Abstract
In many health care systems globally, cancer care is driven by multidisciplinary cancer teams (MDTs). A large number of studies in the past few years and across different literature have been performed to better understand how these teams work and how they manage patient care. The aim of our literature review is to synthesize current scientific and clinical understanding on cancer MDTs and their organization; this, in turn, should provide an up-to-date summary of the current knowledge that those planning or leading cancer services can use as a guide for service implementation or improvement. We describe the characteristics of an effective MDT and factors that influence how these teams work. A range of factors pertaining to teamwork, availability of patient information, leadership, team and meeting management, and workload can affect how well MDTs are implemented within patient care. We also review how to assess and improve these teams. We present a range of instruments designed to be used with cancer MDTs – including observational tools, self-assessments, and checklists. We conclude with a practical outline of what appears to be the best practices to implement (Dos) and practices to avoid (Don’ts) when setting up MDT-driven cancer care.
Keywords: cancer MDT, MDM, cancer meeting, patients with cancer
Introduction
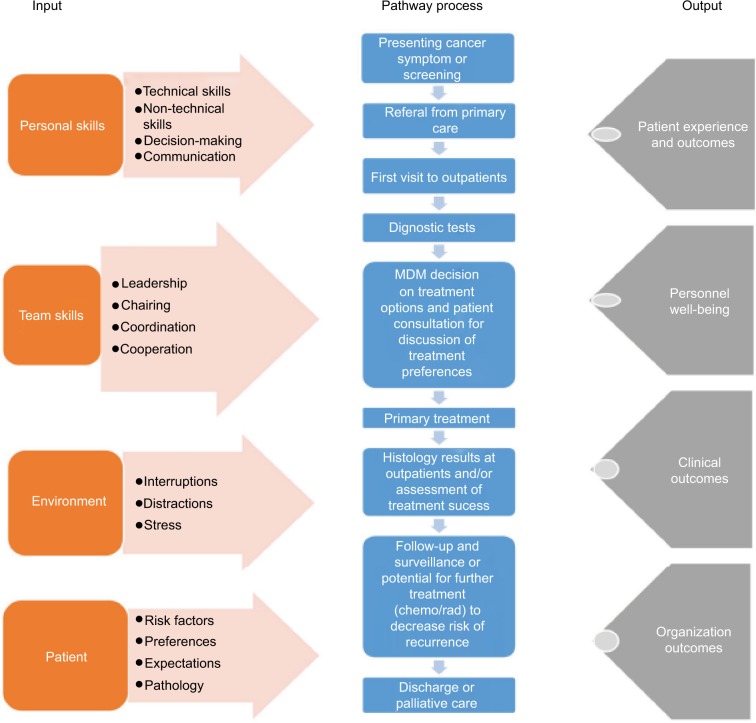
The concept of multidisciplinary team (MDT) working is widely accepted as the “gold standard” of cancer care delivery across the world. The cancer MDTs, and MDT meetings (MDMs) in particular, are at the center of an increasingly complex health care system. Figure 1 offers our conceptualization of modern MDT-driven care, which we apply to an extent to the rest of this paper. Effective MDT-driven care depends on a multitude of inputs (individuals, teams, environment, and patients) and processes (interactions, tests, results). It subsequently results in a range of outputs (patient experience, outcomes, organizational outcomes), which taken together are aspired to achieve high-quality, efficient care for patients.
Figure 1.
A systems model approach to improve the delivery of cancer care representing the cancer pathway with the MDM embedded within it, and various inputs and outputs that affect the whole of the pathway, along with the factors that can impact on the inputs (in the arrows).
Abbreviations: Chemo, chemotherapy; rad, radiotherapy; MDM, multidisciplinary team meeting.
The literature describing MDT working in cancer care is diverse and increasing in scope and volume with an increasing number of systematic1–3,8 and other reviews.4 The field is growing, as many disciplines alongside traditional health care effectiveness reviewing methodology are becoming involved in understanding MDT working, including psychology, improvement science, organizational science, and others. The diversity of the evidence base in itself presents a challenge to health care professionals, patients and their advocates, as well as those involved in health care organization, who want to improve the care of patients with cancer.
There is, therefore, need for the diverse evidence we have on what “works” in implementing MDTs in cancer care and what factors impact on care delivery to be reviewed in an integrated manner. This is what the present review aims to achieve in offering an integrative overview of diverse studies on cancer MDTs and their functioning. Specifically, the aim of our literature review is to synthesize current scientific and clinical understanding on cancer MDTs and their organization; this, in turn, should provide an up-to-date summary of the current knowledge that those planning or leading cancer services can use as a guide for service implementation or improvement.
Methods
In order to identify the relevant literature, we undertook a literature search of PubMed using the search terms “decision-making”, “cancer”, “multidisciplinary”, and “team”; we also hand-searched studies by consulting with experts in the field and by scrutinizing reference lists of retrieved papers, existing reviews, guidelines, and governmental documents. The search was limited to human beings, English language, and dates of publication ranging from 1999 to September 2017.
Overview of evidence
The retrieved evidence is organized into the following five domains that appear critical for effective cancer MDT working:
Background to multidisciplinary teams in cancer care.
Key performance indicators of effective teams and their meetings.
Factors that are known to affect team processes.
Assessment of cancer MDT working.
Improvement of cancer MDT working and its impact on patient care.
Background to multidisciplinary teams in cancer care
Cancer MDTs are made up of surgeons, oncologists, radiologists, pathologists, specialist cancer nurses, physicians, and meeting coordinators who usually meet on a regular basis (e.g., weekly) in cancer MDMs in order to discuss and agree on the care plan for patients with suspected or confirmed cancer. One of the core team members, often the MDT lead, tends to also chair the meeting, although variations between teams exist, with some not having a chair. The diagnosis and treatment of cancer involves a complex care pathway.5 To ensure consistency, the UK’s Department of Health6,7 has made MDMs obligatory in order to ensure reliable and equitable delivery of safe and high-quality care that is necessary to improve patient outcomes – to all cancer patients. The MDM (sometimes termed a cancer conference or tumor board) is thus an integral part of cancer care services in the UK, where it is embedded in the cancer care pathway (Figure 1) and in other countries globally. It is intended to improve the consistency and quality of cancer care locally, regionally, and nationally. Even in countries where MDMs are not mandated, a need for a multi-team system for effective coordination of cancer care has been identified.1
The efficacy of the MDT-based approach to cancer care is poorly understood, however. Indeed, the empirical evidence for MDMs is mixed and unclear,8 and their impact on patient outcomes, and in particular on the survival of patients with cancer, is uncertain. For instance, one study showed improvement in survival of patients with inoperable lung cancer from 3.2 to 6.6 months as a result of MDTs, although the authors noted that this could be due to other factors as well since cancer care is complex.9The MDT approach was found to encourage positive changes to care management,10 where it was found to outperform diagnostic tests11 and lead to modification of diagnosis.12Other researchers, however, have found no difference in diagnosis pre- and post-MDM review.13,14More recently, research has also focused on MDMs identifying and improving various aspects of MDM working, such as the quality and efficacy of clinical decisions using methodologies ranging from surveys and interviews to observation and checklists (see also Table 1 for a list of tools available to assess MDTs that was generated from this evidence base).8,15–17
Table 1.
