Abstract
Introduction
Our current ability to predict the course and outcome of early psychotic symptoms is limited, hampering timely treatment. To improve our understanding of the development of psychosis, a different approach to psychopathology may be productive. We propose to reconceptualise psychopathology from a network perspective, according to which symptoms act as a dynamic, interconnected system, impacting on each other over time and across diagnostic boundaries to form symptom networks. Adopting this network approach, the Mapping Individual Routes of Risk and Resilience study aims to determine whether characteristics of symptom networks can predict illness course and outcome of early psychotic symptoms.
Methods and analysis
The sample consists of n=100 participants aged 18–35 years, divided into four subgroups (n=4×25) with increasing levels of severity of psychopathology, representing successive stages of clinical progression. Individuals representing the initial stage have a relatively low expression of psychotic experiences (general population), whereas individuals representing the end stage are help seeking and display a psychometric expression of psychosis, putting them at ultra-high risk for transition to psychotic disorder. At baseline and 1-year follow-up, participants report their symptoms, affective states and experiences for three consecutive months in short, daily questionnaires on their smartphone, which will be used to map individual networks. Network parameters, including the strength and directionality of symptom connections and centrality indices, will be estimated and associated to individual differences in and within-individual progression through stages of clinical severity and functioning over the next 3 years.
Ethics and dissemination
The study has been approved by the local medical ethical committee (ABR no. NL52974.042.15). The results of the study will be published in (inter)national peer-reviewed journals, presented at research, clinical and general public conferences. The results will assist in improving and fine-tuning dynamic models of psychopathology, stimulating both clinical and scientific progress.
Trial registration number
NTR6205; Pre-results.
Keywords: psychiatry, mental health
Strengths and limitations of this study.
One of the first studies examining the predictive potential of dynamic symptoms networks for the onset and progression of psychopathology.
The study design allows considering within-individual and between-individual variation in symptomatology, both at the micro (day) and macro (year) level.
A dynamic, transdiagnostic approach is adopted; outcome measures include clinical stage, diagnosis, symptoms of a broad range of disorders and functioning.
With annual follow-ups up to four years after baseline, we may not capture all transitions to psychosis.
The exploratory nature of the study warrants replication of the findings.
Introduction
Psychotic disorders are among the most severe mental disorders in terms of individual and societal impact.1 2 Therefore, early detection and intervention in psychosis should be highly prioritised,3 which is increasingly acknowledged.4 Psychosis is currently conceptualised as a continuum of psychotic severity, encompassing both subclinical and clinical expressions.5 As such, psychotic symptoms are present in the context of psychotic disorders and across other, non-psychotic disorders.6 7
Current diagnostic systems in psychiatry are challenged by issues such as high levels of comorbidity, clinical heterogeneity, non-specific treatment effects and lack of diagnosis-specific biological/cognitive markers.8–12 Despite this, traditional diagnoses still dominate psychiatric research, hampering scientific progress. These diagnoses are based on clinical presentation of adults with long-established illness13 and classify individuals according to distinct diagnostic labels8 (eg, schizophrenia or major depressive disorder). However, it is increasingly acknowledged that psychopathology is expressed dimensionally, representing a quantitative as well as qualitative deviation from mental health.8 14–19 In addition, it is increasingly accepted that mental disorders do not emerge fully formed in adulthood but evolve gradually, often manifesting for the first time already in adolescence.20 21
A model that was designed to capture this continuity of both severity and time is the clinical staging model.22 23 This model describes psychopathology as ranging, through subsequent but qualitatively different stages, from increased risk of mental illness at the lowest level to progressive stages of severity, resulting in separable but overlapping syndromes at the highest levels.24 25 Stage 0 represents individuals at increased risk without symptoms; stage 1a represents ‘help-seeking’ individuals with mild, non-specific symptoms; stage 1b represents individuals with an ‘attenuated syndrome’, with moderate but subthreshold symptoms and moderate functional decline; stage 2 holds individuals with a first episode of a clinical, ‘discrete’, disorder; stage 3 holds individuals with persistent or recurrent illness13 22 23 and stage 4 represents individuals with chronic illness. This clinical staging model further hypothesises that psychopathological expression is more multidimensional, non-specific and more susceptible to intervention in early stages and becomes more crystallised, disorder specific and treatment resistant in later stages.25 This model offers a theoretical representation that seems to fit better to the true nature and development of psychopathology9–11 26 and hence may improve diagnostic accuracy. It has been developed most extensively in the context of psychosis23 25 27 but needs further empirical validation. Longitudinal studies assessing predictive validity of the model have mostly concentrated around the transition from stage 1b (ultra-high risk) to stage 2 (first psychotic episode) and found 3-year transition rates of 36%.28 In addition, some biological and cognitive measures seem to be more abnormal in more severe stages, and these measures seem to change in patients who progress in stage.29 30 Finally, some treatments seem more effective for individuals in early stages.30 Taken together, these studies provide at least some support for the clinical staging model of psychosis. However, many questions still remain, for example, about what drives progression through subsequent stages and how the thresholds between the stages should be defined exactly.
The expression and development of early psychotic symptoms are highly variable31–34 and difficult to predict.28 35 One reason for this is that many studies so far have focused on early psychotic symptoms as specific predictors of later schizophrenia. However, this approach may be too narrow25 33 36 because early psychotic symptoms are often transitory,37–39 also occur in the context of6 7 40–42 and predict other mental disorders28 37 43 44 and vice versa.45–47 High levels of comorbidity48 and overlap of risk factors49–52 also challenge the assumed independence of psychosis from other symptom domains. In addition, the information that is used to predict course and outcome is often based on cross-sectional assessment of symptoms and comparisons are often made at the group level. However, symptoms can vary substantially over time, both over short (ie, days) and long intervals (months and years), within one individual and can also cross diagnostic borders.53 This means that the clinical picture can change, particularly in the early phase of a disorder.25 These characteristics of psychopathology suggest that the ‘static’ model prediction may not be fit for the purpose. This is reflected in the modest accuracy and replicability of static prediction models in the psychosis prediction field.54–56
The above-mentioned challenges may be overcome by taking a different approach towards the conceptualisation of psychopathology, its measurement and the way we model it. By taking a more transdiagnostic approach, incorporating symptoms and experiences from multiple (psychotic and non-psychotic) domains, the narrow focus on the sole dimension of psychosis can be broadened. Furthermore, by modelling individual symptom patterns over time, a more developmental as well as a more personalised approach can be taken that, in addition, builds on a more detailed inventory of symptomatology compared with baseline (cross-sectional) assessment scores. Finally, modelling the interconnectivity between symptoms by mapping individual symptom networks and patterns of co-occurrence in and over time could provide us with a better idea of how psychopathology develops and may give us clues on what processes may drive progression through subsequent clinical stages.56 57
A network approach to psychopathology
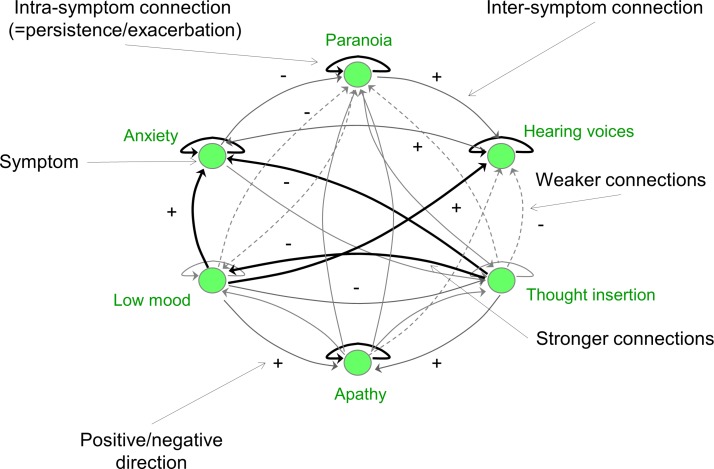
A focus on dynamic symptom networks requires an innovative approach to psychopathology. One of the currently promising alternative approaches comes from network theory. From this network perspective, psychopathology, at a phenomenological level, is hypothesised to result from interactions between symptoms.11 58 59 Mental disorders are thus represented by sets of symptoms, connected in networks by causal relations11 58 (see also figure 1). These networks are dynamic and capture reciprocal influences between symptoms over time (eg, feedback loops). Importantly, symptoms are acknowledged as causal factors in psychopathological development: one symptom (eg, anxiety) can cause another (eg, paranoia). This is in sharp contrast with current dominant models that represent symptoms as independent indicators of underlying, latent constructs (eg, schizophrenia). As stress is important in the development of psychosis,60 61 the sensitivity of symptom networks to risk-enhancing (trauma) and risk-reducing (coping and social support) factors62 63 also needs attention. The network approach has been successfully applied in other fields64 65 but is relatively novel in psychiatry, where it has been investigated mainly in common mental disorders66 but not psychosis.
