Abstract
Objective
To determine the prevalence of Vidian canal types and dehiscence of the bony roof of the canal.
Methods
This study included 594 patients (391 males and 203 females; average age, 32.43±11.98 years; range, 18–65 years). Computed tomography (CT) images were analyzed in terms of the prevalence of Vidian canal types and dehiscence of the bony roof of the canal.
Results
Vidian canal types 1, 2, and 3 based on the sphenoid sinus body were found on the right side in 33.8%, 29.7%, and 6.5%, and on the left side in 36.4%, 27.4%, and 36.2% of the patients, respectively. Dehiscence of the bony roof of the canal was found on the right side in 22.2% of the patients and on the left side in 26.6%. In terms of Vidian canal types based on the sphenoid sinus floor, types 1, 2, 3, and 4 were found on the right side in 53.5%, 27.4%, 7.6%, and 11.5%, and on the left side in 54.9%, 26.6%, 6.6%, and 11.9% of the patients, respectively. On the right side, Vidian canal type 2 was significantly (p=0.002) more frequent in males than in females.
Conclusion
When studying the complex anatomy of the sphenoid sinus, it is essential to consider Vidian canal types. Before endoscopic sinus surgery the Vidian canal and other anatomical structures should be carefully evaluated in all patients during preoperative paranasal sinus CT imaging to avoid complications.
Keywords: Sphenoid sinus, Vidian canal, dehiscence
Introduction
The use of endoscopy in the otorhinolaryngology began with the examination of the nasal cavity in 1901 by Hirschmann using a cystoscope (1, 2). Endoscopic sinus surgery has been increasingly used in the field of rhinology due to reasons such as minimal invasiveness and low complication rate compared to open surgery. Endoscopic sinus surgery continued to develop with the contributions of researchers such as Draft, Grunberg, Messerklinger, Bauer, and Wodak (3, 4).
The developments in endoscopic sinus surgery have made it necessary to know the variations of paranasal sinuses and nasal anatomical formations. Knowing the anatomical variations is important not only for reduction in the complications of endoscopic sinus surgery but also for surgical correction and elimination of the variations that are thought to cause pathology in the paranasal sinuses (5, 6). The best way to avoid complications of sinus surgery is to have full knowledge of the paranasal sinus anatomy. The most useful method for this is the radiological examinations (6, 7). Detailed anatomic information can be obtained preoperatively through computerized tomography (CT) and the surgeon can use CT findings as a surgical map during surgery. For this reason, the evaluation of anatomy and variations through CT in the preoperative period is important for protection from complications (8, 9).
Among the paranasal sinuses, the sphenoid sinus is the most difficult one to reach (10). There are vital anatomical structures around it such as the internal carotid artery, optic nerve, and Vidian canal. Physicians dealing with skull base surgery have to know the important anatomical structures in the skull base. Complications are inevitable in surgical procedures performed with insufficient anatomical knowledge (11, 12). There are very few studies investigating the relationship between the Vidian canal and the sphenoid sinus. Like other anatomic formations around the sphenoid sinus, there are also variations in Vidian canal localization. Lee et al. (11) described four types of Vidian canals according to sphenoid sinus base and three types according to the sphenoid corpus.
In this study, the frequency of Vidian canal types according to the typing defined by Lee et al. (11) and the frequency of dehiscence seen in the bony roof of the Vidian canal were investigated in patients who applied to our clinic complaining nasal trauma and whose paranasal sinus CT was taken.
Methods
This retrospective study was carried out between January 2013 and March 2016 with a total of 594 outpatients aged 18 years and older who had been referred to the otorhinolaryngology, head and neck surgery clinic of our hospital and who underwent paranasal sinus CT due to nasal trauma. Patients who had previously undergone surgery for paranasal sinuses, who had massive nasal polyposis, nasal cavities, and paranasal sinus neoplasms, and who were younger than 18 years were excluded from the study. The study was conducted in accordance with the Helsinki Declaration and Good Clinical Practice Guidelines. Approval for the study was received from the Ethics committee of the same hospital (Ethics Committee No: 2016-195).
