Abstract
Objective
We aimed to determine the prevalence of allergic rhinitis in children aged 12–15 years who lived in the Trabzon Province, specify possible risk factors, and compare the data obtained with those of the other studies conducted in our country and in other countries.
Methods
First, 1372 students from nine primary schools determined according to the recommendations of Department of Public Health and approval of The Provincial Directorate of Health were screened in their schools with questionnaire forms. Second, students providing the response “yes” to the first and/or second questions in the questionnaire forms were considered as possible allergic rhinitis patients and invited to our clinic. Then, 246 students were subjected to a skin prick test. Data were collected with the evalution of questionnaire and skin prick test results together.
Results
The prevalance of allergic rhinitis in children between 12 and 15 years age was found to be 14.5% in Trabzon. Female gender was found to be a relative a risk factor for allergic rhinitis (p=0.015). The prevalence of allergic rhinitis in children whose both parents were smoking was significantly higher than that in children whose only one parent was smoking or both parents were nonsmokers (p=0.0024). In addition, living in an apartment flat (p=0.015) and owing pets (p=0.04) were detected to be other risk factors for allergic rhinitis.
Conclusion
According to our investigations, this is the first prevalence study in Trabzon, which is the largest settlement in the Eastern Black Sea Region. The prevalence of allergic rhinitis in children was found to be 14.5%. Female gender, smoking habits of the parents, owing pets, and living in an apartment flat are risk factors for allergic rhinitis.
Keywords: Allergic rhinitis, prevalence, pediatric
Introduction
Allergic rhinitis is a globally observed disease that can severely affect the quality of life. It includes an intermittent type that is observed in the pollen season and a persistent type that continues throughout the year. Allergens vary according to the climates and countries (1). Diagnosis can be performed with a good medical history, physical examination, and skin test. The complaints of patients can be minimized by protection from allergens and by appropriate medical treatment (2).
In recent years, an increase in allergic diseases preoccupies the role of environmental factors. However, among thousands of environmental factors, the exact factor remains unknown. Findings regarding the role of smoking, exhaust gas, air pollution, and living in hygienic conditions have been reported (3). Because no similar study has been performed in our region so far, we planned to screen 1372 students aged 12–15 years from nine schools. The schools were determined together with the Department of Public Health and Provincial Directorate of Health in Trabzon city center to specify the possible risk factors and to compare the data obtained with those of other studies performed in other cities of Turkey as well as other countries.
This study was performed to determine the prevalence of allergic rhinitis in students aged 12–15 years old in the Trabzon city center.
Methods
Nine primary schools were specified at the city according to the recommendations of the Provincial Directorate of Health and the approval of the school managements in 2010. The study was approved by the Karadeniz Technical University Ethics Committee (file no: 2009/36).
Based on the population of the city where this study was conducted, approximately 1300 students were recommended for screening in order to meet the statistical sufficiency required by the Department of Public Health.
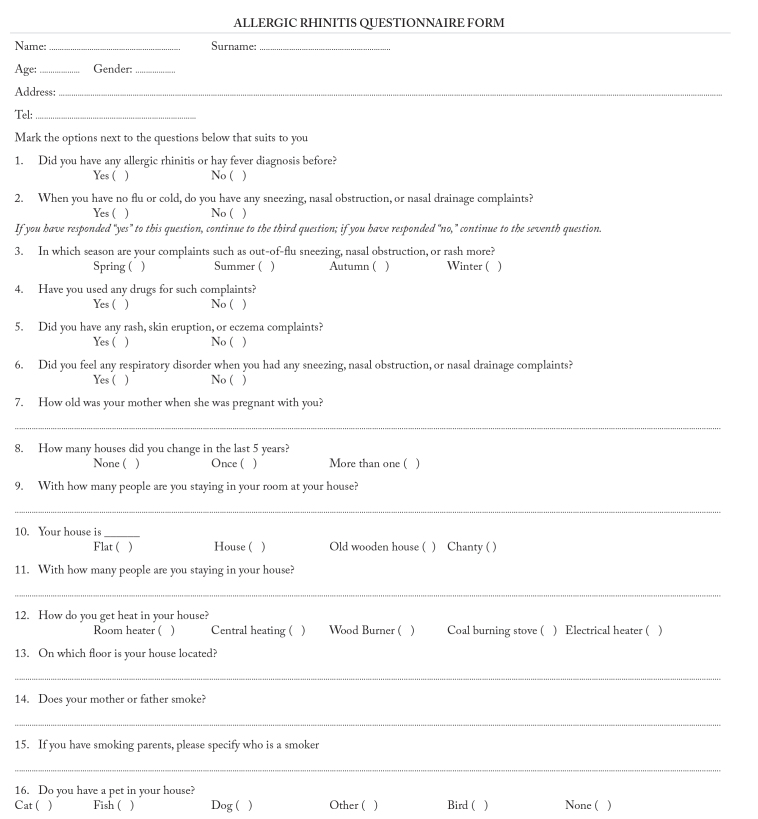
The Department of Public Health suggested screening of the 12–15-year-old age group in the consideration of reliability of the responses to the questionnaire items and easier cooperation during prick tests. Our study consisted of two stages. In the first stage, students were scanned at their schools using the “Questionnaire method.” The questionnaire was prepared by taking the questions on the official site of the European Allergic Rhinitis and Asthma Committee (ECRHS) as the base (4). Questionnaire items included house environments, bedrooms, pet habits, status of allergic complaints according to the seasons, age of the mother, and smoking status of the parents (Figure 1).