Figure 1.
Parameters of a theoretical symptom network. Note: this figure is for illustrative purposes and is not based on real data.
Aims and hypotheses
With the Mapping Individual Routes of Risk and Resilience (Mirorr) study, we aim to investigate the hypothesis of dynamic symptom networks as the basis of psychopathology in general and psychosis in particular. The key hypothesis to be tested centres on the question whether individual networks of a broad scope of transdiagnostic symptoms can predict course and outcome of early psychopathology in young individuals at increased risk for psychosis and other severe mental illness. Furthermore, we aim to investigate the additional hypothesis of symptom networks as markers/indicators of progression of illness through successive clinical stages. Taking a broader, multidimensional and process-oriented approach, we will examine how symptoms of multiple domains influence each other over time and across diagnostic boundaries, in interaction with environmental factors. More specifically, we hypothesise that different clinical stages will be characterised by different symptom networks. In addition, we expect that characteristics of these networks can predict progression through clinical stages. We will explore the predictive potential of several characteristics, such as the strength and directionality of symptom connections (see figure 1) and centrality indices (information about the position of a symptom in the network). Finally, we will evaluate the predictive potential of these characteristics against (more) static assessments of symptom severity.
The Mirorr study is unique in its design and in its attempt to (1) bring together a network approach to psychopathology and the clinical staging model, (2) take a broader perspective on mental illness by (A) taking a transdiagnostic approach towards symptomatology and (B) defining outcome more broadly in the context of clinical staging (incorporating both clinical and functional outcomes) and (3) modelling individual symptom networks over time by using time-series data, enabling us to model more personalised pathways of psychopathological development.
Outcome measures
Traditionally, research in the field of psychosis focuses mostly on transition from clinical high risk to a first episode of psychosis.67 However, there is growing awareness that this may be arbitrary, especially in the context of a staging model that acknowledges expression of illness along a much broader severity spectrum. In addition, functional outcome is becoming more and more an important outcome of interest, as it has been shown that both clinical and functional outcomes are important but not always congruent.68–70 Working from a clinical staging perspective, important outcomes to investigate include therefore progression through clinical stages, functioning and need for care.
Methods and analysis
Study design
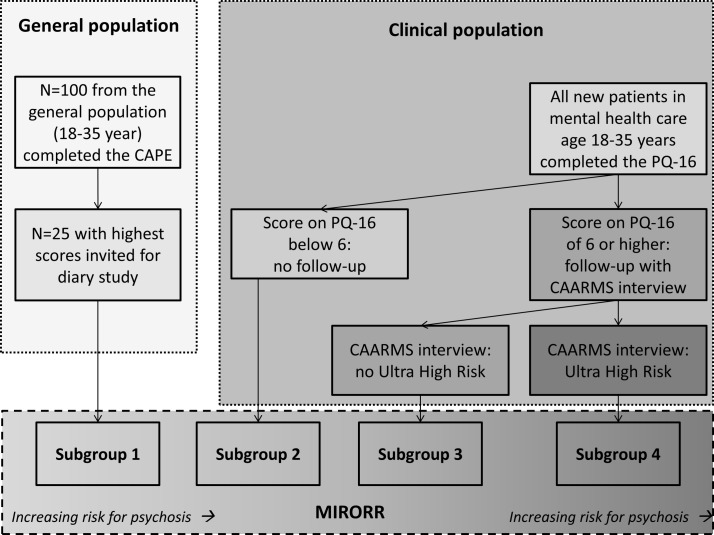
This study combines idiographic (within-person) and nomothetic (between-person) observational study designs. The nomothetic aspect of the study is captured by questionnaire and interview data at baseline and 3 yearly follow-up measurement waves. Among other things, symptomatology, functioning and need for care will be assessed (outcome measures), as well as risk and protective factors. The idiographic aspect is captured by diary assessments at baseline and the first follow-up wave. During the diary periods, participants will complete a diary questionnaire daily for a period of 90 days on their smartphone regarding symptoms, emotions, functioning and stress. These diary data are used to map individual symptom networks. For the second diary period, participants can also opt to keep continuing the questionnaire follow-ups but not have a second diary period. A flow chart of the study is presented in figure 2.
Figure 2.
Flow chart. Note: light grey area within blue dashed square indicates optional measurements.
Study population
The total sample comprises 175 individuals of 18–35 years, whereof 100 will enter the main study (ie, the daily diary study and the yearly follow-ups). For the main study, there will be four subsamples, all n=25 (figure 3) with each subgroup, having an increasingly more severe psychopathological level and thus representing subsequent clinical stages. For subsample 1 (lowest level of psychopathology and thus lowest clinical stage), 100 individuals will be randomly selected from the general population in the north of the Netherlands and administered the Community Assessment of Psychic Experiences (CAPE).71 Of all the respondents who meet the inclusion and exclusion criteria of the study, the highest scoring quartile will be included in the main study. For subsamples 2–4, individuals will be recruited from mental healthcare institutions in the four northern provinces in The Netherlands. For all individuals who are referred to mental healthcare, psychotic symptoms are routinely screened by means of, among other things, the Prodromal Questionnaire (PQ).72 If the score on the PQ is 6 or higher, the Comprehensive Assessment of At Risk Mental State (CAARMS)73 is administered as well. With these scores, it is determined for which subsample (2–4, explained below) eligible subjects will be recruited, where a higher subsample indicates higher levels of psychopathology.
Figure 3.
