Abstract
Background:
Environmental heat exposure is a public health concern. The impacts of environmental heat on mortality and morbidity at the population scale are well documented, but little is known about specific exposures that individuals experience.
Objectives:
The first objective of this work was to catalyze discussion of the role of personal heat exposure information in research and risk assessment. The second objective was to provide guidance regarding the operationalization of personal heat exposure research methods.
Discussion:
We define personal heat exposure as realized contact between a person and an indoor or outdoor environment that poses a risk of increases in body core temperature and/or perceived discomfort. Personal heat exposure can be measured directly with wearable monitors or estimated indirectly through the combination of time–activity and meteorological data sets. Complementary information to understand individual-scale drivers of behavior, susceptibility, and health and comfort outcomes can be collected from additional monitors, surveys, interviews, ethnographic approaches, and additional social and health data sets. Personal exposure research can help reveal the extent of exposure misclassification that occurs when individual exposure to heat is estimated using ambient temperature measured at fixed sites and can provide insights for epidemiological risk assessment concerning extreme heat.
Conclusions:
Personal heat exposure research provides more valid and precise insights into how often people encounter heat conditions and when, where, to whom, and why these encounters occur. Published literature on personal heat exposure is limited to date, but existing studies point to opportunities to inform public health practice regarding extreme heat, particularly where fine-scale precision is needed to reduce health consequences of heat exposure. https://doi.org/10.1289/EHP556
Introduction
Environmental heat is a natural and anthropogenically enhanced hazard with well-documented adverse impacts on human health and well-being (Gasparrini et al. 2015; Parsons 2014). Despite decades of physiological, epidemiological, and climatological research about high temperatures, heat waves, and hot indoor and outdoor environments, information about the actual thermal conditions people experience as they go about their daily lives is scarce, leaving the potential for under-informed risk assessments, policies, and intervention measures concerning heat exposure and health. The recognition that personal exposure can differ substantially from fixed-point measurements has led to more valid and precise understandings of, and solutions for, the impacts of other environmental hazards on people, particularly the effects of air pollution (e.g., Payne-Sturges et al. 2003; Steinle et al. 2013). Analogous information about heat could become an important tool for designing better strategies to monitor exposure and reduce heat-related illness and death.
Heat illness and death occur when body core temperature exceeds a tolerable range for physiological functioning. Because biometric body temperature information is not widely collected and shared, researchers commonly seek proxy indicators for personal heat stress. The data that are often used to reflect indoor and outdoor conditions that can become dangerous for various types of activities and populations are generally well documented and accepted (Parsons 2014). Less understood is how often individual people encounter these conditions and how long exposures last; when, where, to whom, and why these encounters occur; how recurrent exposures may be associated with physiological impacts; and how best to reduce their frequency, duration, and severity.
Meteorological observations and climate model projections indicate that warm-season temperatures and the frequency and severity of extreme heat events have increased in recent decades and that this trend will continue (IPCC 2013). This warming will be exacerbated in many cities owing to the impacts of the built environment on local atmospheric conditions (Oke 1982). As a consequence of both global- and urban-scale processes, increases in heat exposure for some populations are expected. In the absence of additional adaptation—physiological, behavioral, or technological adjustment to actual or expected climate and its effects—adverse heat-related health events may become more common (IPCC 2014; Hondula et al. 2015). The challenges associated with current weather patterns and future warming have motivated many researchers to perform a variety of detailed heat-health risk assessments that largely aim to inform future adaptation efforts, local- to global-scale climate policy, or both (e.g., Gasparrini et al. 2015; Harlan et al. 2012; Vargo et al. 2016; Xiang et al. 2014).
The intent of our commentary is to catalyze discussion of personal heat exposure among environmental health scientists and practitioners. In particular, we lay the groundwork for additional perspectives on how personal heat exposure research could become a useful addition to the portfolio of techniques used to assess heat-health risk and ultimately reduce the health burden of heat. Studies are emerging that involve measuring and estimating personal heat exposure. Some researchers are capturing the environmental conditions experienced by individuals going about their daily lives using small, portable, affordable data loggers (Basu and Samet 2002; Bernhard et al. 2015; Kuras et al. 2015). Other investigators are estimating personal heat exposure via simulation models of the positions and travel patterns of large populations (Glass et al. 2015; Karner et al. 2015; Schlink et al. 2014). We explore how such studies relate to one another and enhance the precision and validity of knowledge about the impacts of heat on people. To do so, we first offer a definition for personal heat exposure. We next share insights from our own experiences studying and collecting personal heat exposure data, as well as perspectives gleaned from extant literature. Subsequently, we review how personal heat exposure research can advance scientific knowledge and inform public health practice.
Discussion
Defining Personal Heat Exposure
The word “personal” distinguishes personal heat exposure research from a large portion of the environmental health literature that assesses impacts of the thermal environment using a surrogate of potential exposure measured at one or more fixed geographical locations. “Personal” shifts the emphasis of the measurement setting from places to people (Ott 1982) and the unit of analysis from populations to individuals.
The word “heat” is more difficult to precisely define in a practical yet accurate manner. In the physical sciences, heat is defined as energy transferred from objects with higher temperatures to objects with lower temperatures. In hot weather, however, it is not only the transfer of energy from the environment to the body that is of concern for human health. In some circumstances, adverse health effects linked to thermal stress may also occur because the body is unable to adequately transfer energy to the environment to maintain core body temperature within normal physiological limits (WHO 2004). We adopt a usage similar to public and medical communication about hot weather and health: heat refers to a state of the environment in which the combination of the four relevant ambient parameters—air temperature, radiation (short- and long-wave), humidity, and air movement (Parsons 2014)—constrains energy dissipation from the body or adds energy to the body, thus posing a risk of discomfort, tissue injury, or a combination of the two secondary to the increase in core body temperature.
For our purposes, we are defining heat exposure as exposure that occurs because a person is present at a location where heat occurs. This exposure can be assessed in terms of magnitude, duration, and frequency. Consistent with the use of the term “exposure” in ambient air pollution research (Ott 1982), we are making a distinction between external exposure and dose. Our definition does not encompass internal exposure to heat (i.e., an internal dose of heat) because this results from the combined effects of environmental heat exposure and internal physiological interactions.
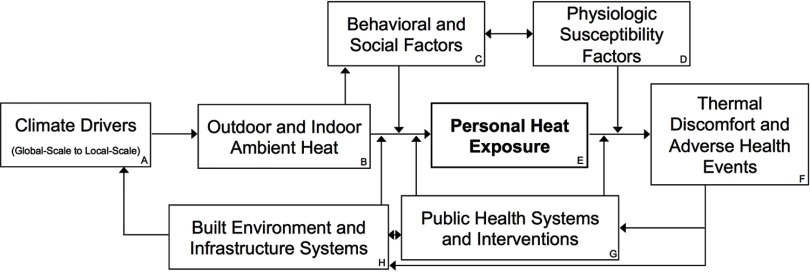
We define personal heat exposure as realized contact between a human and an indoor or outdoor environment in which the air temperature, radiative load, atmospheric moisture content, and air velocity collectively pose a risk of increase in body core temperature, perceived discomfort, or both. Increases in body core temperature are of clinical concern because of the potential for tissue injury and metabolic derangement. Perceived thermal discomfort can occur with or without changes to body core temperature and is a function of several factors including skin temperature, sweating rate/condition, psychological state, prior thermal exposure, and individual expectation of the thermal conditions to be encountered. Personal heat exposure is an important step of the conceptual pathway linking climate drivers and indoor and outdoor environmental conditions to thermal discomfort and adverse health outcomes (Figure 1).