Demographic information of all cases was obtained by scanning the files in the hospital registry system. A CT device having multidetector feature (Siemens Sensation 40, Erlangen, Germany) was used for CT examinations. The images were evaluated with a dose of 120 kV/220 mA, with a minimum of 150–400 sections, with a thickness of 0.5 mm and with a scan area of 21.8’28.8 cm2. The shots were taken without contrast material and in the bone algorithm. Coronal and sagittal CT sections were used in the examination. The images were evaluated with the Mediplus Dicom Viewer System (Mediplus Ltd., High Wycombe, UK). The shootings were made while the patient was in the prone position with the head in hyperextension. The presence of dehiscence was investigated in Vidian canal types and in Vidian canal bony roof through CT. The classification made by Lee et al. (11) was used in typing the relationship between the Vidian canal and the sphenoid sinus. According to the relationship between sphenoid bone corpus and Vidian canal, three types were identified:
Type 1: The Vidian canal is completely embedded in the sphenoid sinus.
Type 2: The Vidian canal is partially embedded in the sphenoid sinus.
Type 3: The Vidian canal is completely embedded in the sphenoid corpus.
And according to the relationship between the sphenoid sinus floor and the Vidian canal, the following types were identified:
Type 1: The sphenoid sinus floor is flat and is the same level as the Vidian canal floor.
Type 2: The sphenoid sinus floor is inclined upward and the Vidian canal is above the floor.
Type 3: The sphenoid sinus floor is inclined downward and the Vidian canal is above the floor.
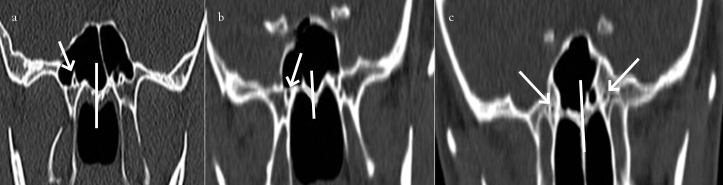
Type 4: The sphenoid sinus floor has an inverted “v” shape and the Vidian canal is below the floor (Figure 1a–c).
Figure 1. a–c.
The images of the Vidian canal (VC) according to the sphenoid sinus floor and corpus in CT coronal sections. (a) Type 1 VC on the right side according to the sphenoid corpus (arrow) and type 2 VC on the left side according to the sphenoid corpus. (b) Type 2 VC according to the sphenoid corpus (arrow), type 3 VC on the right side according to the sphenoid sinus floor, and type 4 VC on the left side. (c) Type 3 VC on the right side according to the sphenoid corpus, type 1 VC on the right side according to the sphenoid sinus floor, and type 2 VC on the left side
While the Vidian canal types and the presence of dehiscence Vidian canal bone roof were examined, the right and left sides were assessed separately.
Statistical analysis
Number Cruncher Statistical System (NCSS) 2007 (Kaysville, Utah, USA) was used for statistical analysis. While the data were evaluated, in addition to descriptive statistical methods (mean, standard deviation, median, frequency, and proportion), Mann-Whitney U test was used in the statistical evaluations of gender distributions. The results were evaluated in a confidence interval of 95% and a significance level of p<0.05.
Results
A total of 594 patients, 391 men (65.8%) and 203 women (34.2%), were included in the study. The age range was 18–65 years (mean age: 32.43±11.98 years). In the typing of sphenoid bone corpus and Vidian canal, while the frequency was 33.8% for type 1, 29.7% for type 2, and 36.5% for type 3 on the right side, it was 36.4% for type 1, 27.4% for type 2, and 36.2% for type 3 on the left side. The presence of dehiscence in the bony roof of Vidian canal was 22.2% on the right side and 26.6% on the left side (Table 1). According to the sphenoid bone corpus, there was no significant difference in the male and female gender distributions of Vidian canal types on both sides (Table 2, 3).
Table 1.
Distribution of Vidian canal types according to sphenoid corpus
| Type | Right side (594) | Left side (594) | Total (1.188) |
|---|---|---|---|
| Type 1 | 201 (33.8%) | 216 (36.4%) | 417 (35.1%) |
| Type 2 | 176 (29.7%) | 163 (27.4%) | 339 (28.5%) |
| Type 3 | 217 (36.5%) | 215 (36.2%) | 432 (36.4%) |
| Presence of dehiscence | 132 (22.2%) | 156 (26.6%) | 288 (24.2%) |
Table 2.
Distribution of Vidian canal types on the right side according to sphenoid corpus considering gender
| Type | Female | Male | p* |
|---|---|---|---|
| Type 1 | 64 (31.5%) | 126 (32.2%) | 0.322 |
| Type 2 | 65 (32.0%) | 112 (28.6%) | 0.098 |
| Type 3 | 74 (36.5%) | 153 (39.1%) | 0.252 |
| Total | 203 | 391 |
Mann-Whitney U test
Table 3.
