Abstract
Please cite this paper as: Bali NK et al. (2012) Knowledge, attitude, and practices about the seasonal influenza vaccination among healthcare workers in Srinagar, India. Influenza and Other Respiratory Viruses 7(4), 540–545.
Background Healthcare workers (HCWs) universally have a poor uptake of influenza vaccination. However, no data are available from India.
Objective To explore knowledge, attitudes, and practices associated with influenza vaccination in HCWs in a temperate climate area in northern India.
Patients and Methods A self‐administered questionnaire was offered to all HCWs in three major hospitals of Srinagar and information sought on motivations, perceptions, preferences and practices regarding influenza vaccination.
Results Of the 1750 questionnaires received, 1421 (81%) were returned. Only 62 (4·4%) HCWs had ever received influenza vaccination even as 1348 (95%) believed that influenza poses adverse potential consequences for themselves or their contacts; 1144 (81%) were aware of a vaccine against influenza and 830 (58%) of its local availability. Reasons cited by 1359 participants for not being vaccinated included ignorance about vaccine availability (435; 32%), skepticism about efficacy (248; 18%), busy schedule (166; 12%), fear of side effects (70; 4%), and a perception of not being‐at‐risk (82; 6%). Sixty‐one percent (865) believed that vaccine programs are motivated by profit. Eighty‐eight percent opined for mandatory vaccination for HCWs caring for the high‐risk patients, as a part of ‘employee health program’. Most of the participants intended to get vaccinated in the current year even as 684 (48%) held that vaccines could cause unknown illness and 444 (31%) believed their adverse effects to be underreported.
Conclusion Influenza vaccination coverage among HCWs is dismally low in Srinagar; poor knowledge of vaccine availability and misperceptions about vaccine effectiveness, fear of adverse effects and obliviousness to being‐at‐risk being important barriers. Multifaceted, adaptable measures need to be invoked urgently to increase the coverage.
Keywords: Healthcare workers, influenza, occupational hazard, vaccination
Introduction
Influenza is an important public health problem and it causes significant morbidity and mortality, particularly in the elderly and high‐risk groups. 1 Unvaccinated healthcare workers (HCWs) are an important source of nosocomial influenza. 2 , 3 , 4 Transmission of influenza virus from patients to HCWs, 5 HCWs to patients 6 and among HCWs 7 , 8 has been well documented. The possible consequences of infected HCWs include increased morbidity and mortality among patients at risk of contracting influenza and a high rate of ‘sickness absenteeism’ among the workers themselves resulting in shortage of staff, additional cost to the healthcare sector and a general draining of the healthcare delivery. 9 Sickness absenteeism in itself reaches proportions of 30–40% during influenza outbreaks in certain parts of the world. 10 Sick HCWs may contribute to transmission by presenting for work, when sick (presenteeism). 11
Influenza vaccination is the most effective strategy for the prevention of influenza virus infection and the potentially severe complications. 12 The World Health Organization and the Advisory Committee on Immunization Practices recommend that HCWs should be vaccinated annually against influenza. 1 , 12 It is also recommended that healthcare organizations implement policies and procedures to encourage HCWs vaccination. However, the coverage of influenza vaccination among HCWs is low at 42% even in countries with aggressive immunization programs. 12 There is a paucity of literature regarding influenza vaccination coverage rates among HCWs in developing countries. In a recent study, among 993 respondents, the vaccination rate was 24·7%, 67·2%, and 46·4% in UAE, Kuwait, and Oman, respectively. 13 While influenza activity has been documented in several studies from India, 14 , 15 , 16 there are no studies addressing the influenza vaccination coverage among HCWs, or their beliefs and behaviors concerning it. This study was designed to explore knowledge, attitudes, and practices (KAP) related to influenza vaccination in HCWs in North India with the ultimate goal to gather data to plan future interventions and policies aimed at increasing influenza vaccination coverage among HCWs.