Definition of subgroups. CAARMS, Comprehensive Assessment of At Risk Mental State; CAPE, Community Assessment of Psychic Experiences; Mirorr, Mapping Individual Routes of Risk and Resilience; PQ, Prodromal Questionnaire.
In order to be eligible to participate in the study, subjects must meet all of the following criteria: (1) aged between 18 and 35 years, (2) read and speak Dutch fluently, (3) capable of following the research procedures and (4) provide informed consent. In addition, participants of subsample 1 should not be in clinical care for mental health at the moment of screening. In contrast, participants of subsamples 2–4 should currently be in clinical care for mental health. In addition, participants of subsample 2 should have mild, non-psychotic psychopathology, as evidenced by a score below 6 on the PQ, participants of subsample 3 should have mild psychopathology including subclinical psychotic symptoms, as evidenced by a score of or above 6 on the PQ but are not at ultra-high risk (UHR) for psychosis, as indexed by the CAARMS. Finally, participants of subsample 4 should be at UHR for psychosis, as indexed by the CAARMS. Exclusions criteria are: (1) a history of or current psychotic episode, according to the Diagnostic and Statistical manual of Mental Disorders 4 (DSM-4) criteria, (2) significant hearing or visual problems impairments and (3) pregnancy, as stated on a general health questionnaire.
Procedure
Recruitment
To recruit subsample 1, the study will be announced at several university sites, public places in Groningen and social media (start recruitment: September 2015). Interested individuals can contact the researchers by phone or email for more information. They will then be sent an information letter, flyer, informed consent form and the initial screenings questionnaires. After receiving the completed screening questionnaires and informed consent forms, the 25 (out of 100) individuals with the highest CAPE scores will be invited to participate in the main study (first inclusion: December 2015). For subsamples 2–4, individuals will be recruited from mental healthcare institutions in four northern Dutch provinces (first inclusion: April 2016). To which subsample they will be recruited is determined using the instruments described under study population. For these sites where patients give their consent for receiving information about ongoing research projects, a package containing detailed information on the study (information letter and flyer), along with screening questionnaires and an informed consent form, will be sent to potential participants. Interested individuals can fill out and return requested forms (including informed consent form). After receiving the requested forms, an individual’s therapist will be consulted about several exclusion criteria. For these sites where participants do not give consent in advance, the individual’s clinical worker will be provided a package containing detailed information on the study (information letter and flyer), along with screening questionnaires and an informed consent form. The clinical worker will prescreen his/her client on the exclusion criteria of the study and hand over the package if he/she fits the profile of the study. Study participants can continue their therapy and medical treatment as usual; they will be asked to register any changes in medication or treatment during the daily ambulatory assessments.
Screening
The information package that interested individuals receive contains an information letter, two screening questionnaires and an informed consent form. All potential participants can ask questions before completing the informed consent form or the screening questionnaires. As mentioned in the information letter, in case subjects decide to participate, they should fill out and send back these questionnaires and the informed consent form. This consent form covers the baseline ambulatory assessment period and the yearly follow-up assessments (three in total). On this consent form, permission will be asked to reinvite subjects for the follow-up ambulatory assessment period, for which they have to complete a separate consent form (1 year later). Also, permission will be asked to use data from the psychiatric case register of the north of the Netherlands. The first screening questionnaire is a screening questionnaire on general health, containing questions on demographics, health complaints (such as visual or hearing impairments), pregnancy, drug and alcohol use, medication use and mental health problems. This will be used to screen on exclusion criteria. The second screening questionnaire is the CAPE. This instrument is used to screen individuals recruited from the general population (subsample 1) on psychotic experiences but will be administered to all participants to enable group comparisons on the level of subclinical psychotic experiences. The highest scoring quartile (n=25) will subsequently be included in the main study. Subjects will have 1 week to decide about participation.
Baseline interview and ambulatory assessments (year 1)
If subjects are eligible to enter the study and agree to participate, they will be invited (by telephone or email) for an introduction interview at the University Medical Centre Groningen. A few days before the interview, self-report questionnaires will be administered via email (see data management for more information). The questionnaires assess symptomatology, functioning, clinical stage and factors of risk and resilience. During the interview, the study will be explained to them in detail, and a diagnostic psychiatric interview will be held. If in an exceptional case the participant does not possess a smartphone, this will be provided to the participant during the study period. An appointment for an end-of-study interview will be planned. Also, the participants will be asked to designate suitable moments at which the researcher can call him/her to inquire on the progression of the study and to help with any problems the participant may experience.
The participants then start completing the electronic daily diary for 3 months. Every evening, they receive a text message with a link that directs them to a web-based diary questionnaire in a secure environment. Measurements are always in the evening, asking about the past day; exact times can vary per person (but not per day) and are fixed according to the participant’s wishes. However, all participants have 24 hours between each measurement point. For example, participant A will always receive her text message at 22:00 and participant B always at 21:15. A window of 1.5 hours will be allowed to fill in the diary, and reminder messages will be send every half hour. Short questions will be presented on sequential screens, which are mainly answered using visual analogue scales. During the research period, participants are also provided a paper log, in which they can note any unusual events, start of or changes in medication use and problems they encounter with the research procedures. The researchers will telephone the participants six times during the study period (every other week) to motivate the participant, answer questions about the study procedures and provide technical help. They will also be available by telephone and email if participants need help at other moments.
During the end-of-ambulatory-assessment (3 months after baseline) interview participants will fill out an online questionnaire battery once more and report on any changes in medical treatment. Furthermore, they will also be asked to comment on the data collection and the study in general. We will use this information to check whether the study affected their thoughts and behaviours in any way, whether there had been special events that might have affected the data collected.
Follow-up assessments
All participants will receive questionnaires about functioning and clinical stage via email 1, 2 and 3 years after baseline. The participants will be able to fill these in at home. Shortly after filling in the questionnaires, participants will be interviewed by telephone or face to face at one of our research facilities, depending on their preferences, to establish the presence/absence of psychiatric disorders with a diagnostic interview. In addition, to distinguish individuals in clinical stage 1a from individuals in clinical stage 1b (all individuals with a score of 6 or higher on the PQ-16), data from the CAARMS interview is needed. Participants will be reminded about the follow-up assessments a few weeks before the actual follow-up by means of an information letter.
Follow-up ambulatory assessment period (year 2)
In the aforementioned information letter, participants will also read information about a second ambulatory assessment period that they can enrol in. If they are interested, they are invited for another introduction interview (given that they still fulfil the inclusion and exclusion criteria as evidenced by their answers to an online version of a general health questionnaire). This interview is similar to the introduction interview at baseline (ie, questionnaire battery and procedures). An exception is that questionnaires about symptomatology, functioning and clinical stage will not be administered, because they have been covered already by the usual follow-up assessments. Participants then start their second 3-month period of ambulatory assessments 1 year after the first diary period. The end of ambulatory assessment interview will take place, again with similar questionnaires to the one held at baseline.
Instruments
A complete overview of the instruments used throughout the study is presented in table 1.
Table 1.