Figure 1.
Conceptual pathway linking climate drivers (A) to outdoor and indoor ambient heat (B), personal heat exposure (E), and heat-related health and comfort outcomes (F). Behavioral and social factors (C) modify the association between ambient heat and personal heat exposure; physiologic susceptibility factors (D) modify the association between personal heat exposure and health and comfort outcomes. This pathway considers public health systems (G) and systems representing the built environment and other infrastructure (H) to be responsive to observed or perceived risks of adverse health or comfort outcomes. These systems can intervene at various stages of the conceptual pathway to reduce risk.
The definition we propose encompasses traditional considerations of both occupational and environmental exposures and intentionally focuses on only the exogenous factors that contribute to thermal discomfort and health outcomes. To sufficiently address an individual’s susceptibility to heat illness or other injuries associated with heat exposure, personal heat exposure information should be combined with information about physiological susceptibility factors (Figure 1, box D). Physiological factors that modify the relationship between personal heat exposure and adverse health events include but are not limited to age, sex, body mass and surface area, hydration status, metabolic rate, preexisting health conditions, psychological state, and acclimatization (Chan et al. 2001; Chen and Ng 2012). Elements and consequences of behavior and social context modify the association between ambient conditions and personal heat exposure (Figure 1, box C) but can also indirectly modify subsequent risks of adverse health events through their influence on physiological state. Applying our definition, two individuals with different physiological states in the same location would experience the same personal heat exposure but would not necessarily be equally susceptible to increases in core body temperature or to associated discomfort or adverse health impacts. Our conceptual pathway considers public health systems (box G) and systems that manage the built environment (box H) to be responsive to observed or perceived risks of thermal discomfort and adverse health events. Modifications to the built environment and to infrastructure systems can directly alter thermal environmental conditions (e.g., shade provisioning, air conditioning) and can alter the association between ambient heat and personal heat exposure (e.g., adding transit stops to reduce walking times). Public health systems and interventions can also modify determinants of personal heat exposure (e.g., behavioral change induced by warning messages) and can additionally modify the impacts of personal heat exposure on health (e.g., through medical care).
Challenges in Current Heat Exposure Assessment
The vast majority of epidemiological studies relating extreme heat to human health outcomes rely on meteorological observations of outdoor temperature and humidity from weather stations proximate to the study population as surrogate indicators for personal heat exposure (e.g., Gasparrini et al. 2015). Yet, we know that personal heat exposure is dependent on outdoor microclimate variability, indoor heat exposure, and a wide suite of social and behavioral factors such as individual travel patterns (e.g., Bernhard et al. 2015). Furthermore, in outdoor settings, radiative heat is a main factor influencing an individual’s heat load (Middel et al. 2016; Thorsson et al. 2007). Thus, heat exposure misclassification is likely widespread and substantial, particularly when considering the full human energy balance. The consequences of this misclassification will not be known until more personal exposure studies and fine-scale meteorological data become available.
Outdoor meteorological measurements from a sparse station network do not adequately represent the range of conditions experienced by people. In rural areas, populations may live dozens of miles away from the nearest weather station. Meteorological measurements are influenced by surrounding land cover (e.g., forest, urban) (Fall et al. 2011) and may be drawn from instruments deployed for reasons other than estimating representative conditions (e.g., at airports to support aviation). Contrasts exist between available observations and outdoor conditions in places of interest. In urban settings, the built environment and land use heterogeneity alter the exchange of energy and moisture between the surface and atmosphere, creating local climate variability and the urban heat island (UHI) effect (Oke 1982).
The scale of misclassification related to weather station siting, however, is likely to be small when compared with the misclassification associated with the location of exposures, and in particular, if the exposure occurs indoors or outdoors. On average in the United States and Canada, large-scale survey data indicate that people spend most of their time () indoors (e.g., Klepeis et al. 2001). In most cases, buildings moderate thermal extremes experienced outdoors by reducing exposure to solar radiation, high and low temperatures, and wind. Today, many buildings are climate-controlled to maintain nearly constant temperature and humidity levels, increasing the divergence between weather station observations and personal heat exposure.
The growing prevalence of air conditioning and divergence between outdoor and indoor thermal conditions does not imply, however, that no heat-health hazards exist indoors. In fact, a high proportion (50–80%) of decedents classified as victims of extreme heat may perish inside their own homes (Fouillet et al. 2006; CDC 2013). Indoor environments are influenced by the composition and configuration of the residential matrix, heating, ventilation, air conditioning, and occupant behavior, preference, and ability or willingness to pay for thermal modification (IOM 2011). Buildings without adequate climate controls may amplify heat exposure above outdoor levels owing to the high thermal mass of many buildings, which absorbs and retains heat and effectively heats the indoor environment, thus increasing the risk of heat-related morbidity and mortality (White-Newsome et al. 2012). Other studies have shown only weak correlations between outdoor and indoor temperatures and moderate correlations between outdoor and indoor humidity (Smargiassi et al. 2008; Uejio et al. 2016).
Exposure misclassification is of particular concern for certain groups of people, including those with limited opportunities to change their exposures. Workers engaged in agriculture, construction, firefighting, manufacturing, military, or resource extraction face heightened health risks owing to exertion and prolonged heat exposures from outdoor conditions, extreme indoor environments, heat generated by machinery or power equipment, or a combination of these factors (Xiang et al. 2014). Athletes and others involved in high-exertion recreational activities may also be at high risk with limited agency and conflicting motivation to engage in adaptive behaviors (Casa et al. 2015). Localized, on-site meteorological monitoring is already recommended or employed in many of the settings in which such circumstances occur (e.g., Parsons 2006). Additional personal exposure monitoring could yield even greater insight into individual-level variability in exposures and time–activity patterns that influence how accurately measures of ambient conditions reflect personal heat exposure in these settings.