Figure 1.
Allergic rhinitis questionnaire form
A total of 1372 students at the city were given this survey. Approvals from the management of the primary schools were obtained, and upon this approval, written consents of the families were also obtained before handing out the questionnaires to the students in their classrooms. Students responding “yes” to the first and/or second questions in the questionnaire were considered as potential allergic rhinitis patients and were invited to our clinic for a prick test. Before the prick test, consents of their families were obtained. Information about antihistaminic or other drug usage, which could degrade the test results of the questionnaire survey, was obtained, and the students were warned not to use any drugs before coming to our clinic for the prick test. In this group, two students had psoriasis; therefore, the test could not be performed on them. The prick test was routinely performed using 24 standardized Alk-Albio (ALK; Berkshire, UK) Allergens. Allergens were applied to both arms and penetrated into the subcutaneous layers via a lancet. After waiting for 15 minutes, the allergens that induced an induration with a diameter equal to or greater than that of the control allergen histamine were accepted as the specific allergen responsible for the development of allergic rhinitis. During the 15-minute waiting period in our clinic, students were accompanied by an attendant, and emergency kit and drugs were kept ready in case of any possible anaphylaxis or allergic reaction.
Our study is summarized by a flow chart (Figure 2). With the findings of the prick test and questionnaire, the correlations between allergic rhinitis and factors such as smoking habits of the parents, heating system in the house, room share in the house, seasonal variations in the symptoms of allergic rhinitis, type of residence, owning pets, and age of the mother were determined.
Figure 2.
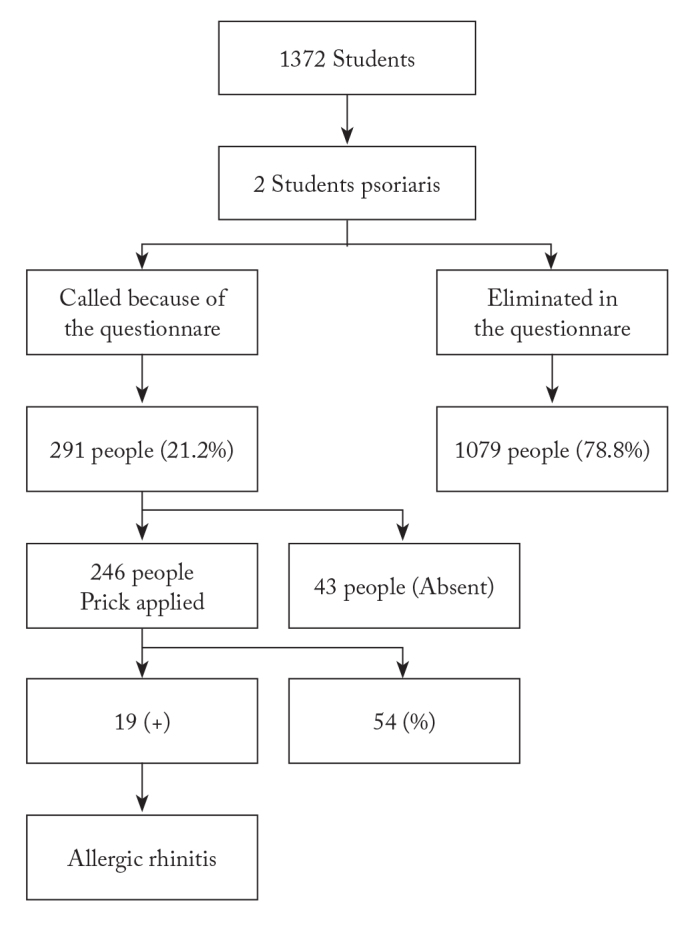
Flow chart of the study
Statistical Analyses
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software program (version 12.0 for Windows) (SPSS Inc.; Chicago, IL, USA). Data normality was assessed using the Kolmogorov–Smirnov test. Comparisons between groups were performed using Student’s t test for normally distributed data. Comparisons between groups for quantitative data and prevalence of allergic rhinitis were performed using the Chi square test. For risk factors associated with allergic rhinitis, analysis was performed using logistic regression analysis, in which allergic rhinitis was taken as the dependent variable. Results were shown as the arithmetic mean±standard deviation (SD) for quantitative data and as percentages for qualitative data. Odds ratio (OR) [95% confidence interval (CI)] was used for logistic regression analysis, and p<0.05 was considered as significant.