Methods
This study is a cross‐sectional survey of HCWs, which was conducted in three hospitals of Srinagar (India), from April to June 2010. The three hospitals (Sheri‐Kashmir Institute of Medical Sciences (SKIMS), SMHS Hospital, and SKIMS Medical College Hospital) constitute the three major public health facilities in Srinagar, the summer capital of the state of Jammu and Kashmir. Influenza vaccinations are available only at a cost and do not constitute a strategy of the hospital or health services. In these hospitals, we contacted hospital staff at various departments, offices, meetings, classes, laboratories, hostels, wards, and support areas like laundry and dietetics. A brief introduction to the purpose of the study and instructions on ‘how to complete the questionnaire’ was given by one or two of the investigators during classrooms, ward seminars, clinical meetings or custom gatherings. The self‐administered survey was distributed, and all HCWs were encouraged to complete the survey. However, only 1750 forms were collected out of a total of about 4950 employees. The survey was voluntary and the completed forms were collected. A returned and completed form was taken as consent to participate in the survey. The participants consisted of more physicians and nurses compared with the ‘other’ staff, the consenting including more than 75% of the physician staff, more than 60% of the total nurses, and 30% of the ‘other’ staff. No identifiers were included and analysis was anonymous. The Institute Ethics Committee approved the survey.
The questionnaire consisted of 19 items and was designed to test the KAP of HCWs about seasonal influenza vaccination. The questionnaire contained only one question regarding the receipt of 2009 pandemic H1N1 vaccine. The questionnaire items addressed demographic information, profession and location of work, type of patients cared for, and importance of the influenza vaccine; whether a person was vaccinated within the last year or the last 5 years, number of times vaccinated in the preceding 5 years, and reasons that prevented HCWs from getting vaccinated. It also contained questions like type of information they needed, high‐risk categories for which influenza vaccine is strongly indicated, and best ways to reach them. General perceptions about vaccination were elicited by asking respondents to rank their agreement with five statements using a Likert scale numbered from 1 (agree) to 5 (disagree); responses were analyzed by recoding the values 1 or 2 as ‘agree’, the value 3 as ‘neutral’, and the values 4 or 5 as ‘disagree’. Data analysis was completed using the statistical package for the social sciences (SPSS for Windows version 11.5, IBM Corporation, Armonk, NY, USA). Statistical analyses used chi‐square (2) tests for comparison between categorical variables and the proportions were compared by z‐test for independent proportions. Bivariate analysis was used to examine associations between vaccination status and other independent variables. A P‐value of <0·05 was considered significant.
Results
Of the 1750 questionnaires distributed, 1421 (81%; 756 women, 665 men) were completed and returned within 1–24 hours. Of these, 1270 (89%) reported direct involvement with patient care. The occupation groups represented were physician and physician trainee (n = 764, 54%), nurse and nurse trainee (n = 478, 33·6%); and other (n = 179, 12·6%) including allied health professional; support staff (orderlies, ward boys, ward clerks, store staff, house‐keepers, maintenance staff, waste handlers, sanitary personnel, etc.). The highest number of respondents were in age group 26–39 (64%), followed by 18–25 years (20%), 40–49 years (15·1%), and more than 50 years 1%.
Analysis of the questions related to influenza knowledge revealed that 1348 (95%) respondents were aware that influenza poses adverse potential consequences for themselves, their family or patients, 1204 (84·7%) considered influenza as a potentially severe disease and 1144 (80·5%) were aware that a vaccine existed for influenza. While 830 (58·4%) participants were aware of its local availability, only 62 (4·4%) had actually received the vaccine 1–3 times (median 1) in the past 5 years. The recipients included 53 physician and physician trainees, six nurses/nurse trainees, and three others with the uptake rate of 4·8% versus 1·8% of the rest (P < 0·001). None of those vaccinated had received it more than thrice in the past 5 years.
The major reasons put forth for not participating in the influenza vaccination for the past 1–5 years by 1359 respondents (Table 1) ranged from ignorance about influenza vaccine availability to inability to find time for vaccination. Obliviousness to being‐at‐risk of influenza (n = 85) and potential harmful effects were also cited as reasons for not getting vaccinated, even as all but 47 (3·45%) considered influenza as a serious illness for the patients as well as for the staff. The ‘other reasons’ cited by 15% participants included, ‘not being‐at‐risk of influenza complications and not in contact with patients’, ‘do not want to get sick’, ‘have robust and overactive immune system’, ‘many people acquire the flu even though they got the shot’, ‘my gut feeling that it is not effective’, and ‘allergy to egg yolk’. Physicians and physician trainees were significantly more aware of a vaccine against influenza and its local availability.
Table 1.
