Abstract
Ibuprofen is widely used in the community to manage pain, inflammation and fever. In cases of prolonged and supratherapeutic ingestion of ibuprofen, renal tubular acidosis (RTA) with profound hypokalemia may occur. Although hypokalemia is known to cause rhabdomyolysis, rhabdomyolysis occurring in the setting of ibuprofen-induced RTA is rare. We present an unusual case of a 34-year-old male who presented with rhabdomyolysis in the setting of profound hypokalemia as a result of ibuprofen-induced RTA. The patient was successfully treated with fluid resuscitation, electrolyte replacement and supportive therapy. This case demonstrates a serious complication of ibuprofen and the importance of monitoring in nonprescription medications.
INTRODUCTION
Ibuprofen is an over-the-counter medication that is widely used due to its anti-inflammatory, antipyretic and analgesic effects. Because it is easily available without prescription, it can commonly cause toxicity in cases of misuse. Nonsteroid anti-inflammatory drugs (NSAIDs) may cause acute kidney injury, interstitial nephritis and nephrotic syndrome. Profound, life-threatening hypokalemia may rarely develop as a result of renal tubular acidosis (RTA) [1].
Rhabdomyolysis is a syndrome characterized by breakdown of skeletal muscle cells. Rhabdomyolysis secondary to hypokalemia has previously been described [2]; however, its occurrence as a result of ibuprofen-induced RTA and hypokalemia is rare. We present a case of a 34-year-old man who presented with ibuprofen-induced RTA and profound hypokalemia, which resulted in rhabdomyolysis. From our experience, we hope to add to the literature a potentially dangerous side effect of ibuprofen, particularly in patients with prolonged unmonitored use of this common nonprescription medication.
CASE REPORT
A 34-year-old male presented with 4-day history of evolving generalized weakness and myalgia. He had a past history of chronic severe migraines and was taking an over-the-counter ibuprofen–codeine combination for the past 14 years, with a daily dose of up to 60 tablets (12.0 g ibuprofen). He denied a history of diarrhea, vomiting, trauma, seizures, prolonged exercise, alcohol or other substance abuse. Neurological examination revealed weakness in upper and lower limbs bilaterally and symmetrically (Medical Research Council Grade 4/5) with hyporeflexia. Sensation was intact.
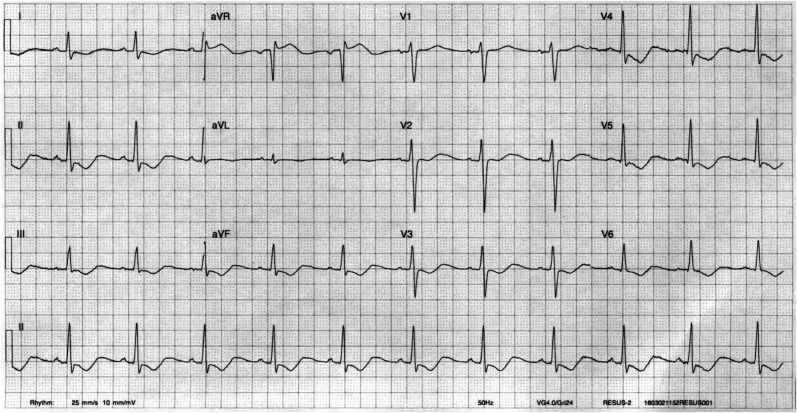
Initial biochemistry showed a serum potassium level of 2.0 mmol/l (reference range, 3.5–5.0 mmol/l). An ECG showed widespread ST depression, T wave inversion, prominent U waves and ST elevation in lead aVR, consistent with hypokalemia (Fig. 1). His venous blood gas revealed a mild metabolic acidosis with pH 7.37 (RR, 7.38–7.43), a bicarbonate level of 19 mmol/l (RR, 22–26 mmol/l) and an anion gap of 12 mmol/l. His urine biochemistry showed urinary potassium wasting with a potassium concentration of 31 mmol/l and a urine potassium–creatinine ratio of 2.6 (Table 1), which was suggestive of RTA.