A list of instruments used to assess and improve MDT working
| Instrument (authors or source) | Brief instrument description | Instrument methodology |
|---|---|---|
| MDT-OARS (Taylor et al24) | “The MDT Observational Assessment Rating Scale” assesses 18 elements of good team functioning as expressed in national UK guidance | Observation |
| TEAM (Taylor et al49) | “The Team Evaluation and Assessment Measure” assesses core functions of the team and their team meetings, based on the components defined in “the characteristics of effective MDT” | Team self-assessment |
| MDT-QuIC (Lamb et al65) | “The MDT Quality Improvement Checklist” is designed to aid decision-making in MDMs by ensuring that all aspects of a case are reviewed by the team | Checklist |
| MDT-MODe (Lamb et al43) | “The MDT Metric of Decision-Making” measures the quality of presented patient information, contribution to case review per specialty, and team ability to reach a decision in the team meeting | Observation |
| MDT Quality Improvement Bundle (Lamb et al22) | A team improvement bundle including checklist application, team skills brief training, and guidance implementation | Quality improvement bundle |
| MDT-MOT (Harris et al48) | “The MDT – Meeting Observational Tool” assesses team attendance, leadership/chairing of the MDM, teamwork and culture | Observation |
| MDT-FIT www.mdtfit.co.uk 66 | “The MDT Feedback for Improving Team Working” encompassing validated components of MDT-MOT and TEAM allows self-assessment of team working, combined with expert feedback from facilitator, and sharing of the outcome with the team as part of a team-reflective discussion | Team self-assessment and observation |
Abbreviations: FIT, feedback for improving team-working; MDM, multidisciplinary team meeting; MDT, multidisciplinary team; MODe, metric of decision-making; MOT, meeting observational tool; OARS, Observational Assessment Rating Scale; TEAM, Team Evaluation and Assessment Measure.
One reason for inconsistent results in research examining the functioning of cancer MDMs, however, could be the fact that novel treatments, technology, and service changes have all evolved in parallel to MDMs and potentially have confounded the findings.15 What is more, designing studies to assess effectiveness has proven difficult; for instance, in the UK, MDMs are mandatory in cancer care and, therefore, orthodox comparative studies, i.e., randomized controlled trials, are not possible.15,16 In addition, implementation of the MDT model of care in itself has some inherent variations since it relies on health care providers delivering it at the frontline, and this introduces human factors into the equation. For instance, in MDMs, decision-making process, team working and interactions, leadership (including chairing), team climate, treatment implementation, team ability to reach a care plan on a first case-presentation, and also waiting times, appropriate use of resources including technologies, as well as patient and health care professional satisfaction with care and quality of life, could be further examined.15,16,18 Periodic survival evaluation of the population as a whole as well as prospective longitudinal studies of treatment implementation may also be useful indicators of team effectiveness.19
It is, therefore, crucial to advance our understanding of the intended advantages of MDMs through the in-depth study of the behaviors, processes, context, and organization of this approach to patient care.19–22
Performance indicators of effective teams and their meetings
For a number of years after the inception of MDTs, there was an absence of empirical evidence about the potential factors that made MDTs effective. This changed in 2010 when the National Cancer Action Team (NCAT) in England defined indicators for highly functioning MDTs, termed “the characteristics of an effective MDT”,23 including effective team meetings (these characteristics are outlined in Table 2). This definition was based on data from a national survey of over 2000 MDT members’ perceptions of effective MDT working. Responses showed that 90% of respondents were in agreement that an effective MDM results in improved clinical decision-making, more coordinated patient care, improvement in overall quality of care, more evidence-based treatment decisions, and improved treatment. NCAT recommended assessing areas of team meetings such as team working and leadership. Key performance indicators have subsequently been generated from the NCAT document to serve as a benchmark against which MDTs can appraise and develop their practice.23
Table 2.
Characteristics of an effective multidisciplinary team for cancer patients
| I. The Team |
| • Level of expertise and specialization |
| • Attendance of MDMs |
| • Leadership (e.g., chair or leader of the MDMs) |
| • Team working and culture (e.g., mutual respect and trust, equality, resolution of conflict, constructive discussion, absence of personal agendas, ability to request, and provide clarification) |
| • Personal development and training |
| II. Infrastructure for MDM |
| • Appropriate meeting room |
| • Availability of technology and equipment |
| III. MDM organization |
| • Regular meetings |
| IV. Logistics |
| • Preparation for meetings |
| • Organization during meetings |
| • Post-meeting coordination of services for the patient |
| V. Patient-centered clinical decision-making |
| • Who to discuss, i.e., having local mechanisms in place to identify all patients where discussion at MDM is needed |
| • Patient-centered care (e.g., patient’s views and preferences are presented by someone who has met the patient, and the patient is given sufficient information to make a well-informed decision on their treatment and care) |
| • Clinical decision-making process |
| • The information the team needs to make informed decisions/recommendations at team meetings are as follows: pathological, radiological, comorbidities, psychosocial, palliative care needs, patient history, and patient views |
| • The decisions/recommendations at team meetings need to be evidence-based (in line with NICE and/or cancer network guidelines), patient-centered, and in line with standard treatment protocols (unless there is a good reason against this) |
| VI. Team governance |
| • Organizational support (e.g., funding and resources) |
| • Data collection during team meetings, analysis, and audit of outcomes (e.g., patient experience surveys); the results of these investigations are fed back to MDTs to support learning and development |
| • Clinical governance (e.g., there are agreed policies, guidelines, and protocols for MDTs; performance assessment and peer review against similar MDTs using cancer peer review processes and other tools) |
Abbreviations: MDM, multidisciplinary team meeting; MDT,multidisciplinary team; NICE, National Institute for Health and Care Excellence.