Results
The questionnaire survey was provided to 1372 students (female, n=712, 52%; male, n=658, 48%), and two students were excluded from the study because of psoriasis. Nearly half (145/291, 49.8%) of the students had marked the “yes” option for the first or second question in the questionnaire. In other words, these patients had allergic rhinitis before or they were sneezing, had nasal drainage, or had nasal obstruction and indicated that they had used drugs before for complaints of sneezing, nasal drainage, and nasal obstruction.
The students (n=291) who had marked the “yes” option for the first or second question were called to our clinic for the skin prick test, and this test was performed for 246 of them. Some (n=192) of the students with positive prick test results were diagnosed with allergic rhinitis.
When the findings of the skin prick test and questionnaire were evaluated together, the prevalence of allergic rhinitis was found to be 14.5%. Investigation of the other factors and statistical evaluation were performed in these patients (Table 1).
Table 1.
Sociodemographic data
| Risk factors | Students with allergic rhinitis | p value | |
|---|---|---|---|
|
| |||
| Gender | female | 115 (16.8%) | 0.015 |
| male | 77 (12.1%) | ||
|
| |||
| Smoking habits of parents | none | 75 (12.2%) | 0.0024 |
| only mother | 13 (13.5%) | ||
| only father | 68 (15.5%) | ||
| both parents are smokers | 36 (21.3%) | ||
|
| |||
| Heating device used in the house | floor heating | 53 (15.3%) | 0.172 |
| central system | 65 (13.7%) | ||
| wood stove | 24 (11.4%) | ||
| coal stove | 44 (17.2%) | ||
| room heater (with electric) | 6 (15.8%) | ||
|
| |||
| Room sharing | single | 73 (13.1%) | 0.214 |
| sharing room with one or more people | 119 (15.5%) | ||
|
| |||
| House type | apartment | 180 (15.4%) | 0.014 |
| others | 12 (8.4%) | ||
|
| |||
| Owning pets | none | 126 (13.8%) | 0.040 |
| pet owner | 66 (16%) | ||
| owner of only cat/dog | 9 (18%) | ||
|
| |||
| Age of the mother at delivery | average age of the mother in students with allergic rhinitis | 25.5±5.1 | 0.163 |
| average age of the mother in students with no allergic rhinitis | 26.1±4.7 | ||
Allergy–Gender
Among the students who were accepted as having allergic rhinitis according to the evaluation of the responses to the questionnaire items and findings of the skin prick test, allergic rhinitis was found in 115 (16.8%) female and 77 (12.1%) male students. It was observed that female gender was a significant risk factor for the diagnosis of allergic rhinitis (p=0.015).
Allergy–Smoking Habits of the Parents
Parents of 616 students (46.7%) were nonsmokers. Fathers of 438 students (33.2%) and mothers of 96 students (7.2%) were the only smokers in the family, while both parents of 169 (12.8%) students were smokers. The relationship between the smoking habits of the parents and allergy was also investigated. Allergic rhinitis was detected in 12.2% of the children whose parents were nonsmokers. The rates of allergic rhinitis in children whose father, mother, or both parents were smokers were 15.5%, 13.5%, and 21.3%, respectively. The prevalence of allergic rhinitis in children whose mother and father were both smokers was significantly higher than that in children whose only one parent was a smoker or both parents were nonsmokers (p=0.04).
Allergy–Heating Devices Used in the House
The students were using room heaters (n= 358: 26.1%), the central system (n=486; 35.5%), wood heaters (n=23016.8%), coal burning stoves (n=266: 19.4%), electrical heaters (n=41; 3%), or both electrical heaters and the central system (n=9). Accordingly, the frequency of allergic rhinitis among the students using wood heaters or other heaters was 17.2% and 13.8%, respectively, without any significant difference between groups (p=0.172).
Allergy–Room Share in the House
The students (n=558) stayed all alone in their private rooms or shared their rooms with one (n=644), two (n=98), three (n=17), and four (n=5) people. The prevalence of allergic rhinitis among students who stayed alone or those who shared their rooms with one or more than one person was 13.1% and 15.5%, respectively. The intergroup difference was not found to be significant (p=0.214).
