoperative recovery of sexual function in elderly men.
-
(ii)
Enucleation along the surgical capsule plane allows a decrease in postoperative incidence of retrograde ejaculation by providing a better preservation of the physiological structure of intravesical sphincter and prostatic fossa, and hence can better preserve the erectile function [33].
So far, meta-analysis is not thought suitable for sexual dysfunction evaluation due to lack of reliable data, while there are no data showing statistical differences in the interference with sexual function between enucleation and traditional TURP. More rigorous-designed trials with extended follow-ups and larger sample size are needed to draw final conclusions about these two procedures.
From the technical point of view, enucleation with bipolar energy shares the same principles with HoLEP, which offers an alternative energy platform for surgeons and allows a wiser option based on the conditions of the patients as well as the centers. Most urologists are familiar with the commonly used bipolar resection, so shortening of the learning curves for TUERP using the same equipment can be expectable. In addition, the bipolar system, as a rather cost effective equipment, can be employed in many developing countries in Asia and other regions.
Limitations in our study mainly reside in the nature of the retrospective research, the data collection from a single center, as well as the small size of the sampling, which necessitate more multi-centre RCTs with larger sample size, precise stratification based on patient characteristics, and longer follow-ups.
5. Conclusion
Enucleation epitomizes an improvement of surgical technique in which this procedure is based on the same principle regardless of the devices used for the surgery, and can be widely conducted due to the easy accessibility to the surgery equipment. More importantly, enucleation procedures can remove the obstructing adenoma more completely, enabling better long-term clinical outcomes. B-TUERP has been proven to be more cost-effective than laser enucleation, and makes the urologists quick learners as it uses currently available instrument that the surgeons have already been familiar with. These findings support the hypothesis that TUERP eventually will supersede TURP as the gold standard for prostate endoscopic procedure.
Conflicts of interest
The authors declare that they have no conflict of interest.
Acknowledgements
We thank Drs. Keong Tatt Foo and Herrmann Thomas for development and dissemination of TUERP, and also they provided administrative and technical support for this project.
Footnotes
Peer review under responsibility of Second Military Medical University.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajur.2017.12.001.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Gratzke C., Bachmann A., Descazeaud A., Drake M.J., Madersbacher S., Mamoulakis C. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67:1099–1109. doi: 10.1016/j.eururo.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 2.Wendt-Nordahl G., Hacker A., Reich O., Djavan B., Alken P., Michel M.S. The Vista system: a new bipolar resection device for endourological procedures: comparison with conventional resectoscope. Eur Urol. 2004;46:586–590. doi: 10.1016/j.eururo.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Fayad A.S., Elsheikh M.G., Zakaria T., Elfottoh H.A., Alsergany R., Elshenoufy A. Holmium laser enucleation of the prostate versus bipolar resection of the prostate: a prospective randomized study. “pros and cons”. Urology. 2015;86:1037–1041. doi: 10.1016/j.urology.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Singh H., Desai M.R., Shrivastav P., Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. J Endourol. 2005;19:333–338. doi: 10.1089/end.2005.19.333. [DOI] [PubMed] [Google Scholar]