Measuring Personal Heat Exposure
What to Measure and How
As individuals move through time and space, they experience a range of thermal environmental conditions. Consider the downtown area of a busy city on a hot and humid day. Within ten city blocks, individuals may be sitting in air-conditioned offices, walking through shaded parks or on sunny sidewalks, welding steel many stories up a new construction project, or doing any number of activities that could affect their environment, clothing, and physical exertion. In a traditional population-based epidemiological assessment, all of these individuals would be assigned the same official meteorological statistics collected at the nearest weather station located ten minutes away. The type of thermal environmental variability experienced by individuals within this city is often not well-captured in heat-health risk assessments. Personal heat exposure approaches address the limitations of current exposure assessment techniques by reducing misclassification at the level of the individual and by increasing precision through measuring temperature exposure at a finer spatial scale. These approaches combine information about the thermal environment, which helps describe where and when heat exposure may occur, with information about human travel patterns and the behavioral and social factors that help explain to whom and how heat exposure is realized. To date, and to the best of our knowledge, data about personal exposure to three of the four relevant parameters (air temperature, radiation, and humidity, but not air velocity) have been collected directly through personal monitoring approaches in which research participants wear devices that log observations as they go about normal activities (e.g., Bernhard et al. 2015; Kuras et al. 2015), and indirectly through simulation, in which meteorological information is merged with activity or transportation information (e.g., Glass et al. 2015; Karner et al. 2015). Personal monitoring addresses environmental conditions and travel patterns simultaneously, whereas simulations address these two components separately (Steinle et al. 2013).
Personal monitoring strategies utilize small, wearable data loggers that sense environmental conditions and store data internally. Commercially available devices exist to measure temperature, humidity, and sunlight (Table 1). Opportunities to measure these parameters using open-source electronics, such as Arduino, and cell phones are rapidly evolving, allowing for lower-cost monitoring (Muller et al. 2015). Light exposure data are useful in estimating time spent outside (outdoor light intensity is easily differentiated from lower-intensity indoor lighting even on cloudy days) and could be useful for estimating radiant heat exposure. Indirect estimates of sunlight exposure can also be obtained through matching activity logs completed by research participants to weather data. Short- and long-wave radiation exposure can be measured using globe thermometers and other sensors that yield mean radiant temperature, but we are not aware of studies that have employed these devices at the individual level. Air movement, typically measured with anemometers at central stations, can be measured at the individual level using globe anemo-radiometers (Nakayoshi et al. 2015), but it has not been explicitly incorporated in direct personal heat-monitoring studies to our knowledge. Simulation approaches have employed various combinations of the four parameters, obtained through central site monitors, gridded meteorological data sets, and remote sensing.
Table 1.
Examples of personal heat exposure measurement devices.
| Manufacturer | Devicea | Accuracyb | Device size | Memory | Additional featuresc | Retail cost (USD) | Website |
|---|---|---|---|---|---|---|---|
| Onset | HOBO TidbiT v2 Water Temperature Data Logger® | 64K bytes | Waterproof to 300 m; solar radiation shield is required | 133 | http://www.onsetcomp.com/products/data-loggers/utbi-001 | ||
| Onset | HOBO Pendant® Temperature/Light 8K or 64K Data Logger | , | 8K or 64K bytes | Waterproof housing for wet or underwater use, up to 30 m | 47 (8K bytes) or 64 (64 K bytes) | http://www.onsetcomp.com/products/data-loggers/ua-002-08 | |
| Onset | HOBO U23 Pro v2 (001–004) Temperature/Relative Humidity Data Logger® | , | 64K bytes | Weatherproof housing; user replaceable battery; model vary by temperature ranges; 003 and 004 can be immersed in water for extended periods of time | 145–170 | http://www.onsetcomp.com/products/data-loggers/u23-001 | |
| Maxim Integrated | iButton-basic® | 16 mm diameter (sensor) | 2 bytes | Alarm triggers | 4.40–8.80d | https://www.maximintegrated.com/en/products/digital/ibutton/DS1920.html | |
| Maxim Integrated | iButton-hygro® | , | 16 mm diameter (sensor) | 8K bytes | Logs time, variable measurement intervals (1 s to 273 hr), delayed start, alarm triggers | 79–149d | https://www.maximintegrated.com/en/products/digital/data-loggers/DS1923.html |
| Aginova | iCelsius Blue T/RH® | , | Storage on mobile device | Requires additional components to make sensor wearable, as well as a corresponding mobile app, bluetooth compatible with many iOS and Android devices | 49 | http://www.icelsius.com/store/icelsius_blue_rh | |
| Honeywell | HIH-4000 Integrated Circuit Humidity Sensor® | 2.54 mm | Requires additional parts | Must be connected to a controller to provide power and read in and store measurements | 10–14d | http://sensing.honeywell.com/HIH-4000-001-Humidity-Sensors | |
| Aosong | DHT22 Temperature- Humidity Sensor® | , | Requires additional parts | See AirBeam as example of wearable devices that incorporates this sensor along with air quality and noise: http://aircasting.org | 8–10d | https://www.adafruit.com/products/385 | |
| Analog Devices | TMP36 - Analog Temperature Sensor® | Requires additional parts | Must be connected to a controller to provide power and read in and store measurements | 1.50 | https://www.adafruit.com/products/165 | ||
| Measurement Specialities | HTU21D-F Temperature & Humidity Sensor Breakout Board® | , | Requires additional parts | Must be connected to a controller to provide power and read in and store measurements | 12–15d | https://www.adafruit.com/product/1899 |
Note: °C, degrees Celsius; K, thousand; RH, relative humidity; USD, U.S. dollars.
This list is not exhaustive but provides an overview of some of the more frequently used and basic measurement devices available at the time of publication and includes devices with which coauthors have direct experience.
Accuracy includes temperature (degrees Celsius), relative humidity (percent), and sunlight (nanometers), as applicable.
All sensors require some type of connector and/or communications device, such as a USB connector, unless otherwise noted in this column.
Total retail cost depends on quantity.
Because personal heat exposure depends upon an individual’s travel patterns through time and space, some aspects of behavior and social context are implicitly included in individual-level heat measurements. The missing elements required to estimate risk of increase in core body temperature, negative health outcomes, and thermal discomfort include individual physiological condition, adaptive strategies such as clothing choices, basal metabolic rate, and physical exertion. When conducting personal monitoring research, questionnaires, daily logs, phone-based apps, and photos may collect information about clothing, comfort, self-reported health status, and observations of heat-related symptoms; in addition, a range of biomarkers, monitors, and sensors can quantify parameters such as heart rate and activity level (e.g., Basu and Samet 2002; Spector et al. 2015). Beyond informing estimates of heat strain, these complementary data sources are useful to understand the circumstances in which heat exposure occurs, associated risk, and the extent to which individuals have agency or motivation to change their exposure.
Operationalizing Direct Exposure Assessment with Wearable Sensors
When designing data collection protocols to measure heat exposure using wearable sensors, a range of factors should be considered; chief among these factors is sensor placement. Thermal sensors should be worn outside of bags and clothing, exposed to atmospheric conditions at all times. Observations from devices placed on top of participants’ shoes, at the waist, and at the neck outside the shirt were relatively consistent for both temperature and relative humidity during no, moderate, and heavy physical activity (Dumas et al. 2016). For light exposure measurements, however, sensor placement on the body should remain consistent among participants because some parts of the body are more typically exposed to solar radiation than others (Weihs et al. 2013). Viable sensor placement must take into account the following:
-
•
Convenience and comfort. Placement on clothes or objects carried by participants yielded reliable data and participant compliance (Kuras et al. 2015; Uejio et al. 2016). Sensors (HOBO®, Onset Computer Corporation) clipped to the shoe resulted in some discomfort among women wearing dress shoes (Bernhard et al 2015).
