Abstract
Multimorbidity has been linked to a variety of negative outcomes although as yet, there has been little research on its association with loneliness. This study examined the association between physical multimorbidity (≥ 2 physical diseases) and loneliness in the general population and its potential mediators. Data came from the Adult Psychiatric Morbidity Survey 2007 (N = 7403, aged ≥16 years). Information was obtained on 20 doctor diagnosed physical conditions that were present in the previous year. An item from the Social Functioning Questionnaire (SFQ) was used to obtain information on loneliness. Multivariable logistic regression analysis was used to examine associations. An increasing number of physical diseases was associated with higher odds for loneliness. Compared to no physical diseases, the odds ratio (OR) (95% confidence interval: CI) for loneliness increased from 1.34 (1.13–1.59) to 2.82 (2.11–3.78) between one and ≥5 physical diseases. This association was particularly strong in the youngest age group (i.e. 16–44 years). The loneliness-physical multimorbidity association was significantly mediated by stressful life events (% mediated 11.1%-30.5%), anxiety (30.2%), and depression (15.4%). Physical multimorbidity is associated with increased odds for loneliness. Prospective research is now needed to further elucidate this association and the factors that underlie it.
Introduction
Multimorbidity (the presence of 2 or more chronic/acute diseases) is common in the general population [1]. A recent study that used World Health Survey data from 27 low- and middle-income countries (LMICs) and 1 high-income country (HIC) showed that the prevalence of multimorbidity ranged from 1.7% (Myanmar) to 15.2% (Nepal) and averaged 7.8% across all LMICs countries [2]. Although research has indicated that the prevalence of multimorbidity increases with age, it is observed in all adult age groups [2,3]. This is alarming as the co-occurrence of chronic disease has been associated with a variety of negative outcomes including worse quality of life [4], poorer physical function [5], greater health care use [6], as well as an increased risk for premature mortality [7].
The current study will examine physical multimorbidity—the co-occurrence of 2 or more physical diseases. Although there has been increased attention on this phenomenon recently [8–11], there are still many gaps in our knowledge. For example, relatively little is known about the association between physical multimorbidity and loneliness, that is, “the unpleasant experience that occurs when a person’s network of social relations is deficient in some important way, either quantitatively or qualitatively” [12]. This may be an important omission. Loneliness is not only common in the general population with studies showing that on average, approximately 5–15% of people report often feeling lonely [13–16], but there is some evidence that loneliness might be a significant factor for health in its own right. Specifically, feeling lonely has been linked to an increased risk for a variety of adverse health outcomes including premature mortality [17–19].
Importantly, previous research has indicated that there might be an association between physical disease and loneliness. In particular, an earlier study found that there was an increased risk for loneliness in individuals with chronic diseases [20]. Other studies have also shown an association between feeling lonely and heart disease, hypertension, stroke [21–23] and Alzheimer disease [24]. However, this research has also indicated that not all physical diseases are linked to loneliness and that the association between loneliness and specific diseases may vary between different population subgroups [21].
Despite these studies linking physical disease and loneliness, as yet, there has been comparatively little research on the association between physical multimorbidity and loneliness. Moreover, to the best of our knowledge, the few studies undertaken to date on the association between the number of illnesses/multimorbidity and loneliness or vice versa have been confined to middle-aged and older adults (age ≥ 45) and produced mixed results [25–29]. Specifically, while studies among adults aged 52–92 in Denmark, 65 and above in the United States and 75 and above in Israel respectively linked the number of chronic illnesses and greater comorbidity to loneliness [25,27,28], a study among veterans aged 60 and above in the United States found that a bivariate association between the number of medical conditions and loneliness became non-significant in a stepwise linear regression analysis [29]. In addition, research undertaken among men and women aged 45 and above in Canada and Australia found that multimorbidity was significantly linked to loneliness in all age-sex groups except among Australian women aged 75 and above [26].
Given the absence of research on the association between (physical) multimorbidity and loneliness among adults of all ages and the mixed findings from research that has focused on the multimorbidity-loneliness association in middle-aged and older adults, the current study had two aims: (1) to examine the association between physical multimorbidity and loneliness in a general population sample; and (2) to determine if any factors might be important for this association.
Materials and methods
Study population
This study used data from the Adult Psychiatric Morbidity Survey (APMS) 2007 (N = 7403). Details of the survey have been published elsewhere previously [30]. In brief, the survey was conducted in England between October 2006 and December 2007 by the National Center for Social Research and Leicester University. To obtain a nationally representative sample of the adult population aged ≥16 years old residing in private households, multistage stratified probability sampling was used. The small user Postcode Address File (PAF) served as the sampling frame with postcode sectors serving as the primary sampling units (PSUs). Sectors were stratified by both region and socioeconomic status. One person was randomly selected from each randomly selected household. The survey response rate was 57% (respondents from 7461/13171 eligible households agreed to participate). To correct for survey non-response, sampling weights were generated to ensure that the sample was representative of its intended target population. Details of the weighting procedure are provided in the survey report [30]. The Royal Free Hospital and Medical School Research Ethics Committee provided ethical approval for the study. The survey methodology was carried out in accordance with the relevant guidelines and regulations with all participants providing written informed consent.
