Abstract
Background:
Few studies have examined variation in the associations between heat waves and mortality in an international context.
Objectives:
We aimed to systematically examine the impacts of heat waves on mortality with lag effects internationally.
Methods:
We collected daily data of temperature and mortality from 400 communities in 18 countries/regions and defined 12 types of heat waves by combining community-specific daily mean temperature , 92.5th, 95th, and 97.5th percentiles of temperature with duration , 3, and 4 d. We used time-series analyses to estimate the community-specific heat wave–mortality relation over lags of 0–10 d. Then, we applied meta-analysis to pool heat wave effects at the country level for cumulative and lag effects for each type of heat wave definition.
Results:
Heat waves of all definitions had significant cumulative associations with mortality in all countries, but varied by community. The higher the temperature threshold used to define heat waves, the higher heat wave associations on mortality. However, heat wave duration did not modify the impacts. The association between heat waves and mortality appeared acutely and lasted for 3 and 4 d. Heat waves had higher associations with mortality in moderate cold and moderate hot areas than cold and hot areas. There were no added effects of heat waves on mortality in all countries/regions, except for Brazil, Moldova, and Taiwan. Heat waves defined by daily mean and maximum temperatures produced similar heat wave–mortality associations, but not daily minimum temperature.
Conclusions:
Results indicate that high temperatures create a substantial health burden, and effects of high temperatures over consecutive days are similar to what would be experienced if high temperature days occurred independently. People living in moderate cold and moderate hot areas are more sensitive to heat waves than those living in cold and hot areas. Daily mean and maximum temperatures had similar ability to define heat waves rather than minimum temperature. https://doi.org/10.1289/EHP1026
Introduction
Globally, there is increasing interest in assessing heat wave–related health effects after major heat waves in the United States and Europe, for example, Chicago in 1995 and Europe in 2003 (Le Tertre et al. 2006; Semenza et al. 1996). Several recent studies have linked heat waves with significant impacts on human health, including mortality (Kent et al. 2014; Li et al. 2015; Wang et al. 2015). The frequency, intensity, and duration of heat waves will increase in the future, which has the potential to greatly exacerbate the health impacts of heat (Field et al. 2014). Thus, understanding the relationship between heat waves and health is crucial for better adaptation and mitigation strategies (Meehl and Tebaldi 2004).
Recently, a few studies have suggested decomposing the health impacts of heat waves into a) effects of high temperature through modeling daily temperature as a numeric explanatory variable, possibly allowing for lagged effects; and b) added effects of heat waves through modeling heat wave days as a categorical variable (Anderson and Bell 2009, 2011; Gasparrini and Armstrong 2011; Hajat et al. 2006). The rationale of this method assumes that the impacts of heat should be modeled as the sum of two items: a) daily temperature has independent impact on health; and b) heat waves lead to an additional risk due to several consecutive days. However, some studies reported that heat waves had added effects on mortality (Anderson and Bell 2009; Hajat et al. 2006; Rocklov et al. 2012), while others suggested that there were no added heat wave effects (Barnett et al. 2012; Gasparrini and Armstrong 2011). Therefore, it is not conclusive for existence and size of the added heat wave effects on mortality.
Studies have shown that associations between heat waves and health vary substantially by location (Anderson and Bell 2009, 2011; Guo et al. 2012). However, there are several challenges in comparison of the heat wave impacts on health from different climate zones or cities/regions/countries. For example, various studies used different heat wave definitions regarding the temperature threshold (e.g., 95th or 97.5th percentiles of temperature), temperature metric (e.g., minimum, mean, or maximum temperatures, or apparent temperature), and duration of heat wave in days (e.g., , , or ). Use of different time periods (e.g., summer, warm season, or whole year of data) also hinders comparison and synthesis of results across studies. Some studies used time-series analyses, while others used case-crossover designs or case-only studies to assess the health effects of heat waves. Also importantly, some studies considered lag periods of heat wave effects, while others did not, which makes it difficult to compare the cumulative effects of heat waves, because, indeed, heat waves could have a significant lag effect.
Therefore, it is important and necessary to conduct research in different regions/countries using the same statistical design to assess and compare the associations between heat waves and health events. Large studies have investigated the impact of heat waves on mortality in Asia (Son et al. 2012), the United States (Anderson and Bell 2011), and Europe (Baccini et al. 2008), but to the best of our knowledge, there are no previous studies of heat waves across the globe. We have recently established a multicountry, multicommunity (MCC) collaborative network to assess impacts of weather on mortality internationally (Gasparrini et al. 2015a, 2015b; Guo et al. 2014, 2016). This setting provides a unique opportunity to examine: a) the effects of heat waves on mortality in 400 communities in 18 countries/regions; b) effect modification by heat wave characteristics (intensity and duration); c) whether heat waves had added effects on mortality; d) regional differences in the heat wave effects; e) potential factors contributing to the heterogeneity of heat wave effects on mortality; and f) comparison for heat waves defined by daily mean, minimum, and maximum temperatures.
Methods
Data Collection
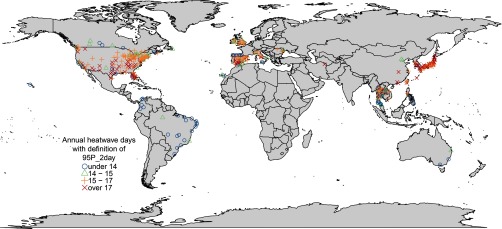
We used daily time-series data of the MCC study, which has been described in previous publications (Gasparrini et al. 2015a, 2015b; Guo et al. 2014, 2016). Briefly, we obtained daily data on all causes/nonaccidental mortality and weather conditions in 400 communities from 18 countries/regions: Australia (3 cities during 1988–2008), Brazil (18 cities during 1997–2011), Canada (26 cities during 1986–2009), China (6 cities during 2002–2007), Colombia (5 cities during 1998–2013), Iran (1 city during 2004–2013), Ireland (all Irish Island national data, including 6 regions: 2 in Northern Ireland and 4 in the Republic of Ireland during 1984–2007), Italy (10 cities during 1987–2010), Japan (47 prefectures, 1985–2012), Moldova (4 cities during 2001–2010), Philippines (4 cities during 2006–2010), South Korea (7 cities during 1992–2010), Spain (51 cities during 1990–2010), Taiwan (3 cities during 1994–2007), Thailand (62 provinces during 1999–2008), United Kingdom (10 regions during 1993–2006), United States (135 cities during 1985–2006), and Vietnam (2 cities during 2009–2013). Daily weather data included daily mean, minimum, and maximum temperatures and relative humidity in all countries/regions, except for daily minimum and maximum temperatures in Italy and Philippines and relative humidity in Italy. The locations are displayed in Figure 1. Supplemental Material provides the details for data collection, and Table S1 shows the list of locations. This study was approved by the Behavioural and Social Sciences Ethical Review Committee, University of Queensland, Australia.
Figure 1.