- 5.Ho H.S., Yip S.K., Lim K.B., Fook S., Foo K.T., Cheng C.W. A prospective randomized study comparing monopolar and bipolar transurethral resection of prostate using transurethral resection in saline (TURIS) system. Eur Urol. 2007;52:517–522. doi: 10.1016/j.eururo.2007.03.038. [DOI] [PubMed] [Google Scholar]
- 6.Eckhardt M.D., van Venrooij G.E., Boon T.A. Urethral resistance factor (URA) versus Schäfer's obstruction grade and Abrams-Griffiths (AG) number in the diagnosis of obstructive benign prostatic hyperplasia. Neurourol Urodyn. 2001;20:175–185. doi: 10.1002/1520-6777(2001)20:2<175::aid-nau20>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 7.Liu C., Zheng S., Li H., Xu K. Transurethral enucleation and resection of prostate in patients with benign prostatic hyperplasia by plasma kinetics. J Urol. 2010;184:2440–2445. doi: 10.1016/j.juro.2010.08.037. [DOI] [PubMed] [Google Scholar]
- 8.Xu A., Zou Y., Li B., Liu C., Zheng S., Li H. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol. 2013;27:1254–1260. doi: 10.1089/end.2013.0107. [DOI] [PubMed] [Google Scholar]
- 9.Shimizu Y., Hiraoka Y., Iwamoto K., Takahashi H., Abe H., Ogawa H. Is complete resection of hypertrophic adenoma of the prostate possible with TURP? J Nippon Med Sch. 2005;72:146–148. doi: 10.1272/jnms.72.146. [DOI] [PubMed] [Google Scholar]
- 10.Walz J., Graefen M., Huland H. Basic principles of anatomy for optimal surgical treatment of prostate cancer. World J Urol. 2007;25:31–38. doi: 10.1007/s00345-007-0159-6. [DOI] [PubMed] [Google Scholar]
- 11.Walz J., Burnett A.L., Costello A.J., Eastham J.A., Graefen M., Guillonneau B. A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol. 2010;57:179–192. doi: 10.1016/j.eururo.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Walz J., Epstein J.I., Ganzer R., Graefen M., Guazzoni G., Kaouk J. A critical analysis of the current knowledge of surgical anatomy of the prostate related to optimisation of cancer control and preservation of continence and erection in candidates for radical prostatectomy: an update. Eur Urol. 2016;70:301–311. doi: 10.1016/j.eururo.2016.01.026. [DOI] [PubMed] [Google Scholar]
- 13.da Silva R.D., Bidikov L., Michaels W., Gustafson D., Molina W.R., Kim F.J. Bipolar energy in the treatment of benign prostatic hyperplasia: a current systematic review of the literature. Can J Urol. 2015;22(Suppl. 1):30–44. [PubMed] [Google Scholar]
- 14.Hiraoka Y., Akimoto M. Transurethral enucleation of benign prostatic hyperplasia. J Urol. 1989;142:1247–1250. doi: 10.1016/s0022-5347(17)39047-x. [DOI] [PubMed] [Google Scholar]
- 15.Gilling P.J., Kennett K., Das A.K., Thompson D., Fraundorfer M.R. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. 1998;12:457–459. doi: 10.1089/end.1998.12.457. [DOI] [PubMed] [Google Scholar]
- 16.Shah H.N., Sodha H.S., Kharodawala S.J., Khandkar A.A., Hegde S.S., Bansal M.B. Influence of prostate size on the outcome of holmium laser enucleation of the prostate. BJU Int. 2008;101:1536–1541. doi: 10.1111/j.1464-410X.2007.07434.x. [DOI] [PubMed] [Google Scholar]
- 17.Elzayat E.A., Elhilali M.M. Holmium laser enucleation of the prostate (HoLEP): long-term results, reoperation rate, and possible impact of the learning curve. Eur Urol. 2007;52:1465–1471. doi: 10.1016/j.eururo.2007.04.074. [DOI] [PubMed] [Google Scholar]
- 18.Neill M.G., Gilling P.J., Kennett K.M., Frampton C.M., Westenberg A.M., Fraundorfer M.R. Randomized trial comparing holmium laser enucleation of prostate with plasmakinetic enucleation of prostate for treatment of benign prostatic hyperplasia. Urology. 2006;68:1020–1024. doi: 10.1016/j.urology.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 19.Liu C.X., Xu A.B., Zheng S.B., Li H.L. Real endo-enucleation of prostate for treatment of benign prostatic hyperplasia. J Urol. 2006;(Suppl. 17):453. [Google Scholar]