Data availability
The data used in this study are third party data (i.e., they are not owned and were not collected by the authors) that have been made publicly available by the National Center for Social Research via the UK data archive. The authors did not have any special access privileges and other authors can access these data in the same manner as the authors in this study did i.e. registration is required and standard conditions of use apply. Details of how to access the Adult Psychiatric Morbidity Survey 2007 dataset are available at: https://discover.ukdataservice.ac.uk/catalogue/?sn=6379
Main measures
Physical illnesses
A question which enquired about the presence of 20 physical health conditions was used to assess physical illnesses (cancer, diabetes, epilepsy, migraine, cataracts/eyesight problems, ear/hearing problems, stroke, heart attack/angina, high blood pressure, bronchitis/emphysema, asthma, allergies, stomach ulcer or other digestive problems, liver problems, bowel/colon problems, bladder problems/incontinence, arthritis, bone/back/joint/muscle problems, infectious disease, and skin problems). To be counted, conditions had to have been diagnosed by a doctor or other health professional and have been present in the previous 12 months. The number of physical diseases was summed and categorized as 0, 1, 2, 3, 4, and ≥5. Multimorbidity was defined as two or more physical diseases [31].
Loneliness
This was measured with one item from the Social Functioning Questionnaire (SFQ) [32]. Respondents were asked to assess to what extent they had felt ‘lonely and isolated from other people’ in the previous two weeks. The answer options were ‘very much’, ‘sometimes’, ‘not often’, and ‘not at all’. In the current study, response options were dichotomized with those who answered ‘sometimes’ and ‘very much’ being categorized as lonely [33].
Covariates
Smoking
The question, ‘Have you ever smoked a cigarette?’ with ‘yes’ or ‘no’ answer options was used to assess smoking status.
Alcohol dependence
This was assessed with two instruments. The Alcohol Use Disorders Identification Test (AUDIT) was firstly used to assess alcohol consumption [34]. When a respondent’s AUDIT score was ≥ 10 they were also assessed for alcohol dependence using the Severity of Alcohol Dependence Questionnaire (SADQ-C) [35]. Those who scored ≥ 4/60 on this measure were categorized as having past 6-month alcohol dependence.
Drug use
Information was obtained on the past year use of the following drugs: cannabis, amphetamines, cocaine, crack, ecstasy, heroin, acid or LSD, magic mushrooms, methadone or physeptone, tranquilizers, amyl nitrate, anabolic steroids, and glues. Respondents taking any of these drugs were categorized as past 12-month drug users.
Disordered eating
Possible eating disorder was assessed with five items from the SCOFF eating disorder screening tool [36]. Respondents were asked whether, in the past year, they (1) had lost more than one stone (6.35kg) in 3 months; (2) had made him/herself be sick because he/she felt uncomfortably full; (3) had worried that he/she had lost control over how much he/she eats; (4) believed [himself/herself] to be fat when others said that he/she was too thin; and (5) thought that food dominated his/her life. Using yes/no response options, a positive screen was categorized as two or more affirmative answers [36].
Obesity
Self-reported weight and height data were used to determine body mass index (BMI), calculated as weight in kilograms divided by height in meters squared. As a preliminary examination of the data revealed that only extreme levels of obesity were associated with loneliness, we used ≥35 kg/m2 (obesity class I) as the cut-off.
Stressful life events
Seventeen questions on the lifetime occurrence of experiences such as the death of a family member, financial crises, sexual abuse etc., were used to assess stressful life events (S1 Table). Two different stressful life events measures were constructed depending on whether the event last occurred when the respondent was <16 or ≥16 years of age. For the latter measure, a summed total number of stressful life events was based on all 17 questions, while 8 age-appropriate potentially stressful life events were assessed before age 16 (all of which had a prevalence of at least 2%) (S1 Table).
Depressive episode and anxiety disorders
The Clinical Interview Schedule Revised (CIS-R), was used to identify non-psychotic symptoms in the prior week to generate ICD-10 diagnoses of depressive episode and anxiety disorders (generalized anxiety disorder, panic disorder, phobia, obsessive-compulsive disorder) [37].
Social support
This was assessed with a 7-item measure. Using answer options ‘not true’ (score = 0), ‘partly true’ (score = 1) and ‘certainly true’ (score = 2), participants responded to statements which inquired if, family and friends did things to make them happy, made them feel loved, could be relied on no matter what, would see that they were taken care of no matter what, accepted them just the way they are, made them feel an important part of their lives, and gave them support and encouragement. Responses were added to create a scale score that could range from 0 to 14. The internal consistency of the scale was good: α = 0.89.
Socio-demographic variables
Information was also obtained on age, sex, equivalized income tertiles (high ≥£29826, middle £14,057 to < £29826, low <£14,057), education [qualification (degree, non-degree, A-level, GCSE, other): yes or no)], and ethnicity (white British or other).
Statistical analysis
Differences in sample characteristics by the presence of loneliness were tested with Chi-square tests and Student’s t-tests for categorical and continuous variables, respectively. To examine the association between physical multimorbidity and loneliness, a multivariable logistic regression analysis was performed with loneliness as the dependent variable and the number of physical diseases as the independent variable that adjusted for the socio-demographic variables (age, sex, income, education, and ethnicity). An age-stratified analysis was also conducted to assess whether the association differed between different age groups.
To determine if any factors mediated the association between loneliness and physical multimorbidity (i.e., ≥2 physical diseases) (outcome), a meditation analysis was performed using the khb (Karlson Holm Breen) command in Stata [38]. This method can be used with logistic regression analysis to decompose the total effect of a variable into its direct and indirect effects (i.e., mediational effect). This allows the percentage of the main association explained by the mediator to be calculated (mediated percentage). Potential mediators (smoking, alcohol dependence, drug use, disordered eating, obesity, stressful life events, social support, depression, anxiety) were selected using past literature as a guide. Each potential mediator was included in the model individually. The mediation analysis controlled for the five socio-demographic variables. In order to assess whether the mediators differ by age group, we also conducted age-stratified analyses.