Overview of instruments
| Domain | Instrument | Method | Purpose | Time (min) |
Screening | Diary pre (baseline) | Diary post | Follow- up 1 | Diary pre | Diary post | Follow- up 2 | Follow-up 3 |
| T0 | T0 | T0 (3 m) | T1 | T1 | T1 (3 m) | T2 | T3 | |||||
| Demographics | Gen. health | SR | Demogr, conf. | 5 | X | X* | ||||||
| Vignette | INT | History psychosis | 5 | X† | ||||||||
| Psychosis | CAPE | SR | Psychotic Sx | 6 | X | X | X | X | X | X | ||
| PQ | SR | Clinical stage | 3 | X‡ | X‡ | X‡ | X‡ | |||||
| CAARMS | INT | Clinical stage | 30–90 | X‡§ | X‡§ | X‡§ | X‡§ | |||||
| Psychopathology | Mini-SCAN | INT | Diagnosis | 30 | X | X | X | X | ||||
| SCL-90 | SR | Severity | 20 | X | X | X | X | |||||
| PsychCaseReg | REG | Care use | – | X | X | X | X | |||||
| Care use – extra | SR | Care use | 1 | X | X | X | X | |||||
| DASS | SR | Depress Anxiety Sx | 3 | X | X | X | X | |||||
| ASRM | SR | Mania Sx | 3 | X | X | X | X | |||||
| Social functioning | GVSG-45 | SR | Social functioning | 8 | X | X | X | X | ||||
| Flourishing Sc | SR | Well-being | 1 | X | X | X | X | |||||
| Risk and resilience | SSL | SR | Social support | 7 | X | X | X | X | ||||
| IPPA | SR | Bonding | 9 | X¶ | ||||||||
| BRS | SR | Resilience | 2 | X | X | X | X | |||||
| UCL | SR | Coping | 5 | X | X | X | X | |||||
| Brugha LTE | SR | Life events, trauma | 4 | X | X | |||||||
| MCTQ | SR | Sleep | 3 | X | X | |||||||
| Faux-Pas Task | INT | Social cognition | 5 | X¶ | ||||||||
| Actical | SENS | Physical activity | – | X** |
*Send out several weeks before the daily diary period to screen on exclusion criteria.
†Only administered when there is a history of a psychiatric disorder according to the information on the General Health Questionnaire.
‡Available as routine outcome monitoring (ROM) data for all individuals in clinical care for mental health at each measurement wave.
§Only administered when PQ score is 6 or higher.
¶Administered only to subgroup 4.
**Offered to participants as optional.
ASRM, Altman Self-Rating Mania Scale; BRS, Brief Resilience Scale; CAARMS, Comprehensive Assessment of At Risk Mental State; CAPE, Community Assessment of Psychic Experiences; conf, confounders; DASS, Depression Anxiety and Stress Scale; demogr, demographics; depress, depression; GVSG-45, Groningse Vragenlijst voor Sociaal Gedrag; IPPA, Inventory of Parent and Peer Attachment; INT, interview; LTE, List of Threatening Experiences; MCTQ, Munich Chronotype Questionnaire; Mini-SCAN, Schedules for Clinical Assessment in Neuropsychiatry, short version; PQ, Prodromal Questionnaire; REG, register; SCL-90, Symptom Check List; SENS, sensor; SR, self-report; SSL, Social Support List; Sx, symptoms; T, measurement wave; UCL, Utrechtse Coping Lijst.
Diary measures
The items assessed in the daily questionnaires will be used to model individual networks of symptoms, experiences and emotions. Items included in the dairy questionnaires were chosen from a transdiagnostic perspective and cover a broad range of feelings and experiences that are characteristic for (subclinical) psychotic experiences, depression, anxiety, mania, obsessive compulsive behaviour and anger. These disorders are known for the co-occurrence of psychotic symptoms6 7 and comorbidity.48 For the complete item list, see online supplementary table 1.
bmjopen-2017-019059supp001.pdf (87.2KB, pdf)
Positive psychotic experiences can be divided into five categories, namely paranoia, delusions, hallucinations, megalomania and paranormal beliefs.74 Because paranormal beliefs are often stable over time, we will include items covering the first four categories. Negative symptoms of psychosis will be covered by items about flattened affect (eg, anhedonia, low motivation and social withdrawal), which resemble closely the negative symptoms of the CAPE. Most items are adopted from previous experience sampling method (ESM) studies,75–77 and all items are adapted for daily use.
Symptoms of depression will be measured using items that correspond closely to the Patient Health Questionnaire-9,78 a self-administered questionnaire for screening and measuring the severity of depression. Anxiety symptoms will be measured using items that correspond closely to the Hospital Anxiety and Depression Scales – Anxiety.79 Mania, obsessive compulsive behaviour and anger are measured with items that correspond closely to items from the DSM-5—screener for the corresponding clinical disorders.80
Positive and negative mood states over the past day will be measured with 12 items from the circumplex model of affect.81 82 Momentary affect will be measured with an item for valence (‘I feel unpleasant – pleasant’) and activation (‘I feel aroused/activated – quiet/still’) at the beginning of each diary entry. Other items cover sleep, daily activities and situations that may influence psychiatric symptoms, such as positive and negative events, social interactions, coping behaviour, physical activity and drug use.
Follow-up measures
Important outcomes that are linked to the above described network characteristics are (progression through) clinical stages, functioning and need for care. Progression through clinical stages will be assessed with the PQ-16, the CAPE and the CAARMS, the Symptom Check List (SCL-90)83 and the Schedules for Clinical Assessment in Neuropsychiatry, short version.84 Social functioning will be assessed using the Groningse Vragenlijst voor Sociaal Gedrag85 and the Flourishing Scale.86 Need for care will be assessed using self-reported information on care use. Additionally, need for care will be assessed by linking data from the psychiatric case registry to our sample when approved by the participant (as stated on the informed consent form). Specifically, the frequency and type of care use throughout the study period will be obtained.
Assessments predaily and postdaily diary period(s)
Before and after the daily diary assessments, several questionnaires will be administered to assess symptomatology, functioning and several risk and resilience factors. Psychotic symptoms will be assessed with the CAPE, depression and anxiety symptoms with the Depression Anxiety and Stress Scale,87 mania symptoms with the Altman Self-Rating Mania Scale,88 social support with the Social Support List,89 resilience with the Brief Resilience Scale90 and coping style with the Utrechtse Coping Lijst.91 Furthermore, physical activity levels will be tracked with an accelerometer, the ActiCal (Respironics, Bend, Oregon, USA), during the first 2 weeks of the second diary period. Output of this instrument will be presented as Energy Expenditure and Metabolic Equivalent of Task. The physical activity measurements are added to serve as a pilot study and are not obligatory.
At baseline, sleep habits will be assessed with the Munich Chronotype Questionnaire92 to optimise the diary assessment process. Also, potential confounders such as smoking, alcohol/drug consumption, socioeconomic status and body mass index will be registered by means of a general health questionnaire. In addition, stressful life events will be assessed, using the list of threatening experiences.93 Finally, pertaining to subgroup 4 only, social cognition will be assessed using the Faux Pas Task,94 and bonding with parents will be assessed with the Inventory of Parent and Peer Attachment.95 96 These factors may be of importance in determining a transition from an UHR status to psychosis.
