Abstract
Lipomas are benign mesenchymal tumors that can be observed all over the body. In total, 25% of lipomas are observed in the head and neck region, and most of them are located in the posterior cervical triangle. Lipomas that are greater than 10 cm in width or more than 1000 g in weight are called giant tumors. Cervico–thoracic lipomas are extremely rare, and only four cases have been reported in the English literature. We report successful surgical excision of a giant lipoma, which started from middle-anterior cervical region covered the anterior cervical triangle, and extended to the mediastinum, without thoracotomy.
Keywords: Lipoma, neck, child
Introduction
Lipomas are benign mesenchymal tumors that can be observed all over the body. Lipomas usually occur in the 5th and 6th decades of life (1). Lipomas and variants, which are rarely observed in the head and neck region (25%), are often subcutaneously localized in the posterior neck (2). Lipomas with their slow growth pattern are generally asymptomatic but can sometimes reach giant sizes. We reviewed the literature and saw very few cervical region giant lipomas extending to the thorax (3–6). Here we report successful surgical excision of symptomatic giant lipoma, which started from the middle jugular region, covered the anterior cervical triangle, and extended to the mediastinum, without the need of thoracotomy.
Case Report
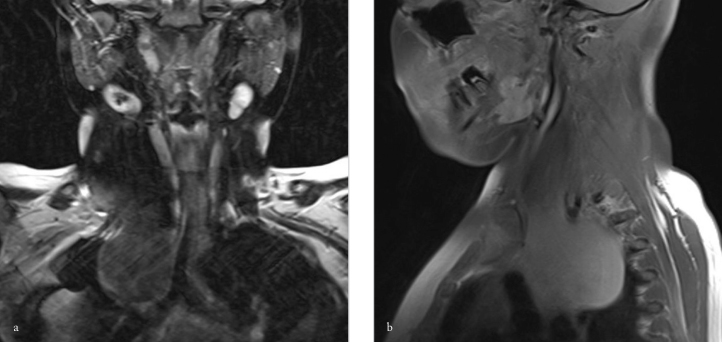
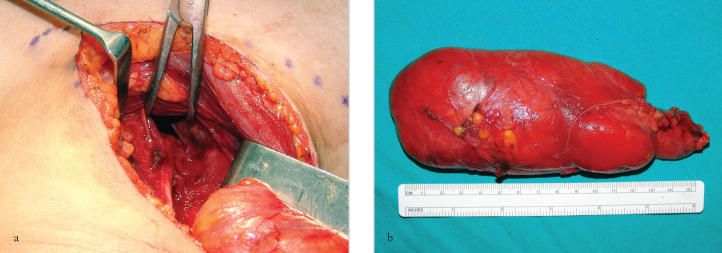
A 13-year-old male patient was referred to our department with a complaint of painless swelling on the right side of his neck the for a long time. The mass grew in size and resulted dysphagia in the last few months. Physical examination revealed a soft, painless mass beginning from the middle jugular region in his neck. The endoscopic examination of nasopharynx and larynx of the patient was unremarkable. On magnetic resonance imaging (MRI), a mass with fat signal intensity was found to replace the carotid artery and jugular vein in the neck, trachea, and esophagus in the mediastinum to the left (Figure 1a, b). Fine-needle aspiration biopsy (FNAB) was performed, and the cytopathological diagnosis was lipoma. The patient was operated under general anesthesia. An incision was made parallel to the front edge of the sternocleidomastoid (SCM) muscle, and the skin, subcutaneous tissue, and platysma was transected. Then, the anterior neck was exposed. A yellowish mass pushing the vascular structures medially was revealed on the medial edge of the SCM muscle. The mass was found to extend from the defect in the supraclavicular region to the mediastinum (Figure 2 a, b). The mass was carefully dissected from the surrounding tissue and totally removed. Pathological examination of the surgical specimen revealed the diagnosis of lipoma. The patient is still being followed up in our department since 3 years. Written informed consent was obtained from patient’s parents who participated in this study.
Figure 1. a, b.
T2-weighted coronal section MRI shows a mass pushing the vascular structures and trachea medially (a) T1-weighted sagittal section MRI shows extension of the mass to mediastinal structures and the spinal region (b)
Figure 2. a, b.