As nearly 20% of the participants had missing income information and in order to avoid the exclusion of a large number of respondents, a missing category for this variable was included in all regression analyses. Age-stratified analyses were not adjusted for age. All variables were included in the models as categorical variables, excepting the stressful life events and social support variables (continuous). The sample weighting and the complex study design were taken into account in order to generate nationally representative estimates. Odds ratios (OR) and 95% confidence intervals (95%CI) are reported. The level of statistical significance was set at P<0.05. All analyses were performed with Stata version 14.1 (Stata Corp LP, College Station, Texas).
Results
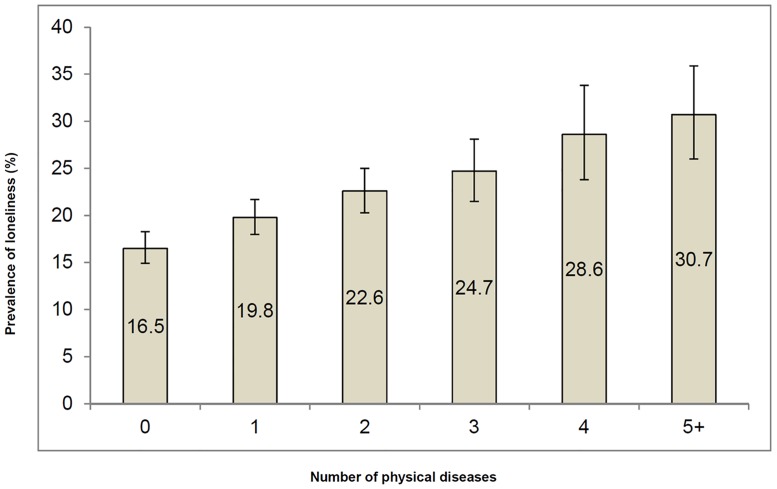
There were significant differences between lonely and non-lonely people for all of the sample characteristics except for ethnicity and smoking status (Table 1). Lonely people were more likely to have two or more physical diseases. A graded association between the presence of physical disease and loneliness is illustrated in Fig 1 with the prevalence of loneliness rising from 16.5% in those with no physical diseases to 30.7% among those with 5 or more diseases. Besides a higher number of physical diseases, lonely people also had a higher prevalence of adverse outcomes such as alcohol dependence, drug use, stressful events across the life course, poorer mental health (anxiety and depression) and lower social support.
Table 1. Sample characteristics (overall and by loneliness).
| Characteristic | Category | Overall | Loneliness | P-valuea | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| Number of physical diseases | 0 | 2,373 | 36.5 | 1,961 | 38.3 | 412 | 29.6 | <0.001 |
| 1 | 2,020 | 28.3 | 1,593 | 28.6 | 427 | 27.5 | ||
| 2 | 1,335 | 16.7 | 1,017 | 16.3 | 318 | 18.5 | ||
| 3 | 804 | 9.4 | 587 | 8.9 | 217 | 11.3 | ||
| 4 | 402 | 4.6 | 276 | 4.1 | 126 | 6.4 | ||
| ≥5 | 423 | 4.5 | 279 | 3.9 | 144 | 6.7 | ||
| Age (y) | 16–44 | 2,871 | 48.1 | 2,183 | 47.0 | 688 | 52.4 | <0.001 |
| 45–64 | 2,406 | 32.3 | 1,864 | 32.6 | 542 | 31.2 | ||
| ≥65 | 1,954 | 19.6 | 1,564 | 20.4 | 390 | 16.5 | ||
| Sex | Male | 3,176 | 48.6 | 2,544 | 50.1 | 632 | 42.8 | <0.001 |
| Female | 4,184 | 51.4 | 3,172 | 49.9 | 1,012 | 57.2 | ||
| Income | High | 1,972 | 35.9 | 1,623 | 37.4 | 349 | 29.5 | <0.001 |
| Middle | 1,932 | 32.6 | 1,512 | 32.9 | 420 | 31.5 | ||
| Low | 1,957 | 31.5 | 1,426 | 29.7 | 531 | 39.0 | ||
| Qualification | No | 2,103 | 23.9 | 1,570 | 23.3 | 533 | 26.1 | 0.041 |
| Yes | 5,225 | 76.1 | 4,123 | 76.7 | 1,102 | 73.9 | ||
| Ethnicity | British White | 6,478 | 85.2 | 5,053 | 85.5 | 1,425 | 84.1 | 0.285 |
| Other | 847 | 14.8 | 639 | 14.5 | 208 | 15.9 | ||
| Smoking | No | 2,481 | 34.7 | 1,971 | 35.3 | 510 | 32.2 | 0.339 |
| Yes | 4,879 | 65.3 | 3,745 | 64.7 | 1,134 | 67.8 | ||
| Alcohol dependence | No | 6,995 | 94.1 | 5,493 | 95.4 | 1,502 | 89.2 | <0.001 |
| Yes | 365 | 5.9 | 223 | 4.6 | 142 | 10.8 | ||
| Drug use | No | 6,813 | 90.7 | 5,369 | 92.3 | 1,444 | 84.7 | <0.001 |
| Yes | 534 | 9.3 | 340 | 7.7 | 194 | 15.3 | ||
| Disordered eating | No | 6,897 | 93.6 | 5,500 | 96.2 | 1,397 | 83.2 | <0.001 |
| Yes | 450 | 6.4 | 206 | 3.8 | 244 | 16.8 | ||
| Obesity class I (BMI≥35 kg/m2) | No | 6,617 | 94.6 | 5,163 | 95.0 | 1,454 | 93.0 | 0.009 |
| Yes | 388 | 5.4 | 280 | 5.0 | 108 | 7.0 | ||
| Stressful life events (≥16 years)b | Mean (SD) | 2.6 (2.0) | 2.5 (1.9) | 3.3 (2.5) | <0.001 | |||
| Stressful life events (<16 years)c | Mean (SD) | 0.5 (1.0) | 0.4 (0.9) | 0.8 (1.2) | <0.001 | |||
| Social supportd | Mean (SD) | 13.2 (1.9) | 13.4 (1.6) | 12.4 (2.8) | <0.001 | |||
| Depression | No | 7,109 | 97.0 | 5,651 | 99.0 | 1,458 | 89.3 | <0.001 |
| Yes | 251 | 3.0 | 65 | 1.0 | 186 | 10.7 | ||
| Anxiety | No | 6,828 | 93.3 | 5,537 | 97.0 | 1,291 | 78.7 | <0.001 |
| Yes | 532 | 6.7 | 179 | 3.0 | 353 | 21.3 | ||
Note: Boldface type indicates statistical significance (p<0.05).