Moreover, the responses from the NCAT national survey were further analyzed by Lamb et al.15 They revealed high agreement between different cancer teams (116 out of 136 agreements) in terms of what constitutes effective MDT working. Nonetheless, subtle variations in team working and clinical decision-making were evident across different tumor types and in relation to the preparation for and organization of MDMs, case selection, and clinical decision-making process.15
The “characteristics of an effective MDT” were further examined a few years later by Taylor et al49 while developing a series of teamwork formative assessment tools: MDT MOT, TEAM, and MDT FIT (Table 1). When testing these tools, Taylor et al49 confirmed the robustness of the characteristics as a benchmark that was applicable to rarer cancers (such as pediatric, brain, and hematology) in teams that faced challenges or complex situations and in MDMs that video-conferenced using multiple sites.49,24
More recently in 2017, a Cancer research UK report on cancer MDTs reiterated that team members expressed a high regard for MDMs, their structure, and process.25 The majority of participants valued the meetings stating that they not only facilitated patient care but also saved them considerable time elsewhere in their clinical or administrative practice.
Factors that are known to affect team processes
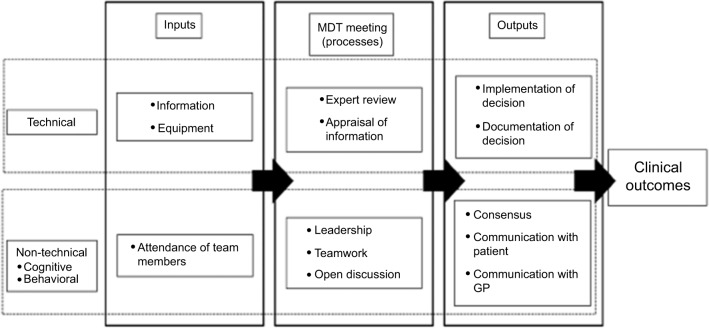
A number of studies have explored factors that have an impact on how well cancer MDMs function; these are related to the “input” element of the input-process-output diagram presented in Figure 1. Research into their working was greatly advanced by Lamb et al who developed a systems approach in 2010 to understand the multiple factors that can affect MDMs (Figure 2).26 This ordered structure was then used as a basis for assessing the efficient functioning of an MDM and designing assessment tools for MDMs to improve team working and the delivery of cancer care (Table 1). They also performed content analysis on the responses to free-text (open) questions pertaining to the effectiveness of MDM working from the 2009 national survey of MDT members in the UK.27 These questions covered three topics: effective team-working in the meetings, efficacy of team decision-making, and patient centeredness. This analysis aimed to further define aspects of effective team working in MDMs, with an emphasis on the similarities and differences in views between different professional groups.
Figure 2.
A systems approach to describe and evaluate the functioning of an MDM. Reprinted from Surgical Oncology. 2011;20(3):163–168. Lamb BW, Green JSA, Vincent C, Sevdalis N. Decision making in surgical oncology with permission from Elsevier.26
Abbreviations: GP, General Practitioner; MDM, multidisciplinary team meeting; MDT,multidisciplinary team.
The authors raised specific questions/issues regarding MDM functioning that could provide an evidence base on which MDTs can develop their practice. Specific areas highlighted included the following: 1) how best to represent patients’ views in MDM, 2) how disagreements within the team should be dealt with, and 3) what are the factors that facilitate participation in the decision-making process in team meetings, including organizational (e.g., lack of time to prepare) and interpersonal factors (e.g., steep hierarchies and lack of trust or respect between team members). It is argued that failure to optimize these factors can have an effect on clinical decision-making and could account for the variability seen in how well MDMs work.
Another contribution to our understanding of the factors that affect the impact of cancer MDTs on patient care comes from a systematic review8 performed on 37 studies published between 2000 and 2008. It was found that MDTs failed to reach a decision for 27%–52% of cases and that when decisions were made they could not be implemented in 1%–16% of cases. The study showed that 1) care management decisions are made predominantly by medical personnel (usually surgeons), while nursing personnel have less of an active role in decision-making and defining treatment options, and patient preferences are rarely discussed and 2) time pressure (including lack of protected time to prepare for meetings), excessive caseload, low attendance, poor team working, and lack of leadership lead to lack of information and deterioration of decision-making. Some of these factors were reiterated in the 2017 Cancer Research UK (CRUK) report (time pressure, expanding workload, and lack of protected time) nearly 10 years later.23
In what follows, we describe in detail the factors affecting MDT working, including factors that impact on MDMs as per “input” in Figure 1.
Personal and team skills
Good relationships between team members and adequate non-technical skills are important for smooth effective MDT functioning (i.e., communication and leadership). In particular, communicating effectively with colleagues at various levels of hierarchy and managing conflict within teams are recognized as key contributors to safe, high-quality care delivery across specialities.23 However, evidence shows unequal participation in discussions on treatment options with medical personnel (including, e.g., oncologists and surgeons) tending to base their care management decisions primarily on biomedical information, seldom considering patient choice. It was also shown that nurses contribute to the meetings with the information about the patient’s views and psychosocial aspects of care, although traditional professional hierarchies often lead to the exclusion of nurses and bias toward biomedical information.8,27 An interview study exploring the views of surgeons, oncologists, nurses, and administrators on various characteristics of MDMs has found that patient discussions do not encompass the contributions of different disciplines equally, i.e., nurses are underrepresented and surgeons, who dominate discussion, are biased toward biomedical information.
Effective leadership of an MDT, which includes chairing of team meetings, can play an important role in ensuring equality and inclusiveness of participation that may enable better decision-making. Nontechnical skills (e.g., communication skills) as well as clinical expertise were cited as key characteristics of an effective meeting chair. Training in nontechnical skills may be of benefit, in particular because the chair does not necessarily need to be a surgeon since other core members with adequate skill could take on this role.28 Some of the best MDMs observed during the development phase of the MDM assessment tools mentioned earlier (Table 1) were chaired by specialist cancer nurses – core team members in MDMs.
When nurses are actively involved in care planning in the meetings, the team is perceived as performing at a higher level. Similarly, teams report that presence of nursing staff and larger and more diverse teams is associated with increased effectiveness.8,29 Nurses tend to involve patients’ views in the decision-making process more than medical personnel do. This is important since only 4% of MDM discussions involve patient’s holistic information directly in the decision-making process.29 In addition, evidence shows that decisions that take into account patients’ preferences, performance status, and comorbidities are more likely to be implemented since such decisions are more clinically appropriate and acceptable to patients.30,31,27 A more recent study showed that a complete patient profile (including, the biomedical aspects of the disease, as well as the information on patients’ co-morbidities, their psychosocial aspects, and views on treatment options), and input into the discussion by all core disciplines (including, the nurses’) are essential for the team to formulate a treatment recommendation for a patient.18,32 And the need for a higher level information on patient comorbidities and nursing input may actually be indicators of more complex discussions18 and validates the inclusion of specialist cancer nurses in the core membership of the MDMs.
