Introduction
Video-assisted thoracic surgery (VATS) via a single incision for major procedures is taking the specialty by a storm over the past 5 years since its description by Gonzalez et al. (1). The development of this approach originated as a progression of the anterior multiport VATS approach, as expansion of the uniportal VATS experience for intermediate procedures (2), but also as a direct evolution from anterior limited thoracotomies. While posterior VATS approaches never really became widely performed even after more than 20 years of being described, the anterior approach alternative has finally been adopted in recent years as a valid widely offered alternative to thoracotomy (3). However, its expansion has taken the best part of 15 years. One has to wonder what are the reasons to explain the rapid adoption of the uniportal VATS approach in contrast to the slow spread of multiport VATS lobectomies.
Beyond the development of purposely-designed surgical instruments, improvements in the optical systems, easy access to surgical videos and expert courses, and refinement on the surgical staplers it is important to evaluate the factors contributing to this rapid expansion and the potential reasons behind surgeons adopting uniportal VATS. We believe that there are oncological factors (as the majority of this procedures deal with malignant processes), factors related to the patients, and finally, relating to the operating surgeons. Some of these factors could be also associated to multiportal VATS if compared to open surgery.
Oncological factors
Anatomical resections
Nearly a decade after the initial reports from Rocco and colleagues in the use of uniportal VATS for intermediate therapeutic procedures in the form of non-anatomical wedge resection of nodules (4), the first lobectomy (lower lobe) performed via this approach was described by Gonzalez et al. (1). Soon all other lobectomies followed (5), with successive reports of anatomical segmentectomies (6), pneumonectomies (7) and complex bronchial (8) and vascular reconstructions (9) as well as en bloc chest wall resections (10) followed. Multiple authors have continued to report, even with large numbers, series of uniportal VATS anatomical resections confirming the reproducibility of the technique (11-14). There is very little doubt now that every anatomical pulmonary procedure can be performed using this approach, even by surgeons without previous multiportal VATS lobectomy experience (15,16).
Some of the newly published reports are confirming a similar rate of completely excised procedures with clear margins between uniportal VATS and other approaches.
Lymphatic strategies
The importance of extensive mediastinal strategies has been highlighted by international societies. The benefits in correct staging are clear, and although the potential survival impact are less so, exploration of mediastinal lymph node stations has been used as a marker of quality of surgery (17). The disregard shown by enthusiasts of modern forms of radiotherapy about the benefits of adequate lymph node examinations should not defer surgeons of trying to achieve excellence in this field.
It did take some time for VATS surgeons to demonstrate at least equal achievements to open surgery in mediastinal exploration. Learning curve, human factors and need to change the position of the optics in multiportal approaches to access different stations might be the reason. Nowadays however there is little doubt that satisfactory lymph node excision can be performed via VATS or open surgery. In most reports comparing uniportal and multiportal VATS surgeons have demonstrated at least as extensive mediastinal exploration with any approach (18-20). It will be discussed in a later point of this manuscript, but the position of the optics in uniportal VATS at the dome of the thoracic cavity in the lateral decubitus position allows direct access to all lymph node stations therefore enabling adequate lymph node strategies with this approach.
Surgical staging
Uniportal VATS provides a great opportunity to improve surgical staging with an incision no greater than the required to place an intercostal drain. Its potential uses prior to commit to a lung resection could include assessment of the pleural fluid for malignant cells, a factor that has been explore in the past by several authors although has repeatedly failed to enter prognostic indicator systems. As described before, the placement of the incision and optics allows full exploration of the thoracic cavity to access any lymph node station that requires examination in addition to any preoperative staging performed. This could be important in Units without access to endoscopic ultrasound techniques.
Preliminary VATS can also be helpful in the assessment of the potential resectability in locally invasive tumors. Single-port VATS has been used by surgeons to achieve this both at mediastinal or even intrapericardial involvement.
Long-term outcomes
Survival and the impact of the potentially limited immune response to trauma are areas that still lack extensive studies, mainly due to the limited on time experience with this approach. VATS lobectomy has been shown to reduce humoral immune response to trauma when compared to thoracotomy (21), and there is no reason to believe that this potential benefit would not continue if single port VATS lobectomy were to be studied similarly. It is important to point out that the real clinical impact of this response has not been established. There is no doubt that in following years we will see published reports of long-term survival after uniportal VATS lobectomy. More doubts arise of whether potential reports would assess prospectively survival in well-designed comparative studies any differences compared to other approaches.