Abbreviation: SD standard deviation; Data are unweighted N and weighted percentage or mean (SD).
a The differences in sample characteristics was tested by Chi-square tests and Student’s t-tests for categorical and continuous variables respectively.
b Based on 17 stressful life events occurring at the age of 16 or after.
c Based on 8 stressful life events occurring before the age of 16.
d Seven items were used to identify the level of social support with each item having scores of 0, 1, or 2. Scores of the 7 items were added to create a scale ranging from 0–14 with higher scores corresponding to higher levels of social support.
Fig 1. Prevalence of loneliness by the number of physical diseases.
Bars denote 95% confidence intervals. Estimates are based on weighted sample.
In a multivariable logistic regression analysis that controlled for socio-demographic factors, there was a statistically significant monotonic association between the number of physical diseases (independent variable) and loneliness (dependent variable) with the OR for loneliness rising from 1.34 (95% CI: 1.13–1.59) for those with one disease to almost 3 (OR: 2.82, 95% CI: 2.11–3.78) for those with 5 or more diseases, compared to those with no physical diseases. When the analysis was stratified by age, the associations were stronger across all levels of disease in the youngest age group (16–44 years) (Table 2).
Table 2. Association between number of physical diseases and loneliness estimated by multivariable logistic regression analysis.
| Overall | Age (16–44 years) | Age (45–64 years) | Age (≥65 years) | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI |
| Number of physical diseases | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 1 | 1.34*** | [1.13,1.59] | 1.41** | [1.14,1.75] | 0.91 | [0.61,1.37] | 0.93 | [0.61,1.43] |
| 2 | 1.66*** | [1.37,2.02] | 1.84*** | [1.39,2.45] | 1.24 | [0.82,1.89] | 1.28 | [0.83,1.97] |
| 3 | 1.92*** | [1.52,2.43] | 2.24*** | [1.49,3.37] | 1.47 | [0.96,2.23] | 1.53 | [0.99,2.35] |
| 4 | 2.57*** | [1.92,3.43] | 2.97*** | [1.68,5.25] | 1.77* | [1.09,2.89] | 1.78* | [1.08,2.93] |
| ≥5 | 2.82*** | [2.11,3.78] | 3.09** | [1.53,6.24] | 1.90** | [1.23,2.93] | 1.94** | [1.25,3.01] |
| Age (years) | ||||||||
| 16–44 | 1.00 | |||||||
| 45–64 | 0.70*** | [0.61,0.82] | ||||||
| ≥65 | 0.44*** | [0.37,0.53] | ||||||
| Sex | ||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 1.21** | [1.07,1.37] | 1.16 | [0.96,1.41] | 1.73*** | [1.34,2.24] | 1.75*** | [1.34,2.28] |
| Income | ||||||||
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Middle | 1.22* | [1.03,1.44] | 1.09 | [0.83,1.43] | 1.49 | [0.89,2.51] | 1.51 | [0.88,2.61] |
| Low | 1.62*** | [1.37,1.91] | 1.65*** | [1.28,2.12] | 1.29 | [0.77,2.15] | 1.28 | [0.74,2.21] |
| Qualification | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.84* | [0.71,0.99] | 0.73 | [0.52,1.04] | 0.68** | [0.54,0.86] | 0.67** | [0.53,0.85] |
| Ethnicity | ||||||||
| British White | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Other | 1.06 | [0.86,1.31] | 1.07 | [0.83,1.37] | 1.46 | [0.80,2.67] | 1.44 | [0.74,2.78] |
Note: Boldface type indicates statistical significance (* p<0.05, ** p<0.01, *** p<0.001)
Abbreviation: OR odds ratio; CI confidence interval
Models are adjusted for all variables in the respective columns.
The mediation analysis showed that stressful life events both before and after 16 years of age mediated 11.1% and 30.5% of the association between loneliness and multimorbidity, respectively, while depression (15.4% mediated), anxiety (30.2%) and disordered eating (10.1%) were also important mediators. In contrast, there were no significant mediational effects for smoking, alcohol dependence, drug use, obesity or social support (Table 3). When an age-stratified mediation analysis was performed, the same variables were important for adults aged 16–44 and 45–64. Specifically, depression, anxiety, stressful life events before and after age 16 and disordered eating were all significant mediators in the association between multimorbidity and loneliness although stressful life events in adulthood was the strongest mediator for adults aged 16–44 whereas for adults aged 45–64, anxiety was the strongest mediator. For adults aged 65 and above the only variable which was a significant mediator was stressful life events in adulthood which mediated 11.8% of the association (S2 Table).