The coordinators in cancer MDMs (for systems that afford this role within the team) also have an important role in improving the quality of care delivered by MDTs through their effect on team effectiveness and climate. However, their administrative role, as an intrinsic part of the cancer team, is often undervalued. The job is often used as an initial entry into working in the health system and many of the coordinators, therefore, have little previous health service experience. A survey has found that coordinators feel that their job plan does not reflect their actual duties.33 They identified needs for further areas of training in oncology, anatomy, physiology, and leadership skills to improve their team performance and consequently cancer care. Their role is central to the care of patients, both locally and through the coordination and sharing of data on wider level. Since coordinators role is pivotal in MDMs, it is important to devise and provide them with adequate training in order to improve team performance as a whole, something further research could focus on.33
Another issue raised by Lamb et al27 was the importance of recording the disagreements when they occur and potentially discussing them with the patient. Although disagreements are uncommon in MDMs, dissent is not detrimental to a team as it can enhance critical thinking and evaluation during decision-making. However, teams that do not tend to dissent are at risk of “group think”, where disagreement exists but are not openly expressed; this may indicate poor team climate and lack of open communication within a team that can lead to poor decision-making. Within an MDM, ensuring open communication where dissent is acknowledged and effectively managed may be a key element of the chair’s role. Further research is nonetheless needed to evaluate how often and where dissent occurs in meetings and how it should be managed and collated and how it should be communicated to the patient.27
Team members report that MDMs are generally highly positive with an open culture for discussion, optimal management plans, coordinated treatment, and low risk of error. Moreover, a rotating leadership, which refers to team members taking turns at chairing the meeting, was found to be highly effective in terms of improving team work and team morale and reducing inter-professional conflict, although MDMs are most commonly led by surgeons. However, the role of the chair is unequally (and irregularly) distributed across disciplinary groups within a MDM, although, disciplines other than surgeons may be able to undertake this role..8
To illustrate this fact, a recent study from Scotland, examining the efficacy of a specialist nurse leading a cancer MDT by comparing clinical outcomes, showed that the nurse-led MDT performed as well if not better than other local units with comparable resources and patient population led by surgeons.35 Other disciplines such as oncology have high levels of contribution to MDM decision-making. But regarding their role in leadership, when surveyed, they thought that they could chair the team meeting as readily as any other professional group. However, they are not taking leadership role at the level that they expect; for example, only one in four oncologists has been chair of the MDT they attend and <40% of the MDMs they attend have a rotating chairmanship, further reducing the opportunity to lead. This prospect is further complicated by the finding that the oncologists who responded tend to participate in at least three MDMs, placing more demand on their time and ability to prepare and attend.18
It may, therefore, be useful to have a clinically noncontributing member chair the meeting to avoid detriments in performance as a result of a dual-task interference, as the job of chairing the meeting, by a clinician, has the potential to diminish the contribution that the clinician can then make to decision-making, during the meeting.18
Environment
While non-technical skills are important, they are not sufficient on their own. Support at an organizational level is also important in the form of protected time in the participants’ job plans to prepare for, attend, and take action on the workload of the meeting. Lamb et al34 found that lack of protected time for team meetings and competing demands or frequent conflicts with other responsibilities were barriers to effective meetings. In particular, team members without protected time for meetings were less likely to attend,27 and that the most frequently cited organizational improvement to MDT working was more time dedicated to prepare for and attend the MDM.25 Further research or audit is needed at an organizational level to ensure that protected time is available and supported organizationally.27,25
Excessive time pressure and lack of, or inadequate, information available at the time of decision-making (including imaging, investigations of tumor stage, review of pathology, and comorbidities) was found to negatively affect team ability to reach definitive care management plan, and lower team morale, resulting in reduced attendance and rushed decision-making. Compounding this, lack of protected time for MDMs to prepare for meeting contributes to excessive workload, time wasting during meetings, and inefficiency.8,25
Technology and decision support systems also play an important role. Telemedicine improves meeting attendance and it is cost-effective. However, it can slow down the team by reducing the number of patient discussed per meeting34 and can negatively affect team’s decision-making.16
Patient
Lack of patient-centered information presents a barrier to decision-making too; that is, failure to consider such information inhibits decision-making, renders decisions clinically inappropriate or unacceptable to patients, and is therefore detrimental to patient care.27 Patients should be represented by team members who know them well. Findings suggest that the clinical nurse specialist is the preferred team member to represent the patients’ views in meetings, but consultant and attending surgeon or other members could also share the duty. Having patients present in MDMs might arguably inhibit the process; hence discussions between the patient and team members following the main MDT discussion may be preferable.27 Nonetheless, patient-centeredness is important; a more recent study showed that patient psychosocial information is a significant predictor of team ability to reach a decision32 and that a complete patient profile is needed for the treatment recommendation to be formulated.18
Further research is needed to gain better understanding of how to best integrate patient-centered information into MDM decision-making – a task that is not necessarily straightforward. This is because patient preferences will vary according to the disease itself, personal values, and circumstances.27 Moreover, it is not clear whether it is in the patient’s best interest that their preferences form part of the decision-making process or whether the team should initially discuss clinical options before patient preferences are considered.27 In addition, any preferences patients express before the full MDM might change according to the advice and reflections emanating from the meeting.27
As a final point, Jalil et al16 investigated views of expert urology and gastrointestinal cancer service providers in relation to the effectiveness of their MDMs in reaching a decision for each patient, with a particular emphasis on identifying the barriers to implementing MDT decisions into patient care and how these can be overcome. The researchers used semi-structured interviews with MDT members of urological and gastrointestinal tumors. It was found that 92% of patient management plans are formed at MDMs and 95% of these are subsequently implemented. The list of factors impacting decision-making and implementation and those that can help improve it are given in Table 3.
Table 3.
A list of factors impacting and improving decision-making and implementation
| I. Factors impacting decision-making and implementation |
| • Lack of necessary information |
| • Lack of considerations of patient comorbidities, choices, and disease progression |
| • Non-attendance of key team members (as this can delay the decision and/or making a decision without the key team member can lead to an inappropriate treatment plan) |
| • Time pressure, i.e., not enough time to discuss all the patients, and so some get deferred (this can also negatively impact the patients) |
| • Technological problems with video conferencing |
| II. Factors improving decision-making and implementation |
| • Better case preparation, e.g., with a pro forma |
| • Effective team leadership (and chairing) |
| • Involvement of an anesthetist in the MDM (to immediately discuss whether patient is fit for surgery) |
| • Not discussing all patients, i.e., refining the inclusion criteria for MDT discussion either by splitting MDM into smaller meetings (logistical difficulties with this approach) or by excluding patients that fall under clear protocol/guidelines (although outside mandatory practice, this should be considered in future) |
| • Inclusion of patients in MDMs – however, there are mixed findings as to the benefit to the patient, and due to practical difficulties, patients in the UK do not attend |
Abbreviations: MDM, multidisciplinary team meeting; MDT, multidisciplinary team.