Locations of the study communities and annual mean heat wave days. Heat wave was defined by daily mean temperature percentile of temperature with duration .
Heat wave definition.
There is no standard heat wave definition worldwide, although they are commonly defined as a few consecutive days with high temperatures above a certain threshold that can either be physiologically based (absolute threshold) or community based (relative threshold) (Robinson 2001). In the present study, relative thresholds based on each community’s own long-term daily mean temperature were used to define heat waves, as this approach allows for regional acclimatization to temperatures normal for a community. To examine the impacts of intensity of heat waves on mortality, we used daily mean temperatures of 90th, 92.5th, 95th, and 97.5th percentiles of each community’s temperature distribution as heat wave thresholds based on year-round data. To examine the impacts of duration of heat waves on mortality, we used duration of (two or more adjacent days), 3 (three or more adjacent days), and 4 d (four or more adjacent days) to define heat waves. Therefore, we defined 12 types of heat waves for each community by combining community-specific daily mean temperature , 92.5th, 95th, and 97.5th percentiles and duration , 3, and 4 d (Table 1).
Table 1.
Heat wave definition.
| Heat wave name | Heat wave definition |
|---|---|
| 90P_2day | 90th percentile with duration |
| 90P_3day | 90th percentile with duration |
| 90P_4day | 90th percentile with duration |
| 92.5P_2day | 92.5th percentile with duration |
| 92.5P_3day | 92.5th percentile with duration |
| 92.5P_4day | 92.5th percentile with duration |
| 95P_2day | 95th percentile with duration |
| 95P_3day | 95th percentile with duration |
| 95P_4day | 95th percentile with duration |
| 97.5P_2day | 97.5th percentile with duration |
| 97.5P_3day | 97.5th percentile with duration |
| 97.5P_4day | 97.5th percentile with duration |
Data Analysis
The analyses were limited to the hot season (four hottest adjacent months) for each community. The heat wave–mortality association was examined with a two-stage hierarchal approach using data from the 400 communities in the 18 countries/regions. In the first stage, we estimated the community-specific heat wave–mortality association. These estimated associations were then pooled in the second stage at the country level using meta-analysis. This approach has been described in previous publications (Gasparrini et al. 2012; Gasparrini and Armstrong 2013).
First stage of analysis (community-specific associations).
In the first stage, we used a time-series Poisson regression model for seasonal data (i.e., hot season) to obtain community-specific estimates allowing for overdispersed death counts. Seasonality was controlled for using a natural cubic spline with 4 degrees of freedom (df; equally spaced knots) for day of the season. Long-term trend was controlled for using a natural cubic spline with 1 df per 10 y (Gasparrini et al. 2015a). A categorical variable was used to control for day of the week, as our preliminary analysis shows mortality risks varied by day of the week. To understand the characteristics of lag effects of heat waves on mortality, a natural cubic spline with 4 df was used to capture the distributed lag effect over time up to 10 d. We placed two internal knots at equally spaced log values of lag, plus intercept. The choice of 10 d for the lag period was motivated by previous studies suggesting that effects of high temperatures were acute and possibly affected by mortality displacement (Gasparrini and Armstrong 2013; Guo et al. 2011, 2014).
We assessed the 12 definitions of heat waves separately (Table 1) for each community to understand the characteristics of the heat wave impacts on mortality risks. All days with temperature above the threshold for a given heat wave definition with duration of , , and days were defined as heat wave days. For example, day 1 of a 4-d wave was considered part of the 4-d wave.
Second stage of analysis (overall country-level associations).
At the second stage, a univariate meta-analysis was used to pool the community-specific cumulative effect estimates of heat waves (lag 0–10 d) obtained from the first-stage model to obtain country-level pooled estimates separately for each type of heat wave.
A multivariate meta-analysis was used to pool the three distributed lag terms expressing the lag–response relationships specific to the heat waves compared to the non–heat wave days. This method has been described previously (Gasparrini and Armstrong 2013).
The univariate/multivariate meta-analyses were fitted using random effects models by maximum likelihood. Heterogeneity was assessed through a multivariate extension of the index, which quantifies the percentage of variability due to true differences across communities. The heat wave–mortality associations were expressed as the estimated relative risks (RR) and 95% confidence interval of mortality associated with heat wave days in comparison to non–heat wave days. For the distinction between cumulative effect and heat wave duration, if a single consecutive day that includes cumulative lag effects up to 4 d has RR of 1.2, the heat waves with 4 consecutive days will have cumulative relative risk of .
Regional difference in heat wave effects.
In order to investigate whether locations have higher effect estimates based on their long-term temperature, we divided the 400 communities into 4 groups (cold, moderate cold, moderate hot, and hot areas) by the quantiles of temperature based on the hot season mean temperature distribution of all 400 communities (each community has one value of hot season mean temperature): (), 25th–50th (), 50th–75th (), and () (see Figure S1). Meta-analyses were used to pool the community-specific effect estimates obtained from the first-stage model separately within each of these four groups for both cumulative effects (lag 0–10 d) and lag exposure–response associations.
Added effects of heat waves.
To examine whether heat waves had added effects on mortality above the effect of single days of high temperature, all other variables from the above first-stage model were maintained except for the variable to control for daily mean temperature. Here, we controlled for the temperature effects using a cross-basis function with a 6-df natural cubic spline for temperature and a 5-df natural cubic spline for lag of temperature up to 10 d (Gasparrini and Armstrong 2011). Then, the same second-stage analysis as above, univariate meta-analysis, was performed to pool the community-specific cumulative added effects of heat waves.
Assessing the potential factors contributing to the heterogeneity of heat wave effects.
Meta-regression models were used to assess the potential factors contributing to the heterogeneity of heat wave effects. We included country, community-specific hot season average temperature, hot season temperature range, hot season temperature variability [standard deviation (SD) of daily mean temperatures], latitude, and longitude as meta-predictors using single predictor models and multipredictor models. Residual heterogeneity was tested and then quantified by the Cochran Q test and statistic.
Comparison for heat waves defined by daily mean, minimum, and maximum temperatures.
We investigated whether effect estimates differed by heat wave definitions for daily mean, minimum, and maximum temperatures. We used daily minimum and maximum temperatures to define heat waves instead of mean temperature, except for Italy and Philippines, due to the unavailable data. The same two-stage analysis strategy was performed as above. In addition, we compared the community-level effect estimates from heat waves defined by daily mean, minimum, and maximum temperatures using the t-test.
Sensitivity analyses.
Sensitivity analyses were performed on the parameters for the community-specific model to test the robustness of our results. We extended the lag days of heat waves to 15 d to examine whether using a lag of 10 d was sufficient to capture the heat wave effects on mortality. We changed degrees of freedom (3–5 df) for lag days, and included relative humidity in the analyses, except for Italy, due to unavailable data. We also changed the degrees of freedom (3–7 df) for seasonality. Furthermore, we excluded the United States, Italy, Moldova, and Vietnam in sequence when we examined the regional difference in heat wave effects on mortality. We controlled for temperature variability (SD of 10-d daily mean temperatures) (Guo et al. 2016) to examine whether temperature variability influences the impacts of heat waves on mortality.