Data analysis plan
To map individual symptom networks of day-to-day symptom levels, multivariate time-series analysis will be employed on each individual’s time series data. Specifically, vector autoregression (VAR) models will be applied.97 These models are particularly suited for investigating the temporal dynamics between two or more variables. The resulting associations between symptoms will subsequently be presented as networks, and network parameters will be estimated. These include (but are not limited to) the strength and directionality of symptom connections (see figure 1) and centrality indices (information about the position of a symptom in the network). Next, symptom networks will be compared (1) across different subgroups of severity and (2) when the second diary period is completed, within each individual.
In addition, a data-driven approach will be used to identify individuals with similar symptom network characteristics by (1) qualitative network comparison, (2) quantitative comparison of centrality indices98 99 and (3) longitudinal mixture models.100 These subgroups will then be compared on their levels of symptomatology and functioning and on course of symptomatology over time. Furthermore, the predictive value of the network parameters will be compared with the predictive value of usual predictors of illness course, namely cross-sectionally assessed level of (subclinical) psychotic pathology. Specifically, sensitivity and specificity of these network characteristics can be compared with sensitivity and specificity of baseline subclinical levels of psychotic symptoms (CAPE) and general psychopathology (SCL-90). Finally, risk and resilience factors, such as stressful events, social interactions, physical activity, coping and resilience, may also influence symptoms and, importantly, their dynamics in the network but may do so differently in individuals with good or poor clinical and functional outcome. The role of these factors will be addressed by including them in individual network analyses to examine their direct and indirect impact on symptomatology and each other.
To control for potential confounding effects of demographic factors, such as sex, age and social economic status, these variables will be added as covariates to all group level analyses.
Based on previous work,101 102 we expect no more than 10% missing data. Missing values will be imputed with expectation-maximisation imputation, following special recommendations for time-series datasets.103 A (two-sided) P value of 0.05 is applied for statistical testing.
Sample size and power
Within-person analyses: constructing individual symptom networks
Exact sample size calculations are not possible in studies using VAR, as it is typically unclear in such studies what effect size can be expected. This is because the direction of causality and the number of lagged influences in the system under investigation are usually unknown, and bidirectional and feedback effects can be present as well.97 However, as previous work from our group101 104 105 and work of others106 suggests, 60–90 measurements suffice to reliably identify reciprocal associations between multiple variables.
Between-person analyses: associating symptom networks to clinical stage
In the between-person analyses, the data have a multilevel structure. Therefore, the unilevel equivalent of the multilevel sample size107 was taken to calculate the power, assuming a conservative intraclass correlation of 0.8. Assuming differences of 0.05 in mean coefficients (SD=0.07) between the different groups,24 the proposed study has a power of 0.8 (to detect significant differences at P<0.05). Subgroups of n=25 are large enough to take into account effects of several covariates.108
Ethics and dissemination
The study will be conducted in accordance with the Declaration of Helsinki, meaning that participation is voluntary and written informed consent will be obtained. Several protocols have been developed for situations where clinical care may be warranted, for example, in case of disclosure of suicidal thoughts or in case of UHR status in one of the lower risk groups.
An online outcome monitoring system, called RoQua (www.roqua.nl) is used for data collection and data storage, to which only designated researchers have access via the use of passwords combined with Google authentication. Participants have access to the questionnaires via a link in their email inbox. The safety of this system is guaranteed by the University Medical Center Groningen (UMCG) (an ‘In Control Statement‘ is available on request). Data management is also organised according to UMCG standards, including a strict separation of identifying patient data (name, date of birth and so on) and the anonymous datasets available for the researchers.
Data gathering was not completed when this manuscript was submitted. After the study has ended and the study’s main results have been published, the data obtained by this study will become available on reasonable request. Requests should be sent to j.t.w.wigman@umcg.nl with the topic name MIRORR data. The results of the study will be published in (inter)national peer-reviewed journals, presented at research, clinical and general public conferences.
Discussion
Current diagnostic systems are increasingly criticised by mental health professionals, researchers and users of mental healthcare.9 12 26 109 Conceptualisation of psychopathology in terms of (1) clinical staging (at macro level) and (2) dynamic, individual symptom networks (at a more micro level), which is the purpose of this study, represents a promising avenue to tackle both scientific and clinical problems. From a scientific perspective, improving our understanding of the factors driving the development of psychopathology by investigating how symptoms influence each other will enhance our ability to identify valid phenotypes to predict onset of (psychotic) mental disorders and to link with other relevant information (eg, genetic or endophenotypic variation). From a clinical perspective, a better understanding of why psychotic symptoms can lead to a need for care in some, but resolve spontaneously in others, will help mental health professionals to adequately recognise the early needs of individuals who are likely to develop mental illness or functional impairments. This is important because interventions are both more effective and less invasive when applied early in the course of illness.22 In more progressive clinical stages, deeper knowledge of the dynamic ways symptoms impact on each other will help to differentiate between those likely to recover or to deteriorate and between those likely to be responsive or resistant to treatment. Using symptom networks will improve the application of individually tailored, person-based interventions, adapted to one’s current clinical stage and symptomatology, as different stages require different types of intervention. Since personalised interventions better fit individual needs, they will result in enhanced treatment response,110 reducing the costs of mental disorders at both personal and societal level. Thus, the use of symptom networks will assist in improving and fine-tuning dynamic models of psychopathology, which will stimulate both clinical (in terms of both diagnostics and intervention) and scientific progress.
Supplementary Material
Acknowledgments
We would like to thank the ROQUA team for their collaboration and for building and maintaining the smartphone web-based (diary) questionnaires. We are grateful to Laura Steenhuis, Roos Willemsen, Marike Fowler, Cornelie Glasbergen, Marijke Muller, Eliese van Deelen, Marion van Dijk, Sieberen Veenstra, Marietta Khachaturyan and Thirza Osinga for their contributions to the field work and data management. We thank Ernst Wit and Elske Bos for their conceptual and methodological input. Finally, we thank Rob Wanders and Ando Emerencia for their help with automating the personalised feedback procedure.
Footnotes
Contributors: JTWW conceived the study. JTWW and SHB designed and are executing the study and drafted the first versions of the manuscript. LW, PdJ, JvO and MCW helped conceptualise the study and provided general advice and input. SS contributed to the study design, specifically to the data gathering and data management part. All authors critically reviewed the manuscript and collaborated in the discussion of the intellectual content of the manuscript. All authors read and approved the final manuscript.