Reasons for not getting vaccinated in the previous 5 years (n = 1359).
| Reason cited | Physician and physician trainee (n = 711) | Nurse and nurse trainee (n = 472) | Others (n = 176) | Total (n = 1359) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Influenza is not a serious illness to staff | 24 (3·4) | 14 (3·0) | 6 (3·4) | 44 (3·2) |
| I did not know about flu vaccine | 155 (21·8) | 224 (47·5) | 56 (31·8) | 435 (32·0) |
| There was no time to get vaccine at work | 123 (17·3) | 34 (7·2) | 9 (5·1) | 166 (12·2) |
| I do not believe flu shot is effective | 183 (25·7) | 47 (9·8) | 18 (10·2) | 248 (18·2) |
| I am not at risk of Influenza | 44 (6·2) | 28 (5·9) | 10 (5·7) | 82 (6·0) |
| Vaccine can harm my health | 10 (1·4) | 6 (1·3) | 1 (0·6) | 17 (1·3) |
| Influenza is not a serious illness to patients | 2 (0·3) | 1 (0·2) | 0 (0·0) | 3 (0·2) |
| I could not afford vaccine | 2 (0·3) | 1 (0·2) | 0 (0·0) | 3 (0·2) |
| Side effects are unpleasant | 21 (3·0) | 30 (6·4) | 2 (1·1) | 53 (3·8) |
| Other reasons* | 147 (20·7) | 54 (11·4) | 6 (3·4) | 207 (15·2) |
| No cited reason | 0 (0·0) | 33 (7·0) | 68 (38·6) | 101 (7·4) |
*‘other’ reasons included ‘medical community is too quick to cosnider it safe’, ‘people feel unwell after it’, ‘I get sick often’, etc"
Most (94·2%) of the respondents considered the vaccine to be safe, whereas 83 (5·8%) considered it unsafe. The reasons put forth for considering the vaccine unsafe included a perception that it could damage central nervous system (26%) or the immune system (17%); or an internet site (12%) or a physician (21%) had suggested that the vaccine was unsafe. Fifteen of the 83 also considered the vaccine unsafe as they had known someone who had been harmed by vaccination. Interestingly, even physicians had concerns about the possible untoward effects of vaccination on immune and the nervous system.
With regard to attitudes about immunization in general (Table 2), there was increasing agreement that vaccination programs are generally beneficial and a decreasing agreement that vaccines weaken immune system or can cause unknown illness. However, nearly 60% believed that vaccination programs are driven and motivated by profit and 31% (n = 444) believed that side effects related to vaccinations are under reported in the medical community.
Table 2.
Perception toward influenza vaccination program in Srinagar, India (n = 1421). The responses are classified as 1 – strongly agree, 2 – agree, 3 – neither agree nor disagree, 4 – disagree, 5 – strongly disagree. The figures in the parentheses represent the percentages
| Perception | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | Median |
|---|---|---|---|---|---|---|
| Vaccines cause unknown illness | 35 (2·5) | 246 (17·3) | 403 (28·4) | 551 (38·8) | 186 (13·1) | 4 |
| Vaccines weaken immune system | 24 (1·7) | 90 (6·3) | 92 (6·5) | 754 (53·1) | 461 (32·4) | 4 |
| Vaccine adverse effects are under reported | 68 (4·8) | 376 (26·5) | 730 (51·4) | 195 (13·7) | 52 (3·7) | 3 |
| Vaccine programs are beneficial | 682 (48) | 648 (45·6) | 40 (2·8) | 26 (1·8) | 25 (1·8) | 2 |
| Vaccine programs are motivated by profit | 241 (17·0) | 624 (43·9) | 351 (24·7) | 123 (8·7) | 82 (5·8) | 2 |
Eighty‐eight percent (n = 1250) of the 1421 respondents agreed that annual influenza vaccination should be mandatory or a condition of employment for HCW’s in high‐risk areas such as oncology, obstetric wards or pediatrics. Of the 808 respondents who identified high‐risk groups, 645 (80%) considered HCWs a high‐risk group for whom influenza vaccination is strongly recommended. Other high‐risk groups identified included persons more than 65 years with or without comorbid illness (n = 97, 12%), children aged 6–23 months (n = 63, 8%), pregnant women (n = 56, 7%), persons of 2–64 years with comorbid illnesses (n = 56, 7%), and residents of long‐term facilities (n = 33, 4%).
The reasons for not participating in the yearly vaccination are depicted in Figure 1 and included, among others, a disbelief about the efficacy of the vaccine and inability to find time for vaccination. A perception about vaccine side effects and its potential to damage the immune and the nervous system predominated among the physician group. None of the participants had received pandemic H1N1 vaccine despite free availability at the hospital pharmacy. However, more than 75% of the participants intended to get vaccinated in the current year.
