PRESENTATION
A 23-year-old male presented with a history of sudden onset painless diminution of vision in the left eye (LE) following bouts of vomiting 4 months ago. His vision had gradually improved over the previous 2 months. There was no history of steroid use. Visual acuity was 20/20 in both eyes. There was no intraocular inflammation. An oblique oval lesion measuring 5 × 4 disc diameters was observed at the posterior pole of the LE. On slit lamp biomicroscopy, it appeared to be an elevated neurosensory retina [Figure 1a]. There were no evident retinal vascular abnormalities or retinal neovascularization. The fundus fluorescein angiogram (FFA) showed subtle window defects at the lesion site, with blockage of fluorescence in the temporal and inferior margins [Figure 1b]. The areas of blocked fluorescence correlated with subtle preretinal brownish pigments [Figure 1a]. No leakage or pooling of dye consistent with central serous chorioretinopathy (CSCR) was evident. Spectral domain optical coherence tomography (SD-OCT, RS-3000, Nidek, Aichi, Japan) showed normal foveal depression with a detached internal limiting membrane (ILM) at and temporal to the fovea [Figure 2a]. The posterior hyaloid was detached at the posterior pole but attached to the optic disc [Figure 2a]. Another SD-OCT image captured along the smaller axis of the elevation showed a sub-ILM cavity [Figure 2b] and localized hyaloid separation [Figure 2b]. Complete blood cell count, blood pressure, and blood sugar levels were normal. A review of records showed that the patient had received a diagnosis of sub-hyaloid or sub-ILM bleed (Valsalva retinopathy) 3 months ago.
Figure 1.
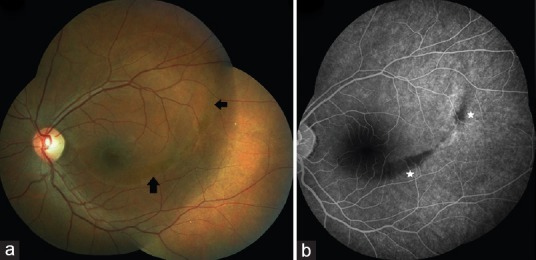
(a) The left eye showed an apparent oblique oval elevation of the neurosensory retina involving the fovea. Areas with subtle brownish pigment were observed along the inferior and temporal margin of the elevation (arrows). (b) Fundus fluorescein angiogram of the left eye revealed subtle window defects at the lesion-site with blockage of fluorescence corresponding to the pigment deposits (star). No leaks or pooling of dye was evident.
Figure 2.
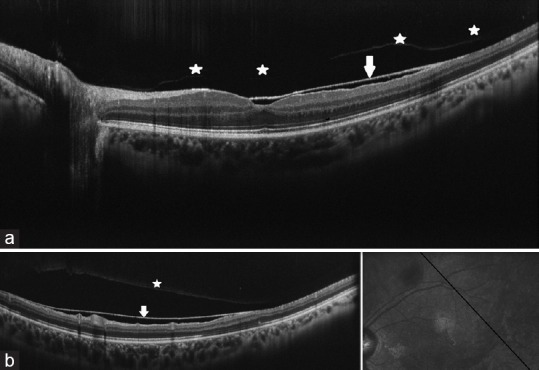
(a) Spectral domain optical coherence tomography (SD-OCT) showed normal foveal depression with a detached internal limiting membrane (ILM) at and temporal to the fovea in the left eye (arrow, Figure 2a). The posterior hyaloid was detached at the posterior pole but attached to the optic disc (stars, Figure 2a). (b) SD-OCT image through the smaller axis of the elevation showed localized separation of a sub-ILM cavity (arrow) and detached posterior hyaloid (star).
DISCUSSION
Valsalva retinopathy is characterized by unilateral loss of vision due to a sub-ILM bleed following episodes of vomiting, coughing, or Valsalva maneuver.[1] The bleed typically resolves after 3–4 months, or following Nd-YAG[2] or argon laser[3] membranotomy, leaving a sub-ILM cavity. Sub-ILM hemorrhage may also be caused by proliferative diabetic retinopathy, anemia, thrombocytopenia, leukemia, subarachnoid hemorrhage (Terson syndrome), hypertension, ruptured retinal artery macroaneurysm, trauma, or shaken baby syndrome.[1] Sub-ILM cavity or ILM detachment may also occur in vitreomacular traction, retinitis,[4] or may not have an identifiable cause.[5]
The exact level of the fluid at the posterior pole may be difficult to ascertain on slit lamp biomicroscopy. Fluid under the ILM forming a sub-ILM cavity may be confused with fluid under the neurosensory retina, which is observed in CSCR. However, the level of deposited pigments can be determined as preretinal, indicating preretinal pathology. OCT is diagnostic in such cases, and reveals the ILM separation, cavity formation, and absence of a neurosensory detachment. In this case, FFA did not reveal any leakage suggestive of CSCR.
Although clearing of blood from the fovea resulted in gradual visual recovery, a sub-ILM cavity formed. The clinical clues for the diagnosis of a resolving Valsalva retinopathy in this patient included a history of vomiting episodes at onset, an oval shaped lesion straddling the superotemporal arcade, and collection of preretinal brownish pigments at the margin of the cavity. Although CSCR and a sub-ILM cavity may appear similar on a cursory clinical examination, and both may resolve with time, detailed clinical examination, FFA, and SD-OCT can help differentiate the two entities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgments
We sincerely acknowledge the invaluable support and suggestions from Trina Sengupta Tripathy, without which the manuscript would have been incomplete.
REFERENCES
- 1.Tripathy K, Chawla R. Valsalva retinopathy. Natl Med J India. 2015;28:310. [PubMed] [Google Scholar]
- 2.Goel N, Kumar V, Seth A, Raina UK, Ghosh B. Spectral-domain optical coherence tomography following Nd:YAG laser membranotomy in valsalva retinopathy. Ophthalmic Surg Lasers Imaging. 2011;42:222–228. doi: 10.3928/15428877-20110224-01. [DOI] [PubMed] [Google Scholar]
- 3.Meyer CH, Mennel S, Rodrigues EB, Schmidt JC. Persistent premacular cavity after membranotomy in valsalva retinopathy evident by optical coherence tomography. Retina. 2006;26:116–118. doi: 10.1097/00006982-200601000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Chawla R, Tripathy K, Gogia V, Venkatesh P. Progressive outer retinal necrosis-like retinitis in immunocompetent hosts. BMJ Case Rep 2016. 2016 doi: 10.1136/bcr-2016-216581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H, Guo X, Tang L. Idiopathic Internal Limiting Membrane Detachment. Retina. 2015;35:378–379. doi: 10.1097/IAE.0000000000000240. [DOI] [PubMed] [Google Scholar]


