Abstract
Tattoo popularity continues to rise, with 3 in 10 Americans bearing at least one. Among tattoo complications, non-tuberculous mycobacteria (NTM) has emerged as a global public health concern. NTM infections associated with tattooing of immunocompetent individuals have occurred as sporadic cases and community outbreaks. Water sources are considered the major pathogenic reservoirs. Tattoo-related inoculation has been linked to contamination of ink, either during the manufacturing process or during dilution of black ink using non-sterile water. NTM infections have also been documented in a number of cosmetic and surgical procedures, including cutaneous surgery, Mohs micrographic surgery, mesotherapy, liposuction and laser resurfacing. NTM inoculation through exposure to contaminated water or non-sterile instruments remains a challenge for dermatologists and risk to patients. We reported a case of cutaneous Mycobacterium massiliense infection following tattoo placement. This report underscores the importance of clinicians to consider NTM infections in the differential diagnosis of procedure-related reactions.
Keywords: dermatology, infections, skin, healthcare improvement and patient safety
Background
The prevalence of tattoos in the USA continues to rise, with reportedly 3 in 10 Americans bearing at least one tattoo, and within this inked population, roughly 7 in 10 having two or more tattoos.1 While the Food and Drug Administration (FDA) does have recommendations regarding tattoo safety, the FDA does not practice regulatory authority and leaves tattoo regulations to local jurisdictions. Tattoo inks are considered cosmetics, and as such, the FDA does not explicitly mandate sterility of tattoo inks or practices.2
Among the well-established and diverse list of tattoo-related complications, infections have classically been attributed to Staphylococcus aureus, β-haemolytic streptococci, hepatitis B or HIV.3 Recently, however, cutaneous inoculation of non-tuberculous mycobacteria (NTM) in immunocompetent individuals has emerged as a global public health concern.4
Since the initial report of NTM inoculation from tattooing by Wolf and Wolf in 2003,5 this unique mode of transmission remains infrequently reported despite continued risk to patients. NTM infections have also been well documented in association with a number of cosmetic and surgical procedures performed by dermatologist and dermatological surgeons, including cutaneous surgery, Mohs micrographic surgery, mesotherapy, local injections, liposuction, laser resurfacing and even intraoperative use of contaminated gentian violet skin markers.6 7 Herein, we report a recent case of cutaneous infection with Mycobacterium massiliense following tattoo placement. We aim to underscore the importance of clinicians to consider NTM infections in the differential diagnosis of patients with a tattoo reaction, or any procedure-related reaction.
Case presentation
An otherwise healthy 37-year-old man presented with an erythematous, papular rash of 1 month duration, localised within new tattoos that had been placed 2 weeks prior to the eruption. He denied a history of similar rash with prior tattoos. He was previously treated by an outside dermatologist with a course of Levaquin and oral prednisone without any improvement.
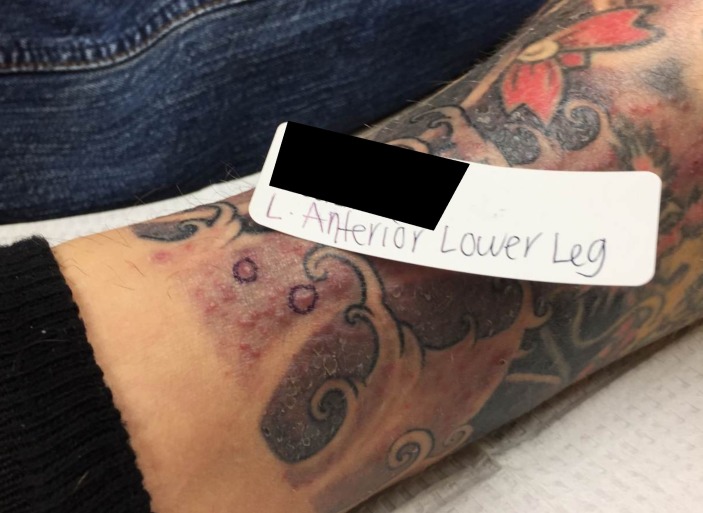
Physical examination revealed focal areas of numerous monomorphic, erythematous, crusted papules scattered within tattoo ink on his left lower leg and bilateral forearms. Lesions were confined to areas of grey ink. There was no local induration or regional lymphadenopathy; he was afebrile and otherwise well appearing. The patient was empirically started on minocycline 100 mg two times per day, though returned 2 weeks later with lesional spread and progressive development of pustules (figure 1).
Figure 1.
Pinpoint pink papules on anterior left lower leg along grey ink tattoo lines.
Outcome and follow-up
Two 4 mm punch biopsies were obtained, and histopathological examination revealed suppurative, granulomatous inflammation. Results from routine culture, periodic acid-Schiff stain, Gram stain and acid-fast bacilli (AFB) smear were negative for microorganisms. AFB culture grew Mycobacterium abscessus and additional speciation testing identified M. massiliense. Susceptibility testing revealed resistance to tetracyclines and sensitivity to oral agents limited only to macrolides. He was seen in consultation with infectious disease specialists and started on monotherapy with azithromycin 500 mg daily. After 3 months of treatment, lesions had completely resolved.