R software (version 3.2.2; R Development Core Team) was used for data analysis. The dlnm package was used to create the distributed lag model (Gasparrini et al. 2010), and the mvmeta package was used to fit the meta-analyses (Gasparrini et al. 2012).
Results
Table 2 shows the summary of the study period, mortality count, and heat waves in the 18 countries/regions. This study included 400 communities of 18 countries/regions. The study period covered 1972 to 2012, but the years of data varied by country. The total number of deaths included in the study data was over 26 million. In general, there were similar numbers of heat wave days per year across countries within each type of heat wave definition. Table S1 summarizes the heat waves in 400 communities. The numbers of deaths and annual heat wave days were different by community.
Table 2.
Summary of the study periods, number of deaths, and heat waves in the 18 countries/regions.
| Country | Period | No. of deaths | No. of communities | Mean of heat wave days per year (range) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 90P_2day | 90P_3day | 90P_4day | 92.5P_2day | 92.5P_3day | 92.5P_4day | 95P_2day | 95P_3day | 95P_4day | 97.5P_2day | 97.5P_3day | 97.5P_4day | ||||
| Australia | 1988–2009 | 361,984 | 3 | 26 (23, 29) | 19 (15, 23) | 14 (9, 19) | 18 (16, 21) | 12 (9, 16) | 9 (6, 13) | 11 (10, 14) | 7 (5, 10) | 4 (2, 8) | 5 (4, 6) | 2 (2, 3) | 1 (1, 2) |
| Brazil | 1997–2011 | 1,101,149 | 18 | 23 (17, 28) | 18 (12, 24) | 15 (8, 22) | 17 (11, 21) | 13 (7, 19) | 10 (5, 15) | 11 (6, 14) | 8 (4, 11) | 6 (2, 10) | 5 (1, 7) | 3 (1, 5) | 2 (0, 4) |
| Canada | 1986–2011 | 944,105 | 26 | 30 (28, 33) | 26 (23, 29) | 22 (19, 25) | 22 (21, 24) | 18 (16, 19) | 14 (12, 16) | 14 (13, 15) | 11 (8, 12) | 8 (6, 10) | 7 (6, 7) | 4 (3, 6) | 3 (2, 4) |
| China | 2002–2009 | 172,703 | 6 | 37 (32, 54) | 32 (26, 49) | 27 (21, 44) | 30 (24, 54) | 26 (19, 49) | 21 (11, 44) | 16 (14, 21) | 13 (8, 15) | 10 (6, 12) | 10 (6, 21) | 7 (4, 15) | 5 (2, 12) |
| Colombia | 1998–2013 | 267,736 | 5 | 15 (11, 19) | 10 (8, 12) | 7 (5, 8) | 10 (7, 15) | 7 (5, 9) | 4 (2, 5) | 6 (5, 10) | 4 (3, 6) | 2 (1, 2) | 3 (2, 5) | 1 (1, 2) | 1 (0, 1) |
| Iran | 2004–2013 | 40,824 | 1 | 34 (34, 34) | 31 (31, 31) | 27 (27, 27) | 25 (25, 25) | 22 (22, 22) | 16 (16, 16) | 18 (18, 18) | 15 (15, 15) | 12 (12, 12) | 8 (8, 8) | 6 (6, 6) | 4 (4, 4) |
| Ireland | 1984–2007 | 316,652 | 6 | 31 (30, 31) | 26 (24, 28) | 22 (21, 24) | 23 (22, 23) | 18 (17, 19) | 16 (14, 17) | 15 (14, 15) | 11 (10, 12) | 8 (7, 10) | 7 (6, 8) | 5 (4, 6) | 4 (3, 5) |
| Italy | 1987–2010 | 248,808 | 10 | 33 (30, 35) | 30 (25, 34) | 28 (23, 31) | 24 (21, 26) | 21 (17, 24) | 19 (15, 23) | 15 (13, 17) | 13 (11, 16) | 11 (8, 14) | 7 (6, 8) | 6 (4, 7) | 4 (2, 6) |
| Japan | 1972–2012 | 10,075,406 | 47 | 35 (33, 36) | 32 (29, 34) | 29 (25, 32) | 26 (24, 29) | 23 (21, 26) | 21 (18, 24) | 17 (16, 18) | 14 (13, 16) | 12 (10, 15) | 8 (7, 10) | 6 (5, 8) | 5 (3, 7) |
| Moldova | 2001–2010 | 18,828 | 4 | 34 (33, 34) | 29 (29, 30) | 26 (25, 26) | 24 (24, 25) | 20 (18, 22) | 17 (16, 20) | 16 (14, 16) | 13 (12, 14) | 11 (10, 12) | 8 (8, 8) | 7 (7, 8) | 6 (5, 6) |
| Philippines | 2006–2010 | 90,917 | 4 | 24 (16, 28) | 20 (12, 24) | 18 (9, 23) | 20 (15, 23) | 16 (11, 20) | 13 (7, 18) | 12 (7, 15) | 10 (5, 12) | 8 (4, 11) | 6 (4, 7) | 5 (2, 6) | 4 (2, 6) |
| South Korea | 1992–2010 | 472,421 | 7 | 33 (25, 35) | 30 (23, 33) | 28 (21, 31) | 25 (19, 26) | 22 (17, 24) | 21 (16, 23) | 16 (12, 17) | 14 (10, 16) | 13 (9, 14) | 8 (6, 8) | 6 (4, 7) | 5 (3, 6) |
| Spain | 1990–2010 | 1,054,098 | 51 | 32 (11, 36) | 29 (9, 33) | 24 (7, 30) | 24 (8, 27) | 20 (6, 24) | 16 (4, 22) | 15 (5, 18) | 12 (3, 16) | 9 (3, 14) | 7 (2, 8) | 5 (1, 7) | 3 (0, 5) |
| Taiwan | 1994–2007 | 218,302 | 3 | 35 (34, 36) | 30 (29, 32) | 28 (26, 30) | 25 (24, 26) | 21 (20, 22) | 18 (16, 19) | 17 (16, 18) | 14 (12, 15) | 12 (10, 13) | 8 (7, 10) | 7 (6, 9) | 5 (4, 7) |
| Thailand | 1999–2008 | 619,432 | 62 | 26 (6, 35) | 23 (4, 33) | 20 (3, 32) | 20 (4, 28) | 17 (3, 25) | 15 (2, 23) | 13 (3, 18) | 11 (2, 15) | 9 (2, 14) | 6 (2, 9) | 5 (1, 8) | 4 (0, 6) |
| United Kingdom | 1990–2012 | 3,513,043 | 10 | 30 (29, 31) | 26 (25, 27) | 23 (21, 24) | 22 (22, 23) | 19 (18, 20) | 16 (16, 17) | 15 (14, 15) | 12 (11, 13) | 10 (9, 11) | 7 (7, 8) | 6 (5, 6) | 4 (3, 5) |
| United States | 1985–2006 | 7,106,601 | 135 | 33 (18, 40) | 28 (15, 36) | 24 (10, 34) | 24 (14, 32) | 20 (10, 28) | 16 (6, 25) | 16 (8, 23) | 12 (5, 18) | 10 (3, 16) | 8 (3, 10) | 5 (2, 8) | 4 (1, 7) |
| Vietnam | 2009–2013 | 35,655 | 2 | 32 (31, 33) | 26 (25, 28) | 22 (21, 24) | 22 (22, 22) | 18 (17, 18) | 14 (14, 15) | 16 (15, 16) | 12 (11, 12) | 10 (8, 11) | 8 (8, 8) | 6 (4, 7) | 4 (3, 6) |
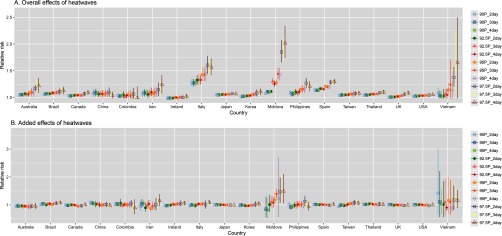
Figure 2A shows the pooled cumulative (lag 0–10 d) estimated RRs for the impacts of heat waves on mortality in 18 countries/regions for the 12 definitions of heat waves. There were significant associations of heat waves on mortality in all countries/regions for all types of heat waves. In general, higher temperature thresholds had higher effect estimates, except for China. For heat waves using the same threshold, longer heat waves (based on longer duration of days; ) did not have higher heat wave effect estimates on mortality than heat wave definitions with shorter duration of days () in each country/region.