Allergy–Seasonal Variations in Symptoms
The students complained of allergic rhinitis symptoms for one (n=52), two (n=15), or all four seasons (n=5). No significant difference was found between the seasonal differences and symptoms (p=0.112). However, when we considered the allergens according to the seasons, from the findings of the prick test, it was observed that the symptoms of the children who were allergic to the weed group, main tree group, and main prairie group were significantly higher in the spring season, according to their own information (according to the questionnaire answers) (p<0.001).
Allergy–House Type Relationship
With regard to the type of the house where the students were living, we observed that 1169 students lived in an apartment flat and 118 students lived in a private garden house. The incidence rate of allergic rhinitis among students living in an apartment flat was 15.4%, while that among the students living in a private garden house, wooden house, or other types of houses was 8.4%. According to these results, living in an apartment flat is a risk factor for allergic rhinitis (p=0.015).
Allergy–Pet Feeding Relationship
When we looked at the responses to the question “Do you have a pet at your house?,” we found that students had cats (n=18), dogs (35), pet birds (n=98), aquarium fish (n=202), and turtles (n=60); in total, 413 students had pets at their n-homes. The relationship of allergic rhinitis with pet feeding in the house was considered; the prevalence of allergic rhinitis in the students having a pet in their house was found to be 16%, while that in students who had no pets in their house was found to be 13.8%. The prevalence of allergic rhinitis in students who fed cats and dogs at their houses, which were accepted as allergens other than fish, turtles, and birds, was found to be 17%. Depending on these numbers, owing pets was considered as a risk factor for allergic rhinitis (p=0.04).
Correlation Between Allergy and Mother’s Age
When the responses to the question “How old was your mother when you were born?” were evaluated, the mean age of the mothers of the allergy-negative students who had allergic rhinitis before was found to be 26.1±4.7 years and that of the mothers of the allergy-positive students was found to be 25.5±5.1 years, without significant difference between groups (p=0.163).
Allergy–Prick Test Results
Students who had responded “yes” to the first and/or second question were called for the prick test. The prick test was performed by the original 24-fold allergen extracts of Alk-Albio in 246 of 291 students who consented and came to our clinic. In 192 of them, positive (+) results were found in the prick test, and allergic rhinitis was diagnosed. Distribution according to the allergenic parameters observed in the prick test is shown in Table 2.
Table 2.
Prick test results
| Weed allergy | 48 students (25%) |
| Main tree group (pine, birch, hazelwood) | 68 students (35%) |
| Main prairie group (dactylis, festuca, lolium, phleum, phoa) | 39 students (20.3%) |
| Main wheat group | 1 student (0.5%) |
| Fungi group | 0 |
| Penicillin notatum | 2 students (1%) |
| Candida albicans | 1 student (0.5%) |
| Silverbirch | 1 student (0.5%) |
| Willow | 2 students (1%) |
| Ligustrum | 2 students (1%) |
| Dermatophytes pteronyssinus | 96 students (50%) |
| Dermatophytes farinae | 96 students (50%) |
| Sambucus tree | 2 students (1%) |
| Pine tree | 4 students (2.1%) |
| Poplar tree | 3 students (1.6%) |
| Sweet spring grass | 31 students (16.1%) |
| Cat | 4 students (2.1%) |
| Dog | 5 students (2.6%) |
| Corn | 0 |
| Hazelnut | 1 student (0.5%) |
| Dead nettle | 1 student (0.5%) |
| Cynodon dactylon | 2 students (1%) |
According to these results, in children who had allergic rhinitis in the Trabzon city center, most frequent allergic reactions were detected against Dermatophagoides pteronyssinus and D. farinae, known as mites. This was followed by allergies against the main grass group and main tree group.
Based on logistic regression analysis, living in an apartment flat (OR: 2.17; 95% CI: 1.16–4.05) and smoking habits of parents (OR: 1.93; 95% CI: 1.23–3.03) were found to be independent risk factors for allergic rhinitis (Table 3).
Table 3.
Logistic regression analysis
| OR | 95% CI (confidence interval) | p value | ||
|---|---|---|---|---|
|
| ||||
| Gender | Male | 1 | ||
| Female | 1.42 | 1.04–1.95 | p=0.015 | |
| Room sharing | Single | 1 | ||
| Sharing room with one or more people | 1.24 | 0.89–1.73 | p=0.197 | |
| House type | Others | 1 | ||
| Apartment | 2.17 | 1.16–4.05 | p=0.015 | |
| Smoking habits of parents | None | 1 | ||
| Only mother | 1.34 | 0.93–1.91 | p=0.116 | |
| Only father | 1.17 | 0.62–2.22 | p=0.634 | |
| Both parents are smokers | 1.93 | 1.23–3.03 | p=0.0024 | |
| Heating device used in the house | Floor heating | 1 | ||
| Central system | 0.84 | 0.57–1.25 | p=0.395 | |
| Wood stove | 0.69 | 0.41–1.17 | p=0.168 | |
| Coal stove | 1.15 | 0.74–1.81 | p=0.534 | |
| Room heater (with electric) | 1.08 | 0.39–3.00 | p=0.880 | |
| Owning pets | None | 1 | ||
| Pet owner | 1.06 | 0.65–1.73 | p=0.816 | |
| Owner of only cat/dog/bird | 1.05 | 0.71–1.55 | p=0.822 | |
Constant: −2.93; OR: odds ratio
Discussion
Allergic diseases are one of most studied diseases. Their pathophysiology and etiological factors have been gradually understood better, which contributes to the development of novel treatment modalities. Although the prevalence of allergic rhinitis varies on the basis of regions, countries, and climates, its prevalence rates presumably increase (5).