Figure 1:
ECG on presentation shows widespread ST depression, T wave inversion, ST elevation in aVR and prominent U waves, consistent with hypokalemia.
Table 1:
Initial laboratory investigations on admission
| Laboratory value | Reference range | |
|---|---|---|
| Serum | ||
| Hb, g/dl | 8.6 | 13.0–18.0 |
| MCV, fl | 63 | 80–96 |
| pH | 7.37 | 7.38–7.43 |
| PCO2, mmHg | 33 | 35–45 |
| HCO3−, mmol/l | 19 | 22–26 |
| Na+, mmol/l | 142 | 136–142 |
| K+, mmol/l | 2.1 | 3.8–5.0 |
| Cl−, mmol/l | 113 | 95–110 |
| Urea, mmol/l | 5.6 | 2.3–7.6 |
| Creatinine, µmol/l | 96 | 60–110 |
| Albumin, g/l | 37 | 38–50 |
| Fe, µmol/l | 3 | 10–30 |
| Ferritin, ng/l | 76 | 20–300 |
| Transferrin, g/l | 2.5 | 2.2–2.7 |
| Transferrin saturation | 5 | 13–47 |
| Urine | ||
| K+, mmol/l | 31 | |
| Na+, mmol/l | 22 | |
| Cl−, mmol/l | 68 | |
| Creatinine, mmol/l | 11.9 | |
| pH | 6.5 | 5.0–7.0 |
| Myoglobin, mg/l | 182.0 | |
| Protein/creatinine ratio, mg/mmol | 243 | |
His full blood examination and iron studies revealed iron deficiency anemia, which is consistent with ibuprofen gastrointestinal toxicity. Further investigations confirmed the diagnosis of rhabdomyolysis with a serum creatinine kinase level of 19 689 units/l (RR, 0–250 units/l) with evidence of myoglobin in the urine. However, there was no evidence of an acute kidney injury.
Despite 132 mmol potassium replacement, he remained profoundly hypokalemic and was admitted to the intensive care unit for intravenous potassium replacement. He subsequently received a further 820 mmol of potassium, which incremented his potassium to 3.9 mmol/l. Intravenous fluids were administered for the management of rhabdomyolysis. A buprenorphine patch was started for opioid withdrawal symptoms. His weakness resolved with the resolution of the hypokalemia. The patient was discharged from the intensive care unit on Day 3 of his admission. His potassium was 4.0 mmol/l and his ECG normalized. A follow-up blood test 4 days post discharge from intensive care unit showed normal renal function with a potassium level of 4.1 mmol/l and a serum creatinine kinase level of 1819 units/l.
DISCUSSION
RTA associated with ibuprofen has been described in the literature [1, 3]. Although the mechanism of ibuprofen-induced RTA is poorly understood, it is thought to be due to inhibition of carbonic anhydrase (CA) [4]. CA is an enzyme that catalyzes the reversible hydration of carbon dioxide-to-bicarbonate and H+. It is present in both the proximal and distal tubules and is required for the acidification of urine [5]. Ibuprofen may cause both proximal and distal RTA [1]. The absence or inhibition of CA is associated with metabolic acidosis, which is observed in congenital CA deficiency [6]. RTA tends to occur in patients who had prolonged supratherapeutic doses of ibuprofen; however, RTA in patients taking therapeutic doses has been reported [1].
RTA is characterized by defects in the resorption of bicarbonate, excretion of hydrogen iron, or both, causing metabolic acidosis. Distal (type 1) RTA is caused by impaired acidification of urine in the distal nephron despite systemic acidemia. Proximal (type 2) RTA is a result of impaired bicarbonate resorption in the proximal nephron. In both conditions, hypokalemia occurs due to renal potassium wasting [7]. In our patient, the diagnosis of RTA was confirmed in the presence of a normal anion gap metabolic acidosis and kaluriesis despite profound hypokalemia. In addition, the presence of mild metabolic acidosis and negative urinary anion gap is suggestive of proximal RTA. While urinary anion gap is consistently positive in distal RTA, proximal RTA can present with negative urinary anion gap [8].