Distribution of Vidian canal types on the left side according to sphenoid corpus considering gender
| Type | Female | Male | p* |
|---|---|---|---|
| Type 1 | 73 (36.0%) | 144 (36.8%) | 0.486 |
| Type 2 | 59 (29.1%) | 97 (24.8%) | 0.072 |
| Type 3 | 71 (34.9%) | 150 (38.4%) | 0.068 |
| Total | 203 | 391 |
Mann-Whitney U test
In the typing of Vidian canal according to sphenoid sinus floor, while the frequency was 53.5% for type 1, 27.4% for type 2, 7.6% for type 3, and 11.5% for type 4 on the right side, the same order for the right side was 54.9%, 26.6%, 6.6%, and 11.9%, respectively (Table 4). Type 2 Vidian canal was significantly higher in males than in females on the right side (p=0.002). There was no significant difference between male and female gender distributions on both sides in other Vidian canal types according to the sphenoid sinus floor (all p values >0.05) (Table 5, 6).
Table 4.
Distribution of Vidian canal types according to sphenoid sinus floor
| Type | Right side (594) | Left side (594) | Total (1.188) |
|---|---|---|---|
| Type 1 | 318 (53.5%) | 326 (54.9%) | 644 (54.2%) |
| Type 2 | 163 (27.4%) | 158 (26.6%) | 321 (27.1%) |
| Type 3 | 45 (7.6%) | 39 (6.6%) | 84 (7.0%) |
| Type 4 | 68 (11.5%) | 71 (11.9%) | 139 (11.7%) |
Table 5.
Distribution of Vidian canal types on the right side according to sphenoid sinus floor
| Type | Female (203) | Male (391) | p* |
|---|---|---|---|
| Type 1 | 104 (51.3%) | 214 (54.7%) | 0.214 |
| Type 2 | 43 (21.2%) | 120 (30.6%) | 0.002 |
| Type 3 | 18 (8.8%) | 27 (6.9%) | 0.166 |
| Type 4 | 38 (18.7%) | 30 (7.6%) | 0. 068 |
Mann-Whitney U test
Table 6.
Distribution of Vidian canal types on the left side according to sphenoid sinus floor
| Type | Female (203) | Male (391) | p* |
|---|---|---|---|
| Type 1 | 106 (52.2%) | 220 (56.3%) | 0.906 |
| Type 2 | 42 (20.7%) | 116 (29.7%) | 0.132 |
| Type 3 | 19 (9.4%) | 20 (5.1%) | 0.108 |
| Type 4 | 36 (17.7%) | 35 (8.9%) | 0. 076 |
Mann-Whitney U test
Discussion
The Vidian nerve, artery, and canal were described by the researcher Vidius in the middle of the 16th century (13). The Vidian nerve consists of the preganglionic parasympathetic fibers of the nervus petrosus major and postganglionic fibers of the deep petrosal nerve, and it enters the pterygopalatine fossa from behind the sphenopalatine ganglion (14, 15). The Vidian nerve is an important anatomical formation for foramen lacerum, mandibular nerve, foramen ovale, pterygopalatine fossa, and Eustachian tube. The Vidian nerve is located in the posteromedial of the lacerum segment of the internal carotid artery and in the caudal part of the lateral vertical segment in the anterolateral side of the pterygopalatine fossa (16). The Vidian canal ostium is located just below the foramen rotundum. Foramen lacerum is located in the superior and medial of the Vidian canal. Naturally, the Vidian canal is located in the inferolateral of the internal carotid artery. The internal carotid artery is bordered by the Vidian canal in the inferolateral and by the mandibular nerve in the superolateral portion (17). The Vidian canal is formed as a result of the pterygoid process and the emergence of the large wing of the sphenoid bone (18).
The anatomical and radiological features of the Vidian canal were demonstrated in previous studies, and its association with different anatomical structures was shown. Different variations related to the direction, configuration, and length of Vidian canal are reported. Vidian canal length is reported in the literature between 10 and 18 mm (19, 20).
Vidian canal localization is affected by neighboring anatomical formations. Kazkayasi et al. (10) reported in their study that Vidian canal protrusion was associated with pterygoid process pneumatization. Vidian canal is a reliable and important anatomical formation regardless of the degree of sphenoid sinus pneumatization.