Funding: This work was supported by the Netherlands Organization for Scientific Research (NWO) (Veni JTWW: no. 016.156.019). In addition, MCW was supported by an H2020 European Research Council Consolidator Grant (ERC-CoG-2015, project 681466 – TRANS-ID).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethics Committee of the University Medical Centre Groningen (ABR no. NL52974.042.15).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.van Os J, Kapur S. Schizophrenia. The Lancet 2009;374:635–45. 10.1016/S0140-6736(09)60995-8 [DOI] [PubMed] [Google Scholar]
- 2.Eaton WW, Martins SS, Nestadt G, et al. . The burden of mental disorders. Epidemiol Rev 2008;30:1–14. 10.1093/epirev/mxn011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCrone PR, Dhanasiri S, Patel A, et al. . Paying the price: the cost of mental health care in England to 2026: King’s Fund, 2008. [Google Scholar]
- 4.Volksgezondheid NK. Psychisch functioneren: Zijn er verschillen tussen Nederland en andere landen? Preventie gericht op psychisch functioneren van jeugd. [Google Scholar]
- 5.van Os J, Linscott RJ, Myin-Germeys I, et al. . A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 2009;39:179–95. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- 6.Wigman JT, van Nierop M, Vollebergh WA, et al. . Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity-implications for diagnosis and ultra-high risk research. Schizophr Bull 2012;38:247–57. 10.1093/schbul/sbr196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wigman JT, van Os J, Abidi L, et al. . Subclinical psychotic experiences and bipolar spectrum features in depression: association with outcome of psychotherapy. Psychol Med 2014;44:325–36. 10.1017/S0033291713000871 [DOI] [PubMed] [Google Scholar]
- 8.Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 2003;160:4–12. 10.1176/appi.ajp.160.1.4 [DOI] [PubMed] [Google Scholar]
- 9.Widiger TA. A dimensional model of psychopathology. Psychopathology 2005;38:211–4. 10.1159/000086094 [DOI] [PubMed] [Google Scholar]
- 10.Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the diagnostic and statistical manual of mental disorders–fifth edition. J Abnorm Psychol 2005;114:494–504. 10.1037/0021-843X.114.4.494 [DOI] [PubMed] [Google Scholar]
- 11.Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychol Med 2011;41:1143–50. 10.1017/S0033291710001844 [DOI] [PubMed] [Google Scholar]
- 12.Kupfer DJ, First MB, Regier DA. A research agenda for DSM V: American psychiatric pub, 2008. [Google Scholar]
- 13.Hickie IB, Scott J, McGorry PD. Clinical staging for mental disorders: a new development in diagnostic practice in mental health. Med J Aust 2013;198:461–2. 10.5694/mja13.10431 [DOI] [PubMed] [Google Scholar]
- 14.Strauss JS. Hallucinations and delusions as points on continua function. Rating scale evidence. Arch Gen Psychiatry 1969;21:581–6. [DOI] [PubMed] [Google Scholar]
- 15.Haslam N, Holland E, Kuppens P. Categories versus dimensions in personality and psychopathology: a quantitative review of taxometric research. Psychol Med 2012;42:903–20. 10.1017/S0033291711001966 [DOI] [PubMed] [Google Scholar]
- 16.Kendler KS, Gardner CO. Boundaries of major depression: an evaluation of DSM-IV criteria. Am J Psychiatry 1998;155:172-7 10.1176/ajp.155.2.172 [DOI] [PubMed] [Google Scholar]
- 17.Angst J, Gamma A, Benazzi F, et al. . Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J Affect Disord 2003;73:133–46. 10.1016/S0165-0327(02)00322-1 [DOI] [PubMed] [Google Scholar]
- 18.Carter RM, Wittchen HU, Pfister H, et al. . One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety 2001;13:78–88. 10.1002/da.1020 [DOI] [PubMed] [Google Scholar]
- 19.Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behav Res Ther 2002;40:485–99. 10.1016/S0005-7967(02)00016-5 [DOI] [PubMed] [Google Scholar]
- 20.Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci 2008;9:947–57. 10.1038/nrn2513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Berglund P, Demler O, et al. . Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005;62:593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 22.McGorry PD, Hickie IB, Yung AR, et al. . Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry 2006;40:616–22. 10.1080/j.1440-1614.2006.01860.x [DOI] [PubMed] [Google Scholar]
- 23.McGorry PD. Issues for DSM-V: clinical staging: a heuristic pathway to valid nosology and safer, more effective treatment in psychiatry. Am J Psychiatry 2007;164:859–60. 10.1176/ajp.2007.164.6.859 [DOI] [PubMed] [Google Scholar]
- 24.Wigman JT, van Os J, Thiery E, et al. . Psychiatric diagnosis revisited: towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS One 2013;8:e59559 10.1371/journal.pone.0059559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGorry P, van Os J. Redeeming diagnosis in psychiatry: timing versus specificity. Lancet 2013;381:343–5. 10.1016/S0140-6736(12)61268-9 [DOI] [PubMed] [Google Scholar]
- 26.Hyman SE. The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol 2010;6:155–79. 10.1146/annurev.clinpsy.3.022806.091532 [DOI] [PubMed] [Google Scholar]
- 27.McGorry PD, Killackey E, Yung AR. Early intervention in psychotic disorders: detection and treatment of the first episode and the critical early stages. Med J Aust 2007;187:S8–10. [DOI] [PubMed] [Google Scholar]
- 28.Fusar-Poli P, Bonoldi I, Yung AR, et al. . Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry 2012;69:220–9. 10.1001/archgenpsychiatry.2011.1472 [DOI] [PubMed] [Google Scholar]
- 29.McGorry P, Keshavan M, Goldstone S, et al. . Biomarkers and clinical staging in psychiatry. World Psychiatry 2014;13:211–23. 10.1002/wps.20144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wood SJ, Yung AR, McGorry PD, et al. . Neuroimaging and treatment evidence for clinical staging in psychotic disorders: from the at-risk mental state to chronic schizophrenia. Biol Psychiatry 2011;70:619–25. 10.1016/j.biopsych.2011.05.034 [DOI] [PubMed] [Google Scholar]
- 31.Scott J, Leboyer M, Hickie I, et al. . Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry 2013;202:243–5. 10.1192/bjp.bp.112.110858 [DOI] [PubMed] [Google Scholar]
- 32.Keshavan MS, DeLisi LE, Seidman LJ. Early and broadly defined psychosis risk mental states. Schizophr Res 2011;126:1–10. 10.1016/j.schres.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fusar-Poli P, Yung AR, McGorry P, et al. . Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med 2014;44:17–24. 10.1017/S0033291713000184 [DOI] [PubMed] [Google Scholar]
- 34.Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res 2009;110:1–23. 10.1016/j.schres.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 35.Lin A, Nelson B, Yung AR. ‘At-risk’ for psychosis research: where are we heading? Epidemiol Psychiatr Sci 2012;21:329–34. 10.1017/S2045796012000388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Os J. The dynamics of subthreshold psychopathology: implications for diagnosis and treatment. Am J Psychiatry 2013;170:695–8. 10.1176/appi.ajp.2013.13040474 [DOI] [PubMed] [Google Scholar]
- 37.Kaymaz N, Drukker M, Lieb R, et al. . Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med 2012;42:2239–53. 10.1017/S0033291711002911 [DOI] [PubMed] [Google Scholar]