Table 3. Lifestyle and other potential mediators in the association between loneliness and multimorbidity.
| Mediator | Effect | OR | 95%CI | P-value | % Mediated |
|---|---|---|---|---|---|
| Smoking | Total | 1.67 | [1.46, 1.91] | <0.001 | NA |
| Direct | 1.66 | [1.46, 1.90] | <0.001 | ||
| Indirect | 1.01 | [1.00, 1.01] | 0.085 | ||
| Alcohol dependence | Total | 1.67 | [1.46, 1.91] | <0.001 | NA |
| Direct | 1.65 | [1.44, 1.88] | <0.001 | ||
| Indirect | 1.01 | [1.00, 1.03] | 0.078 | ||
| Drug use | Total | 1.67 | [1.46, 1.91] | <0.001 | NA |
| Direct | 1.65 | [1.44, 1.88] | <0.001 | ||
| Indirect | 1.01 | [1.00, 1.03] | 0.137 | ||
| Disordered eating | Total | 1.67 | [1.46, 1.91] | <0.001 | 10.1 |
| Direct | 1.58 | [1.38, 1.81] | <0.001 | ||
| Indirect | 1.05 | [1.02, 1.08] | <0.001 | ||
| Obesity class I | Total | 1.64 | [1.44, 1.88] | <0.001 | NA |
| (BMI≥35 kg/m2) | Direct | 1.62 | [1.42, 1.86] | <0.001 | |
| Indirect | 1.01 | [1.00, 1.03] | 0.081 | ||
| Stressful life events | Total | 1.68 | [1.47, 1.93] | <0.001 | 30.5 |
| (≥16 years) | Direct | 1.44 | [1.25, 1.65] | <0.001 | |
| Indirect | 1.17 | [1.13, 1.22] | <0.001 | ||
| Stressful life events | Total | 1.67 | [1.46, 1.91] | <0.001 | 11.1 |
| (<16 years) | Direct | 1.58 | [1.38, 1.81] | <0.001 | |
| Indirect | 1.06 | [1.03, 1.09] | <0.001 | ||
| Social support | Total | 1.67 | [1.47, 1.91] | <0.001 | NA |
| Direct | 1.68 | [1.46, 1.93] | <0.001 | ||
| Indirect | 1.00 | [0.97, 1.02] | 0.806 | ||
| Depression | Total | 1.67 | [1.46, 1.91] | <0.001 | 15.4 |
| Direct | 1.54 | [1.35, 1.77] | <0.001 | ||
| Indirect | 1.08 | [1.05, 1.12] | <0.001 | ||
| Anxiety | Total | 1.67 | [1.46, 1.91] | <0.001 | 30.2 |
| Direct | 1.43 | [1.25, 1.64] | <0.001 | ||
| Indirect | 1.17 | [1.12, 1.22] | <0.001 |
Note: Boldface type indicates statistical significance (p<0.05)
Abbreviation: OR odds ratio; CI confidence interval
Models are adjusted for age, sex, income, qualification, and ethnicity.
Multimorbidity refers to two or more physical diseases.
Percentage mediated is only provided when the indirect effect is statistically significant.
Discussion
This study examined the association between multiple co-occurring physical diseases and loneliness in a nationally representative sample of the English population. The results showed that the number of co-occurring physical diseases was associated with loneliness in a dose-response fashion after adjustment for socio-demographic factors, particularly in the youngest age group (aged 16–44 years). In addition, stressful life events across the life course and poor mental health (anxiety and depression) were important mediators in the association between multimorbidity and loneliness.
Although prior research has produced mixed results on the association between the number of diseases/multimorbidity and loneliness [25–29], the results of the current study accord with previous studies which showed an association [25–28], and which also found that the strength of the association varied between different populations/population subgroups [26]. The exact way in which physical disease and loneliness are linked is uncertain although the results from the mediation analysis point to several possible pathways. In particular, mental illness was an important mediator in the association. This accords with research which has linked physical multimorbidity and depression [10], possibly due to the feelings of inadequacy, dependency and dejection it can give rise to [39], as well as with studies which have shown that worse mental health is associated with loneliness [40]. In terms of the specific association, a recent study found that depression was linked to lower participation in social leisure activities in older adults with multimorbidity [41] which might be important for feelings of loneliness.
Stressful life events across the life course (both before and after age 16) were also an important factor in the association between multimorbidity and loneliness. Research has shown that stressful events in early life are linked to an increased risk for both later multimorbidity and loneliness [42,43] possibly as a result of physiological changes they may cause that might increase the risk for future disease [44] as well as through problems with bonding and trust [43]. Given this, it is possible that such events might be a common third factor underlying the occurrence of both multimorbidity and loneliness in adulthood. Alternatively, stressful life events might also mediate the association with loneliness. For example, stressors such as divorce, separation and widowhood that might be important for loneliness have been associated with multimorbidity in middle-aged adults [45]. Another adult stressor which might be a direct consequence of co-occurring physical diseases—an inability to work—might also play a role here, as multimorbidity has been associated with unemployment [46] which in turn, might be important for loneliness [12,47].
As this study was cross-sectional it was not possible for us to establish causality or determine the direction of the observed associations. It is possible therefore that loneliness might also have led to multimorbidity. For instance, it has been suggested that the hypervigilance for social threats in the surrounding environment, distorted cognitions and a negative disposition (e.g. feelings of stress, anxiety, hostility) that are all associated with loneliness may result in behavioral and physiological changes that can impact negatively on health [48]. Indeed, there is a growing body of evidence that loneliness is linked to biological changes that might be adverse for health such as higher systolic blood pressure [49], differences in diastolic blood pressure reactivity [50] and cardiovascular functioning [51], as well as an increased risk for metabolic syndrome [52] that might underlie co-occurring physical diseases. Our finding that stressful life events link multimorbidity and loneliness also provides some support for the idea that loneliness might be a precursor of physical disease and multimorbidity as previous research has indicated that (perceived) stress may mediate the association between loneliness and physical ill health [53,54].
