Abstract
Thyroglossal duct cyst (TGDC) is the most common congenital midline neck mass in children. It usually becomes symptomatic following a respiratory tract infection and is usually diagnosed at 5 years of age. Thyroglossal duct cyst is rarely observed in less than 1-year-old infants. In this study, we present a 3-month-old infant with TGDC, who was administered multiple courses of antibiotic therapy for the hyperemic, draining, midline neck mass that had existed since he was 15 days old. Physical examination revealed an infrahyoid midline neck mass measuring 3×3 cm, which moved while swallowing and had a sinus opening in the overlying skin. The patient underwent Sistrunk operation under general anesthesia. Histopathologic examination revealed TGDC. One-year follow-up revealed no recurrence.
Keywords: Thyroglossal duct cyst, neck mass, congenital anomaly, Sistrunk operation
Introduction
Thyroglossal duct cysts (TGDCs) are benign cystic formations that develop as a result of a partial or complete obliteration deficiency of the thyroglossal duct and the secretory properties of the epithelium in the duct. If these lesions are fistulized on the skin, they are called the thyroglossal cyst fistula (1). Approximately 10% of neck masses seen in children are congenital neck masses, and TGDCs or their fistulas are the most common congenital neck midline masses (2, 3). They are encountered equally in both genders. Although they are often seen in childhood, particularly in the first 5 years, they may be seen in every decade of life (4); this rate was reported to be approximately 7% in the adult population (5). They may be found at the intralingual, suprahyoid/submental, tirohyoid, or suprasternal localizations. Patients consult a doctor with the most common complaint of the presence of infections and symptoms, and the rate at which these instances occur is approximately 50% (4–6).
Dermoid cysts, branchial cleft cysts, thyroid pyramidal lobe, thyroid adenoma, thyroid carcinoma, aberrant thyroid tissue, hemangioma, lymphadenopathy, lymphangioma, laryngocele, lipomas, and teratomas should be considered in the differential diagnosis (7, 8).
The treatment of these cysts is surgical, and the most common method used in surgery is the Sistrunk procedure, in which the cyst and hyoid bone are removed together.
Case Report
A 3-month-old male infant was taken to the health institution several times by his family because he had a swelling located in the midline of the neck since birth, with redness around the swelling and occasional discharge from this swelling. He received antibiotic treatment for infection. On physical examination (PE), a mass that was approximately 3×3 cm in size, mobile during swallowing and had a sinus opening on the skin above it, was found in the neck midline at the infrahyoidal level. Although ultrasonography (USG) revealed normal-sized thyroid lobes and homogeneous parenchymas, a well-circumscribed cystic nodular lesion (16×24×25 mm in size) that contained mobile echogenic sediments was detected in the midline of the neck in the submental area. As the patient’s PE and USG findings suggested the presence of a TGDC, an additional examination was not requested from the patient and the operation was planned (Figure 1). The Sistrunk procedure was performed under general anesthesia (Figure 2, 3). No complications developed in the early postoperative follow-up of the patient, and he was discharged with recommendations on the fourth postoperative day. Histopathologic examination of the cyst was reported as a TGDC. No recurrence was observed in the postoperative 1-year follow-up of the patient. Written informed consent was received from the parent of the infant in this case presentation.
Figure 1.

Preoperative view of the patient
Figure 2.
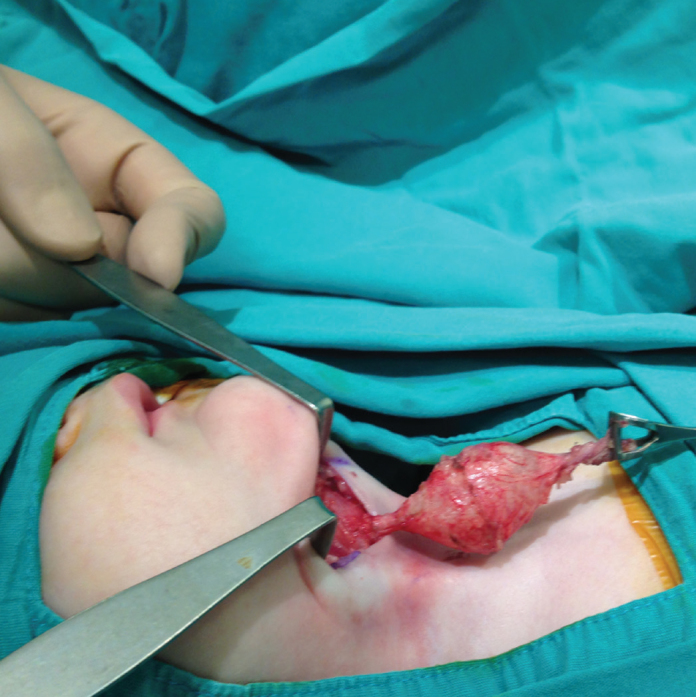
The image of the mass dissected from the surrounding tissues
Figure 3.

The macroscopic view of the mass
Discussion
Thyroglossal duct anomalies are the most common neck midline masses that occur at a rate of 70%. They are usually seen as cysts. Although sporadic and genetic factors are thought to play a role in its development, they are considered to develop rather sporadically. Although they are of embryonic origin, rare symptomatic cases have been reported during infancy. Of the cases, 25% present symptoms in preschool children and 50% of them present symptoms before the age of 20 years (9). In our case, the situation was interesting because the symptoms emerged during the infant period.
A detailed anamnesis and PE findings are important in the differential diagnosis. In PE, the up-and-down movement of a non-soft mass in the midline of the neck during the protrusion of the tongue or swallowing is pathognomonic (3, 10). USG is the first imaging method to be performed in a patient who is considered to have TGDC. Thyroid USG or thyroid scintigraphy should be performed to detect the presence of preoperative normal thyroid tissues. The advantages of USG are that it is not expensive, it does not require sedation in children, it is not an interventional procedure, it does not involve radiation, and it provides useful information about the mass and normal thyroid tissue.