Figure 2.
Cumulative effects of heat waves on mortality (A. overall effects of heat waves and B. added effects of heat waves after controlling for effects of daily mean temperature) over lag 0–10 d in 18 countries/regions for 12 types of heat wave definitions. Please refer Table 1 for heat wave definitions.
In general, Italy, Moldova, and Vietnam had higher effect estimates than other countries/regions. The effect estimates varied greatly by community, with RRs from 0.84 in Phetchabun, Thailand to 2.19 in Falesti, Moldova for the heat wave definition of percentile and duration. However, there were no added effects of heat waves on mortality in all countries/regions when controlling for the effects of daily mean temperature, except for Brazil, Moldova, and Taiwan using the percentile for the heat wave definition (Figure 2B).
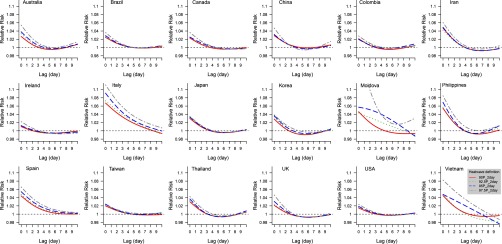
The estimated effects of heat waves on mortality appeared immediately and generally lasted 3 or 4 d in all countries/regions (Figure 3 and Figures S2 and S3), except in Italy and Spain, where the risks persisted longer. There was a period of RR below 1.0 at longer lags, consistent with mortality displacement (harvesting effect) after exposure to heat waves in Canada, Iran, Ireland, Japan, South Korea, Philippines, Thailand, United Kingdom, and, to a lesser extent, in Colombia and the United States.
Figure 3.
Lag effects of heat waves on mortality along lag 0–10 d in 18 countries/regions for 4 types of heat wave definitions. Please refer to Table 1 for heat wave definitions.
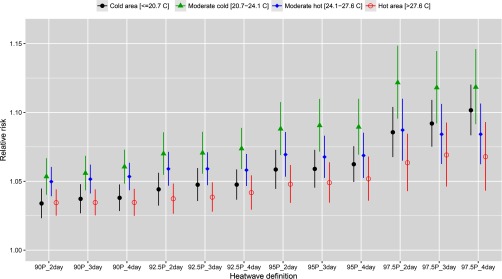
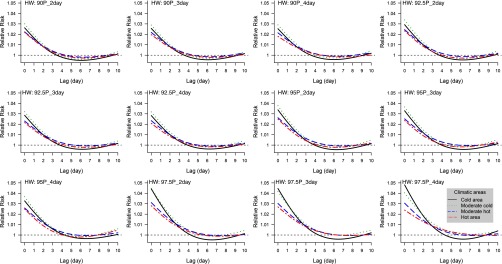
Figure 4 shows the pooled cumulative (lag 0–10 d) associations between heat waves and mortality in cold, moderate cold, moderate hot, and hot areas. In general, heat waves had higher effects on mortality in moderate cold and hot areas than cold and moderate hot areas for all types of heat wave definitions. However, heat waves had similar effects on mortality in cold and hot areas, except under the percentile of temperature definition, for which the effect estimates were higher in cold areas than in hot areas.
Figure 4.
Cumulative effects of heat waves on mortality over lag 0–10 d in 4 climatic areas (cold, moderate cold, moderate hot, and hot areas) for 12 types of heat wave definitions. Cold areas: mean temperature of hot season: ; moderate cold areas: mean temperature of hot season: ; moderate hot areas: mean temperature of hot season: ; and hot areas: mean temperature of hot season: . Please refer to Table 1 for heat wave definitions.
There was suggestive evidence in mortality displacement (harvesting effect) after exposure to heat waves in cold areas for all types of heat waves (Figure 5). Also, the heat wave effects on mortality generally lasted longer for those using the percentile of temperature as the threshold in moderate cold, moderate hot, and hot areas.
Figure 5.
Lag effects of heat waves on mortality along lag 0–10 d in 4 climatic areas (cold, moderate cold, moderate hot, and hot areas) for 12 types of heat wave definitions. Cold areas: mean temperature of hot season: ; moderate cold areas: mean temperature of hot season: ; moderate hot areas: mean temperature of hot season: ; and hot areas: mean temperature of hot season: . Please refer to Table 1 for heat wave definitions.
Table 3 and Table S2 show results from the analysis of heterogeneity for overall heat wave effects and added heat wave effects, with a comparison of statistics from the random effect meta-analyses (no meta-predictor) and random effect meta-regressions with a single meta-predictor or all meta-predictors. For overall heat wave effects, a substantial amount of (residual) heterogeneity could be explained by between-country differences, as indicated by the larger decrease in the statistics when indicators for country were included as a meta-predictor. The other meta-predictors [community-specific hot season average temperature, hot season temperature range, hot season temperature variability (SD of daily mean temperatures), latitude, and longitude] could only explain a limited part of the residual heterogeneity. For added heat wave effects, there was little residual heterogeneity in all the models, as tested by the Cochran Q test.
Table 3.