- 38.Velthorst E, Nieman DH, Klaassen RM, et al. . Three-year course of clinical symptomatology in young people at ultra high risk for transition to psychosis. Acta Psychiatr Scand 2011;123:36–42. 10.1111/j.1600-0447.2010.01593.x [DOI] [PubMed] [Google Scholar]
- 39.Zammit S, Kounali D, Cannon M, et al. . Psychotic experiences and psychotic disorders at age 18 in relation to psychotic experiences at age 12 in a longitudinal population-based cohort study. Am J Psychiatry 2013;170:742–50. 10.1176/appi.ajp.2013.12060768 [DOI] [PubMed] [Google Scholar]
- 40.Kelleher I, Keeley H, Corcoran P, et al. . Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry 2012;201:26–32. 10.1192/bjp.bp.111.101543 [DOI] [PubMed] [Google Scholar]
- 41.van Rossum I, Dominguez MD, Lieb R, et al. . Affective dysregulation and reality distortion: a 10-year prospective study of their association and clinical relevance. Schizophr Bull 2011;37:561–71. 10.1093/schbul/sbp101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wigman JT, Lin A, Vollebergh WA, et al. . Subclinical psychosis and depression: co-occurring phenomena that do not predict each other over time. Schizophr Res 2011;130:277–81. 10.1016/j.schres.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 43.Werbeloff N, Drukker M, Dohrenwend BP, et al. . Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry 2012;69:467–75. 10.1001/archgenpsychiatry.2011.1580 [DOI] [PubMed] [Google Scholar]
- 44.Addington J, Cornblatt BA, Cadenhead KS, et al. . At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry 2011;168:800–5. 10.1176/appi.ajp.2011.10081191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yung AR, Phillips LJ, Yuen HP, et al. . Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr Res 2003;60:21–32. 10.1016/S0920-9964(02)00167-6 [DOI] [PubMed] [Google Scholar]
- 46.Yung AR, Phillips LJ, Yuen HP, et al. . Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res 2004;67:131–42. 10.1016/S0920-9964(03)00192-0 [DOI] [PubMed] [Google Scholar]
- 47.Demjaha A, Valmaggia L, Stahl D, et al. . Disorganization/cognitive and negative symptom dimensions in the at-risk mental state predict subsequent transition to psychosis. Schizophr Bull 2012;38:351–9. 10.1093/schbul/sbq088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kessler RC, Birnbaum H, Demler O, et al. . The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry 2005;58:668–76. 10.1016/j.biopsych.2005.04.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Breetvelt EJ, Boks MP, Numans ME, et al. . Schizophrenia risk factors constitute general risk factors for psychiatric symptoms in the population. Schizophr Res 2010;120:184–90. 10.1016/j.schres.2010.03.033 [DOI] [PubMed] [Google Scholar]
- 50.Weiser M, van Os J, Davidson M. Time for a shift in focus in schizophrenia: from narrow phenotypes to broad endophenotypes. Br J Psychiatry 2005;187:203–5. 10.1192/bjp.187.3.203 [DOI] [PubMed] [Google Scholar]
- 51.Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull 2009;35:482–90. 10.1093/schbul/sbp020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hill SK, Reilly JL, Harris MS, et al. . A comparison of neuropsychological dysfunction in first-episode psychosis patients with unipolar depression, bipolar disorder, and schizophrenia. Schizophr Res 2009;113:167–75. 10.1016/j.schres.2009.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bystritsky A, Nierenberg AA, Feusner JD, et al. . Computational non-linear dynamical psychiatry: a new methodological paradigm for diagnosis and course of illness. J Psychiatr Res 2012;46:428–35. 10.1016/j.jpsychires.2011.10.013 [DOI] [PubMed] [Google Scholar]
- 54.Strobl EV, Eack SM, Swaminathan V, et al. . Predicting the risk of psychosis onset: advances and prospects. Early Interv Psychiatry 2012;6:368–79. 10.1111/j.1751-7893.2012.00383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fusar-Poli P, Borgwardt S, Bechdolf A, et al. . The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry 2013;70:107–20. 10.1001/jamapsychiatry.2013.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nelson B, McGorry PD, Wichers M, et al. . Moving from static to dynamic models of the onset of mental disorder: a review. JAMA Psychiatry 2017;74:528–34. 10.1001/jamapsychiatry.2017.0001 [DOI] [PubMed] [Google Scholar]
- 57.Guloksuz S, Pries LK, van Os J. Application of network methods for understanding mental disorders: pitfalls and promise. Psychol Med 2017;47:2743–52. 10.1017/S0033291717001350 [DOI] [PubMed] [Google Scholar]
- 58.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 2013;9:91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 59.Borsboom D, Cramer AO, Schmittmann VD, et al. . The small world of psychopathology. PLoS One 2011;6:e27407 10.1371/journal.pone.0027407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature 2010;468:203–12. 10.1038/nature09563 [DOI] [PubMed] [Google Scholar]
- 61.Wigman J, Kelleher I, Devlin N, et al. . Coping as a moderating factor between psychotic symptoms and functioning in adolescents with mental illness. BMC Psychiatry 2013;22:S108–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roe D, Yanos PT, Lysaker PH. Coping with psychosis: an integrative developmental framework. J Nerv Ment Dis 2006;194:917–24. 10.1097/01.nmd.0000249108.61185.d3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yanos PT, Moos RH. Determinants of functioning and well-being among individuals with schizophrenia: an integrated model. Clin Psychol Rev 2007;27:58–77. 10.1016/j.cpr.2005.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barabási A, Frangos J. Linked: the new science of networks science of networks: Basic Books, 2014. [Google Scholar]
- 65.Barabási A. Bursts: the hidden patterns behind everything we do from your e-mail to bloody crusades: Penguin, 2010. [Google Scholar]
- 66.Schmittmann VD, Cramer AOJ, Waldorp LJ, et al. . Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol 2013;31:43–53. 10.1016/j.newideapsych.2011.02.007 [DOI] [Google Scholar]
- 67.Yung AR, Nelson B, Thompson A, et al. . The psychosis threshold in Ultra High Risk (prodromal) research: is it valid? Schizophr Res 2010;120:1–6. 10.1016/j.schres.2010.03.014 [DOI] [PubMed] [Google Scholar]
- 68.Oorschot M, Lataster T, Thewissen V, et al. . Symptomatic remission in psychosis and real-life functioning. Br J Psychiatry 2012;201:215–20. 10.1192/bjp.bp.111.104414 [DOI] [PubMed] [Google Scholar]
- 69.Verma S, Subramaniam M, Abdin E, et al. . Symptomatic and functional remission in patients with first-episode psychosis. Acta Psychiatr Scand 2012;126:282–9. 10.1111/j.1600-0447.2012.01883.x [DOI] [PubMed] [Google Scholar]
- 70.Wunderink L, Nieboer RM, Wiersma D, et al. . Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry 2013;70:913–20. 10.1001/jamapsychiatry.2013.19 [DOI] [PubMed] [Google Scholar]
- 71.Konings M, Bak M, Hanssen M, et al. . Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand 2006;114:55–61. 10.1111/j.1600-0447.2005.00741.x [DOI] [PubMed] [Google Scholar]