Figure 1.
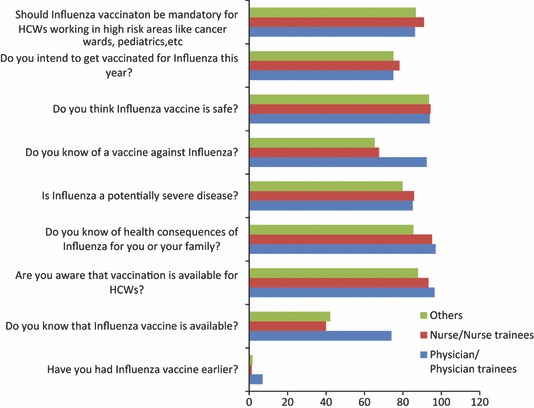
Showing the knowledge and perceptions held by different professional groups about influenza vaccination (bars depict positive responses).
The respondents in this survey expressed an urgent need for convenient dissemination of information about various aspects of influenza vaccination including safety and efficacy of the vaccine, information about outbreaks, difference between influenza and common cold and adverse effects of vaccination. Most preferred method for obtaining such information ranged from SMS via mobile phone (58·5%), through electronic mail (31·6%), or print newsletter (8·6%).
Discussion
Our data reveal a low coverage of influenza vaccination among HCWs in Srinagar, India despite a heightened awareness about post‐pandemic influenza in 2010 and a free‐of‐cost‐pandemic flu vaccine. Our study, to the best of our knowledge, is the first study addressing the KAP of seasonal influenza vaccination among the HCWs in India and demonstrates a vaccination rates far lower than that for other countries. 12 , 13 , 17 While regular influenza vaccination campaigns are routine in the developed countries, the vaccination strategies for seasonal influenza in India are mainly the initiatives of individual physicians and some hospitals, rather than a national policy and in most of the public hospitals guidelines or policies regarding flu vaccination of HCWs are non‐existent.
A combination of factors was found to influence the attitudes and practices of influenza vaccination among HCWs in Srinagar that ranged from a lack of awareness of the availability of flu vaccine to a reduced perception of risk and misperceptions about efficacy and adverse effects of the vaccine. About 60% believed that vaccination programs are motivated by profit and 31% believed that adverse effects are under reported. These trends, also reported earlier, 18 are logically plausible suggesting that non‐participants and low‐level participants were more likely to harbor unscientific beliefs about the harmful and beneficial effects of vaccination. Poor vaccination rates in the face of a widespread belief that influenza is a potentially dangerous disease depict a serious disconnect between the perception and practice and call for educational programs aimed at removing the barriers that limit compliance. Variable knowledge about the general and local availability of the vaccine among various groups of employees and a difference in the uptake between physicians and physician trainees and all others call for even more enhanced and intensive education of the nurse and nurse trainee and ‘other’ groups. Nearly, 47% of the participant nurses and nurse trainees and 32% of ‘other staff’ reported that they did not know about the flu vaccine. These results call for concerted educational efforts to increase the awareness about the existence and the availability of the vaccine against influenza.
Nearly, 26% (n = 183) of participant physician/physician trainees and nearly 10% of the other groups (Table 1) had a perceived lack of efficacy of the vaccine as a major dissuasion from immunization. The efficacy of influenza vaccines against confirmed influenza among adults is 70–90% when the vaccine strains match the circulating strains. 19 Immunization has been shown to significantly reduce influenza like and upper respiratory illnesses and sick leave for influenza in HCW and other healthy working adults. 20 , 21 It has been estimated that 80% of the HCWs must be vaccinated to achieve herd immunity within the healthcare facilities, 22 the goal of coverage being 100% of employees who do not have medical contraindications. Such bits of information need to be continually fed to the HCWs in order to improve the vaccination coverage rates.