Assessment of cancer MDT working
Studies show that MDM’s decision-making ability and the success in reaching a treatment plan when first reviewing a patient are good markers of the quality of teamworking.16,8,34,36 Teams’ choice of treatment and the implementation of these recommendations (rather than survival rates which are difficult to directly attribute to MDM working) can also be measured. Hence, a number of observational assessment tools have been designed to help measure and subsequently improve the impact of cancer MDMs on patient care. As such, observational approaches to MDM working are useful, feasible, and non-intrusive (i.e., do not intrude on patient time or add to team workload), providing an opportunity to perform out assessments in real-life setting and understand areas in which the MDMs are doing particularly well and those that need further improvement. Such approaches were developed on the backdrop of a growing tradition within health care for the use of observational evaluations of team skills and performance in both clinical environments, e.g., operating theaters,37 intensive care units,38 emergency departments,39 and within simulated settings.40 Overall, this is based on the premise that team assessment and feedback can help teams reflect on their own performance and improve their working.
However, observational methodology has its drawbacks. For example, it can be time consuming, lacks insight into what participants think or feel, lacks control over extraneous factors, can present with limited replicability, and poses a challenge for a researcher to be accepted (non-clinical researcher) or to distance themselves from the environment (clinical researcher). Using structured and validated observation instruments by trained observers and ensuring good interobserver reliability can help adequately address these drawbacks. This is important, because, on balance, observation of MDTs is an important methodological approach to study such complex organizational behavior and to help improve safety and quality. Table 1 presents a list and description of tools designed and used for assessing MDTs together with study examples.
In the past few years, numerous studies have been performed applying observational techniques to better understand, assess, and improve MDT working. A number of studies have used a validated observational tool, MDT-MODe (Metric for the Observation of Decision-making in cancer multidisciplinary teams), to assess decision-making processes across different specialties, including the breast, urology, lung and colorectal cancers.18,32,41,42,44–47 For instance, Lamb et al22 revealed that the ability of an MDT to reach a clinical decision was positively associated with high-quality comprehensive and necessary information available at the point of decision-making (from case history, radiology, pathology), team contribution, and cases that are discussed at the beginning of meetings. However, high-quality information and team contribution were positively correlated with the larger team size, higher number of cases per meeting, and longer case discussions. Furthermore, using MDT-MODe, Soukup et al18,22 found that a complete patient profile and representation by all core disciplines are necessary to maxi-mize the ability of an MDM to reach management recommendations for all cases. More recently, MDT FIT has been developed as a web-based self-assessment tool for use by UK cancer teams to assess themselves locally and regionally by using validated instruments such as MDT MOT48 and TEAM49embedded within them (Table 1).
In addition, there are developed and validated instruments within the social sciences that, although have not been specifically developed for cancer MDMs, could be profitably used in this context. For instance, the Team Climate Inventory,46 a short questionnaire, can provide insight into individual members’ perspectives of their team dynamics and has been successfully used with cancer MDTs.17 Bales Interaction Process Analysis51 is an observational coding system developed with small groups engaged in a problem-solving task (a context that resembles MDMs). It measures socioemotional (e.g., showing solidarity or tension) and task-related areas (e.g., giving suggestions and asking for opinion), and it has been successfully used as an observational assessment tool with MDTs.50–54 Team interactions can also be assessed using conversation analysis, which allows detailed examination of communication between members from audio- or video-recorded data transcribed using Jefferson notation system55 that captures not only what is said but also how it was said with symbols indicating various aspects of talk, including intonation, pauses, overlaps, gaps, pace, loudness, and cut-offs, for instance. It has been previously used to study MDTs in the context of weekly meetings,56,57as well as in the operating theater.58,59 Overall, these are untapped translational resources that could be profitably used to gain better understanding of team processes and dynamics and allow effective assessment of different levels of MDT working.
Improvement of cancer MDT working and its impact on patient care
Some of the assessment tools described earlier has been used in intervention packages. For instance, Lamb et al22 performed an intervention study that encompassed the following: 1) half-day training session on the evidence for improved clinical decision-making followed by an interactive workshop and discussion, 2) MDT QuIC to support decision-making, 3) training session for surgical residents on how to use MDT QuIC to prepare and structure cases in advance of the team meeting, and 4) guidance to the team by providing hardcopy and via e-mail setting out how team members could draw optimal clinical information required for decision-making. These interventions were found to improve decision-making and the likelihood of the team formulating a clinical management plan, both necessary for high-quality patient care. Decision support tools, such as the MDT-QuIC, were also shown to improve patient care and increase compliance with clinical practice guidelines. MDT FIT, a self-assessment tool mentioned earlier, was also designed to be an intervention to improve cancer team working and thus ultimately the delivery of enhanced patient care. Since its inception, it has proven useful to all UK cancer teams that have used it and everyone has found areas for improvement.60
Based on the flourishing area of team assessment and improvement tools that have been developed and applied in the past few years, we are optimistic that interventions that combine best evidence as found elsewhere in health care, such as combinations of skills training and checklist application, possibly using simulation as a training approach61 will find their way into MDM improvement in the coming years.
Health services have changed significantly since MDTs were introduced 20 years ago. There has been a sustained increase in the workload of MDTs as a result of growing number of patients to be discussed in MDMs, along with the complexities of an aging population and growing number of treatment options available.25 The increase in the demand for MDT working has not been matched by greater availability of resources, with only minor increases in capacity seen. One potential solution, which has been identified by researchers and policymakers alike, is to streamline MDM working62,63,25 to allow more straightforward cases to assign less discussion time. This strategy might allow more time and resources in MDMs for discussion of complex or rarer cases, where patients have unusual or multiple problems requiring a truly multidisciplinary approach. Combined with the initiatives to improve the quality of MDT working, such a strategy, could help optimize the MDT approach for those patients in need of it.64
Summary
As a central part of the care pathway, cancer MDMs are a clinically valued resource allowing a diverse range of health care experts, necessary for an increasingly complex cancer care, to come together and discuss treatment options for patients. They are an expensive resource, however, and with an increase in the health and economic pressures, its value has been progressively placed under scientific scrutiny.
The past decade has thus seen research on cancer MDTs rapidly evolving. The lack of empirical evidence led to the NCAT’s characteristics of effective teams. This was followed by an array of studies examining various aspects of team functioning; they encompass observational approaches and tool developments, but also surveys and interviews assessing the team members’ and patients’ perspectives on MDTs. The importance of weekly MDMs for cancer MDTs was further reiterated recently in the report by the CRUK.
While evidence has consistently shown variations in team working and clinical decision-making across different cancers, we have learned that certain factors pertaining to personal and team skills, the environment and patient-centeredness can impact team functioning and decision-making (Tables 3 and 4). Hence the importance of a team-centered approach to improving cancer MDMs; led by a clinically feasible, observational methodology, and adequate training opportunities in non-technical skills.