The Vidian canal is an anatomical formation that can be quite helpful for the surgeon in the determination of lacerum segment of the internal carotid artery. Therefore, the determination step of the Vidian canal is very important for surgeons who will be performing skull base surgery (20).
Because of the associations of the Vidian canal with the sphenoid sinus, sphenoid sinus surgery is highly risky for the Vidian canal. Sphenoid sinus pneumatization can be at different degrees. As the sphenoid sinus pneumatization changes, the localization and size of the surrounding anatomic formations will change. Depending on the degree of pneumatization, it may be difficult to determine the anatomical formations around it. In this case, very serious complications may occur during operation. However, the iatrogenic injury of important adjacent formations is possible in all cases. In addition, variations of adjacent anatomic formations may cause chronic or recurrent sinusitis (20, 21).
Different variations between the Vidian canal and the sphenoid sinus may cause Vidian nerve to be affected in sinus diseases. The Vidian neuralgia described deep in the nasal cavity shows that the Vidian nerve is affected (17).
There are very few studies describing the relationship between the Vidian canal and the sphenoid sinus. Thus, the anatomic variations between the Vidian canal and the sphenoid sinus were not fully clarified. The location of the Vidian canal was determined by considering the sphenoid sinus floor and the sphenoid corpus in the study conducted by Lee et al. (11). Although not generally accepted, the classification system established by Lee et al. (11) is the most commonly used. The radiological study of Yazar et al. (5) evaluating the relationship between the localization of Vidian canal and sphenoid sinus revealed that the Vidian canal was embedded in the sphenoid corpus in 36% of the cases, partially penetrated into the sphenoid sinus in 54% of the cases, and it was connected to the sphenoid sinus with a bony prominence in 10% of the cases. Liu et al. (22) reported in their study that type 1 was 53.4%, type 2 was 34.2%, and type 3 was 12.5%. Mohebbi et al. (17) reported in the radiological study they performed that type 1 was 28%, type 2 was 48%, and type 3 was 24%. In this study, while type 1 was 33.8%, type 2 was 29.7%, and type 3 was 36.5% on the right side, type 1 was 36.4%, type 2 was 27.4%, and type 3 was 36.2% on the left side. There was no significant difference in the right- and left-side distributions of Vidian canal types. This finding is compatible with the results of previous anatomical studies in the literature. Unlike previous studies, it was shown in this study that there was no difference between female and male genders in the distribution of the types. Since the gender factor was ignored in previous studies, it became difficult to compare the results of this study. This feature adds a different value to the work.
There are very few studies evaluating the relationship between sphenoid sinus floor and Vidian canal. Liu et al. (22) reported that the frequency of Vidian canal localization according to the sphenoid sinus floor was 53.4% for type 1, 25.8% for type 2, 8.8% for type 3, and 11.9% for type 4. In this study, while the frequency was 53.5% for type 1, 27.4% for type 2, 7.6% for type 3, and 11.5% for type 4 on the right side, the same order for the left side was 54.9%, 26.6%, 6.6%, and 11.9%. While no significant difference was found between the sides in the distribution of the types, it was found that the type 2 Vidian canal was observed more frequently in males. In previous studies, the gender factor was not assessed, but this finding should be verified in future studies. For the first time in the literature, it has been shown in this study that type 2 Vidian canal is more common in male gender according to sphenoid sinus floor.
Dehiscences can be found in the bony roof of Vidian canal. Preoperative detection of the dehiscences in the canal will make the surgical procedure more careful and safe. Davoodi et al. (23) reported in their study that the rate of dehiscence in the Vidian canal bony roof was 34.4% in males and 37.5% in females. In the study in which they evaluated 300 CT examinations, Hewaidi et al. (24) reported dehiscence rate in the Vidian canal bony roof to be 37%. Yazar et al. (5) reported that the dehiscence frequency was 32% in the Vidian canal bony roof and it was less in patients with Vidian canal protruding into the sphenoid sinus. In this study, the presence of dehiscence in the Vidian canal bony roof was 22.2% on the right side and 26.6% on the left side. Detecting the presence of dehiscence in the Vidian canal before the surgery will reduce the risk of Vidian nerve injury.
Determination of the location of Vidian canal is necessary for Vidian neurectomy, for transnasal endoscopic skull base surgery, for the access to internal carotid artery through transnasal endoscopy or for the tumors around the Vidian nerve. Vidian neurectomy can be very rarely performed because of the difficulty of identification and transaction of the Vidian nerve and because of postoperative complications. Vidian neurectomy can be performed using different methods. Robinson and Wormald (25) described endoscopic transnasal Vidian neurectomy in 2006, and Liu et al. (22) described endoscopic transsphenoidal Vidian neurectomy.