Stratifying the analysis by age revealed that the association between physical multimorbidity and loneliness was strongest in the youngest age group. Given that multimorbidity has been associated with increasing age [55] and that it has been hypothesized that the effects of loneliness might accrue across the life course in terms of their negative effect on physiological resilience (and thus, health) [56], the finding of a stronger association between multimorbidity and loneliness in the youngest age group is somewhat unexpected and it can only be speculated what underlies this result. It is possible, for instance, that a higher number of chronic diseases might affect a younger person’s ability to engage in age-related social roles (e.g., spouse, parent, and/or worker) and social activities and thus act to isolate them. In contrast, older individuals might have fewer roles or activities and/or had more time to adapt to the inhibiting effects of several physical illnesses so that only those with a higher number of co-occurring illnesses experience loneliness. Indeed, the potentially greater detrimental impact of co-occurring diseases at a younger age might explain why depression and anxiety were important mediators in the association between multimorbidity and loneliness in those aged under 65 but not in the oldest age group. The same might also be true when looking at loneliness leading to physical disease. Specifically, as research has indicated that the prevalence of loneliness might be higher at both ends of the life span i.e. in adolescence/young adulthood and old age [57], it is possible that loneliness might have a stronger effect on well-being during an age period where people are expected to be involved in a variety of personal and work-related relations and where loneliness is less common.
This study has several limitations. Physical illnesses were self-reported and were not verified against other sources of data such as medical records. This might have resulted in misreporting in some instances especially as evidence suggests that while self-reports of physical illness mostly accord with doctor’s reports, not all diseases are reported with equal accuracy, and there might also be age-related differences in the reliability of reports for some diseases [58]. In addition, the survey response rate was moderate (57%) [30]. As research has shown that lonely individuals trust others less and may be less likely to disclose intimate information for fear that confidentiality will not be maintained [59], it is possible that they might have been over-represented among non-responders which might have affected the results (i.e. non-response bias). Finally, following the lead of an earlier study which used APMS data [33], we used an item from the SFQ as a measure of loneliness. However, it should be noted that this item also mentioned ‘isolation’. We were unable therefore to tease apart the association between loneliness and social isolation in our study despite the fact that they are often studied separately and may have different effects on health outcomes [60].
In conclusion, this study has shown that physical multimorbidity is associated with increased odds for loneliness. Given the possible bi-directionality of the association between ill health and loneliness, this highlights the importance of future longitudinal research to better specify the association between these phenomena across time, and the potential mechanisms that might underlie it.
Supporting information
Events that occurred before the age of 16 are indicated with a tick mark.
(DOCX)
(DOCX)
Acknowledgments
We would like to thank the National Center for Social Research and the University of Leicester who were the Principal Investigators of this survey. In addition, we would also like to thank the UK Data Archive and the National Center for Social Research as the data collectors and for making these data publically available. They bear no responsibility for this analysis or interpretation of this publicly available dataset.
Data Availability
The data used in this study are third party data (i.e., they are not owned and were not collected by the authors) that have been made publicly available by the National Center for Social Research via the UK data archive. The authors did not have any special access privileges and other authors can access these data in the same manner as the authors in this study did, i.e., registration is required and standard conditions of use apply. Details of how to access the Adult Psychiatric Morbidity Survey 2007 dataset are available at: https://discover.ukdataservice.ac.uk/catalogue/?sn=6379.
Funding Statement
Ai Koyanagi’s work was supported by the Miguel Servet contract financed by the CP13/00150 and PI15/00862 projects, integrated into the National R + D + I and funded by the ISCIII - General Branch Evaluation and Promotion of Health Research - and the European Regional Development Fund (ERDF-FEDER). These organizations had no role in the study design, collection, analysis and interpretation; in the writing of the manuscript; and in the decision to submit the paper for publication.