The first study on children with allergic rhinitis in Turkey was conducted in Ankara between 1966 and 1967. While 23% of 1163 atopic children aged between 6 and 13 years had only persistent allergic rhinitis, the remaining 77% also had asthmatic bronchitis or atopic dermatitis (6). The prevalence studies on adults conducted in Şanlıurfa and Manisa reported the prevalence of allergic rhinitis to be 2.9% and 14.5%, respectively (7, 8). However, based on the studies on the pediatric population in Zonguldak and İstanbul, the prevalence of allergic rhinitis was found to be 37.7% and 7.9 %, respectively (9, 10).
Studies on the prevalence of allergic rhinitis have generally been conducted by pediatric and otorhinolaryngology clinics, and these studies have used two questionnaire types to date. While pediatrics departments have usually used the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, the ECRHS questionnaire, which was easy to modify and apply to every age group, has been preferred more frequently in studies conducted by otorhinolaryngology clinics. The reason behind this difference is that researches conducted by the pediatrics departments generally involved not only allergic rhinitis but also other allergic conditions such as asthma and childhood eczema (4). We used the ECRHS questionnaire in this study as well.
In this study, the prevalence of “allergic rhinitis” was determined as 14.5% according to our questionnaire results. When we examined the prevalence studies conducted all around the world, we found that Selnes et al. (11) reported the prevalence of allergic rhinitis to be 29.6% in 2005 in Norway among Western European countries. In a study conducted by Bauchau and Durham (12) in six countries in 2004, the prevalence of allergic rhinitis were reported to be 28.5% in Belgium, 24.5% in France, 20.6% in Germany, 16.9% in Italy, 21.5 % in Spain, and 26% in England. This prevalence study by Bauchau and Durham. was conducted on adults, but there is no such extensive study in children. It is one of the most comprehensive studies in Europe. Accordingly, the prevalence of allergic rhinitis in our region was comparable to that reported in other studies conducted in Turkey and but lower than that detected in Western Europe.
Some studies have revealed that male gender is a relative risk factor for allergic rhinitis, while some others studies could not demonstrate any difference between genders. In the study conducted by by Alsowaidi et al. (13) in United Arab Emirates, it was reported that the prevalence of allergic rhinitis was higher in the female population. In a study conducted by Van Gysel et al. (14) in Belgium, while allergic rhinitis was significantly higher in males in children younger than 8 years of age, a significant increase was observed in the prevalence of allergic rhinitis in females. The time interval from 8 to 10 years was accepted to be significant for children in the study, and the prevalence rate of allergic rhinitis evidently increased for females during this period. It was stated that gender and age-related changes involved the pre-pubertal period in females in this age group and were related to hormonal changes. As other examples in the literature, female gender was found to be a significant risk factor for allergic rhinitis in our study.
Smoking stimulates inflammatory cells of the airway. It causes airway inflammation by proinflammatory mediator release and neurologic inflammation (15). In a multi-center study conducted by Kurt et al. (16) in 17 provinces in Turkey in 2007, smoking was effective in respiratory tract allergies and the prevalence of allergic rhinitis was higher in smokers.
In their study involving 6794 preschool children in Singapore, Zuraimi et al. (17) determined that smoking in the house was related to the deterioration of rhinitis symptoms. On the other hand, Keil et al. (18) conducted a study on 1314 children in Germany and reported that smoking of mothers was a risk factor only in children of allergic parents.
In this study, one or both parents of 52.8% of children were smokers. Our study showed that smoking of both parents was a significant risk factor in terms of allergic rhinitis (p=0.004).