-
•
Participants’ physical attributes and anticipated behaviors. Sweat-inducing activities potentially affect humidity readings.
-
•
Environmental characteristics. Contact with wet or high-heat-radiating surfaces and exposure to or submersion in water should be avoided. Care should also be given to sensor placement in the context of highly localized point sources of heat (e.g., welding), which may not substantively reflect the environmental conditions of interest to the researcher.
-
•
Body heat. The extent to which body heat influences sensor readings should stay consistent among participants as much as is possible. The relationship between sensor placement and heat exposure estimates requires further investigation.
-
•
Safety concerns. In certain occupational or recreational settings, some configurations for sensor placement may not be available, safe, or preferable for participants (e.g., because of risks of the sensor getting tangled or interfering with equipment).
Finally, participants should be encouraged to avoid touching or repositioning sensors unnecessarily.
Although wearing or carrying a data logger is less intrusive than other research activities, recruiting individuals to participate is a limiting factor for study design. We have found that participants usually consider the sensors noted above to be unobtrusive in their daily lives. In an occupational setting, recruitment may involve working with an agency, then managers, and finally individual staff. This top-down recruitment of a specific population may be effective but could limit individual interest and raise concerns about coerced participation, adequate representation of exposures experienced, and data ownership (Jagger et al. 2016). In other circumstances, individuals may be recruited directly in a neighborhood or community context through existing organizations, fliers in businesses, or word of mouth (Kuras et al. 2015). Partnering with community organizations allowed community partners to follow up with participants and respond to concerns about wearing the monitor in various settings (Bernhard et al. 2015). Investigations that involve participants more actively throughout the research process, including study design, data collection, and data analysis, may also increase participant buy-in and the relevance of the research to on-the-ground community concerns. Although such buy-in is critical in all human-subjects research, tasks inherent in personal monitoring (i.e., remembering to place sensors on the body) demand a level of commitment above and beyond that required for methods such as surveys, interviews, or diaries.
Estimating Personal Heat Exposure Indirectly
There are limits to the scale at which personal heat exposure data can be collected with wearable sensors. Alternate approaches leverage large-scale data sets to estimate personal heat exposure indirectly, enabling examination of larger populations while introducing greater uncertainties regarding the accuracy and precision of environmental and time–activity data. The most comprehensive method for assessing personal heat exposure indirectly would involve combining high-resolution thermal environment data (including temperature, humidity, radiation, and wind speed) for all indoor and outdoor locations occupied by individuals in a population of interest along with detailed time–location records for each individual. The intersection of these two data sources would produce simulated personal heat exposure profiles that could be interrogated to answer various questions of interest to researchers and practitioners. To date, researchers have combined meteorological data with large-scale census, survey, and/or activity pattern simulations to estimate exposure in different local environments, examining particular drivers of risk or certain circumstances associated with exposure (e.g., Glass et al. 2015; Karner et al. 2015; Schlink et al. 2014).
Environmental data sources for indirect personal heat exposure methods offer trade-offs with respect to representativeness, spatial coverage, and labor and data processing needs. Citizen scientist networks of weather stations such as WeatherBug increase the density of data availability (Muller et al. 2015), but data may be sparse in low-income urban settings that are most affected by UHIs, and this approach requires additional quality control and bias correction. Alternatively, researchers (or public officials) can implement their own high-density sensor networks on public property, such as lampposts or trees, or on the private property of community volunteers (e.g., the Array of Things Project, Jacob 2015). Intentional transects, in which individuals move along predefined paths while making meteorological measurements, provide another strategy for researchers to collect high-density heat information in areas with high microclimatic variability (e.g., Nakayoshi et al. 2015; Tsin et al. 2016). Enriching the volume and quality of data available regarding indoor environments is an urgent need. Across outdoor and indoor environments, collecting measurements that are both of high quality and representative of the human experience presents a range of challenges, from microclimatic variability to device accuracy to sensor placement and response time (Oke 2006).
Many researchers have used remotely sensed (usually satellite-derived) and model-derived temperature estimates in analyses of heat impacts or vulnerability assessments (e.g., Harlan et al. 2012). Although remotely sensed measurements offer unprecedented spatial coverage and bypass the challenges of implementing reliable in situ heat monitoring networks, researchers must make assumptions when linking remote temperature measurements with those relevant to personal heat exposure. Remotely sensed radiometric temperature estimates are based on surface emission of thermal infrared radiation. They correlate strongly with air temperature at a large scale, but neighborhood-scale correlations are significantly lower because of variability in surface emissive properties, shadowing effects, and the influence of wind on air temperature (e.g., Prihodko and Goward 1997; Nichol et al. 2009). Other shortcomings include data gaps due to infrequent satellite overpass schedules, lack of representativeness due to cloud interference, and inadequate spatial resolution for some applications. High-resolution climate model simulation output (e.g., Heaton et al. 2014) and gridded/interpolated meteorological data sets (e.g., DayMet, Thornton et al. 1997) are also viable for indirect methods. In addition to retrospective analysis, these tools can be used to explore the impacts of projected or possible changes in the urban landscape and global climate on personal heat exposure. However, scale mismatch and bias correction limit the ability of these data sources to capture extremes in environmental conditions, which might lead to misrepresentation of exposures of interest (e.g., Guentchev et al. 2016).
Information about the thermal environment must be complemented with information about individuals’ locations and activities, particularly time outdoors, distances traveled, and use of transportation. These data can be collected through tracking devices, including dedicated GPS devices (Kerr et al. 2011), cell phone–based location information (Khan et al. 2015), light-sensing devices (e.g., Bernhard et al. 2015), or through personal reports via logs, surveys, time–activity diaries, or interviews (e.g., Klepeis et al. 2001; McCurdy and Graham 2003). These approaches require volunteers who are willing to report their travel patterns or to have them recorded. Recall and reporting errors can be a problem for self-reported activity logs, and tracking devices need to be carried and activated to be meaningful. Large-scale simulations of time–activity patterns, often used in transportation planning, provide an additional type of data about human mobility (Glass et al. 2015; Karner et al. 2015). Geographic Information Systems (GIS) may help researchers integrate such information about travel patterns with thermal environment data, thereby facilitating visualizations and predictions across time and space.
Analyzing Personal Heat Exposure Data
Strategies for analyzing personal heat exposure data have used a variety of aggregating and statistical techniques with the goal of understanding exposure patterns. Several issues have been explored, including the following:
-
•
Correlations between data from personal heat exposure sampling, often at relatively high frequencies (e.g., 1–5-min intervals), and data from stationary monitors with lower sampling frequencies (e.g., hourly), for periods of up to 1 wk (Basu and Samet 2002; Bernhard et al. 2015; Kuras et al. 2015).