Second-stage random effects meta-analysis and meta-regression models for explaining variation in overall heat wave effects and added heat wave effects: Cochran Q test for heterogeneity, statistics for residual heterogeneity.
| Heat wave definition | Model | Predictor | Overall heat wave effect | Added heat wave effect | ||
|---|---|---|---|---|---|---|
| for Q test | (%) | for Q test | (%) | |||
| 90P_2day | Intercept only | No predictor | 73.33 | 0.372 | 2.12 | |
| Single predictor | Average temperature | 70.83 | 0.376 | 2.04 | ||
| Temperature range | 73.40 | 0.399 | 1.63 | |||
| Temperature variability | 73.03 | 0.412 | 1.39 | |||
| Longitude | 72.26 | 0.359 | 2.35 | |||
| Latitude | 72.16 | 0.361 | 2.31 | |||
| Country | 44.72 | 0.335 | 2.86 | |||
| Full | Average temperature | |||||
| Temperature range | ||||||
| Temperature variability | 43.99 | 0.402 | 1.61 | |||
| Longitude | ||||||
| Latitude | ||||||
| Country | ||||||
| 92.5P_2day | Intercept only | No predictor | 74.37 | 0.031 | 12.03 | |
| Single predictor | Average temperature | 72.84 | 0.038 | 11.42 | ||
| Temperature range | 74.34 | 0.030 | 12.11 | |||
| Temperature variability | 73.52 | 0.028 | 12.25 | |||
| Longitude | 73.72 | 0.028 | 12.25 | |||
| Latitude | 73.61 | 0.028 | 12.24 | |||
| Country | 46.52 | 0.024 | 12.87 | |||
| Full | Average temperature | |||||
| Temperature range | ||||||
| Temperature variability | 43.83 | 0.030 | 12.39 | |||
| Longitude | ||||||
| Latitude | ||||||
| Country | ||||||
| 95P_2day | Intercept only | No predictor | 74.99 | 0.095 | 8.59 | |
| Single predictor | Average temperature | 74.51 | 0.108 | 8.13 | ||
| Temperature range | 74.91 | 0.149 | 6.88 | |||
| Temperature variability | 74.20 | 0.116 | 7.88 | |||
| Longitude | 74.65 | 0.100 | 8.40 | |||
| Latitude | 74.61 | 0.090 | 8.78 | |||
| Country | 49.54 | 0.082 | 9.28 | |||
| Full | Average temperature | |||||
| Temperature range | ||||||
| Temperature variability | 46.66 | 0.097 | 8.72 | |||
| Longitude | ||||||
| Latitude | ||||||
| Country | ||||||
| 97.5P_2day | Intercept only | No predictor | 73.99 | 0.038 | 11.47 | |
| Single predictor | Average temperature | 74.02 | 0.038 | 11.47 | ||
| Temperature range | 73.73 | 0.074 | 9.45 | |||
| Temperature variability | 73.43 | 0.057 | 10.30 | |||
| Longitude | 74.03 | 0.043 | 11.11 | |||
| Latitude | 73.92 | 0.053 | 10.48 | |||
| Country | 51.82 | 0.089 | 9.00 | |||
| Full | Average temperature | |||||
| Temperature range | ||||||
| Temperature variability | 47.79 | 0.080 | 9.42 | |||
| Longitude | ||||||
| Latitude | ||||||
| Country | ||||||
Note: Please refer to Table 1 for heat wave definitions.
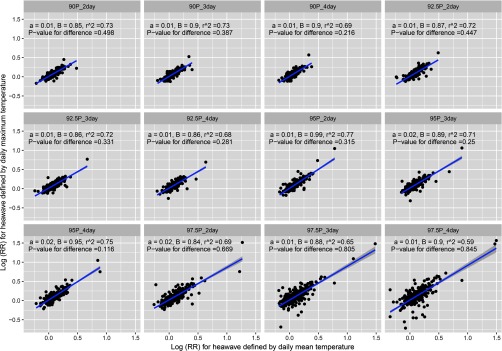
Generally, heat waves defined by daily mean temperature gave similar effect estimates [log (RR)] as heat waves defined by daily maximum temperature (Figure 6), while there was statistical difference in effect estimates modeled by heat waves defined by daily mean and minimum temperatures (Figure S4). Heat waves defined by daily mean temperature typically produced higher community-level effect estimates than those defined by daily maximum and minimum temperatures. However, the country-level results were similar when we used daily mean, minimum, and maximum temperatures to define heat waves (Figure 2 and Figure S5).
Figure 6.
Comparison for cumulative effects of heat waves on mortality over lag 0–10 d in 16 countries/regions for 12 types of heat wave definitions using daily mean and maximum temperatures. Please refer to Table 1 for heat wave definitions. a, B, and are intercept, coefficient, and r-squared, respectively, derived from linear regression model for effect estimates modeled by heat waves defined by daily mean and maximum temperatures. for difference is modeled by the t-test between effect estimates modelled by heat waves defined by daily mean and maximum temperatures.
Our results were robust to a changed lag structure of 15 d, modified degrees of freedom for lag (3–5 df), changed degrees of freedom for day of season (3–7 df), and inclusion of a variable for relative humidity in the model (results not shown). The regional difference in the estimated heat wave effects on mortality did not change substantially when we excluded the United States (Figures S6 and S7), Italy (Figures S8 and S9), Moldova (Figures S10 and S11), and Vietnam (Figures S12 and S13). The estimated effects of heat waves on mortality did not change after controlling for temperature variability (Figure S14).
Discussion
This study examined heat wave–mortality associations using consistent methods for 400 communities across 18 countries/regions, including countries from both developing and developed regions with different climates (i.e., tropical, subtropical, and temperate). We developed 12 definitions of heat waves by combining four temperature thresholds (90th, 92.5th, 95th, and 97.5th percentile of temperature, indicating intensity of heat waves) and three definitions of duration (, 3, and 4 d) to determine how heat wave effects changed when heat waves were more intense and longer. Although many studies have suggested that heat wave characteristics modify mortality risks, to the best of our knowledge, this is the largest and first multicountry study of heat waves to examine effect modification by heat wave duration and intensity. We found that in all countries/regions, heat waves were associated with increased risk of death for all types of heat wave definitions. The estimated effects of heat wave on mortality were higher when using higher temperature thresholds (e.g., 97.5th vs. 95th percentile of temperature). In general, the effects of heat waves varied by country; for example, Italy had highest heat wave effects. The effects of heat waves appeared acutely and lasted for 3 and 4 d for most countries. Heat waves effect estimates were higher in moderate cold and moderate hot areas than in cold and hot areas. However, heat waves did not have added effects on mortality when controlling for the effects of daily mean temperature in all countries/regions, except for Brazil, Moldova, and Taiwan, using the percentile of temperature as the heat wave definition. Heat waves defined by daily mean and maximum temperatures produced similar effect estimates, which are higher than those defined by daily minimum temperature.