Factors relating to patients
Number and size of incisions
The first thing that patients will see after surgery and indeed would leave a lasting effect in some is the size and number of scars. In the uniportal approach the incision is located in a covered area, between the anterior axillary line and the submammary crease. It might seem to us as surgeons as a minor issue, but patients do carry the scars for life. The size of the incision is limited by the need to remove the specimen and the tumor, and it is therefore adapted to it. While it is routine to be able to perform single port VATS procedures using a 2-cm incision (i.e., for pneumothorax surgery, lung biopsy or excision of small nodules), the incisions for lung resections are sized between 4 and 6 cm depending of the lobe to be removed and the size of the tumor. Some VATS surgeons have advocated piecing the specimens before removal in order to use smaller incisions, but this option does not seem reasonable when the pathological analysis is to be performed in a meaningful manner.
Postoperative pain
Both short and long term pain following surgery have been proven to be improved when VATS is performed instead of open surgery. The vast majority of these reports involve multiport VATS (22,23). It is not adventurous to assume that with uniportal surgery that avoids entry of posterior narrower intercostal spaces and does not use trocars would at the very least equal the improvements of traditional VATS.
Moreover, some reports are arising with the benefits of single port VATS in comparison to multiport VATS (24). It is likely that future information will focus in this issue as it is a topic of interest.
Recovery after surgery
As with the issue of postoperative pain, the advantages of VATS over open surgery have been extensively reported (25-27). Once again, it is likely that future work will focus in the advantages of uniportal surgery in term of postoperative hospital stay and returning to normal activities. In this field, it is likely that the advantages of uniportal surgery will be at the very least similar compared to multiport VATS procedures.
Perception of patients of the surgical processes
A factor that is not commonly mentioned (perhaps because of the difficulties to assess subjective data) is the patients’ perception of the process of surgery. Patients are attracted to options that carry less trauma and at present uniportal VATS represent the least invasive technique for major lung resection. Other factors such as the attraction to the “new” cannot be underestimated. This can lead to a better engagement of patients and careers to the recovery process, which is an important part of enhanced recovery after surgery schemes. The most recent development of non-intubated anesthetic techniques applied to uniportal VATS could enhanced the concept of less invasiveness (28,29).
Factors related to the operating surgeon
The single port VATS lobectomy was described as the progress from an anterior two-port VATS popularized by Daniels et al. (30). The initial 3−4 port VATS was initially described by surgeons using both anterior or posterior approaches (31,32). In the uniportal VATS the surgeon and assistant tend to be positioned together in front of the patient that lies in a lateral position with a very important hyperextension of the chest wall.
View of the thoracic cavity
The main screen is placed directly in front of the operating surgeon supporting the impression of the “direct” approach of uniportal VATS. A second screen can be placed behind the surgeons for the benefit of the scrub nurse who stands behind the patient. With a 30 degree optic placed at the posterior end of the incision the entire thoracic cavity can be visualized and explored. As the incision is placed at the anterior axillary line, the position of the camera (the surgeon’s eye) lies very close to the dome of the thoracic cavity when the patient is placed in the lateral position, and at mid-point between the apex and the base of the cavity allowing closer access to all areas than if the optics are placed at the base of the pleural cavity.
The position of the camera permits variation on the surgical strategy simply by moderate movements of the operating table and gentle lung retraction. For example, to access the hilar structures directly a gentle rotation of the table away from the surgeon is sufficient, and for dissection of posterior mediastinal pleura or some nodal stations a forward rotation and lung traction permits excellent direct exposure. The facility to access the entire thoracic cavity permits the surgeon to perform the lobectomies in different steps, enabling individual strategy for every patient according to which part of the dissection appears easier in order to make progress (Figures 1,2,3).
Figure 1.
Initial division of right upper lobe bronchus before artery and vein (33). The direct view of uniportal surgery allows for the surgeon to choose the strategy for any individual case. In this case during an upper lobectomy the recurrent branch of the pulmonary artery is first dissected and divided followed by the division of the upper bronchus. The division of the anterior hilar structures (upper truncus of pulmonary artery and upper pulmonary vein) were performed after. Available online: http://www.asvide.com/articles/1008
Figure 2.
In contrast, in this case the hilar structures were divided first, followed by the division of the upper segmental bronchus from “anterior to posterior” (34). Available online: http://www.asvide.com/articles/1009
Figure 3.