-
•
Appropriate sampling periods to capture exposures that may lead to heat stress. Physiologically, capturing exposure at relatively short intervals (e.g., every 15 minutes) may be most appropriate in extreme heat settings. Karner et al. (2015) generated an Extreme Degree-Minute metric that aggregates the time simulated individuals spent above a certain heat threshold while participating in nonmotorized transport.
-
•
Statistical approaches for managing personal exposure data and linking exposure data from different sources, for example, estimating the relationship between outdoor conditions and personal heat exposure by incorporating a random effect term into a linear mixed model (Bernhard et al. 2015).
Despite the progress that has been made, several issues remain, including temporal autocorrelation, diurnal cycles, and within- and between-participant behaviors and physiology. Future personal heat exposure analyses should utilize and refine more sophisticated statistical approaches, such as random forest models (Brokamp et al. 2017) or two-stage semi-parametric regression models (Deffner et al. 2016), that have been employed in air pollution personal exposure data analyses to build prediction models that include the contributions of outdoor, indoor, and home characteristics and behaviors to personal exposure. More work is also needed to understand the time-lagged relationship between personal exposure and the onset of physiological symptoms, including increasing body core temperature (e.g., Figure 1 of Koehler and Peters 2015). Future work should also leverage prior research establishing thresholds for characterizing dangerous exposures based on generalized physiological principles and observations, such as charts of physiologically equivalent temperature (e.g., Matzarakis et al. 1999), exertion–rest thresholds based on the wet-bulb globe temperature (WBGT) index (e.g., Parsons 2006), and thresholds and triggers informed through analyses of specific populations and health end points (e.g., Petitti et al. 2015). More detailed analyses will be useful for determining optimal sampling frequencies and frames, sample sizes, and metrics for exploring associations with various health outcomes.
Implications of Personal Heat Exposure Research
We identify four broad areas in which personal heat exposure research can have a positive impact on research and practice: developing a more valid and precise understanding of the human experience with heat, more effective targeting of intervention measures, evaluation of interventions and spatiotemporal trends, and community engagement and outreach. More generally, we envision that personal heat exposure data could become a fundamental component of how we think about and respond to societal challenges associated with extreme heat. Achieving this broad goal will require a large community of practice comprising collaborators from disciplines including atmospheric science, computer science, epidemiology, anthropology, medicine, engineering, environmental health, geography, and urban planning.
By measuring the thermal environment as experienced by individuals, personal heat exposure approaches may illuminate fine-scale differences in attributes, behaviors, preferences, and access to cooling resources within or between populations. Although this knowledge does not complete the pathway from environmental hazard to health outcome, it may illuminate mechanisms and patterns through which suspected risk factors (e.g., urban form, poverty, social or linguistic isolation, housing quality) and capacity for resilience (e.g., adaptive behavior, heat-mitigating infrastructure) are realized into exposure, particularly when appropriate qualitative methods are involved to provide necessary context. Further, personal exposure approaches may both facilitate early diagnosis and intervention related to clinical heat illness and provide a more complete understanding of the total health burden of heat, a topic of long-standing debate in the literature, given that administrative health records do not often provide sufficient information regarding exposure history (e.g., Shen et al. 1998; Whitman et al. 1997).
If available on a larger scale, personal heat exposure data could be incorporated into epidemiological and geographical research aiming to pinpoint social and environmental determinants of risk and vulnerable populations. The surrogate exposure variables used in current time series and spatial models for heat morbidity and mortality, for example, could be supplemented by or replaced with personal heat exposure estimates, highlighting exposure-driven differences in outcomes that have not yet been explored. The primary opportunity we see at present for personal exposure research is to inform the modeling approaches that output exposure data for use in subsequent epidemiological analyses. Recently published research, for example, demonstrates that fixed-point airport temperature data may underestimate the effect of temperature on mortality when compared with a higher-resolution, satellite-derived, spatially continuous estimate of the same variable (Lee et al. 2016). We propose that these positive developments can be even further accelerated with guidance from personal heat exposure studies. Personal monitoring data and time–activity assessment have been similarly leveraged in air pollution epidemiology for at least the past decade (e.g., Nethery et al. 2008; Özkaynak et al. 2013; Baxter et al. 2013).
Personal heat exposure research offers a promising means of informing decision making and targeting intervention measures because it can substantially enhance our knowledge of the who, why, where, and when dimensions of exposure-related health risks. Reports of personal heat exposure studies should clearly communicate methodological limitations and uncertainties in study findings to help policy makers and decision makers understand how this type of information might complement existing research or decision support tools already in use. Such transparency is particularly important at present, when personal heat exposure studies are limited in number and scope. A potential policy application of this research is providing guidance for the targeted deployment of heat mitigation strategies such as cool roofs or green infrastructure. Additionally, individuals may learn more about their own exposure patterns and might be able to take preventative actions in advance of dangerous increases in core temperature if able to interact with their own exposure data. We envision that users of their own personal heat exposure data would likely come from particular niches such as athletics, the military, or certain outdoor occupations, sectors where methods of providing real-time physiological information related to heat stress are already being explored (e.g., Wickwire et al. 2012). Enhancing decision-support tools for institutions and individuals with personal exposure data is consistent with goals to increase the adoption of the evidence-based public health framework for climatic hazards and climate change (Hess et al. 2014).
Just as personal heat exposure research enables better targeting of extreme heat intervention measures, so too can it facilitate the evaluation of their effectiveness by reducing the potential for misclassification related to exposure. Such an improvement would come at a critical time: in a recent review, Boeckmann and Rohn (2014) reported that “concrete evidence for the effectiveness” of strategies such as heat warning systems “is lacking,” citing challenges in defining a counterfactual and the absence of true control groups as major hindrances to rigorous evaluative research. Ecological epidemiological studies reporting declines in heat-related mortality coincident with the deployment of heat warning systems have been unable to draw conclusions based on process and mechanism (Boeckmann and Rohn 2014), complicating claims of causality. Used in appropriate study designs, direct measurements of personal heat exposure could dramatically improve our understanding of whether and why certain adaptation measures work. For example, Longo et al. (2017) found that homeless individuals enrolled in a residential program at a local shelter experienced reduced heat exposure compared with homeless individuals not in the program, which may help explain differential health outcomes between those two groups. At a larger scale, examining exposure patterns more rigorously can help us understand why spatial and temporal patterns in heat-related deaths and illness have emerged, as well as predict the impact of future climate change on heat-related deaths and illnesses (Hondula et al. 2015).