- 20.Chen Y., Xu H., Xu H., Gu M., Zhou J., Cai Z. Comparison of plasmakinetic enucleation of the prostate with holmium laser enucleation of the prostate in the treatment of benign prostate hyperplasia. Int J Clin Exp Med. 2016;9:7328–7333. [Google Scholar]
- 21.Brunckhorst O., Ahmed K., Nehikhare O., Marra G., Challacombe B., Popert R. Evaluation of the learning curve for holmium laser enucleation of the prostate using multiple outcome measures. Urology. 2015;86:824–829. doi: 10.1016/j.urology.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Elkoushy M.A., Elshal A.M., Elhilali M.M. Postoperative lower urinary tract storage symptoms: does prostate enucleation differ from prostate vaporization for treatment of symptomatic benign prostatic hyperplasia? J Endourol. 2015;29:1159–1165. doi: 10.1089/end.2015.0202. [DOI] [PubMed] [Google Scholar]
- 23.Furuya Y., Akakura K., Tobe T., Ichikawa T., Igarashi T., Ito H. Changes in serum prostate-specific antigen following prostatectomy in patients with benign prostate hyperplasia. Int J Urol. 2000;7:447–451. doi: 10.1046/j.1442-2042.2000.00228.x. [DOI] [PubMed] [Google Scholar]
- 24.Geavlete B., Stanescu F., Iacoboaie C., Geavlete P. Bipolar plasma enucleation of the prostate vs open prostatectomy in large benign prostatic hyperplasia cases—a medium term, prospective, randomized comparison. BJU Int. 2013;111:793–803. doi: 10.1111/j.1464-410X.2012.11730.x. [DOI] [PubMed] [Google Scholar]
- 25.Palaniappan S., Kuo T.L., Cheng C.W., Foo K.T. Early outcome of transurethral enucleation and resection of prostate compared with transurethral resection of the prostate. Singap Med J. 2016;57:676–680. doi: 10.11622/smedj.2016026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao Z., Zeng G., Zhong W., Mai Z., Zeng S., Tao X. A prospective, randomised trial comparing plasmakinetic enucleation to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: three-year follow-up results. Eur Urol. 2010;58:752–758. doi: 10.1016/j.eururo.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 27.Zhu L., Chen S., Yang S., Wu M., Ge R., Wu W. Electrosurgical enucleation versus bipolar transurethral resection for prostates larger than 70 ml: a prospective, randomized trial with 5-year followup. J Urol. 2013;189:1427–1431. doi: 10.1016/j.juro.2012.10.117. [DOI] [PubMed] [Google Scholar]
- 28.Geavlete B., Bulai C., Ene C., Checherita I., Geavlete P. Bipolar vaporization, resection, and enucleation versus open prostatectomy: optimal treatment alternatives in large prostate cases? J Endourol. 2015;29:323–331. doi: 10.1089/end.2014.0493. [DOI] [PubMed] [Google Scholar]
- 29.Zong H.T., Peng X.X., Yang C.C., Zhang Y. The impact of transurethral procedures for benign prostate hyperplasia on male sexual function: a meta-analysis. J Androl. 2012;33:427–434. doi: 10.2164/jandrol.111.013490. [DOI] [PubMed] [Google Scholar]
- 30.Mishriki S.F., Grimsley S.J., Lam T., Nabi G., Cohen N.P. TURP and sex: patient and partner prospective 12 years follow-up study. BJU Int. 2012;109:745–750. doi: 10.1111/j.1464-410X.2011.10396.x. [DOI] [PubMed] [Google Scholar]
- 31.Capogrosso P., Ventimiglia E., Ferrari M., Serino A., Boeri L., Capitanio U. Long-term sexual outcomes after holmium laser enucleation of the prostate: which patients could benefit the most? Int J Impot Res. 2016;28:189–193. doi: 10.1038/ijir.2016.29. [DOI] [PubMed] [Google Scholar]
- 32.Kim S.H., Yang H.K., Lee H.E., Paick J.S., Oh S.J. HoLEP does not affect the overall sexual function of BPH patients: a prospective study. Asian J Androl. 2014;16:873–877. doi: 10.4103/1008-682X.132469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu Y.W., Liu C.X., Zheng S.B., Li H.L., Fang P., Chen B.S. Transurethral enucleation of the prostate for treatment of benign prostatic hyperplasia in patients less than 50 years old. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30:2708–2710. [article in Chinese] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.