The socioeconomic level has been examined in almost all studies on allergy. The fact that the risk of allergic rhinitis was higher in groups with a higher socioeconomic level has been associated with the fact that such people express their complaints clearer and seek medical help more frequently (8). On the other hand, some studies have also demonstrated that allergic rhinitis is less frequently observed in people with a low socioeconomic level and in farmers. According to the compilation of Mösges from Germany, numerous environmental risk factors in parents with higher socioeconomic level were eliminated (19). Smoking is not advised during pregnancy. When the family has a newborn baby in the house, it is not recommended to have a pet. In addition, breastfeeding should not be discontinued prematurely. Although such risks are eliminated, allergic rhinitis may develop in children with a high socioeconomic status because the “protective” effect of exposure to bacteria is also eliminated (20). In our study, the socioeconomic level was not included in the questionnaire. This factor was not examined because it would not be proper and realistic to investigate the net income or education level of the family as the questionnaire survey was given to children aged 12 to 15 years. Socioeconomic levels in the Trabzon city center, where the study was conducted, did not vary considerably. Furthermore, the investigation would cause classification or grouping among the children in this age group who would enter into the period of adolescence.
Internal environment pollutants such as nitrogen oxides, carbon monoxide, and sulfur dioxide were risk factors for respiratory tract allergies, and it was known that the main sources for nitrogen dioxide and carbon monoxide were the heating stoves and furnaces (7). When the relationship between allergic rhinitis and heating methods, which was accepted as a risk factor, was considered, the incidence of allergic rhinitis in people using wood heaters (17.2%) was found to be higher than that in people using other types of heating sources (13.8%). However, this difference could not be construed as being statistically significant.
The Trabzon Province is surrounded by high mountains from the sea level toward inner areas in the Eastern Black Sea region. Trabzon is the largest city in the Black Sea Region. Geographical features, climate, and vegetation of Turkey vary considerably. As a natural result of this fact, the climate of every region and, accordingly, aeroallergens vary. In the study conducted by Ayvaz et al. (21) regarding seasonal distribution of aeroallergens in the atmosphere of Trabzon, aeroallergens consisted of pollens of trees and woody plants (59.2%) and herbaceous plants (40.8%). In this study, the most frequently encountered aeroallergens according to the annual average were Corylus (nut) (17.9%), Poacea (graminae) (13.6%), Pinus (pine) (7.9%), and Alnus (alder) (5.3%). According to the pollen calendar, in our region, pollens were mostly encountered in June (21).
In Trabzon, where the Black Sea climate is dominant, summer is cool, winter is relatively warm, and it is rainy every season (22). Major differences in temperature or sharp transitions between the seasons are not observed within the year. As a reflection of this, in our questionnaire, when we examined persistent allergic rhinitis symptoms according to seasons, a statistical significance could not be observed between seasonal differences and symptoms (p=0.112). We considered that this result was associated with less temperature transitions between the seasons and the absence of very dense winds or very arid climates.
However, when we observed the allergens according to the seasons and considered the responses of the children with allergy to questionnaire items in the main weed group and main prairie group in the skin prick test results, we saw that allergens were more important in spring (p<0.001).
Another factor questioned for allergic rhinitis in our study was the “quality of the house.” Allergic rhinitis was diagnosed in a significant number of students living in an apartment flat in comparison with those living in a house (p=0.015). This was also, as specified in the study of Tomaç et al. (9) in Zonguldak and in the study of Selnes et al. (11) in Norway, supported by the theory that allergic rhinitis was more frequently observed in children living in an apartment flat than in children living in a house or a closed area for a long time in bigger city centers with more air pollution, termed as “West type living” (18).
The results of studies in which allergic rhinitis and pet feeding relationship was evaluated have also demonstrated variations. In the questionnaire study of Kalyoncu et al. (23) on 4639 university students and in the study of Gysel et al. (14) and study of Mösges (19), a significant relationship between pet feeding in the house and allergic rhinitis was observed, but in the other studies conducted in our country, no such relationship was observed (8–10). In our study, the correlation between pet feeding in the house and allergic rhinitis was significant (p=0.04).
In the literature, different results have been oberved in studies that were conducted on the age of mothers and allergic rhinitis. In the ECRHS questionnaire survey study of Laerum et al. (24) in Norway performed on 16190 patients between 23 and 54 years of age who visited the chest diseases clinic, it was revealed that a relatively younger age of the mother was related to asthma rather than rhinitis. In the questionnaire study of Szu-Pin-Hsu et al. (25) in Taiwan, the authors specified that there was no significant relationship between the age of mothers and allergic rhinitis in 368 study participants aged between 6 and 13 years. The mean age of the mothers of 182 students diagnosed with allergic rhinitis was 25.5±5.1 years, while mean age of the mothers of 966 students without allergic rhinitis was 26.1±4.7 years. The difference between these two values was not significant (p=0.163).
The findings of skin prick tests were evaluated, and the most common allergens at Trabzon city center were specified as D. pteronyssinus and D. farinae, which are also known as house dusts or mites. This was followed by allergies against the main prairie group and main tree group. Such values were deemed as compatible to the values reported in the literature.