Personal heat exposure research creates new opportunities for community and educational outreach. Several authors of this paper have engaged communities during and after personal heat exposure studies by organizing lectures at local libraries, hosting a temperature-themed bingo game, leading a thermal historical walking tour, and delivering reports and presentations to study participants with their exposure data. Similarly to the ways in which participatory research with air pollution sensors have empowered some communities to pursue environmental justice and reduce health disparities related to poor air quality (e.g., Grineski 2006), we can also imagine—and have begun to observe in some of our own projects—that personal heat exposure data can be leveraged for communities to advocate for and achieve socioenvironmental changes.
Limitations
Personal heat exposure methods have limitations worth noting even if their application leads to more valid and precise exposure estimates. An overarching challenge that researchers face at present, and will continue to face for some time, is a lack of standards and best practices, which will hinder the comparability of studies and could limit interpretation and uptake by decision makers and policy makers. Similar to other developments that leverage technology to gather individualized data (e.g., precision medicine), other potential issues include privacy, selection bias, data ownership, data quality, and cost. Given the interest in linking personal heat exposure with location and activity data, data collection could be seen as intrusive or burdensome, constraining generalizability. Similarly, there may be issues with employers or other gatekeepers regarding correlation of personal heat exposure and activity data and regarding data ownership. Many of these issues are clearly surmountable with the use of appropriate techniques and safeguards; nevertheless, they should be mentioned. A final caveat involves the potential for overemphasizing precision in heat exposure estimates at the expense of investment in other important heat-health research questions. Determining adequate precision in exposure estimates required to support evaluation of interventions is likely the most effective way to advance both research and practice goals.
Conclusions
In this commentary, we defined personal heat exposure as realized contact between a person and an indoor or outdoor environment that poses a risk of increases in body core temperature, perceived discomfort, or both. Focusing on personal heat exposure using novel methods and devices for data collection presents opportunities to increase both validity and precision in heat exposure assessment. These methods also allow researchers and public health practitioners to gain important insights into human behavior and environmental conditions. Although the published literature is limited, this approach highlights individual aspects of the heat-health relationship that may be key to understanding how to best reduce the frequency, duration, and severity of exposure. Knowledge gained can be applied to developing a better understanding of how people experience hot weather, to designing and evaluating interventions, to analyzing spatiotemporal trends, and to targeting community engagement and outreach activities to reduce the health burden of heat.
Acknowledgments
The authors acknowledge K. Brown, J. Brown-Saracino, M. Chester, M. Evans, C. Gronlund, S. Harlan, E. Johnson, E. Johnston, M. O’Neill, B. Ruddell, B. Stone, S. Threadgill Matthews, S. Tyson, and other collaborators for their contributions to prior and ongoing personal heat exposure research efforts, some of which are referenced in this commentary.
E.K. and D.H. were partially supported by the National Science Foundation (NSF) through the Central Arizona-Phoenix Long-Term Ecological Research (CAP LTER) program (BCS-1026865). M.B. was supported in part by the National Institutes of Health (NIH) (T32 HL105349) and the Nutrition Obesity Research Center (P30DK0563360). M.B., J.G., A.S., and B.Z. are partially supported by NIH grant R01 ES023029. J.H. was partially supported by NIH grant R21TW009535. A.S. was supported in part by NSF Integrative Graduate Education and Research Traineeship Program (IGERT) DGE-1069213. J.S. was supported in part by Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health (CDC/NIOSH) grant 5K01OH010672-02. D.H. was partially supported by the Virginia G. Piper Trust Health Policy Informatics Initiative and NSF grant SES-1520803. J.V., A.M., and D.H. were partially supported by NSF Sustainability Research Network (SRN) Cooperative Agreement 1444758. The opinions expressed are those of the authors and do not necessarily represent those of the NIH, NSF, CDC, NIOSH, or any other organization.
References
- Basu R, Samet JM. 2002. An exposure assessment study of ambient heat exposure in an elderly population in Baltimore, Maryland. Environ Health Perspect 110(12):1219–1224, PMID: 12460801, 10.1289/ehp.021101219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter LK, Dionisio KL, Burke J, Ebelt Sarnat S, Sarnat JA, Hodas N, et al. 2013. Exposure prediction approaches used in air pollution epidemiology studies: key findings and future recommendations. J Expos Sci Environ Epidemiol 23(6):654–659, PMID: 24084756, 10.1038/jes.2013.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhard MC, Kent ST, Sloan ME, Evans MB, McClure LA, Gohlke JM. 2015. Measuring personal heat exposure in an urban and rural environment. Environ Res 137:410–418, PMID: 25617601, 10.1016/j.envres.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeckmann M, Rohn I. 2014. Is planned adaptation to heat reducing heat-related mortality and illness? A systematic review. BMC Public Health 14:1112, PMID: 25349109, 10.1186/1471-2458-14-1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokamp C, Jandarov R, Rao MB, LeMasters G, Ryan P. 2017. Exposure assessment models for elemental components of particulate matter in an urban environment: a comparison of regression and random forest approaches. Atmos Environ 151:1–11, 10.1016/j.atmosenv.2016.11.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casa DJ, DeMartini JK, Bergeron MF, Csillan D, Eichner ER, Lopez RM, et al. 2015. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train 50(9):986–1000, PMID: 26381473, 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention). 2013. Heat illness and deaths–New York City, 2000-2011. MMWR Morb Mortal Wkly Rep 62(3):617–621, PMID: 23925170. [PMC free article] [PubMed] [Google Scholar]
- Chan NY, Stacey MT, Smith AE, Ebi KL, Wilson TF. 2001. An empirical mechanistic framework for heat-related illness. Clim Res 16(2):133–143, 10.3354/cr016133. [DOI] [Google Scholar]
- Chen L, Ng E. 2012. Outdoor thermal comfort and outdoor activities: A review of research in the past decade. Cities 29(2):118–125, 10.1016/j.cities.2011.08.006. [DOI] [Google Scholar]
- Deffner V, Küchenhoff H, Maier V, Pitz M, Cyrys J, Breitner S, et al. 2016. Personal exposure to ultrafine particles: two-level statistical modeling of background exposure and time-activity patterns during three seasons. J Expo Sci Environ Epidemiol 26(1):17–25, PMID: 25407347, 10.1038/jes.2014.73. [DOI] [PubMed] [Google Scholar]
- Dumas JS, Jagger MA, Kintziger KW. 2016. Where to wear ibuttons: Individual level temperature and humidity observations for public health surveillance [Abstract]. In: American Meteorological Society Annual Meeting. https://ams.confex.com/ams/96Annual/webprogram/Paper280434.html [accessed 17 May 2016].