Association between hypokalemia and rhabdomyolysis has been described previously. The mechanism by which hypokalemia causes rhabdomyolysis is thought to be related to its role in the regulation of muscle blood flow. During muscle activity, there is an increase in potassium in the muscle, which facilitates vasodilatation and increased blood flow [9]. Therefore, in hypokalemia, blood supply to muscles is impaired due to vasoconstriction, causing muscle hypoxia and necrosis [9].
Treatment of rhabdomyolysis includes fluid resuscitation, prevention of end-organ damage and correction of electrolytes [10]. There may be a role for alkalinization of the urine with sodium bicarbonate; however, this may have worsened the hypokalemia in this case. In cases of ibuprofen-induced rhabdomyolysis, the causative agent needs to be ceased.
Combined analgesics with an opioid component are easily accessible over the counter in many countries. Multiple previous studies have reported toxicity caused by ibuprofen–codeine combination misuse [1, 3]. This is likely due to the fact that ibuprofen is one of the few NSAIDs that are available as a nonprescription combination medication with an opioid. As seen in this case, opiate addiction may result in excessive intake of combined analgesic medications, leading to toxicity from the nonopioid component.
This case demonstrates a rare occurrence of rhabdomyolysis in a patient presenting with ibuprofen-induced RTA and hypokalemia. Although rhabdomyolysis is a rare complication of ibuprofen, clinicians need to be aware of this complication as kidney injury may be preventable with treatment. This case also highlights the importance of medication monitoring, particularly nonprescription medications which are easily accessible by the public.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
There is no source of funding for this study.
ETHICAL APPROVAL
There is no ethical approval required for this study.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
GUARANTOR
M.H.D. is the guarantor for this study.
REFERENCES
- 1.Ng JL, Morgan DJ, Loh NK, Gan SK, Coleman PL, Ong GS, et al. Life-threatening hypokalaemia associated with ibuprofen-induced renal tubular acidosis. Med J Aust 2011;194:313–6. [DOI] [PubMed] [Google Scholar]
- 2.Wen Z, Chuanwei L, Chunyu Z, Hui H, Weimin L. Rhabdomyolysis presenting with severe hypokalemia in hypertensive patients: a case series. BMC Res Notes 2013;6:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lambert AP, Close C. Life-threatening hypokalaemia from abuse of Nurofen Plus. J R Soc Med 2005;98:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salter MD. Ibuprofen-induced hypokalemia and distal renal tubular acidosis: a patient's perceptions of over-the-counter medications and their adverse effects. Case Rep Crit Care 2013;2013:875857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Purkerson JM, Schwartz GJ. The role of carbonic anhydrases in renal physiology. Kidney Int 2007;71:103–15. [DOI] [PubMed] [Google Scholar]
- 6.Sly WS, Hewett-Emmett D, Whyte MP, Yu YS, Tashian RE. Carbonic anhydrase II deficiency identified as the primary defect in the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification. Proc Natl Acad Sci USA 1983;80:2752–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sebastian A, McSherry E, Morris RC., Jr Renal potassium wasting in renal tubular acidosis (RTA): its occurrence in types 1 and 2 RTA despite sustained correction of systemic acidosis. J Clin Invest 1971;50:667–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haque SK, Ariceta G, Batlle D. Proximal renal tubular acidosis: a not so rare disorder of multiple etiologies. Nephrol Dial Transplant 2012;27:4273–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knochel JP, Schlein EM. On the mechanism of rhabdomyolysis in potassium depletion. J Clin Invest 1972;51:1750–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sauret JM, Marinides G, Wang GK. Rhabdomyolysis. Am Fam Physician 2002;65:907–12. [PubMed] [Google Scholar]