The main prairie group and main tree group were frequently seen as allergens responsible for intermittent allergic rhinitis. While the studies conducted in our country had similar findings as our results, the clinical picture was different from that in the studies conducted in other countries. In a study of Prasad et al. (26) in India, the most common allergens detected in the prick test study performed on 48 patients with nasobranchial allergy were insects, mites, and pollens, in decreasing order of frequency.
Conclusion
To our knowledge, this is the first prevalence study in this age group in Trabzon, which is the largest settlement in the Eastern Black Sea Region. Our findings determined the prevalence of allergic rhinitis in this region to be 14.5%. For allergic rhinitis, female gender, smoking habit of parents, owning pets, and living in a flat were significant potential risk factors. Sharing bedroom with one or more people, using wood burning stove as the heating system and older age of the mother at delivery were found to increase the likelihood of having allergic rhinitis, but the difference was not significant. Further research with larger sample sizes would be a promising next step to reveal the impact of these risk factors on the development of allergic rhinitis.
Footnotes
This study was presented at the 32nd National Otorhinology Head and Neck Surgery Congress as an oral presentation, 27–31 October 2010, Antalya, Turkey.
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Karadeniz Technical University (file no:2009/36).
Informed Consent: Written informed consent was obtained from patients’ parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - H.B.Ç.; Design - H.B.Ç. Supervision - A.I.; Materials - H.B.Ç.; Data Collection and/or Processing - M.T., H.B.Ç.; Literature Search - H.B.Ç.; Writing Manuscript - H.B.Ç.; Critical Review - A.U.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Keleş N. Alerjik rinitte medikal tedavi. Kulak Burun Boğaz Cerrahisinde Güncel Yaklaşım-Allerjik Rinosinüzitler. 2005;1:48–52. [Google Scholar]
- 2.Durham SR. Scott Brown’s otolaryngology. 6th edition. Vol. 4. London: Butterworth; 1997. Mechanisms and treatment of allergic rhinitis; pp. 10–15. [Google Scholar]
- 3.Keleş N. Alerjik rinit. In: Koç C, editor. Kulak Burun Boğaz Hastalıkları ve Baş-Boyun Cerrahisi. Ankara: Güneş Tıp Kitabevleri; 2013. pp. 681–69. [Google Scholar]
- 4.Europian community respiratory health survey web site. Available from: http://www.ecrhs.org.
- 5.King CK, Mabry RL, Mabry CS. Allergy in ENT Practise: A Basic Guide. Thieme Medical Publishers; New York: 1998. pp. 143–64. [Google Scholar]
- 6.Kalyoncu AF. Perennial and seasonal rhinitis in Ankara, Turkey. Allergy. 1997;52:1040–1. doi: 10.1111/j.1398-9995.1997.tb02431.x. [DOI] [PubMed] [Google Scholar]
- 7.Zeyrek CD, Zeyrek F, Sevinç E, Demir E. Prevalence of asthma and allergic diseases in Şanlıurfa, Turkey, and the relation to enviromental and socioeconomic factors: is hygiene hypothesis enough? J Invesstig Allergol Clin Immunol. 2006;16:290–5. [PubMed] [Google Scholar]
- 8.Yuksel H, Dinç G, Sakar A, Yılmaz O, Yorgancıoğlu A, Çelik P, et al. Prevalence and comorbidity of allergic eczama, rhinitis and asthma in a city in Western Turkey. J Investig Allergol Clin Immunol. 2008;18:31–5. [PubMed] [Google Scholar]
- 9.Tomaç N, Demirel F, Acun C, Ayoğlu M. Prevalence and risk factors for childhood asthma in Zonguldak, Turkey. Allergy and Asthma Proc. 2005;26:397–402. [PubMed] [Google Scholar]
- 10.Tamay Z, Akçay A, Ones Ü, Güler N, Kılıç G, Zincir M. Prevalence and risk factors for allergic rhinitis in primary school children. Int J Pediatr Otorhinolaryngol. 2007;71:463–71. doi: 10.1016/j.ijporl.2006.11.013. http://dx.doi.org/10.1016/j.ijporl.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Selnes A, Nystad W, Bolle R, Lund E. Diverging prevalence trends of atopic disorders in Norwegian children. Results from three cross-sectional studies. Allergy. 2005;60:894–9. doi: 10.1111/j.1398-9995.2005.00797.x. http://dx.doi.org/10.1111/j.1398-9995.2005.00797.x. [DOI] [PubMed] [Google Scholar]