After lipoma excision, a defect is observed on the apex of the thorax (a) Excised material (b)
Discussion
Lipoma is the most common mesenchymal tumor that is rarely observed in the anterior neck location (3). Lipomas are usually observed in obese patients; the only difference that separates it from the normal adipose tissue is the fibrous capsule around it (2, 3). Lipomas, with their slow growth pattern, are generally asymptomatic but can sometimes reach giant sizes. Lipomas that are greater than 10 cm in width or more than 1000 g in weight are called giant tumors (7). They are usually observed in the elderly and are very rare in children. Solitary lipoma lesions are more common in females, whereas multiple lipomas are mostly observed in men. Congenital cases of lipoma have also been reported in children (1, 8). Lipomas rarely occur in the head and neck region. They most frequently settle on the posterior cervical triangle in the head and neck region, and the anterior neck location is very rare in case of head and neck lipomas (8, 9). In our case, the size of the lipoma was 16×7 cm and its weight was 1120 g. In addition, unlike previous reports, our patient was of a young age and the location of the mass was the anterior cervical triangle.
Clinically lipomas appear as a slow-growing, mobile, painless, palpable mass. Most of them are asymptomatic. Depending on the closeness of the mass to the spinal region and mediastinum, complaints such as difficulty in swallowing and chest pain can be observed. Patients with neck lipoma extending to the mediastinum may present with dyspnea (3).
Although the etiology of lipomas is not exactly known, genetic, endocrine, and traumatic factors are the most common causes of the disease. The uncontrolled growth mechanism of lipomas remains unclear. Blunt trauma is one of the possible reasons. Rupture of the fibrous tissue after blunt trauma may result in proliferation of the adipose tissue (10). In some cases lipomas are also associated with several syndromes such as Gardner’s syndrome, Madelung’s disease, and Dercum’s disease (1, 8).
The difference between giant cervical lipoma and liposarcoma should be defined in the preoperative period. In such a case, FNAB should be considered. Gaskin and Helms (11) retrospectively reviewed 126 fatty masses to define the role of MRI in the differential diagnosis of simple lipomas and liposarcomas. They reported that MRI is highly sensitive in the diagnosis of well-differentiated liposarcomas and highly specific for simple lipomas. In the diagnosis of lipomas, ultrasonography is the initial radiological assessment, as in other head and neck masses (2). Computed tomography (CT) and MRI could be preferred in order to determine the lesion’s connection with the surrounding tissue. On CT scans, lipomas appear as homogeneous masses with few septations and do not typically show contrast enhancement (2, 9). On MRI, simple lipomas have a characteristic appearance and usually appear as a discrete, encapsulated, homogeneous fatty mass. Lipomas have high signal intensity on T1-weighted images (9, 11). They could be correctly diagnosed by comparing the signal intensity on T1- and T2-weighted images at the preoperative period (2).
Treatment modalities for lipomas range from liposuction and steroid injection to surgical excisions (8). The basic treatment of giant neck lipomas is total resection (12). Possible complications after surgery are vascular injury, vagus nerve dysfunction, hematoma formation, surgery infection, fat embolus, and excessive scarring (1, 3, 8). Although lipomas do not have high recurrence rates, resecting them could be difficult because of their large size and adherence to the surrounding tissues (13). The case reported here is similar. Our patient was at risk because of the critical anatomic location of the mass in the neck and its mediastinal extension. As the mass was in the upper mediastinum in the thorax, we decided not to perform thoracotomy. Then, we decided to begin the surgery from the neck region. The surgery eventually caused no functional loss, and excellent cosmetic results were obtained. Recurrence may take up 15 months to 10 years; patients should be regularly followed up during this period (12).
Cervico–thoracic lipomas are extremely rare, and only four cases have been reported in the English literature (3–6). Cutilli et al. (4) reported a giant cervico–mediastinal lipoma case in a 77-year-old woman. The patient also had complaints such as dysphagia, persistent cough, dyspnea, and palpitations. Venkatramani et al. (5) also reported a 43-year-old human immunodeficiency virus-positive patient with a giant cervicothoracic lipoma. They proposed that this lipodystrophy was associated with human immunodeficiency virus disease. One of the lipoma cases that extended to the anterior mediastinum was reported by Sharma et al. (3). The only pediatric case with a giant cervico–mediastinal thymolipoma was presented by Patel et al. (6). The patient was an 11-year-old boy who presented with a cervical mass extending from behind the right side of the neck and plunging into the right side of the chest under the sternum. Therefore, we have reported the second case of pediatric cervico–thoracic giant lipoma.