Fissure first dissection during right lower lobectomy (35). The exposure that uniportal VATS produce has helped the options of dissection of the fissures first in the same way it would be performed in open surgery. In this case of a right lower lobectomy the pulmonary artery was first dissected in the fissure and divided after completion. The lower bronchus was divided after and finally the inferior pulmonary vein. Available online: http://www.asvide.com/articles/1010
As the incision is placed halfway between apex and base (4th or 5th intercostal space), the exposure is excellent for both these areas in every patient, simply by direct camera movements. This facility is especially helpful when performing the lymphadenopathy or when extensive procedures are performed (Figure 4).
Figure 4.
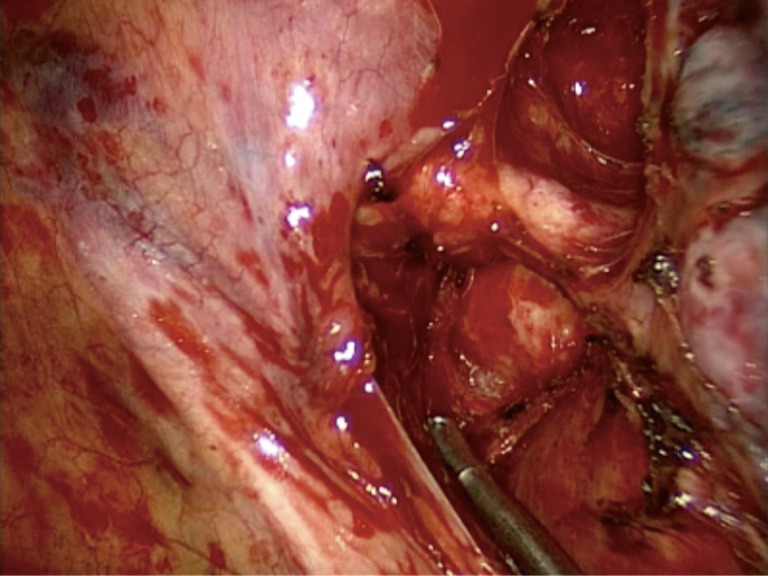
Close view of resected station 5 during a left upper lobectomy.
Angle of vision, no rotational effect
As the instruments are used parallel to the optics, directly into the hilar structures, the view perceived by surgeons is the same as in an anterior thoracotomy, favored by many surgeons. The surgeon’s movements with this approach are therefore replicating those of an anterior thoracotomy. The direct line between surgeon, surgical target and screen permits the “global” continuity between those three points.
This global continuity was further explored by Bertolaccini et al. (36). Due to the placement of the instruments and optics in a sagittal plane and the direct approach surgeon-target-screen, the surgeon does maintain an excellent impression of depth which is the main difficulty to get used to in the multiport VATS approach. This is one of the main reasons why surgeons used to open anterior thoracotomy can rapidly transition into the uniportal VATS.
In multiport VATS using a triangular placement of instruments and camera a rotation angle is created, as a new optical plane is created. This torsion angle requires time to get used to and it is more notorious when trying to acquire the sense of depth during VATS (37). Perhaps the development of 3-D systems can help with the training as they do represent the depth better than in traditional 2-D screens.
Ergonomics
One of the issues of triangular multiport VATS is the deficient ergonomic position of the operating surgeon. The arms abducted, sometimes elevated and not moving in a sagittal plane contribute to poor ergonomics, moreover in long procedures. Another problem is continuous elbow and wrist flexion associated with these approaches.
In uniportal VATS the surgeon stands directly to the target and screen, so the back is not under torsion or bending, there is no tension on the cervical spine and the arms are not abducted or elevated. In practical terms the arm movements are very similar to those in a good ergonomic position during open surgery.
The Ergon Trial was performed to compare single vs. multiport VATS in wedge resections and concluded that the physical demands on multiport VATS were higher based on overall workload, a more stressful body position and less direct viewing than in single port VATS. In contrast, the surgeon can maintain a more neutral body posture during uniportal VATS by standing straight and facing the monitor with only minimal neck extension/rotation (38).