References
- 1.Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016; 71: 205–214. doi: 10.1093/gerona/glv128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Afshar S, Roderick PJ, Kowal P, Dimitrov BD, Hill AG. Multimorbidity and the inequalities of global ageing: a cross-sectional study of 28 countries using the World Health Surveys. BMC Public Health. 2015; 15: 776 doi: 10.1186/s12889-015-2008-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012; 380: 37–43. doi: 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 4.Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D. Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes. 2004; 2: 51 doi: 10.1186/1477-7525-2-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kadam UT, Croft PR, North Staffordshire GP Consortium Group. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007; 24: 412–419. doi: 10.1093/fampra/cmm049 [DOI] [PubMed] [Google Scholar]
- 6.Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011; 28: 516–523. doi: 10.1093/fampra/cmr013 [DOI] [PubMed] [Google Scholar]
- 7.The Emerging Risk Factors Collaboration. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015; 314: 52–60. doi: 10.1001/jama.2015.7008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stickley A, Koyanagi A, Takahashi H, Ruchkin V, Inoue Y, Kamio Y. Attention-deficit/hyperactivity disorder and physical multimorbidity: a population-based study. Eur Psychiatry. 2017; 45: 227–234. doi: 10.1016/j.eurpsy.2017.07.010 [DOI] [PubMed] [Google Scholar]
- 9.Quirk SE, Stuart AL, Berk M, Pasco JA, Brennan Olsen SL, Koivumaa-Honkanen H, et al. Personality disorder is an excess risk factor for physical multimorbidity among women with mental state disorders. Psychiatry Res. 2017; 257: 546–549. doi: 10.1016/j.psychres.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 10.Stubbs B, Vancampfort D, Veronese N, Kahl KG, Mitchell AJ, Lin PY, et al. Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol Med. 2017; 47: 2107–2117. doi: 10.1017/S0033291717000551 [DOI] [PubMed] [Google Scholar]
- 11.Stubbs B, Koyanagi A, Veronese N, Vancampfort D, Solmi M, Gaughran F, et al. Physical multimorbidity and psychosis: comprehensive cross sectional analysis including 242,952 people across 48 low- and middle-income countries. BMC Med. 2016; 14: 189 doi: 10.1186/s12916-016-0734-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perlman D, Peplau LA. Toward a social psychology of loneliness In: Duck S, Gilmour R, editors. Personal relationships: 3. Personal relationships in disorder. London: Academic Press; 1981. pp. 31–56. [Google Scholar]
- 13.Griffin J. The lonely society? London: Mental Health Foundation; 2010. [Google Scholar]
- 14.Victor CR, Yang K. The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol. 2012; 146: 85–104. doi: 10.1080/00223980.2011.613875 [DOI] [PubMed] [Google Scholar]
- 15.Stickley A, Koyanagi A, Koposov R, Schwab-Stone M, Ruchkin V. Loneliness and health risk behaviours among Russian and U.S. adolescents: a cross-sectional study. BMC Public Health. 2014; 14: 366 doi: 10.1186/1471-2458-14-366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stickley A, Koyanagi A, Roberts B, Richardson E, Abbott P, Tumanov S, et al. Loneliness: its correlates and association with health behaviours and outcomes in nine countries of the former Soviet Union. PLoS One. 2013; 8: e67978 doi: 10.1371/journal.pone.0067978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olsen RB, Olsen J, Gunner-Svensson F, Waldstrøm B. Social networks and longevity. A 14 year follow-up study among elderly in Denmark. Soc Sci Med. 1991; 33: 1189–1195. [DOI] [PubMed] [Google Scholar]
- 18.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012; 74: 907–914. doi: 10.1016/j.socscimed.2011.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holwerda TJ, Beekman AT, Deeg DJ, Stek ML, van Tilburg TG, Visser PJ, et al. Increased risk of mortality associated with social isolation in older men: only when feeling lonely? Results from the Amsterdam Study of the Elderly (AMSTEL). Psychol Med. 2012; 42: 843–853. doi: 10.1017/S0033291711001772 [DOI] [PubMed] [Google Scholar]
- 20.Penninx BW, van Tilburg T, Kriegsman DM, Boeke AJ, Deeg DJ, van Eijk JT. Social network, social support, and loneliness in older persons with different chronic diseases. J Aging Health. 1999; 11: 151–168. doi: 10.1177/089826439901100202 [DOI] [PubMed] [Google Scholar]
- 21.Tomaka J, Thompson S, Palacios R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J Aging Health. 2006; 18: 359–384. doi: 10.1177/0898264305280993 [DOI] [PubMed] [Google Scholar]
- 22.Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009; 71: 836–842. doi: 10.1097/PSY.0b013e3181b40efc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Momtaz YA, Hamid TA, Yusoff S, Ibrahim R, Chai ST, Yahaya N, et al. Loneliness as a risk factor for hypertension in later life. J Aging Health. 2012; 24: 696–710. doi: 10.1177/0898264311431305 [DOI] [PubMed] [Google Scholar]
- 24.Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry 2007; 64: 234–240. doi: 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- 25.Jessen MAB, Pallesen AVJ, Kriegbaum M, Kristiansen M. The association between loneliness and health—a survey-based study among middle-aged and older adults in Denmark. Aging Ment Health. 2017; in press: doi: 10.1080/13607863.2017.1348480 [DOI] [PubMed] [Google Scholar]
- 26.Wister A, Kendig H, Mitchell B, Fyffe I, Loh V. Multimorbidity, health and aging in Canada and Australia: a tale of two countries. BMC Geriatr. 2016; 16: 163 doi: 10.1186/s12877-016-0341-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Arch Psychiatr Nurs. 2009; 23: 387–396. doi: 10.1016/j.apnu.2008.11.002 [DOI] [PubMed] [Google Scholar]
- 28.Cohen-Mansfield J, Shmotkin D, Goldberg S. Loneliness in old age: longitudinal changes and their determinants in an Israeli sample. Int Psychogeriatr. 2009; 21: 1160–1170. doi: 10.1017/S1041610209990974 [DOI] [PubMed] [Google Scholar]
- 29.Cower P, Knaevelsrud C, Pietrzak RH. Loneliness among older veterans in the United States: results from the National Health and Resilience in Veterans Study. Am J Geriatr Psychiatry. 2014; 22: 564–569. doi: 10.1016/j.jagp.2013.02.013 [DOI] [PubMed] [Google Scholar]
- 30.McManus S, Meltzer H, Brugha T, Bebbington P, Jenkins R. Adult psychiatric morbidity in England 2007: results of a household survey. London: National Centre for Social Research; 2009. [Google Scholar]