- 12.Bauchau V, Durham SR. Prevalence and rate of diagnosis of allergic rhinitis in Europe. Eur Respir J. 2004;24:758–64. doi: 10.1183/09031936.04.00013904. http://dx.doi.org/10.1183/09031936.04.00013904. [DOI] [PubMed] [Google Scholar]
- 13.Alsowaidi S, Abdulle A, Shehab A, Zuberbier T, Bernsen R. Allergic rhinitis: prevalence and possible risk factors in a gulf Arab population. Allergy. 2010;65:208–12. doi: 10.1111/j.1398-9995.2009.02123.x. http://dx.doi.org/10.1111/j.1398-9995.2009.02123.x. [DOI] [PubMed] [Google Scholar]
- 14.Van Gysel D, Govare E, Katia MC, Doli E, Baets F. Messages from the Aalst Allergy Study. World J Pediatr. 2009;5:182–90. doi: 10.1007/s12519-009-0035-0. http://dx.doi.org/10.1007/s12519-009-0035-0. [DOI] [PubMed] [Google Scholar]
- 15.Floreani AA, Rennard SI. The role of cigarette smoke in the pathogenesis of asthma and as a triger for acute symptoms. Curr Opin Pulm Med. 1999;5:38–46. doi: 10.1097/00063198-199901000-00007. http://dx.doi.org/10.1097/00063198-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Kurt E, Metintaş S, Başyiğit İ, Bulut İ, Coşkun E, Dabak Ş, et al. Prevalence and risk factors of allergies in Turkey: Results of a multicentric cross-sectional study in children. Pediatr Allergy Immunol. 2007;18:566–74. doi: 10.1111/j.1399-3038.2007.00551.x. [DOI] [PubMed] [Google Scholar]
- 17.Zuraimi M, Tham KW, Chew P, Ooi L, David O. Home exposures to environmental tobacco smoke and allergic symptoms among young children in Singapore. Int Arch Allergy Immunol. 2008;146:57–65. doi: 10.1159/000112503. http://dx.doi.org/10.1159/000112503. [DOI] [PubMed] [Google Scholar]
- 18.Keil T, Lau S, Roll S, Gröber C, Nickel R, Niggemann B, et al. Maternal smoking increases risk of allergic sensitization and wheezing only in children with allergic predisposition: longitudinal analysis from birth to 10 years. Allergy. 2009;64:445–51. doi: 10.1111/j.1398-9995.2008.01867.x. [DOI] [PubMed] [Google Scholar]
- 19.Mösges R. The increasing prevalence of allergy: a challenge for the physician. Clin Exp All Rev. 2002;2:13–7. http://dx.doi.org/10.1046/j.1472-9725.2002.00029.x. [Google Scholar]
- 20.Strachan P, Cook G. Parental smoking and allergic sensitisation in Children. Thorax. 1998;53:117–23. doi: 10.1136/thx.53.2.117. http://dx.doi.org/10.1136/thx.53.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayvaz A, Baki A, Doğan C. Trabzon atmosferindeki aeroallerjenlerin mevsimsel dağılımı. Astım Alerji İmmunoloji. 2008;6:11–6. [Google Scholar]
- 22.Bayramoğlu E. Trabzon İlinde İklim Değişikliğinin Mevsimsel Bitki Su Tüketimine Etkisi: Penman-Monteith Yöntemi. Kastamonu Üni., Orman Fakültesi Dergisi. 2013;13:300–6. [Google Scholar]
- 23.Kalyoncu AF, Demir AU, Özçakar B, Bozkurt B, Artvinli B. Asthma and allergy in Turkish university students: two cross-sectional surveys 5 years apart. Allergol Immunopathol. 2001;29:264–71. doi: 10.1016/s0301-0546(01)79068-4. http://dx.doi.org/10.1016/S0301-0546(01)79068-4. [DOI] [PubMed] [Google Scholar]
- 24.Laerum B, Svanes C, Wentzel-Larsen T, Gulsvik A, Tore’n K, Norrman E, et al. Young maternal age at delivery is associated with asthma in adult offspring. Respiratory Medicine. 2007;101:1431–8. doi: 10.1016/j.rmed.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 25.Hsu Szu-Pin, Lin Kai-Nan, Tan Ching-Ting, Lee Fei-Peng, Huang Hung-Meng. Prenatal risk factors and occurrence of allergic rhinitis among elementary school children in an urban city. Int J Pediatr Otorhinolaryngol. 2009;73:807–10. doi: 10.1016/j.ijporl.2009.02.023. http://dx.doi.org/10.1016/j.ijporl.2009.02.023. [DOI] [PubMed] [Google Scholar]
- 26.Prasad R, Verma SK, Dua R, Kant S, Kushwaha RA, Agarwal SP. A study of skin sensitivity to various allergens by skin prick test in patients of nasobronchial allergy. Lung India. 2009;26:70–3. doi: 10.4103/0970-2113.53228. http://dx.doi.org/10.4103/0970-2113.53228. [DOI] [PMC free article] [PubMed] [Google Scholar]