- Fall S, Watts A, Nielsen‐Gammon J, Jones E, Niyogi D, Christy JR, et al. 2011. Analysis of the impacts of station exposure on the U.S. Historical Climatology Network temperatures and temperature trends. J Geophys Res 116(D14):2156–2202, 10.1029/2010jd015146. [DOI] [Google Scholar]
- Fouillet A, Rey G, Laurent F, Pavillon G, Bellec S, Guihenneuc-Jouyaux C, et al. 2006. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health 80(1):16–24, PMID: 16523319, 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. 2015. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 386(9991):369–375, PMID: 26003380, 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass K, Tait P, Hanna E, Dear K. 2015. Estimating risks of heat strain by age and sex: A population-level simulation model. Int J Environ Res Public Health 12(5):5241–5255, PMID: 25993102, 10.3390/ijerph120505241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grineski S. 2006. Local struggles for environmental justice: Activating knowledge for change. J Poverty 10(3):25–49, 10.1300/j134v10n03_02. [DOI] [Google Scholar]
- Guentchev GS, Rood RB, Ammann CM, Barsugli JJ, Ebi K, Berrocal V, et al. 2016. Evaluating the appropriateness of downscaled climate information for projecting risks of Salmonella. Int J Environ Res Public Health 13(3):267, PMID: 26938544, 10.3390/ijerph13030267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti D. 2012. Neighborhood effects on heat deaths: Social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect 121(2):197–204, PMID: 23164621, 10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton MJ, Sain SR, Greasby TA, Uejio CK, Hayden MH, Monaghan AJ, et al. 2014. Characterizing urban vulnerability to heat stress using a spatially varying coefficient model. Spat Spatiotemporal Epidemiol 8:23–33, PMID: 24606992, 10.1016/j.sste.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Hess JJ, Eidson M, Tlumak JE, Raab KK, Luber G. 2014. An evidence-based public health approach to climate change adaptation. Environ Health Perspect 122(11):1177–1186, PMID: 25003495, 10.1289/ehp.1307396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hondula DM, Balling RC, Vanos JK, Georgescu M. 2015. Rising temperatures, human health, and the role of adaptation. Curr Clim Change Rep 1(3):144–154, 10.1007/s40641-015-0016-4. [DOI] [Google Scholar]
- IOM (Institute of Medicine). 2011. Climate Change, the Indoor Environment, and Health. Washington, DC:National Academies Press; https://www.nap.edu/catalog/13115/climate-change-the-indoor-environment-and-health [accessed 20 February 2016]. [Google Scholar]
- IPCC (Intergovernmental Panel on Climate Change). 2013. Summary for Policymakers. In: Climate Change 2013: The Physical Science Basis. Stocker TF, Qin D, Plattner G-K, Tignor MMB, Allen SK, Boschung J, et al. , eds. New York, NY:Cambridge University Press; http://www.ipcc.ch/report/ar5/wg1/ [accessed 25 March 2016]. [Google Scholar]
- IPCC. 2014. In: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part B: Regional Aspects. Barros VR, Field CB, Dokken DJ, Mastrandrea MD, Mach KL, Bilir TE, et al. , eds. New York, NY:Cambridge University Press; http://www.ipcc.ch/report/ar5/wg2/ [accessed 25 March 2016]. [Google Scholar]
- Jacob R. 2015. Informing urban decision making with an array of things. In: 2015 American Geophysical Union (AGU) Fall Meeting 14–18 December 2015 San Francisco, CA https://agu.confex.com/agu/fm15/webprogram/Paper58770.html [accessed 17 May 2016]. [Google Scholar]
- Jagger MA, Kintziger KW, Cavicchia P, Chalmers J, Duclos C, Dumas JS, et al. 2016. Lessons learned from a collaborative occupational heat exposure pilot using iButtons: Florida Department of Health, Florida State University, and the City of Tallahassee. In: Proceedings: 2016 Summit on Environmental Hazards and Health Effects 26–29 January 2016 Atlanta, GA. [Google Scholar]
- Karner A, Hondula DM, Vanos JK. 2015. Heat exposure during non-motorized travel: implications for transportation policy under climate change. J Transport Health 2(4):451–459, 10.1016/j.jth.2015.10.001. [DOI] [Google Scholar]
- Kerr J, Duncan S, Schipperjin J. 2011. Using Global Positioning Systems in Health Research. Am J Prev Med 41(5):532–540, PMID: 22011426, 10.1016/j.amepre.2011.07.017. [DOI] [PubMed] [Google Scholar]
- Khan A, Imon S, Das S. 2015. A novel localization and coverage framework for real-time participatory urban monitoring. Pervasive Mob Comput 23:122–138, 10.1016/j.pmcj.2015.07.001. [DOI] [Google Scholar]
- Klepeis N, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, et al. 2001. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol 11(3):231–252, PMID: 11477521, 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- Koehler KA, Peters TM. 2015. New methods for personal exposure monitoring for airborne particles. Curr Environ Health Rep 2(4):399–411, PMID: 26385477, 10.1007/s40572-015-0070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuras ER, Hondula DM, Brown-Saracino J. 2015. Heterogeneity in individually experienced temperatures (IETs) within an urban neighborhood: Insights from a new approach to measuring heat exposure. Int J Biometeorol 59(10):1363–1372, PMID: 25567543, 10.1007/s00484-014-0946-x. [DOI] [PubMed] [Google Scholar]
- Lee M, Shi L, Zanobetti A, Schwartz JD. 2016. Study on the association between ambient temperature and mortality using spatially resolved exposure data. Environ Res 151:610–617, PMID: 27611992, 10.1016/j.envres.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo J, Kuras E, Smith H, Hondula DM, Johnston E. 2017. Technology use, exposure to natural hazards, and being digitally invisible: implications for policy analytics. Policy & Internet 9(1):76–108, 10.1002/poi3.144. [DOI] [Google Scholar]
- Matzarakis A, Mayer H, Iziomon M. 1999. Applications of a universal thermal index: physiological equivalent temperature. Int J Biometeorol 43(2):76–84, PMID: 10552311, 10.1007/s004840050119. [DOI] [PubMed] [Google Scholar]
- Mccurdy T, Graham S. 2003. Using human activity data in exposure models: Analysis of discriminating factors. J Expo Anal Environ Epidemiol 13(4):294–317, PMID: 12923556, 10.1038/sj.jea.7500281. [DOI] [PubMed] [Google Scholar]
- Middel A, Selover N, Hagen B, Chhetri N. 2016. Impact of shade on outdoor thermal comfort - A seasonal field study in Tempe, Arizona. Int J Biometeorol 60(12):1849–1861, PMID: 27192997, 10.1007/s00484-016-1172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller CL, Chapman L, Johnston S, Kidd C, Illingworth S, Foody G, et al. 2015. Crowdsourcing for climate and atmospheric sciences: Current status and future potential. Int J Climatol 35(11):3185–3203, 10.1002/joc.4210. [DOI] [Google Scholar]