Table 4.
Practices to implement (Dos) and those to avoid (Don’ts) when setting up MDT-driven cancer care
| Dos | Don’ts |
|---|---|
| Good relationships between team members | Unequal participation in discussion on treatment options |
| Communicating effectively with colleagues | Basing decisions primarily on biomedical information |
| Managing conflict within teams effectively | Seldom considering patient choice |
| Incorporating patient choice into decision-making | – |
| Incorporate patient views on the treatment options into decision-making | – |
| Incorporate patient psychosocial factors into decision-making | – |
| Incorporate patient comorbidities into decision-making | – |
| Ensuring equality and inclusiveness of team participation, in particular nurses | – |
| Rotating chairing duties within and between disciplines and, where possible, have a clinically non-contributing individual chair the meeting | – |
Abbreviation: MDT, multidisciplinary team.
What is more, we have also grown to think of MDMs as an input-process-output model. This provides a necessary framework that allows the design and execution of studies necessary for producing and accumulating the knowledge base, thereby steadily building our understanding of what practices MDTs should reinforce and avoid. Table 4 below presents a summary of these practices as mentioned within our review.
Strengths and limitations of the review
Regarding limitations, this review is a summary of current understanding – academic and clinical – of cancer MDT working; due to the heterogeneity of the studies, metrics, and outcomes we reviewed, a fully systematic review methodology was not feasible. Furthermore, in being inclusive of different designs and methods and adopting a descriptive approach, we did not assess the methodology and analyses undertaken within the studies that form the evidence for this review. Strengths of the review include that it offers a summary of a very disparate evidence base and it covers validated metrics for the evaluation of MDT work processes.
Conclusion
This review presents an up-to-date summary of the recent literature on the impact of cancer teams on the management of patients with cancer. We hope that this review will serve as a comprehensive reference document for health care professionals, patients, and their advocates, as well as those involved in the organization of cancer services, to enable them to critically evaluate and improve multidisciplinary team working in their own domain. MDTs are essential to cancer care, and cancer MDMs are a particularly important part since they allow the team with a diverse range of clinical specialties to come together and formulate treatment recommendations for patients with suspected or confirmed cancer. A range of factors pertaining to teamwork, availability of patient information, leadership, meeting management, and workload can affect the impact of an MDM on patient care. Studies to date have demonstrated that measuring and improving MDM working is possible and that improvements in patient care can be achieved as a result.
Acknowledgments
This work was supported by the UK’s National Institute for Health Research (NIHR) via the Imperial Patient Safety Translational Research Center (RD PSC 79560). Nick Sevdalis’ research was supported by the NIHR Collaboration for Leadership in Applied Health Research and Care South London at King’s College Hospital NHS Foundation Trust. Nick Sevdalis is a member of King’s Improvement Science, which is part of the NIHR CLAHRC South London and comprises a specialist team of improvement scientists and senior researchers based at King’s College London. Its work is funded by King’s Health Partners (Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust, King’s College London, and South London and Maudsley NHS Foundation Trust), Guy’s and St Thomas’ Charity, the Maudsley Charity, and the Health Foundation (ISCLA01131002). The views expressed are those of the authors and not necessarily those of the National Health Services, the NIHR, or the Department of Health.
Footnotes
Disclosure
Nick Sevdalis is the Director of London Safety and Training Solutions Ltd, which provides patient safety and quality improvement skills training and advice on a consultancy basis to hospitals and training programs. James Green is a Director of Green Cross Medical Ltd that developed MDT FIT for use by National Health Service Cancer Teams in the UK. The authors report no other conflicts of interest in this work.
References
- 1.Basta YL, Bolle S, Fockens P, Kristien MAJT. The value of multidisciplinary team meetings for patients with gastrointestinal malignancies: a systematic review. Ann Surg Oncol. 2017;24(9):2669–2678. doi: 10.1245/s10434-017-5833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holliday EB, Ahmed AA, Yoo SK, Jagsi R, Hoffman KE. Does cancer literature reflect multidisciplinary practice? A systematic review of oncology studies in the medical literature over a 20-year period. Int J Radiat Oncol Biol Phys. 2015;92(4):721–731. doi: 10.1016/j.ijrobp.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Stairmand J, Signal L, Sarfati D, et al. Consideration of comorbidity in treatment decision making in multidisciplinary meetings: a systematic review. Ann Oncol. 2015;26(7):1325–1332. doi: 10.1093/annonc/mdv025. [DOI] [PubMed] [Google Scholar]
- 4.Denton E, Conron M. Improving outcomes in lung cancer: the value of the multidisciplinary health care team. J Multidiscip Healthc. 2016;9:137–144. doi: 10.2147/JMDH.S76762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noyes K, Monson JRT, Rizvi I, Savastano A, Green JSA, Sevdalis N. Regional multiteam systems in cancer care delivery. J Oncol Pract. 2016;12(11):1059–1066. doi: 10.1200/JOP.2016.013896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health . Manual for Cancer Services. London: the Department of Health; 2004. [Google Scholar]
- 7.Department of Health . National Peer Review Report: Cancer Services 2012/2013. London, UK: the Department of Health; 2013. [Google Scholar]
- 8.Lamb BW, Brown KF, Nagpal K, Vincent C, Green JSA, Sevdalis N. Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol. 2011;18:2116–2125. doi: 10.1245/s10434-011-1675-6. [DOI] [PubMed] [Google Scholar]