In the present study, HCWs without direct patient contact were strategically included because such staff members continue to work when ill with influenza and may infect coworkers who are direct caregivers, or may infect patients in public areas of the facility such as corridors and the cafeteria. Finally, restricting influenza vaccination to staff members with direct patient contact may reinforce the belief that influenza vaccination is intended to protect the health of patients ‘at the expense, potential harm, and burden of responsibility of the staff’. 23
Influenza vaccination among HCWs need be measured regularly and monitored. An incentive for vaccination, an intensified advertising campaign, and offering a choice of influenza vaccines have been shown to improve vaccination rates in the workplace. 24 , 25 A mandatory influenza vaccination policy, exempting only those HCWS with a medical contraindication, has been demonstrated to be a highly effective in achieving high vaccine coverage, 26 , 27 with some programs requiring persons refusing vaccination without valid reason to wear a surgical mask during influenza season in some programs. 26 Healthcare administrators must consider the level of vaccination coverage among HCWs to be one measure of a patient safety quality program and consider obtaining signed declinations from personnel who decline influenza vaccination without medical contraindications. 12 , 27 A high degree of agreement by the participants in the present survey regarding the linking of employment in high‐risk areas to influenza vaccination may prove just the silver lining to emphasize that HCWs as a whole constitute the high risk for whom the peers recommend universal vaccination. As such the data emphasizes the development of clear cut guidelines by hospitals to offer routine influenza vaccination as a standard policy for all HCWs.
The participants in the current survey wanted to have convenient access to influenza vaccine at work. As such programs that combine publicity and education with efforts to remove the administrative and financial barriers to vaccination are urgently needed everywhere. The fact that HCWs did not cite affordability as a major reason for non‐participation in the vaccination, majority of them desired the vaccine to be provided free of cost as a part of employee health policy. However, intense sensitization regarding vaccination needs to be undertaken because the uptake of pandemic flu vaccine was nil among the participants even when it was provided free under a national program. However, it must be noted that pandemic influenza vaccine was made available in spring 2010 by which time pandemic H1N1 had largely waned across most areas in the world including India. Additionally, the vaccine was offered without any information/educational campaign and without any incentives. Many studies have demonstrated that the highest level of coverage is reached when vaccine is provided free of charge after extensive educational programs and in association with an incentive. 28 , 29 , 30
There are several limitations to this study. First, influenza vaccination status was self‐reported by respondents, not subject to independent verification, and potentially influenced by social desirability bias. Recall bias is another potential limitation; however, the survey was fielded in April to June 2010 of the influenza season in question, thus limiting the time elapsed since the typical influenza vaccination season.
In conclusion, influenza vaccination coverage is dismally low in the HCWs in the northern Indian state of Jammu and Kashmir. Low rates stem from a variety of reasons ranging from inadequacy of knowledge to misperceptions and fears regarding vaccine effectiveness and safety. Intensive education activities and other adaptable measures aimed at removing of the barriers to vaccination need to be embarked upon urgently so that influenza vaccination is considered an ethical responsibility and a subject of patient safety, thus making it a personal issue, a professional issue, and an institutional mandate.
References
- 1. World Health Organization . Influenza vaccines. WHO position paper. Wkly Epidemiol Rec 2002; 28:229–240. [Google Scholar]
- 2. Horcajada JP, Pumarola T, Martinez JA et al. A nosocomial outbreak of influenza during a period without influenza epidemic activity. Eur Respir J 2003; 21:303–307. [DOI] [PubMed] [Google Scholar]
- 3. Clynes NS, Schneider N. Hospital‐acquired influenza: seek and ye shall find. Am J Infect Control 2005; 33:E123–E124. [Google Scholar]
- 4. Harrison J, Abbott P. Vaccination against influenza: UK health care workers not on message. Occup Med 2002; 52:277–279. [DOI] [PubMed] [Google Scholar]
- 5. Kapila R, Linz DI, Tecson FT, Ziskin L, Louria DB. A nosocomial outbreak of influenza. Chest 1977; 71:576–579. [DOI] [PubMed] [Google Scholar]