- 72.Ising HK, Veling W, Loewy RL, et al. . The validity of the 16-item version of the Prodromal Questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr Bull 2012;38:1288–96. 10.1093/schbul/sbs068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yung AR, Yuen HP, McGorry PD, et al. . Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry 2005;39:964–71. 10.1080/j.1440-1614.2005.01714.x [DOI] [PubMed] [Google Scholar]
- 74.Wigman JT, Vollebergh WA, Raaijmakers QA, et al. . The structure of the extended psychosis phenotype in early adolescence–a cross-sample replication. Schizophr Bull 2011;37:850–60. 10.1093/schbul/sbp154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Oorschot M, Kwapil T, Delespaul P, et al. . Momentary assessment research in psychosis. Psychol Assess 2009;21:498–505. 10.1037/a0017077 [DOI] [PubMed] [Google Scholar]
- 76.Myin-Germeys I, Marcelis M, Krabbendam L, et al. . Subtle fluctuations in psychotic phenomena as functional states of abnormal dopamine reactivity in individuals at risk. Biol Psychiatry 2005;58:105–10. 10.1016/j.biopsych.2005.02.012 [DOI] [PubMed] [Google Scholar]
- 77.Wigman JT, Collip D, Wichers M, et al. . Altered transfer of momentary mental states (ATOMS) as the basic unit of psychosis liability in interaction with environment and emotions. PLoS One 2013;8:e54653 10.1371/journal.pone.0054653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kroenke K, Spitzer RL, Williams JB. The Phq‐9. J Gen Intern Med 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 80. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub, 2013. [Google Scholar]
- 81.Yik M, Russell JA, Steiger JH. A 12-point circumplex structure of core affect. Emotion 2011;11:705–31. 10.1037/a0023980 [DOI] [PubMed] [Google Scholar]
- 82.Feldman Barrett L, Russell JA. Independence and bipolarity in the structure of current affect. J Pers Soc Psychol 1998;74:967–84. 10.1037/0022-3514.74.4.967 [DOI] [Google Scholar]
- 83.Derogatis LR, Unger R. Symptom checklist‐90‐revised, Corsini encyclopedia of psychology, 2010. [Google Scholar]
- 84.Nienhuis FJ, van de Willige G, Rijnders CA, et al. . Validity of a short clinical interview for psychiatric diagnosis: the mini-SCAN. Br J Psychiatry 2010;196:64–8. 10.1192/bjp.bp.109.066563 [DOI] [PubMed] [Google Scholar]
- 85.De Jong A, Lubbe PM. Groningse vragenlijst over sociaal gedrag: zelfbeoordelingsvragenlijsten voor het vaststellen van problemen in het interpersoonlijke functioneren. handleiding: Rob Giel Onderzoekcentrum, 2001. [Google Scholar]
- 86.Diener E, Wirtz D, Tov W, et al. . New well-being measures: short scales to assess flourishing and positive and negative feelings. Soc Indic Res 2010;97:143–56. 10.1007/s11205-009-9493-y [DOI] [Google Scholar]
- 87.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther 1995;33:335–43. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- 88.Altman EG, Hedeker D, Peterson JL, et al. . The altman self-rating mania scale. Biol Psychiatry 1997;42:948–55. 10.1016/S0006-3223(96)00548-3 [DOI] [PubMed] [Google Scholar]
- 89.van Sonderen E, Lijst–Interacties SS. SSL-I) en sociale steun lijst-discrepanties (SSL-D): noorderlijk centrum voor gezondheidsvraagstukken. Groningen, 1993. [Google Scholar]
- 90.Smith BW, Dalen J, Wiggins K, et al. . The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 91.Schreurs P, Van de Willige G. Omgaan met problemen en gebeurtenissen. De Utrechtse Coping Lijst (UCL)(Coping with problems and events. The Utrecht Coping List 1998. [Google Scholar]
- 92.Roenneberg T, Kuehnle T, Juda M, et al. . Epidemiology of the human circadian clock. Sleep Med Rev 2007;11:429–38. 10.1016/j.smrv.2007.07.005 [DOI] [PubMed] [Google Scholar]
- 93.Rosmalen JG, Bos EH, de Jonge P. Validation of the Long-term Difficulties Inventory (LDI) and the List of Threatening Experiences (LTE) as measures of stress in epidemiological population-based cohort studies. Psychol Med 2012;42:2599–608. 10.1017/S0033291712000608 [DOI] [PubMed] [Google Scholar]
- 94.Stone VE, Baron-Cohen S, Knight RT. Frontal lobe contributions to theory of mind. J Cogn Neurosci 1998;10:640–56. 10.1162/089892998562942 [DOI] [PubMed] [Google Scholar]
- 95.Armsden GC, Greenberg MT. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc 1987;16:427–54. 10.1007/BF02202939 [DOI] [PubMed] [Google Scholar]
- 96.Deković M, Noom MJ, Meeus W. Expectations regarding development during adolescence: Parental and adolescent perceptions. J Youth Adolesc 1997;26:253–72. 10.1007/s10964-005-0001-7 [DOI] [Google Scholar]
- 97.Brandt PT. Multiple time series models. Sage, 2007. [Google Scholar]
- 98.Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Networks 2010;32:245–51. 10.1016/j.socnet.2010.03.006 [DOI] [Google Scholar]
- 99.Epskamp S, Cramer A, Waldorp L, et al. . Qgraph: network representations of relationships in data, R package version 0.4, 2011:10. [Google Scholar]
- 100.Wit E, Abbruzzo A. Factorial graphical lasso for dynamic networks. arXivpreprint arXiv:1205.2911 2012. [Google Scholar]
- 101.van Gils A, Burton C, Bos EH, et al. . Individual variation in temporal relationships between stress and functional somatic symptoms. J Psychosom Res 2014;77:34–9. 10.1016/j.jpsychores.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 102.Bouwmans ME, Bos EH, Booij SH, et al. . Intra-and inter-individual variability of longitudinal daytime melatonin secretion patterns in depressed and non-depressed individuals. Chronobiol Int 2015;32:441–6. 10.3109/07420528.2014.973114 [DOI] [PubMed] [Google Scholar]
- 103.Honaker J, King G, Blackwell M. Amelia II: a program for missing data. J Stat Softw 2011;45 http://www.jstatsoft.org/v45/i07 10.18637/jss.v045.i07 [DOI] [Google Scholar]
- 104.Rosmalen JG, Wenting AM, Roest AM, et al. . Revealing causal heterogeneity using time series analysis of ambulatory assessments: application to the association between depression and physical activity after myocardial infarction. Psychosom Med 2012;74:377–86. 10.1097/PSY.0b013e3182545d47 [DOI] [PubMed] [Google Scholar]
- 105.Bos EH, Hoenders R, de Jonge P. Wind direction and mental health: a time-series analysis of weather influences in a patient with anxiety disorder. BMJ Case Rep 2012:bcr2012006300 10.1136/bcr-2012-006300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lütkepohl H. New introduction to multiple time series analysis, 2005. [Google Scholar]
- 107.Snijders TB, Bosker RR. Multilevel analysis: an introduction to basic and advanced multilevel modeling, 1999. [Google Scholar]
- 108.Hsu LM. Random sampling, randomization, and equivalence of contrasted groups in psychotherapy outcome research. J Consult Clin Psychol 1989;57:131–7. 10.1037/0022-006X.57.1.131 [DOI] [PubMed] [Google Scholar]
- 109.Insel T, Cuthbert B, Garvey M, et al. . Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 2010;167:748–51. 10.1176/appi.ajp.2010.09091379 [DOI] [PubMed] [Google Scholar]
- 110.Boertien D. Herstel en empowerment (recovery and empowerment) In: Veling W, Van der Wal M, Jansen S, eds Handboek vroege psychose (manual for early psychosis), 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019059supp001.pdf (87.2KB, pdf)