- 9.Forrest LM, McMillan DC, McArdle CS, Dunlop DJ. An evaluation of the impact of a multidisciplinary team, in a single centre, on treatment and survival in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2005;93(9):977–978. doi: 10.1038/sj.bjc.6602825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newman E, Guest A, Helvie M, et al. Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer. 2006;107(10):2343–2351. doi: 10.1002/cncr.22266. [DOI] [PubMed] [Google Scholar]
- 11.Davies AR, Deans DA, Penman I, et al. The multidisciplinary team meeting improves staging accuracy and treatment selection for gastro-esophageal cancer. Dis Esophagus. 2006;19(6):496–503. doi: 10.1111/j.1442-2050.2006.00629.x. [DOI] [PubMed] [Google Scholar]
- 12.Acher PL, Young AJ, Etherington-Foy R, McCahy PJ, Deane AM. Improving outcomes in urological cancers: the impact of “multidisciplinary team meetings”. Int J Surg. 2005;3(2):121–123. doi: 10.1016/j.ijsu.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Kee F, Owen T, Leathem R. Decision making in a multidisciplinary cancer team: does team discussion result in better quality decisions? Med Decis Making. 2004;24(6):602–613. doi: 10.1177/0272989X04271047. [DOI] [PubMed] [Google Scholar]
- 14.Kee F, Owen T, Leathem R. Offering a prognosis in lung cancer: when is a team of experts an expert team? J Epidemiol Community Health. 2007;61(4):308–313. doi: 10.1136/jech.2005.044917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamb BW, Sevdalis N, Taylor C, Vincent C, Green JSA. Multidisciplinary team working across different tumour types: analysis of a national survey. Ann Oncol. 2012;23:1293–1300. doi: 10.1093/annonc/mdr453. [DOI] [PubMed] [Google Scholar]
- 16.Jalil R, Akhter W, Sevdalis N, Green JSA. Chairing and leadership in cancer MDTs: development and evaluation of an assessment tool. Eur Urol Supp. 2013;12(6):132–133. [Google Scholar]
- 17.Raine R, Xanthopoulou P, Wallace I, et al. Determinants of treatment plan implementation in multidisciplinary team meetings for patients with chronic diseases: a mixed-methods study. BMJ Qual Saf. 2014;23:867–876. doi: 10.1136/bmjqs-2014-002818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soukup T, Petrides KV, Lamb BW, et al. The anatomy of clinical decision-making in multidisciplinary cancer meetings: a cross-sectional observational study of teams in a natural context. Medicine. 2016;95(24):e3885. doi: 10.1097/MD.0000000000003885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leo F, Venissac N, Poudenx M, Otto J, Mouroux J, Groupe d’Oncologie Thoracique Azureen Multidisciplinary management of lung cancer: how to test its efficacy? J Thorac Oncol. 2007;2:69–72. doi: 10.1097/JTO.0b013e31802bff56. [DOI] [PubMed] [Google Scholar]
- 20.Coory M, Gkolia P, Yang IA, Bowman RV, Fong KM. Systematic review of multidisciplinary teams in management of lung cancer. Lung Cancer. 2008;60:14–21. doi: 10.1016/j.lungcan.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Tattersall MHN. Multidisciplinary team meetings: where is the value? Lancet Oncol. 2006;7(11):886–888. doi: 10.1016/S1470-2045(06)70916-0. [DOI] [PubMed] [Google Scholar]
- 22.Lamb BW, Green JSA, Benn J, Brown KF, Vincent CA, Sevdalis N. Improving decision-making in multidisciplinary tumor boards: prospective longitudinal evaluation of multicomponent intervention for 1,421 patients. J Am Coll Surg. 2013;2173:412–420. doi: 10.1016/j.jamcollsurg.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 23.National Cancer Action Team . The Characteristics of an Effective Multidisciplinary team (MDT) London: National Cancer Action Team; 2010. [Google Scholar]
- 24.Taylor C, Brown K, Lamb B, Harris J, Sevdalis N, Green JS. Developing and testing TEAM (Team Evaluation and Assessment Measure), a self-assessment tool to improve cancer multidisciplinary teamwork. Ann Surg Oncol. 2012;19(13):4019–4027. doi: 10.1245/s10434-012-2493-1. [DOI] [PubMed] [Google Scholar]
- 25.Cancer Research UK . Improving the Effectiveness of Multidisciplinary Team Meetings in Cancer Services. London, UK: Cancer Research UK; 2017. [Google Scholar]
- 26.Lamb BW, Green JSA, Vincent C, Sevdalis N. Decision making in surgical oncology. Surg Oncol. 2011;20(3):163–168. doi: 10.1016/j.suronc.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Lamb BW, Taylor C, Lamb JN, et al. Facilitators and barriers to team-working and patient centeredness in multidisciplinary cancer teams: findings from a national study. Ann Surg Oncol. 2013;20:1408–1416. doi: 10.1245/s10434-012-2676-9. [DOI] [PubMed] [Google Scholar]
- 28.Lamb BW, Payne H, Vincent C, Sevdalis N, Green JSA. The role of oncologists in multidisciplinary cancer teams in the UK: an untapped resource for team leadership? J Eval Clin Pract. 2011;17:1200–1206. doi: 10.1111/j.1365-2753.2010.01507.x. [DOI] [PubMed] [Google Scholar]
- 29.Lamb BW, Allchorne P, Sevdalis N, Vincent C, Green JSA. The role of the cancer nurse specialist in the urology multidisciplinary team meeting. Int J Urol Nurs. 2011;5:59–64. [Google Scholar]
- 30.Blazeby JM, Wilson L, Metcalfe C, Nicklin J, English R, Donovan JL. Analysis of clinical decision-making in multi-disciplinary cancer teams. Ann Oncol. 2006;17(3):457–460. doi: 10.1093/annonc/mdj102. [DOI] [PubMed] [Google Scholar]
- 31.Wood JJ, Metcalfe C, Paes A, et al. An evaluation of treatment decisions at a colorectal cancer multidisciplinary team. Colorectal Dis. 2008;10(8):769–772. doi: 10.1111/j.1463-1318.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 32.Soukup T, Lamb BW, Sarkar S, et al. Predictors of treatment decisions in multidisciplinary oncology meetings: a quantitative observational study. Ann Surg Oncol. 2016;23:4410–4417. doi: 10.1245/s10434-016-5347-4. [DOI] [PubMed] [Google Scholar]
- 33.Jalil R, Lamb BW, Russ S, Sevdalis N, Green JSA. The cancer multidisciplinary team from the coordinators perspective: results from a national survey in the UK. BMC Health Serv Res. 2012;12:457. doi: 10.1186/1472-6963-12-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lamb BW, Sevdalis N, Arora S, Pinto A, Vincent C, Green JSA. Teamwork and team decision-making at multidisciplinary cancer conferences: barriers, facilitators, and opportunities for improvement. World J Surg. 2011;35:1970–1976. doi: 10.1007/s00268-011-1152-1. [DOI] [PubMed] [Google Scholar]
- 35.McGlynn B, Johnston M, Green J. A nurse-led multidisciplinary team approach in urology-oncology: addressing the new cancer strategy. J Clin Urol. 2017. https://doi.org/10.1177/2051415817700034.