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. 10.1510/icvts.2010.256222 [DOI] [PubMed] [Google Scholar]
- 2.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. 10.1016/S0003-4975(03)01219-0 [DOI] [PubMed] [Google Scholar]
- 3.Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. 10.1016/j.ejcts.2009.09.012 [DOI] [PubMed] [Google Scholar]
- 4.Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. 10.1016/j.jtcvs.2004.08.027 [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. 10.1016/j.athoracsur.2012.10.070 [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. 10.1093/ejcts/ezs482 [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. 10.1016/j.jtcvs.2013.02.052 [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang CL, Cheng CY, Lin CH, et al. Single-port thoracoscopic rib resection: a case report. J Cardiothorac Surg 2014;9:49. 10.1186/1749-8090-9-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery lobectomy in semiprone position: primary experience of 105 cases. J Thorac Dis 2015;7:2389-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. 10.1016/j.athoracsur.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 13.Feng M, Shen Y, Wang H, et al. Uniportal video assisted thoracoscopic lobectomy: primary experience from an Eastern center. J Thorac Dis 2014;6:1751-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anile M, Diso D, Mantovani S, et al. Uniportal video assisted thoracoscopic lobectomy: going directly from open surgery to a single port approach. J Thorac Dis 2014;6:S641-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aragón J, Pérez Méndez I. From open surgery to uniportal VATS: asturias experience. J Thorac Dis 2014;6:S644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hagan ME, Williams ST, Socci L, et al. Completing the audit cycle improves surgical standards in lung cancer. Why do some patients still not receive the best care? J Thorac Oncol 2013;8:779-82. 10.1097/JTO.0b013e31828c61a5 [DOI] [PubMed] [Google Scholar]
- 18.Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-72. [DOI] [PubMed] [Google Scholar]
- 19.Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. 10.4103/0366-6999.167298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ng CS, Lee TW, Wan S, et al. Thoracotomy is associated with significantly more profound suppression in lymphocytes and natural killer cells than video-assisted thoracic surgery following major lung resections for cancer. J Invest Surg 2005;18:81-8. 10.1080/08941930590926320 [DOI] [PubMed] [Google Scholar]
- 22.Tsubokawa N, Harada H, Takenaka C, et al. Comparison of Postoperative Pain after Different Thoracic Surgery Approaches as Measured by Electrical Stimulation. Thorac Cardiovasc Surg 2015;63:519-25. 10.1055/s-0035-1546427 [DOI] [PubMed] [Google Scholar]
- 23.Nagahiro I, Andou A, Aoe M, et al. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg 2001;72:362-5. 10.1016/S0003-4975(01)02804-1 [DOI] [PubMed] [Google Scholar]
- 24.Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. 10.1186/1749-8090-8-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li WW, Lee RL, Lee TW, et al. The impact of thoracic surgical access on early shoulder function: video-assisted thoracic surgery versus posterolateral thoracotomy. Eur J Cardiothorac Surg 2003;23:390-6. 10.1016/s1010-7940(02)00795-9 [DOI] [PubMed] [Google Scholar]
- 26.Kaseda S, Aoki T, Hangai N, et al. Better pulmonary function and prognosis with video-assisted thoracic surgery than with thoracotomy. Ann Thorac Surg 2000;70:1644-6. 10.1016/S0003-4975(00)01909-3 [DOI] [PubMed] [Google Scholar]
- 27.Li WW, Lee TW, Lam SS, et al. Quality of life following lung cancer resection: video-assisted thoracic surgery vs thoracotomy. Chest 2002;122:584-9. 10.1378/chest.122.2.584 [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. 10.1093/icvts/ivu209 [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. 10.1093/ejcts/ezv136 [DOI] [PubMed] [Google Scholar]
- 30.Daniels LJ, Balderson SS, Onaitis MW, et al. Thoracoscopic lobectomy: a safe and effective strategy for patients with stage I lung cancer. Ann Thorac Surg 2002;74:860-4. 10.1016/S0003-4975(02)03764-5 [DOI] [PubMed] [Google Scholar]
- 31.Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. 10.1016/s1010-7940(02)00814-x [DOI] [PubMed] [Google Scholar]
- 32.McKenna RJ., Jr Lobectomy by video-assisted thoracic surgery with mediastinal node sampling for lung cancer. J Thorac Cardiovasc Surg 1994;107:879-81; discussion 881-2. [PubMed] [Google Scholar]
- 33.Martin-Ucar AE, Socci L. Initial division of right upper lobe bronchus before artery and vein. Asvide 2016;3:248. Available online: http://www.asvide.com/articles/1008
- 34.Martin-Ucar AE, Socci L. In contrast, in this case the hilar structures were divided first, followed by the division of the upper segmental bronchus from “anterior to posterior”. Asvide 2016;3:249. Available online: http://www.asvide.com/articles/1009
- 35.Martin-Ucar AE, Socci L. Fissure first dissection during right lower lobectomy. Asvide 2016;3:250. Available online: http://www.asvide.com/articles/1010
- 36.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bertolaccini L, Viti A, Terzi A, et al. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. 10.21037/acs.2015.12.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. 10.1007/s00464-014-4024-6 [DOI] [PubMed] [Google Scholar]