Several plausible physiological mechanisms have been proposed for the effects of heat waves on mortality (Fuller et al. 2010). When ambient temperature is extremely high, the human body responds through thermoregulation; blood vessels dilate near the skin to transfer heat from the body’s core to the skin, and then sweat transfers heat from the skin by evaporation (Havenith 2005). Thermoregulation can strain the cardiovascular system, even when body temperature remains normal (Havenith 2005). In general, the higher the intensity (temperature) or the longer the duration of the heat wave, the more work required of the cardiovascular system to maintain normal temperature. Therefore, more intense or longer heat waves are thought to have greater health impacts (Li et al. 2016; Madaniyazi et al. 2016).
Our findings that heat waves had significant impacts on mortality have been strongly indicated by the ensemble of previous studies (Anderson and Bell 2011; Baccini et al. 2008; Fouillet et al. 2006; Le Tertre et al. 2006; Sun et al. 2014; Tong et al. 2012). However, we used consistent statistical methods across a wide range of communities to address whether different methods lead to difficult comparisons. In addition, previous studies have used a variety of heat wave definitions, lags, and methods to control for time-varying confounders, each of which can change the estimates of heat wave–mortality relationships.
There were substantial variations in the estimated RRs of mortality associated with heat waves between and within countries/regions. We found that Italy, Moldova, and Vietnam had higher heat wave–related mortality risks than other countries. This finding is not supportive with our prior hypothesis that persons in developing countries (Vietnam, Brazil, Moldova, Thailand, and China) would be more sensitive to heat waves than those in wealthy countries, but it would be premature to consider this as strong evidence against that hypothesis. The low rate of air-conditioning use in Italy and Moldova and the low-level socioeconomic development in Moldova and Vietnam might be the reason that these countries had higher heat wave effects on mortality than other countries. In addition, the variation in the impact of heat waves on mortality might be modified by: a) demographic characteristics (e.g., population in high-risk categories, such as the elderly or less healthy) (Schifano et al. 2009); b) community-level adaptation levels to heat waves (e.g., heat wave warning systems) (Ebi et al. 2004); or c) personal adaptation strategies (e.g., air-conditioner use, housing structure, clothing type) (Barnett et al. 2013; Farbotko and Waitt 2011).
Interestingly, our results suggested that the heat wave effects on mortality were higher in moderate cold and moderate hot areas than cold and hot areas. These findings are somewhat different from previous studies, such as U.S. studies that reported higher effects in cold areas (Anderson and Bell 2009; Braga et al. 2001), while European studies found a reversed pattern (Baccini et al. 2008). The difference might result from the large number of communities involved in this study, which enhances our ability to divide areas into detailed climatic areas. Thus, what might have been cold areas in previous studies were only moderate cold areas in this study. However, if we only compare results based on heat waves defined by the 97.5th percentile as the temperature threshold, the estimated heat wave effects on mortality were higher in cold areas than hot areas. Another possible reason for our results might be that in moderate cold and moderate hot areas, absolute temperature is important, but for the hot and cold areas, adaptation becomes important and is dominant in the hottest climate area. Furthermore, heat wave–related impacts within a given type of climate may vary, due to differences in indoor/outdoor activity and housing structures, such as the higher prevalence of air-conditioning in the United States compared to Europe. This study indicates that more attention should be paid to heat waves in moderate cold and moderate hot areas across the world, given the potential for substantial impact to public health.
This study provided evidence on the importance of heat wave intensity (temperature thresholds), but not duration in relation to the health impacts of heat waves. This differs from some earlier studies that suggest that both heat wave intensity and duration modified heat wave impacts on health (Anderson and Bell 2011). Several studies have found that longer heat waves had greater mortality effects (Díaz et al. 2002; Kalkstein and Smoyer 1993; Smoyer 1998). Other work found increases in mortality risks associated with heat wave definitions that were longer (i.e., higher duration) or more intense (i.e., higher temperature) (Gasparrini and Armstrong 2011; Hajat et al. 2006). One potential reason for the differences between our findings and previous studies might be that unlike earlier work, we considered lag effects. Our results showed that there were significant lag effects of heat waves on mortality in all countries/regions, and the estimated effects lasted for 3 and 4 d (even longer in Italy and Spain). These findings suggest that if the lag effects were not considered, the longer-duration heat waves could capture the lag effect (e.g., for a 6-d duration heat wave, the effects of the fourth to sixth days of the heat wave might include the lag effects of first to third days of the heat wave and the effects of days 4 to 6), but the shorter-duration heat waves would not capture the lag effect (e.g., for a 2-d duration heat wave, the lag effect of these 2 d would not be captured). Thus, modeling the cumulative effects of heat waves on mortality including the lags is very important to fully understand the impact of heat wave duration. Another possible reason for differences with some other studies is that those studies allocated each day of a heat wave to the category of duration up to that day only (Anderson and Bell 2009, 2011; Gasparrini and Armstrong 2011; Hajat et al. 2006).
Understanding the lag pattern of heat wave effects on mortality is helpful in preventing heat wave–related health events, particularly for estimating mortality displacement during and after heat waves (Armstrong et al. 2014; Saha et al. 2014). Our results suggest that the effects of heat waves appeared immediately and lasted for 3–4 d in all countries (Figure 3) and all climate areas (Figure 5), except for Italy and Spain, with 7-d lag effects. This finding is consistent with previous studies for effects of heat waves and high temperatures on mortality (Gasparrini et al. 2015a; Guo et al. 2014; Tong et al. 2012). This means prompt preventive actions are necessary for reducing heat wave effects on health events. Interestingly, we found there was mortality displacement after heat waves in some countries, particularly in cold climate areas (Figure 5). The reason might be that people living in cold climate areas have not adapted to the extreme high temperatures (Curriero et al. 2002). Thus, when heat waves appeared, some excess deaths occurred during and shortly after the heat wave, resulting in fewer deaths in the coming days or weeks. Generally, the mortality displacement mainly occurs in chronically ill individuals, for example, the elderly and people with cardiovascular and respiratory diseases (Qiao et al. 2015).
An interesting finding is that heat waves did not have added effects on mortality when we decomposed the effects of heat waves into effects of temperature and added effects of heat waves in all countries/regions, except for Brazil, Moldova, and Taiwan, using the percentile of temperature for the heat wave definition. This finding suggests that heat wave effects can be adequately captured by the effects of temperature modeled by distributed lag nonlinear models in most countries, except for Brazil, Moldova, and Taiwan. This is consistent with some previous studies conducted in the United States (Barnett et al. 2012; Gasparrini and Armstrong 2011). However, it is still debatable as to whether to estimate heat wave effects as a part of the effects of temperature; some studies find heat waves to have added effects. Based on the findings of this study, the provision of developing heat wave warning systems might be flawed. Instead, concerted efforts to develop high-temperature warning systems might be more warranted to reduce health risks.