- 6. Center for Disease Control . Suspected nosocomial influenza cases in an intensive care unit. MMWR Morb Mortal Wkly Rep 1998; 37:3–4. [PubMed] [Google Scholar]
- 7. Horman JT, Stetler HC, Israel E, Sorley D, Schipper MT, Joseph JM. An outbreak of Influenza A in a nursing home. Am J Public Health 1986; 76:501–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CDC . Outbreak of Influenza A in a nursing home – New York. December 1991–January 1992. MMWR Morb Mortal Wkly 1992; 41:129–131. [PubMed] [Google Scholar]
- 9. Koul PA. Influenza vaccination and healthcare workers: ‘From slumber thou rise’ (Editorial). J Med Med Sci 2010; 1:433–436. [Google Scholar]
- 10. Hansen S, Stamm‐Balderjahn S, Zuschneid I et al. Closure of medical departments during nosocomial outbreaks: data from a systematic analysis of the literature. J Hosp Infect 2007; 65:348–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tosh PK, Jacobson RM, Poland GA. Influenza vaccination in health care workers. The Vaccine Companion to….the Influenza Paradox and the need for implementation of the Guidelines for the Control of Influenza Disease. 2009;2:vii–viii. [Google Scholar]
- 12. Centers for Disease Control and Prevention . Prevention & control of influenza with vaccines – Recommendations of the Advisory Committee on Immunization Practices (ACIP) 2010. MMWR Recomm Rep 2010; 59:1–62. [PubMed] [Google Scholar]
- 13. Abu‐Gharbieh E, Fahmy S, Rasool BA, Khan S. Influenza vaccination: healthcare workers attitude in three middle east countries. Int J Med Sci 2010; 7:319–325. Available from http://www.medsci.org/v07p0319.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mishra AC, Chadha MS, Choudhary ML, Potdar VA. Pandemic influenza (H1N1) 2009 is associated with severe disease in India. PLoS ONE 2010; 5:e10540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tandale BV, Pawar SD, Gurav YK et al. Seroepidemiology of pandemic influenza A (H1N1) 2009 virus infections in Pune, India. BMC Infect Dis 2010; 10:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koul PA, Mir MA, Bali NK, et al. Pandemic and seasonal influenza viruses among patients with acute respiratory illness in Kashmir (India). Influenza Other Respi Viruses 2011; 5:e521–e527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kroneman M, Paget WJ, van Essen GA. Influenza vaccination in Europe: an inventory of strategies to reach target populations and optimize vaccination uptake. Euro Surveill 2003; 8:130–138. [PubMed] [Google Scholar]
- 18. Hurwitz ES, Haber M, Chang A et al. Effectiveness of influenza vaccination of day care children in reducing influenza‐related morbidity among household contacts. JAMA 2000; 284:1677–1682. [DOI] [PubMed] [Google Scholar]
- 19. Fukuda K, Levandowski RA, Bridges CB, Cox NJ. Inactivated influenza vaccines; in Plotkin SA, Orenstein WA. (eds): Vaccines, 4th edn Philadelphia, PA: Saunders, 2004; 339–370. [Google Scholar]
- 20. Saxen H, Virtanen M. Randomized, placebo‐controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J 1999; 18:779–783. [DOI] [PubMed] [Google Scholar]
- 21. Nichol KL, Lind A, Margolis KL et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med 1995; 333:889–893. [DOI] [PubMed] [Google Scholar]
- 22. Maltezou HC. Nosocomial influenza: new concepts and practice. Curr Opin Infect Dis 2008; 21:337–343. [DOI] [PubMed] [Google Scholar]
- 23. Manuel DG, Henry B, Hockin J, Naus M. Health behavior associated with influenza vaccination among healthcare workers in long‐term care facilities. Infect Control Hosp Epidemiol 2002; 23:609–614. [DOI] [PubMed] [Google Scholar]
- 24. Nowalk MP, Lin CJ, Toback S et al. Improving influenza vaccination rates in the workplace: a randomized trial. Am J Prev Med 2010; 8:237–246. [DOI] [PubMed] [Google Scholar]
- 25. CDC . Interventions to increase influenza vaccination of health‐care workers – California and Minnesota. MMWR Morb Mortal Wkly Rep 2005; 54:196–199. [PubMed] [Google Scholar]
- 26. Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis 2010; 50:459–464. [DOI] [PubMed] [Google Scholar]
- 27. Pavia AT. Mandate to protect patients from health care‐associated influenza. Clin Infect Dis 2010; 50:465–467. [DOI] [PubMed] [Google Scholar]
- 28. Lindley MC, Horlick GA, Shefer AM, Shaw FE, Gorji M. Assessing state immunization requirements for healthcare workers and patients. Am J Prev Med 2007; 32:459–465. [DOI] [PubMed] [Google Scholar]
- 29. Canning HS. Healthcare workers beliefs about influenza vaccine and reasons for non‐vaccination – a cross‐sectional survey. J Clin Nurs 2005; 14:922–925. [DOI] [PubMed] [Google Scholar]
- 30. Soung JY, Park CW, Jeeong WH, Cheong HJ, Kim WJ, Kim SR. Effect of a hospital campaign for influenza vaccination of healthcare workers. Infect Control Hosp Epidemiol 2006; 27:612–617. [DOI] [PubMed] [Google Scholar]