Although it is quite rare to encounter TGDC during the newborn or infant period, it has been reported in the literature that lingual thyroid cases are more common in this period (10–13). This condition is often asymptomatic, but depending on the size of the mass, it may cause symptoms such as dysphagia and a foreign body sensation in the throat in addition to dysphonia or voice coarsening (12).
Because the risk of infection development is high in TGDC, cysts should be excised under elective conditions. The Sistrunk procedure, which has the least recurrence rate, is the most common surgical method. Inadequate surgery, infected cyst, false diagnosis, draining of the cyst, perforation of the cyst during surgery, and patient’s being younger than 2 years of age are the factors that increase the risk of recurrence (2, 7, 10).
Conclusion
TGDCs are the most common congenital masses that are seen in the neck. They occur frequently in the first decade of life, and although they are seen at an average age of 5 years, rare cases presenting symptoms in the infant period may also be encountered, as in our patient.
Footnotes
This study was presented at the 37th Turkish National Congress of Otolaryngology Head and Neck Surgery as a poster 28 October–01 November 2015, Antalya, Turkey.
Informed Consent: Written informed consent was obtained from patient’s parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - S.A., A.Ç.; Design - S.A., A.Ç.; Supervision - S.A.; Resource - A.Ç., E.K.; Materials - E.K, A.Ç.; Data Collection and/or Processing - A.Ç., E.K.; Analysis and/or Interpretation - A.Ç., E.K.; Literature Search - A.Ç.; Writing - A.Ç.; Critical Reviews - S.A., A.Ç.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Atalay BE, Bora F, Şekercan Ö, Ceylan S, Batmaz T, Yücel Z. Thyroglossal duct fistula with double tract. Istanbul Med J. 2011;12:141–4. http://dx.doi.org/10.5505/1304.8503.2011.33042. [Google Scholar]
- 2.Al-Khateeb TH, Al Zoubi F. Congenital neck masses: a descriptive retrospective study of 252 cases. J Oral Maxillofac Surg. 2007;65:2242–7. doi: 10.1016/j.joms.2006.11.039. http://dx.doi.org/10.1016/j.joms.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 3.Ahuja AT, Wong KT, King AD, Yuen EH. Imaging for thyroglossal duct cyst: the bare essentials. Clin Radiol. 2005;60:141–8. doi: 10.1016/j.crad.2004.08.009. http://dx.doi.org/10.1016/j.crad.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Sanders LE, Cady B. Embryology and developmental abnormalities. In: Cady B, Rossi RL, editors. Surgery of the thyroid and parathyroid glands. Philadelphia: W.B. Saunders; 1991. pp. 5–12. [Google Scholar]
- 5.Ellis PD, van Nostrand AW. The applied anatomy of thyroglossal tract remnants. Laryngoscope. 1977;87:765–70. doi: 10.1002/lary.5540870512. http://dx.doi.org/10.1002/lary.5540870512. [DOI] [PubMed] [Google Scholar]
- 6.Telander RL, Deane SA. Thyroglossal and branchial cleft cysts and sinuses. Surg Clin North Am. 1977;57:779–91. doi: 10.1016/s0039-6109(16)41288-0. http://dx.doi.org/10.1016/S0039-6109(16)41288-0. [DOI] [PubMed] [Google Scholar]
- 7.Athow AC, Fagg NL, Drake DP. Management of thyroglossal duct cysts in children. Br J Surg. 1989;76:811–14. doi: 10.1002/bjs.1800760815. http://dx.doi.org/10.1002/bjs.1800760815. [DOI] [PubMed] [Google Scholar]
- 8.Josephson GD, Spencer WR, Josephson JS. Thyroglossal duct cyst: the New York Eye and Ear Infirmary experience and a literature review. Ear Nose Throat J. 1998;77:642–51. [PubMed] [Google Scholar]
- 9.Yılmaz B, Şengül E, Gül A, Akdağ M, Özkurt Fazıl E, ve ark Özkan H. Tiroglossal duktus kisti ve fistüllerindeki tecrübelerimiz. Int J Clin Res. 2014;2:49–51. [Google Scholar]
- 10.Mondin V, Ferlito A, Muzzi E, Silver CE, Fagan JJ, Devaney KO, et al. Thyroglossal duct cyst: personal experience and literature review. Auris Nasus Larynx. 2008;35:11–25. doi: 10.1016/j.anl.2007.06.001. http://dx.doi.org/10.1016/j.anl.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Ulug T, Ulubil SA, Alagöl F. Dual ectopic thyroid: report of a case. J Laryngol Otol. 2003;117:574–6. doi: 10.1258/002221503322113076. http://dx.doi.org/10.1258/002221503322113076. [DOI] [PubMed] [Google Scholar]
- 12.Hazarika P, Siddiqui SA, Pujary K, Shah P, Nayak DR, Balakrishnan R. Dual ectopic thyroid: a report of two cases. J Laryngol Otol. 1998;112:393–5. doi: 10.1017/s0022215100140563. http://dx.doi.org/10.1017/S0022215100140563. [DOI] [PubMed] [Google Scholar]
- 13.Majumdar Indrajit, Mastrandrea Lucy D. Lingual Thyroid as a Cause of Primary Hypothyroidism: Congenital Hypothyroidism in the Neonatal Period and Beyond. Clin Pediatr. 2010;49:885–8. doi: 10.1177/0009922810364660. http://dx.doi.org/10.1177/0009922810364660. [DOI] [PubMed] [Google Scholar]