Our results demonstrate that using daily mean and maximum temperatures for heat wave definition was better at predicting mortality than daily minimum temperature. Generally, heat waves defined by daily mean temperature produced higher RRs than those using daily maximum and minimum temperatures. This is consistent with a previous study in Europe (Hajat et al. 2006), while a U.S. study suggested that no one temperature measure was superior to others for predicting mortality (Barnett et al. 2010). The potential reason might be that the daily mean temperature, which is the average of the entire day, may better reflect the complete exposure. However, daily maximum temperature often occurs during the afternoon hours when outdoor activity is more likely than overnight; it may be a better surrogate for high/dangerous exposures than daily mean or minimum temperature. Daily minimum temperature usually happens in the night when most people stay at home. Thus, daily minimum temperature might lead to measure error if people live in an area with good home insulation and high rates of air-conditioning use.
This study has some limitations. Similar to other studies using time-series data, we used the data on temperature from fixed sites to define heat waves, rather than individual exposure, which could introduce exposure error to some extent. However, these exposure errors are likely to be random, which would usually result in an underestimation of the estimated relative risks (Lee et al. 2016). Air pollutants were not adjusted for in this study because the data were not available for some countries. However, previous research showed that temperature effects on mortality in the United States were robust to air pollution (Anderson and Bell 2009). Also, air pollutants might be on the causal path between temperature and health, which can also complicate interpretation of adjusted models (Buckley et al. 2014). Extensive data are needed to investigate in detail the reasons for the variation in heat wave–mortality associations across communities, countries, and regions, such as with respect to different population characteristics and adaptation. In addition, our data set did not include age- or cause-specific mortality, so we investigated all causes/nonaccidental mortality. Relative humidity was not used in our main analyses, but main results were shown to be insensitive to its inclusion in sensitivity analyses. The use of relative humidity might be problematic because of its dependence on temperature (Davis et al. 2016). However, we could not choose a humidity variable with greater physiological relevance because of data availability. Also due to data availability, the time period of data was varied by country, which might have impacted the results, as the impacts of temperature on mortality may have changed over recent years (Gasparrini et al. 2015a). It is important to understand whether socioeconomic status contributes to the heterogeneity of heat wave effects on mortality, but it is beyond the scope of our analysis, and gathering such data would be a substantial undertaking. Future studies are needed to address the above limitations.
Conclusions
Understanding the characteristics of heat wave effects on mortality is important to better protect public health, particularly because heat waves will be more frequent, longer, and more intense in the future (Meehl and Tebaldi 2004). To the best of our knowledge, this study is unique among heat wave studies in its international scale, multiple heat wave definitions, and consideration of how heat wave intensity and duration may modify heat wave effects. Our findings suggest that mortality risk increased during heat waves in comparison to the communities’ usual climates, and the effects lasted for 3 to 4 d. The heat wave effects on mortality were affected by the intensity, but not duration. People living in moderate cold and moderate hot areas might be more vulnerable to heat waves than those living in cold and hot areas. There were no added heat wave effects compared to the impact of high temperature on mortality in most countries. Daily mean and maximum temperatures had similar abilities to define heat waves, but not daily minimum temperature. In addition, the observed variation in heat wave effects on mortality between communities/countries/regions indicates the importance of developing local heat wave response plans.
Supplemental Material
Acknowledgments
We thank relevant institutes/agencies who provided data on mortality and weather conditions.
Y.G. was supported by the Career Development Fellowship of Australian National Health and Medical Research Council (#APP1107107). This work was supported by the Australian Research Council (Australia) (Grant ID: DP110100651); the Medical Research Council, UK (Grant ID: MR/M022625/1); the Ministry of Education, Spain (Grant ID: PRX12/00515); the Environment Research and Technology Development Fund (S-10 and S14) of the Ministry of the Environment, Japan; and the National Research Foundation of Korea (Grant ID: K21004000001-10A0500-00710).
References
- Anderson BG, Bell ML. 2009. Weather-related mortality: How heat, cold, and heat waves affect mortality in the United States. Epidemiology 20(2):205–213, PMID: 19194300, 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Bell ML. 2011. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect 119(2):210–218, PMID: 21084239, 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong B, Gasparrini A, Hajat S. 2014. Estimating mortality displacement during and after heat waves. Am J Epidemiol 179(12):1405–1406, PMID: 24812157, 10.1093/aje/kwu083. [DOI] [PubMed] [Google Scholar]
- Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, Analitis A, et al. 2008. Heat effects on mortality in 15 European cities. Epidemiology 19(5):711–719, PMID: 18520615, 10.1097/EDE.0b013e318176bfcd. [DOI] [PubMed] [Google Scholar]
- Barnett G, Beaty M, Chen D, McFallan S, Meyers J, Nguyen M, et al. 2013. Pathways to Climate Adapted and Healthy Low Income Housing. Gold Coast: National Climate Change Adaptation Research Facility. [Google Scholar]
- Barnett A, Hajat S, Gasparrini A, Rocklöv J. 2012. Cold and heat waves in the United States. Environ Res 112:218–224, PMID: 22226140, 10.1016/j.envres.2011.12.010. [DOI] [PubMed] [Google Scholar]
- Barnett AG, Tong S, Clements ACA. 2010. What measure of temperature is the best predictor of mortality? Environ Res 110(6):604–611, PMID: 20519131, 10.1016/j.envres.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Braga AL, Zanobetti A, Schwartz J. 2001. The time course of weather-related deaths. Epidemiology 12(6):662–667, PMID: 11679794. [DOI] [PubMed] [Google Scholar]
- Buckley JP, Samet JM, Richardson DB. 2014. Does air pollution confound studies of temperature? Epidemiology 25(2):242–245, PMID: 24487206, 10.1097/EDE.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. 2002. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 155(1):80–87, PMID: 11772788. [DOI] [PubMed] [Google Scholar]
- Davis RE, McGregor GR, Enfield KB. 2016. Humidity: A review and primer on atmospheric moisture and human health. Environ Res 144(Pt A):106–116, PMID: 26599589, 10.1016/j.envres.2015.10.014. [DOI] [PubMed] [Google Scholar]
- Díaz J, Jordán A, García R, López C, Alberdi JC, Hernández E, et al. 2002. Heat waves in Madrid 1986–1997: Effects on the health of the elderly. Int Arch Occup Environ Health 75(3):163–170, PMID: 11954983, 10.1007/s00420-001-0290-4. [DOI] [PubMed] [Google Scholar]
- Ebi KL, Teisberg TJ, Kalkstein LS, Robinson L, Weiher RF. 2004. Heat watch/warning systems save lives: Estimated costs and benefits for Philadelphia 1995-98. Bull Amer Meteor Soc 85:1067–1073, 10.1175/BAMS-85-8-1067. [DOI] [Google Scholar]
- Farbotko C, Waitt G. 2011. Residential air-conditioning and climate change: voices of the vulnerable. Health Promot J Austr S13–S16. [PubMed] [Google Scholar]
- Field CB, Barros VR, Mach K, Mastrandrea M. 2014. “Climate Change 2014: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change.” http://www.ipcc.ch/report/ar5/wg2/.