- Nakayoshi M, Kanda M, de Dear R. 2015. Globe Anemo-radiometer. Boundary-Layer Meteorol 155(2):209–227, 10.1007/s10546-014-0003-7. [DOI] [Google Scholar]
- Nethery E, Leckie SE, Teschke K, Brauer M. 2008. From measures to models: an evaluation of air pollution exposure assessment for epidemiological studies of pregnant women. Occup Environ Med 65(9):579–586, PMID: 18070798, 10.1136/oem.2007.035337. [DOI] [PubMed] [Google Scholar]
- Nichol JE, Fung WY, Lam KS, Wong MS. 2009. Urban heat island diagnosis using ASTER satellite images and ‘in situ’ air temperature. Atmospheric Research 94(2):276–284, 10.1016/j.atmosres.2009.06.011. [DOI] [Google Scholar]
- Oke TR. 1982. The energetic basis of the urban heat island. Q J R Meteorol Soc 108(455):1–24, 10.1002/qj.49710845502. [DOI] [Google Scholar]
- Oke TR. 2006. Towards better scientific communication in urban climate. Theor Appl Climatol 84(1–3):179–190, 10.1007/s00704-005-0153-0. [DOI] [Google Scholar]
- Ott W. 1982. Concepts of human exposure to air pollution. Environ Int 7(3):179–196, 10.1016/0160-4120(82)90104-0. [DOI] [Google Scholar]
- Özkaynak H, Baxter LK, Dionisio KL, Burke J. 2013. Air pollution exposure prediction approaches used in air pollution epidemiology studies. J Expos Sci Environ Epidemiol 23(6):566–572, PMID: 23632992, 10.1038/jes.2013.15. [DOI] [PubMed] [Google Scholar]
- Parsons K. 2006. Heat stress standard ISO 7243 and its global application. Ind Health 44(3):368–379, PMID: 16922180, 10.2486/indhealth.44.368. [DOI] [PubMed] [Google Scholar]
- Parsons K. 2014. Human Thermal Environments: The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort, and Performance. Boca Roton, FL:CRC Press. [Google Scholar]
- Payne-Sturges D, Burke T, Breysse P, Diener-West M, Buckley T. 2003. Personal exposure meets risk assessment: a comparison of measured and modeled exposures and risks in an urban community. Environ Health Perspect 112(5):589–598, PMID: 15064166, 10.1289/ehp.6496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitti D, Hondula DM, Yang S, Harlan S, Chowell G. 2015. Multiple trigger points for quantifying heat-health impacts: new evidence from a hot climate. Environ Health Perspect 124(2):176–183, PMID: 26219102, 10.1289/ehp.1409119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prihodko L, Goward S. 1997. Estimation of air temperature from remotely sensed surface observations. Remote Sens Environ 60(3):335–346, 10.1016/s0034-4257(96)00216-7. [DOI] [Google Scholar]
- Schlink U, Kindler A, Großmann K, Schwarz N, Franck U. 2014. The temperature recorded by simulated mobile receptors is an indicator for the thermal exposure of the urban inhabitants. Ecol Indic 36:607–616, 10.1016/j.ecolind.2013.09.017. [DOI] [Google Scholar]
- Shen T, Howe H, Alo C, Moolenaar R. 1998. Toward a broader definition of heat-related death: comparison of mortality estimates from medical examiners' classification with those from total death differentials during the July 1995 heat wave in Chicago, Illinois. Am J Forensic Med Pathol 19(2):113–118, PMID: 9662104, 10.1097/00000433-199806000-00003. [DOI] [PubMed] [Google Scholar]
- Smargiassi A, Fournier M, Griot C, Baudouin Y, Kosatsky T. 2008. Prediction of the indoor temperatures of an urban area with an in-time regression mapping approach. J Expo Sci Environ Epidemiol 18(3):282–288, PMID: 17579651, 10.1038/sj.jes.7500588. [DOI] [PubMed] [Google Scholar]
- Spector J, Krenz J, Blank K. 2015. Risk factors for heat-related illness in Washington crop workers. J Agromedicine 20(3):349–359, PMID: 26237726, 10.1080/1059924x.2015.1047107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinle S, Reis S, Sabel C. 2013. Quantifying human exposure to air pollution—moving from static monitoring to spatio-temporally resolved personal exposure assessment. Sci Total Environ 443:184–193, PMID: 23183229, 10.1016/j.scitotenv.2012.10.098. [DOI] [PubMed] [Google Scholar]
- Thornton P, Running S, White M. 1997. Generating surfaces of daily meteorological variables over large regions of complex terrain. Journal of Hydrology 190(3–4):214–251, 10.1016/s0022-1694(96)03128-9. [DOI] [Google Scholar]
- Thorsson S, Lindberg F, Eliasson I, Holmer B. 2007. Different methods for estimating the mean radiant temperature in an outdoor urban setting. Int J Climatol 27(14):1983–1993, 10.1002/joc.1537. [DOI] [Google Scholar]
- Tsin PK, Knudby A, Krayenhoff ES, Ho HC, Brauer M, Henderson SB. 2016. Microscale mobile monitoring of urban air temperature. Urban Climate 18:58–72, 10.1016/j.uclim/2016.10.001. [DOI] [Google Scholar]
- Uejio C, Tamerius J, Vredenburg J, Asaeda G, Isaacs D, Braun J, et al. 2016. Summer indoor heat exposure and respiratory and cardiovascular distress calls in New York City, NY, U.S. Indoor Air 26(4):594–604, PMID: 26086869, 10.1111/ina.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargo J, Stone B, Habeeb D, Liu P, Russell A. 2016. The social and spatial distribution of temperature-related health impacts from urban heat island reduction policies. Environ Sci Policy 66:366–374, 10.1016/j.envsci.2016.08.012. [DOI] [Google Scholar]
- Weihs P, Schmalwieser A, Reinisch C, Meraner E, Walisch S, Harald M. 2013. Measurements of personal UV exposure on different parts of the body during various activities. Photochem Photobiol 89(4):1004–1007, PMID: 23587050, 10.1111/php.12085. [DOI] [PubMed] [Google Scholar]
- White-Newsome J, Sánchez BN, Jolliet O, Zhang Z, Parker EA, Dvonch JT, et al. 2012. Climate change and health: indoor heat exposure in vulnerable populations. Environ Res 112:20–27, PMID: 22071034, 10.1016/j.envres.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitman S, Good G, Donoghue E, Benbow N, Shou W, Mou S. 1997. Mortality in Chicago attributed to the July 1995 heat wave. Am J Public Health 87(9):1515–1518, PMID: 9314806, 10.2105/ajph.87.9.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2004. International Statistical Classification of Diseases and Related Health Problems, 10th Revision (Vol. 1). Geneva, Switzerland:World Health Organization. [Google Scholar]
- Wickwire P, Buresh R, Tis L, Collins M, Jacobs R, Bell M. 2012. Comparison of an in-helmet temperature monitor system to rectal temperature during exercise. J Strength Cond Res 26(1):1–8, PMID: 22002518, 10.1519/jsc.0b013e31823b0a5a. [DOI] [PubMed] [Google Scholar]
- Xiang J, Bi P, Pisaniello D, Hansen A. 2014. Health impacts of workplace heat exposure: an epidemiological review. Ind Health 52(2):91–101, PMID: 24366537, 10.2486/indhealth.2012-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]