Discussion
NTM skin infections associated with tattooing have occurred as both sporadic cases and large community outbreaks.2 4 6 NTM are ubiquitous in the environment, with infected water sources considered major pathogenic reservoirs.6 Tattoo-related inoculation has primarily been linked to contamination of tattoo ink, either during the manufacturing process (using contaminated ingredients) or more commonly, when artists use non-sterile water to dilute black ink to grey.2 Ink dilution also dilutes preservatives within the product, thereby reducing their efficacy and enhancing contamination. As in our case, a substantial number of the previously reported cases of tattoo associated NTM infections similarly noted lesional localisation to grey tattoo pigment. Inoculation has also resulted from artists using non-sterile water to rinse tattoo needles between colours.2
Diagnosis of atypical mycobacterial infection should be suspected on a clinical basis in any patient with a tattoo reaction, characterised by an acute eruption of papules or pustules within 1–4 weeks following tattoo placement. Itching and pain are common.4 Variability in clinical presentation and lesional morphology contribute to delayed diagnosis and treatment. Punch biopsies should be obtained for histopathological evaluation and AFB culture, though negative culture does not exclude this diagnosis as only 40%–60% of reported cases yielded positive cultures.8
Several species of NTM can cause atypical mycobacterial infections, with rapidly growing mycobacterium (RGM) species (M. abscessus, M. chelonae and M. fortuitum) accounting for the majority of skin and soft tissue infections, including tattoo-related infections.4 6 Progressive advances in differentiating subspecies has enabled M. abscessus to be further divided into three subspecies (massiliense, abscessus and bolletii). It is now understood that sub speciation has profound clinical and prognostic utility. Distinction is based on erm(41) gene patterns, resulting in subsp. abscessus having intrinsic resistance to macrolide antibiotics. Contrastingly, subsp. massiliense, as cultured from our patient, does not have inducible resistance and can effectively be treated with macrolides.9 In addition to antimicrobial resistance associated with subsp. abscessus, it is also resistant to disinfectants, thereby increasing pathogenesis in nosocomial, surgical and postprocedural infections.9
The optimal antibiotic regimen and duration of treatment for cutaneous NTM infections have not yet been established. Current guidelines recommend treatment should be species dependent and guided by susceptibility testing.6 Given the significant difference in therapeutic response and treatment outcomes between subspecies, we recommend cultures growing M. abscessus undergo additional sub speciation testing. In the treatment of RGM species, many favour the use of at least two antibiotics continued for an average of 4–6 months.10 In our patient, however, the infectious disease specialists recommended discontinuation of treatment after 3 months, once complete resolution of all cutaneous lesions was observed and maintained. Adjuvant surgical therapy may be considered in localised infections. More severe cases may require use of parenteral antibiotics initially, followed by oral therapy for 6–12 months.10
Learning points.
Non-tuberculous mycobacteria inoculation by exposure to contaminated water or non-sterile instruments in the setting of tattooing has emerged as a global health concern.
Transmission can also occur iatrogenically in the clinic setting, in association with a number of cosmetic and surgical procedures performed by dermatologists.
These infections remain a major diagnostic and therapeutic challenge for clinicians, as well as a significant ongoing health hazard to patients.
Furthermore, specific speciation should be pursued to optimise targeted antibiotic treatment, decrease resistance and hasten recovery.
Footnotes
Contributors: SA and SW c, reporting and assessment of the patient and the value of their situation. LV and JH researched and wrote the manuscript. SW and SA edited and completed the final manuscript.
Disclaimer: All authors have no relevant financial interest in this manuscript and no activities, affiliations, or relationships to disclose. This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other peer-reviewed media.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Haris Interactive: Harris Polls Tattoo Takeover. Three in ten Americans have tattoos, and most don’t stop at just one. http://www.theharrispoll.com/health-and-life/Tattoo_Takeover.html (accessed 10 Feb 2017).
- 2.Centers for Disease Control and Prevention (CDC). Tattoo-associated nontuberculous mycobacterial skin infections--multiple states, 2011-2012. MMWR Morb Mortal Wkly Rep 2012;61:653–6. [PubMed] [Google Scholar]
- 3.Sergeant A, Conaglen P, Laurenson IF, et al. Mycobacterium chelonae infection: a complication of tattooing. Clin Exp Dermatol 2013;38:140–2. 10.1111/j.1365-2230.2012.04421.x [DOI] [PubMed] [Google Scholar]
- 4.Falsey RR, Kinzer MH, Hurst S, et al. Cutaneous inoculation of nontuberculous mycobacteria during professional tattooing: a case series and epidemiologic study. Clin Infect Dis 2013;57:e143–e147. 10.1093/cid/cit347 [DOI] [PubMed] [Google Scholar]
- 5.Wolf R, Wolf D. A tattooed butterfly as a vector of atypical mycobacteria. J Am Acad Dermatol 2003;48:S73–4. 10.1067/mjd.2003.166 [DOI] [PubMed] [Google Scholar]
- 6.Drage LA, Ecker PM, Orenstein R, et al. An outbreak of Mycobacterium chelonae infections in tattoos. J Am Acad Dermatol 2010;62:501–6. 10.1016/j.jaad.2009.03.034 [DOI] [PubMed] [Google Scholar]
- 7.Safranek TJ, Jarvis WR, Carson LA, et al. Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentian violet skin-marking solution. N Engl J Med 1987;317:197–201. 10.1056/NEJM198707233170403 [DOI] [PubMed] [Google Scholar]
- 8.Brooks J, Behrens E, Prickett K. Painful and pruritic papules in the gray shading of a tattoo. JAMA Dermatol 2016;152:205–6. 10.1001/jamadermatol.2015.3448 [DOI] [PubMed] [Google Scholar]
- 9.Lee MR, Sheng WH, Hung CC, et al. Mycobacterium abscessus complex infections in humans. Emerg Infect Dis 2015;21:1638–46. 10.3201/2109.141634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez-Santiago TM, Drage LA. Nontuberculous mycobacteria: skin and soft tissue infections. Dermatol Clin 2015;33:563–77. 10.1016/j.det.2015.03.017 [DOI] [PubMed] [Google Scholar]