- 36.Lamb BW, Sevdalis N, Mostafid H, Vincent C, Green JS. Quality improvement in multidisciplinary cancer teams: an investigation of teamwork and clinical decision-making and cross-validation of assessments. Ann Surg Oncol. 2011;18(13):3535–3543. doi: 10.1245/s10434-011-1773-5. [DOI] [PubMed] [Google Scholar]
- 37.Russ S, Hull L, Rout S, Vincent C, Darzi A, Sevdalis N. Observational teamwork assessment for surgery: feasibility of clinical and nonclinical assessor calibration with short-term training. Ann Surg. 2012;255(4):804–809. doi: 10.1097/SLA.0b013e31824a9a02. [DOI] [PubMed] [Google Scholar]
- 38.Heasman B, Reader TW. What can acute medicine learn from qualitative methods? Curr Opin Crit Care. 2015;21(5):460–466. doi: 10.1097/MCC.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 39.Flowerdew L, Gaunt A, Spedding J, et al. A multicentre observational study to evaluate a new tool to assess emergency physicians’ nontechnical skills. Emerg Med J. 2012;30(6):437–443. doi: 10.1136/emermed-2012-201237. [DOI] [PubMed] [Google Scholar]
- 40.Stefanidis D, Sevdalis N, Paige J, et al. Association for Surgical Education Simulation Committee. Ann Surg. 2015;261(5):846–853. doi: 10.1097/SLA.0000000000000826. [DOI] [PubMed] [Google Scholar]
- 41.Arora S, Sevdalis N, Tam C, Kelley C, Babu ED. Systematic evaluation of decision-making in multidisciplinary breast cancer teams: a prospective, cross-sectional study. Eur J Surg Oncol. 2012;38(5):459. [Google Scholar]
- 42.Gandamihardja T, McInerney S, Soukup T, Sevdalis N. Improving team working within a breast MDT: an observational approach. Eur J Surg Oncol. 2014;40(5):604. [Google Scholar]
- 43.Lamb BW, Wong HWL, Vincent C. Teamwork and team performance in multidisciplinary cancer teams: development of an observational assessment tool. BMJ Qual Saf. 2013;20:849–856. doi: 10.1136/bmjqs.2010.048660. [DOI] [PubMed] [Google Scholar]
- 44.Jalil R, Akhter W, Lamb BW, et al. Validation of team performance assessment of multidisciplinary tumor boards. J Urol. 2014;192(3):91–898. doi: 10.1016/j.juro.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 45.Sarkar S, Arora S, Soukup T, et al. A multi-centre study evaluating performance of multidisciplinary teams: urology vs the top cancer killers. Eur Urol Suppl. 2014;13:e878–e878a. [Google Scholar]
- 46.Shah S, Arora S, Atkin G, et al. Decision-making in colorectal cancer tumor boards meetings: results of a prospective observational assessment. Surg Endosc. 2014;28(10):2783–2788. doi: 10.1007/s00464-014-3545-3. [DOI] [PubMed] [Google Scholar]
- 47.Seretis C, Mankotia R, Goonetilleke K, Rawstorne E. Quality assessment of decision-making in colorectal cancer multidisciplinary meetings. J BUON. 2014;19(4):913–916. [PubMed] [Google Scholar]
- 48.Harris J, Taylor C, Sevdalis N, Jalil R, Green JSA. Development and testing of the cancer multidisciplinary team meeting observational tool (MDT-MODe) Int J Qual Health. 2016;28(3):332–338. doi: 10.1093/intqhc/mzw030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor C, Atkins L, Richardson A, Tarrant R, Ramirez A-J. Measuring the quality of MDT working: an observational approach. BMC Cancer. 2012;12:202. doi: 10.1186/1471-2407-12-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anderson NR, West MA. Measuring climate for work group innovation: development and validation of the team climate inventory. J Organ Behav. 1998;19:235–258. [Google Scholar]
- 51.Bales R. Interaction Process Analysis. Cambridge, USA: Addison Wesley; 1950. [Google Scholar]
- 52.Bell L. Patterns of interactions in multidisciplinary child protection teams in New Jersey. Child Abuse Negl. 2011;25(1):65–80. doi: 10.1016/s0145-2134(00)00224-6. [DOI] [PubMed] [Google Scholar]
- 53.Gibbon B. An investigation of interprofessional collaboration in stroke rehabilitation team conferences. J Clin Nurs. 1994;8:246–252. doi: 10.1046/j.1365-2702.1999.00240.x. [DOI] [PubMed] [Google Scholar]
- 54.Atwal A, Caldwell K. Do all health and social care professionals interact equally: a study of interactions in multidisciplinary teams in the United Kingdom. Scand J Caring Sci. 2005;19:268–273. doi: 10.1111/j.1471-6712.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- 55.Jefferson G. Glossary of transcript symbols with an introduction. In: Lerner GH, editor. Conversation Analysis: Studies from the First Generation. Amsterdam: John Benjamins Publishing Company; 2004. pp. 13–31. [Google Scholar]
- 56.Dew K, Subbe M, Signal L, et al. Cancer care decision making in multidisciplinary meetings. Qual Health Res. 2015;25(3):397–407. doi: 10.1177/1049732314553010. [DOI] [PubMed] [Google Scholar]
- 57.Dew K. Purifying and hybridising categories in healthcare decision-making: the clinic, the home, and the multidisciplinary team meeting. Health Sociol Rev. 2016;25(2):142–156. [Google Scholar]
- 58.Bezemer J, Murtagh G, Cope A, Kress G, Kneebone R. “Scissors, please”: the practical accomplishment of surgical work in the operating theatre. Symb Interact. 2011;34(3):398–414. [Google Scholar]
- 59.Korkiakangas T, Sharon-Marie W, Bezemer J, Kneebone R. Nurse-surgeon object transfer: video analysis of communication and situation awareness in the operating theatre. Int J Nurs Stud. 2014;51(9):1195–1206. doi: 10.1016/j.ijnurstu.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 60. MDTFIT.co.uk [homepage on the Internet] NCAT in collaboration with Green Cross Medical Ltd and the University of Surrey Clinical Informatics Research Group. [Accessed April 7, 2017]. ©2011–2017 [updated May 2, 2014; cited April 7, 2017] Available from: http//mdtfit.co.uk/ for further examples, please see also www.youtube.com/watch?v=8bWI2ieSjWE and www.youtube.com/watch?v=FOdkfFb2BQU.
- 61.Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304(15):1693–1700. doi: 10.1001/jama.2010.1506. [DOI] [PubMed] [Google Scholar]
- 62.Lamb BW, Jalil RT, Sevdalis N, Vincent C, Green JSA. Strategies to improve the efficiency and utility of multidisciplinary team meetings in urology cancer care: a survey study. BMC Health Serv Res. 2014;14:377. doi: 10.1186/1472-6963-14-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.England NHS. Achieving World-Class Cancer Outcomes: Taking the Strategy Forward. UK: NHS England; 2016. [Google Scholar]
- 64.England NHS. Achieving World-Class Outcomes: A Strategy for England 2015–2020. UK: NHS England; 2015. [Google Scholar]
- 65.Lamb BW, Sevdalis N, Vincent C, Green JSA. Development and evaluation of a checklist to support decision making in cancer multidisciplinary team meetings: MDT-QuIC. Ann Surg Oncol. 2012;19:1759–1765. doi: 10.1245/s10434-011-2187-0. [DOI] [PubMed] [Google Scholar]
- 66.MDT-FIT Homepage on the Internet. [Accessed October 16, 2017]. Available at www.mdtfit.co.uk.