The inclusion of the patients in whom CT was taken due to only nasal trauma and the fact that the effects of the study on the frequency of complications in terms of surgery are not known can be considered as the limitations of this study. The fact that it is a one-centered study prevents it to be generalizable for the Turkish society. The study will contribute to the literature more prominently if it is planned randomly and retrospectively and if it can be done to investigate the correlation between the complication rate and this typing in patients who have undergone endoscopic sphenoid sinus surgery. However, we think that our study is important in terms of revealing Vidian canal types and the frequency of canal dehiscence in our society.
Conclusion
Physicians dealing with endoscopic sinus surgery must know the nasal anatomy and important anatomical formations on the skull base. Complications are inevitable in surgeries performed with insufficient anatomical knowledge and experience. Before the endoscopic sinus surgery, paranasal sinus CT scanning in all patients is very important in terms of protection from complications and in terms of having full knowledge of anatomy. Increasing the experience in endoscopic sinus surgery and acceleration of the studies in anatomy will eliminate the deficiencies in this area.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Bakırköy Dr. Sadi Konuk Training and Research Hospital (Ethics board no: 2016/195).
Informed Consent: Informed consent was not received due to the retrospective nature of the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Design - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Supervision - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Resource - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Materials - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Data Collection and/or Processing - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Analysis and/or Interpretation - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Literature Search - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Writing - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.; Critical Reviews - Y.Y., M.Ç., B.M.Ş., A.A., B.O., F.T.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Vescan AD, Snyderman CH, Carrau RL, Mintz A, Gardner P, Branstetter BT, et al. Vidian canal: analysis and relationship to the internal carotid artery. Laryngoscope. 2007;117:1338–42. doi: 10.1097/MLG.0b013e31806146cd. https://doi.org/10.1097/MLG.0b013e31806146cd. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy DW, Zinreich SJ, Kuhn F, Shaalan H, Naclerio R, Loch E. Endoscopic middle meatal antrostomy: theory, technique and patency. Laryngoscope. 1987;97:1–9. doi: 10.1288/00005537-198708002-00001. https://doi.org/10.1288/00005537-198708002-00001. [DOI] [PubMed] [Google Scholar]
- 3.Ritter FN. The paranasal sinuses: anatomy and surgical technique. St. Louis: C.V. Mosby; 1978. [Google Scholar]
- 4.Messerklinger W. Endoscopy of the nose. Baltimore: Urban and Schwaaenberg; 1978. [Google Scholar]
- 5.Yazar F, Cankal F, Haholu A, Kilic C, Tekdemir I. CT evaluation of the vidian canal localization. Clin Anat. 2007;20:751–4. doi: 10.1002/ca.20496. https://doi.org/10.1002/ca.20496. [DOI] [PubMed] [Google Scholar]
- 6.Unal B, Bademci G, Bilgili YK, Batay F, Avci E. Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat. 2006;28:195–201. doi: 10.1007/s00276-005-0073-9. https://doi.org/10.1007/s00276-005-0073-9. [DOI] [PubMed] [Google Scholar]
- 7.Pata YS, Ünal M, Akbaş Y. Paranazal sinüsler ve nazal kavitenin anatomik varyasyonları; bilgisayarlı tomografi çalışması. Turk Arch Otorhinolaryngol. 2005;43:201–6. [Google Scholar]
- 8.Çağıcı CA, Yavuz H, Erkan AN, Akkuzu B, Özlüoğlu L. Paranazal sinüs anatomik varyasyonların değerlendirilmesinde bilgisayarlı tomografi. Turk Arch Otorhinolaryngol. 2006;44:201–10. [Google Scholar]