- 31.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013; 35: 75–83. [DOI] [PubMed] [Google Scholar]
- 32.Tyrer P, Nur U, Crawford M, Karlsen S, McLean C, Rao B, et al. The Social Functioning Questionnaire: a rapid and robust measure of perceived functioning. Int J Soc Psychiatry. 2005; 51: 265–275. [PubMed] [Google Scholar]
- 33.Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013; 48: 5–13. doi: 10.1007/s00127-012-0515-8 [DOI] [PubMed] [Google Scholar]
- 34.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993; 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 35.Stockwell T, Sitharthan T, McGrath D, Lang E. The measurement of alcohol dependence and impaired control in community samples. Addiction. 1994; 89: 167–174. [DOI] [PubMed] [Google Scholar]
- 36.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999; 319: 1467–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med. 1992; 22: 465–486. [DOI] [PubMed] [Google Scholar]
- 38.Breen R, Karlson KB, Holm A. Total, direct, and indirect effects in logit and probit models. Sociol Methods Res. 2013; 42: 164–191. [Google Scholar]
- 39.Eckerblad J, Theander K, Ekdahl A, Jaarsma T, Hellstrom I. To adjust and endure: a qualitative study of symptom burden in older people with multimorbidity. Appl Nurs Res. 2015; 28: 322–327. doi: 10.1016/j.apnr.2015.03.008 [DOI] [PubMed] [Google Scholar]
- 40.Chrostek A, Grygiel P, Anczewska M, Wciórka J, Świtaj P. The intensity and correlates of the feelings of loneliness in people with psychosis. Compr Psychiatry. 2016; 70: 190–199. doi: 10.1016/j.comppsych.2016.07.015 [DOI] [PubMed] [Google Scholar]
- 41.Galenkamp H, Gagliardi C, Principi A, Golinowska S, Moreira A, Schmidt AE, et al. Predictors of social leisure activities in older Europeans with and without multimorbidity. Eur J Ageing. 2016; 13: 129–143. doi: 10.1007/s10433-016-0375-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sinnott C, Mc Hugh S, Fitzgerald AP, Bradley CP, Kearney PM. Psychosocial complexity in multimorbidity: the legacy of adverse childhood experiences. Fam Pract. 2015; 32: 269–275. doi: 10.1093/fampra/cmv016 [DOI] [PubMed] [Google Scholar]
- 43.Palgi Y, Shrira A, Ben-Ezra M, Shiovitz-Ezra S, Ayalon L. Self- and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging Ment Health. 2012; 16: 423–430. doi: 10.1080/13607863.2011.638903 [DOI] [PubMed] [Google Scholar]
- 44.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012; 106: 29–39. doi: 10.1016/j.physbeh.2011.08.019 [DOI] [PubMed] [Google Scholar]
- 45.Taylor AW, Price K, Gill TK, Adams R, Pilkington R, Carrangis N, et al. Multimorbidity—not just an older person’s issue. Results from an Australian biomedical study. BMC Public Health. 2010; 10: 718 doi: 10.1186/1471-2458-10-718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang HH, Wang JJ, Wong SY, Wong MC, Li FJ, Wang PX, et al. Epidemiology of multimorbidity in China and implications for the healthcare system: cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014; 12: 188 doi: 10.1186/s12916-014-0188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin Psychol Rev. 2006; 26: 695–718. doi: 10.1016/j.cpr.2006.04.002 [DOI] [PubMed] [Google Scholar]
- 48.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010; 40: 218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006; 21: 152–164. doi: 10.1037/0882-7974.21.1.152 [DOI] [PubMed] [Google Scholar]
- 50.Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004; 29: 593–611. doi: 10.1016/S0306-4530(03)00086-6 [DOI] [PubMed] [Google Scholar]
- 51.Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol. 2003; 85: 105–120. [DOI] [PubMed] [Google Scholar]
- 52.Whisman MA. Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychol. 2010; 29: 550–554. doi: 10.1037/a0020760 [DOI] [PubMed] [Google Scholar]
- 53.Segrin C, Passalacqua SA. Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun. 2010; 25: 312–322. doi: 10.1080/10410231003773334 [DOI] [PubMed] [Google Scholar]
- 54.Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Soc Sci Med. 2016; 152: 80–86. doi: 10.1016/j.socscimed.2016.01.020 [DOI] [PubMed] [Google Scholar]
- 55.Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011; 61: e12–e21. doi: 10.3399/bjgp11X548929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hawkley LC, Cacioppo JT. Aging and loneliness: downhill quickly? Curr Dir Psychol Sci. 2007; 16: 187–191. [Google Scholar]
- 57.Qualter P, Vanhalst J, Harris R, Van Roekel E, Lodder G, Bangee M, et al. Loneliness across the life span. Perspect Psychol Sci. 2015; 10: 250–264. doi: 10.1177/1745691615568999 [DOI] [PubMed] [Google Scholar]
- 58.Kriegsman DM, Penninx BW, van Eijk JT, Boeke AJ, Deeg DJ. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996; 49: 1407–1417. [DOI] [PubMed] [Google Scholar]
- 59.Rotenberg KJ. Loneliness and interpersonal trust. J Soc Clin Psychol. 1994; 13: 152–173. [Google Scholar]
- 60.Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health. 2012; 24: 1346–1363. doi: 10.1177/0898264312460275 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Events that occurred before the age of 16 are indicated with a tick mark.
(DOCX)
(DOCX)
Data Availability Statement
The data used in this study are third party data (i.e., they are not owned and were not collected by the authors) that have been made publicly available by the National Center for Social Research via the UK data archive. The authors did not have any special access privileges and other authors can access these data in the same manner as the authors in this study did, i.e., registration is required and standard conditions of use apply. Details of how to access the Adult Psychiatric Morbidity Survey 2007 dataset are available at: https://discover.ukdataservice.ac.uk/catalogue/?sn=6379.
The data used in this study are third party data (i.e., they are not owned and were not collected by the authors) that have been made publicly available by the National Center for Social Research via the UK data archive. The authors did not have any special access privileges and other authors can access these data in the same manner as the authors in this study did i.e. registration is required and standard conditions of use apply. Details of how to access the Adult Psychiatric Morbidity Survey 2007 dataset are available at: https://discover.ukdataservice.ac.uk/catalogue/?sn=6379