- Fouillet A, Rey G, Laurent F, Pavillon G, Bellec S, Guihenneuc-Jouyaux C, et al. 2006. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health 80(1):16–24, PMID: 16523319, 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller A, Dawson T, Helmuth B, Hetem RS, Mitchell D, Maloney SK. 2010. Physiological mechanisms in coping with climate change. Physiol Biochem Zool 83(5):713–720, PMID: 20578846, 10.1086/652242. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B. 2011. The impact of heat waves on mortality. Epidemiology 22(1):68–73, PMID: 21150355, 10.1097/EDE.0b013e3181fdcd99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B. 2013. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med Res Methodol 13:1–10, PMID: 23297754, 10.1186/1471-2288-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward M. 2010. Distributed lag non‐linear models. Stat Med 29(21):2224–2234, PMID: 20812303, 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2012. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med 31(29):3821–3839, PMID: 22807043, 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, et al. 2015a. Temporal variation in heat–mortality associations: a multicountry study. Environ Health Perspect 123(11):1200–1207, 10.1289/ehp.1409070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. 2015b. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386(1991):369–375, 10.1016/S0140-6736(1014)62114-62110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, et al. 2014. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 25(6):781–789, PMID: 25166878, 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, et al. 2016. Temperature variability and mortality: a multi-country study. Environ Health Perspect 124(10):1554–1559, PMID: 27258598, 10.1289/EHP149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Barnett AG, Pan X, Yu W, Tong S. 2011. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect 119(12):1719–1725, PMID: 21827978, 10.1289/ehp.1103598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Barnett AG, Tong S. 2012. High temperatures-related elderly mortality varied greatly from year to year: important information for heat-warning systems. Sci Rep 2:830, 10.1038/srep00830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S, Armstrong B, Baccini M, Biggeri A, Bisanti L, Russo A, et al. 2006. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology 17(6):632–638, PMID: 17003686, 10.1097/01.ede.0000239688.70829.63. [DOI] [PubMed] [Google Scholar]
- Havenith G. 2005. Temperature regulation, heat balance and climatic stress. In: Extreme Weather Events and Public Health Responses. New York, NY:Springer, 69–80. [Google Scholar]
- Kalkstein LS, Smoyer KE. 1993. The impact of climate change on human health: Some international implications. Experientia 49(11):969–979, PMID: 8253171. [DOI] [PubMed] [Google Scholar]
- Kent ST, McClure LA, Zaitchik BF, Smith TT, Gohlke JM. 2014. Heat waves and health outcomes in Alabama (USA): the importance of heat wave definition. Environ Health Perspect 122(2):151–158, PMID: 24273236, 10.1289/ehp.1307262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Tertre A, Lefranc A, Eilstein D, Declercq C, Medina S, Blanchard M, et al. 2006. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology 17(1):75–79, PMID: 16357598. [DOI] [PubMed] [Google Scholar]
- Lee M, Shi L, Zanobetti A, Schwartz JD. 2016. Study on the association between ambient temperature and mortality using spatially resolved exposure data. Environ Res 151:610–617, PMID: 27611992, 10.1016/j.envres.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, Gu S, Bi P, Yang J, Liu Q. 2015. Heat waves and morbidity: Current knowledge and further direction-a comprehensive literature review. Int J Environ Res Public Health 12(5):5256–5283, PMID: 25993103, 10.3390/ijerph120505256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Zhou Y, Williams G, Jaakkola JJ, Ou C, Chen S, et al. 2016. Seasonality and temperature effects on fasting plasma glucose: a population-based longitudinal study in China. Diabetes Metab 42(4):267–275, PMID: 26851820, 10.1016/j.diabet.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Madaniyazi L, Zhou Y, Li S, Williams G, Jaakkola JJK, Liang X, et al. 2016. Outdoor temperature, heart rate and blood pressure in Chinese adults: effect modification by individual characteristics. Sci Rep 6:21003, PMID: 26876040, 10.1038/srep21003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehl GA, Tebaldi C. 2004. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 305(5686):994–997, PMID: 15310900, 10.1126/science.1098704. [DOI] [PubMed] [Google Scholar]
- Qiao Z, Guo Y, Yu W, Tong S. 2015. Assessment of short- and long-term mortality displacement in heat-related deaths in Brisbane, Australia, 1996-2004. Environ Health Perspect 123(8):766–772, PMID: 25794410, 10.1289/ehp.1307606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson PJ. 2001. On the definition of a heat wave. J Appl Meteor 40(4):762–775, . [DOI] [Google Scholar]
- Rocklov J, Barnett AG, Woodward A. 2012. On the estimation of heat-intensity and heat-duration effects in time series models of temperature-related mortality in Stockholm, Sweden. Environ Health 11(1):23, 10.1186/1476-069X-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha MV, Davis RE, Hondula DM. 2014. Mortality displacement as a function of heat event strength in 7 US cities. Am J Epidemiol 179(4):467–474, PMID: 24264293, 10.1093/aje/kwt264. [DOI] [PubMed] [Google Scholar]
- Schifano P, Cappai G, De Sario M, Michelozzi P, Marino C, Bargagli AM, et al. 2009. Susceptibility to heat wave-related mortality: a follow-up study of a cohort of elderly in Rome. Environ Health 8(1):50, 10.1186/1476-069X-8-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL, et al. 1996. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med 335(2):84–90, PMID: 8649494, 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Smoyer KE. 1998. A comparative analysis of heat waves and associated mortality in St. Louis, Missouri–1980 and 1995. Int J Biometeorol 42(1):44–50, PMID: 9780845, 10.1007/s004840050082. [DOI] [PubMed] [Google Scholar]
- Son JY, Lee JT, Anderson G, Bell ML. 2012. The impact of heat waves on mortality in seven major cities in Korea. Environ Health Perspect 120(4):566–571, PMID: 22266672, 10.1289/ehp.1103759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Sun Q, Yang M, Zhou X, Li X, Yu A, et al. 2014. Effects of temperature and heat waves on emergency department visits and emergency ambulance dispatches in Pudong New Area, China: A time series analysis. Environ Health 13:77, PMID: 25273545, 10.1186/1476-069X-13-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S, Wang XY, Guo Y. 2012. Assessing the short-term effects of heatwaves on mortality and morbidity in Brisbane, Australia: comparison of case-crossover and time series analyses. PloS One 7(5):e37500, PMID: 22655052, 10.1371/journal.pone.0037500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang XY, Guo Y, FitzGerald G, Aitken P, Tippett V, Chen D, et al. 2015. The impacts of heatwaves on mortality differ with different study periods: a multi-city time series investigation. PloS One 10(7):e0134233, PMID: 26217945, 10.1371/journal.pone.0134233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.