- 9.Kaplanoglu H, Kaplanoplu V, Dilli A, Toprak U, Hekimoğlu B. Analysis of the ethmoid roof by using computed tomography. Eurasian J Med. 2013;45:115–25. doi: 10.5152/eajm.2013.23. https://doi.org/10.5152/eajm.2013.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kazkayasi M, Karadeniz Y, Arikan OK. Anatomic variations of the sphenoid sinus on computed tomography. Rhinology. 2005;43:109–14. [PubMed] [Google Scholar]
- 11.Lee JC, Kao CH, Hsu CH, Lin YS. Endoscopic transsphenoidal vidian neurectomy. Eur Arch Otorhinolaryngol. 2011;268:851–6. doi: 10.1007/s00405-010-1482-x. https://doi.org/10.1007/s00405-010-1482-x. [DOI] [PubMed] [Google Scholar]
- 12.Kasemsiri P, Solares CA, Carrau RL, Prosser JD, Prevedello DM, Otto BA, et al. Endoscopic endonasal transpterygoid approaches: anatomical landmarks for planning the surgical corridor. Laryngoscope. 2013;123:811–5. doi: 10.1002/lary.23697. https://doi.org/10.1002/lary.23697. [DOI] [PubMed] [Google Scholar]
- 13.Tubbs RS, Salter EG. Vidius Vidius (Guido Guidi): 1509–1569. Neurosurgery. 2006;59:201–3. doi: 10.1227/01.NEU.0000219238.52858.47. https://doi.org/10.1227/01.NEU.0000219238.52858.47. [DOI] [PubMed] [Google Scholar]
- 14.Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R. Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus. 2005;19:E6, 1–10. https://doi.org/10.3171/foc.2005.19.1.7. [PubMed] [Google Scholar]
- 15.Kim HS, Kim DI, Chung IH. High resolution CT of the pterygopalatine fossa and its communications. Neuroradio. 1996;38:120–6. doi: 10.1007/BF02278138. https://doi.org/10.1007/BF02278138. [DOI] [PubMed] [Google Scholar]
- 16.Frautschi RS, Halasa B, Orra S, Mlynek K, Steiner CP, Papay FA. Pterygopalatine fossa anatomy for a surgical approach to sphenopalatine ganglion. J Craniofac Surg. 2016;27:1866–9. doi: 10.1097/SCS.0000000000003053. https://doi.org/10.1097/SCS.0000000000003053. [DOI] [PubMed] [Google Scholar]
- 17.Mohebbi A, Rajaeih S, Safdarian M, Omidian P. The sphenoid sinus, foramen rotundum and vidian canal: a radiological study of anatomical relationships. Braz J Otorhinolaryngol. 2016 May 24; doi: 10.1016/j.bjorl.2016.04.013. pii: S1808-8694(16)30093-3. [Epub ahead of print] https://doi.org/10.1016/j.bjorl.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahmati A, Ghafari R, AnjomShoa M. Normal variations of sphenoid sinus and the adjacent structures detected in cone beam computed tomography. J Dent (Shiraz) 2016;17:32–7. [PMC free article] [PubMed] [Google Scholar]
- 19.Sirikci A, Bayazit YA, Bayram M, Mumbuç S, Güngör K, Kanlikama M. Variations of sphenoid and related structures. Eur Radiol. 2000;10:844–8. doi: 10.1007/s003300051016. https://doi.org/10.1007/s003300051016. [DOI] [PubMed] [Google Scholar]
- 20.Yeh IK, Wu IS. Computed tomography evaluation of the sphenoid sinus and the vidian canal. B-ENT. 2013;9:117–21. [PubMed] [Google Scholar]
- 21.Inal M, Muluk NB, Arikan OK, Şahin S. Is there a relationship between optic canal, foramen rotundum, and vidian canal? J Craniofac Surg. 2015;26:1382–8. doi: 10.1097/SCS.0000000000001597. https://doi.org/10.1097/SCS.0000000000001597. [DOI] [PubMed] [Google Scholar]
- 22.Liu SC, Wang HW, Su WF. Endoscopic vidian neurectomy: the value of preoperative computed tomographic guidance. Arch Otolaryngol Head Neck Surg. 2010;136:595–602. doi: 10.1001/archoto.2010.72. https://doi.org/10.1001/archoto.2010.72. [DOI] [PubMed] [Google Scholar]
- 23.Davoodi M, Saki N, Saki G, Rahim F. Anatomical variations of neurovascular structures adjacent sphenoid sinus using CT scan. Pak J Biol Sci. 2009;12:522–5. doi: 10.3923/pjbs.2009.522.525. https://doi.org/10.3923/pjbs.2009.522.525. [DOI] [PubMed] [Google Scholar]
- 24.Hewaidi G, Omami G. Anatomic variation of sphenoid sinus and related structures in Libyan population: CT scan study. Libyan J Med. 2008;3:128–33. doi: 10.4176/080307. https://doi.org/10.4176/080307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson SR, Wormald PJ. Endoscopic vidian neurectomy. Am J Rhinol. 2006;20:197–202. [PubMed] [Google Scholar]