Conclusion
Contrary to the literature, our patient was a male child and the mass originated from the anterior cervical triangle and extended to the mediastinum. The patient had painless swelling in his neck for a long time, and dysphagia developed in the recent period. For radiological diagnosis, ultrasound and MRI are useful. Before the decision regarding the surgery, FNAB might be performed. During the surgery, the mass was totally removed from the neck without the need of thoracotomy. No complication developed in the postoperative period. The patient is still under follow-up.
Footnotes
This study was presented at the 2nd Congress of Swallowing Disorders as a poster, 5–7 December 2013, Ankara, Turkey.
Informed Consent: Written informed consent was obtained from patient’s parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.A.E., A.Y.; Design - A.Y., H.Y.; Supervision - M.A.E., M.A.; Resources - M.A., H.Y. Materials - M.A., H.Y.; Data Collection and/or Processing - A.Y., H.Y.; Analysis and/or Interpretation - H.Y., M.A.; Literature Search - A.Y., H.Y.; Writing Manuscript - M.A.E., A.Y. Critical Review - M.A.E., M.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Salam G. Lipoma excision. Am Fam Physician. 2002;65:901–4. [PubMed] [Google Scholar]
- 2.WuWei C, Chi HP, Chiang FY, Hsu YC, Chan LP, Kuo WR. Case report giant lipoma arising from deep lobe of the parotidgland. World J Surg Oncol. 2006;4:28. doi: 10.1186/1477-7819-4-28. http://dx.doi.org/10.1186/1477-7819-4-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma BK, Khanna SK, Bharati M, Gupta A. Anterior neck lipoma with anterior mediastinal extention – a rare case report. Kathmandu Univ Med J. 2013;11:88–90. doi: 10.3126/kumj.v11i1.11048. [DOI] [PubMed] [Google Scholar]
- 4.Cutilli T, Schietroma M, Marcelli VA, Ascani G, Corbacelli A. Giant cervico-mediastinal lipoma. A clinical case. Minerva Stomatol. 1999;48:23–8. [PubMed] [Google Scholar]
- 5.Venkatramani H, Ramani V, Sabapathy SR. Giant cervicothoracic lipoma as a manifestation of human immunodeficiency virus-associated lipodystrophy. Plast Reconstr Surg. 2010;126:316–8. doi: 10.1097/PRS.0b013e3181f640df. http://dx.doi.org/10.1097/PRS.0b013e3181f640df. [DOI] [PubMed] [Google Scholar]
- 6.Patel RV, Evans K, Sau I, Huddart S. Peadiatric giant cervicomediastinal thymolipoma. BMJ Case Rep. 2014;20:2014. doi: 10.1136/bcr-2014-203585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanchez M, Golomb F, Moy J, Potozkin JR. Giant lipoma. Case report and review of the literature. Am J Acad Dermatol. 1993;28:266–8. doi: 10.1016/s0190-9622(08)81151-6. http://dx.doi.org/10.1016/S0190-9622(08)81151-6. [DOI] [PubMed] [Google Scholar]
- 8.Medina C, Schneider S, Mitra A, Spears J, Mitra A. Giant submental lipoma: case report and review of literature. Can J Plast Surg. 2007;15:219–22. doi: 10.1177/229255030701500405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salvatore C, Antonio B, Del Veccio W, Lanza A, Tartaro G, Giuseppe C. Giant infiltrating lipoma of the face: CT and MR imaging findings. Am J Neuroradiol. 2003;24:283–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Meggit BF, Wilson JN. The battered buttock syndrome: fat fractures: a report on a group of traumatic lipomata. Br J Surg. 1972;59:165–9. doi: 10.1002/bjs.1800590302. [DOI] [PubMed] [Google Scholar]
- 11.Gaskin CM, Helms CA. Lipomas, lipoma variants and well-differentiated liposarcomas (atypicallipomas): Results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182:733–9. doi: 10.2214/ajr.182.3.1820733. http://dx.doi.org/10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 12.Terzioglu A, Tuncali D, Yuksel A, Bingul F, Aslan G. Giant lipomas: a series of 12 consecutive cases and a giant liposarcoma of the thigh. Dermatol Surg. 2004;30:463–7. doi: 10.1111/j.1524-4725.2004.30022.x. http://dx.doi.org/10.1111/j.1524-4725.2004.30022.x. [DOI] [PubMed] [Google Scholar]
- 13.Basmaci M, Hasturk AE. Giant occipitocervical lipomas: evaluation with two cases. J Cutan Aesthet Surg. 2012;5:207–9. doi: 10.4103/0974-2077.101387. http://dx.doi.org/10.4103/0974-2077.101387. [DOI] [PMC free article] [PubMed] [Google Scholar]