Abstract
Background:
The 1974 Safe Drinking Water Act (SDWA) regulates public water systems to protect health, but not private wells. State and local government requirements for private well water testing are rare and inconsistent; the responsibility to ensure water safety remains with individual households. Over the last two decades, geogenic arsenic has emerged as a significant public health concern due to high prevalence in many rural American communities.
Objectives:
We build the case for universal screening of private well water quality around arsenic, the most toxic and widespread of common private water contaminants. We argue that achieving universal screening will require policy intervention, and that testing should be made easy, accessible, and in many cases free to all private well households in the United States, considering the invisible, tasteless, odorless, and thus silent nature of arsenic.
Discussion:
Our research has identified behavioral, situational and financial barriers to households managing their own well water safety, resulting in far from universal screening despite traditional public health outreach efforts. We observe significant socioeconomic disparities in arsenic testing and treatment when private water is unregulated. Testing requirements can be a partial answer to these challenges.
Conclusions:
Universal screening, achieved through local testing requirements complemented by greater community engagement targeting biologically and socioeconomically vulnerable groups, would reduce population arsenic exposure greater than any promotional efforts to date. Universal screening of private well water will identify the dangers hidden in America’s drinking water supply and redirect attention to ensure safe water among affected households. https://doi.org/10.1289/EHP629
Background
Water is the basis for life. The United States has a long history of ensuring public access to safe drinking water, which has been key to human health and development. A federal law enacted by Congress in 1974, the Safe Drinking Water Act (SDWA) (U.S. EPA 1974), authorizes the U.S. Environmental Protection Agency (U.S. EPA) to set national drinking water standards to protect against health effects from naturally occurring and man-made contaminants. However, these enforceable maximum contaminant levels (MCLs) only apply to public water systems, not individual private wells. Although nearly people supplied by over 170,000 public water systems benefit from the protection of the SDWA and regular water quality monitoring, approximately mostly rural Americans dependent on private well water, or roughly one in every seven households, do not (Maupin et al. 2014). Therefore, the safety of their drinking water is unknown. The health risks from drinking potentially unsafe well water have caught the attention of the American Academy of Pediatrics (AAP), leading it to publish and to re-affirm a policy statement that recommends annual testing of private well water (AAP 2009).
Among noted microbiological and chemical contaminants of health concern, geologically sourced arsenic stands out for its toxicity and its widespread occurrence in domestic well waters. Exposure to inorganic arsenic in drinking water, even at low-to-moderate levels (), is being recognized as a major environmental health issue (Carlin et al. 2015). Research evidence led the National Research Council (NRC) to conclude in 2001 that arsenic-induced internal cancers should be the focus of arsenic risk assessment and estimated that lifetime risks for bladder and lung cancer at the then new MCL of would be between 12 and 23 per 10,000 people, dependent on sex and type of cancer (NRC 2001). In 2013, the NRC provided an update of evidence for the associations between chronic exposure to arsenic in drinking water and a range of noncancer health effects (NRC 2014): cardiovascular disease, diabetes, nonneoplastic respiratory changes, and negative pregnancy and child development outcomes. Of particular concern is in utero and early life exposure to arsenic, which even at relatively low concentrations impairs intellectual development and increases the risk of adverse health effects later in life.
The U.S. EPA adopted a total arsenic MCL of even though exposure at this level is likely to result in higher than the 1 in a million excess mortality criterion that has been applied when setting drinking water standards for other environmental toxins. Like other carcinogens, the MCL Goal for arsenic is also set to zero; the enforceable MCL was chosen using the U.S. EPA’s discretionary authority to set less stringent standards based on a cost–benefit analysis that ruled out and as being too expensive for small community water utilities to comply. Unsatisfied with a federal MCL that would not provide the level of protection required by state law, New Jersey went further in 2004 by adopting an arsenic MCL of , which remains the most protective in the nation (Christen 2004).
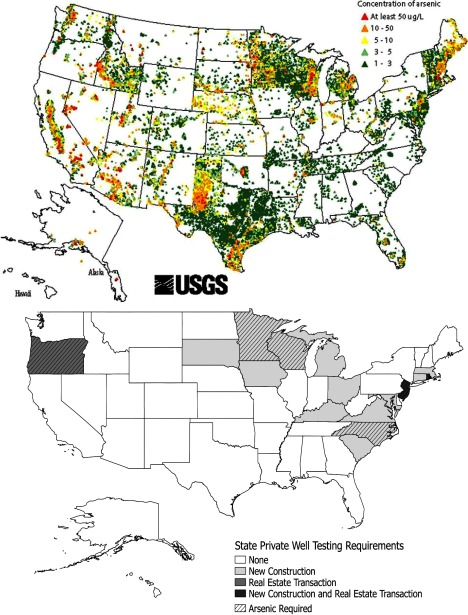
The toxicity of arsenic is concerning given the frequency of its occurrence in well water. Arsenic was detected in 51.4% of 7,580 domestic wells tested nationwide 1986–2001, with 10.6% of wells exceeding the U.S. EPA’s MCL of (Focazio et al. 2006). USGS measurements of arsenic in mostly nonprivate wells (Figure 2) reveal states in New England and the western and south-central United States with particularly high occurrence (Gronberg 2011). Without nationally representative sampling of private well water, the true extent of the population at risk remains unknown. Based on the National Water Quality Assessment (NAWQA) groundwater database (U.S. Geological Survey 2015), the number of households relying on well water, and average household sizes by census division in each state (U.S. Census Bureau 2015), we estimate that Americans may drink from wells with arsenic levels above the federal arsenic MCL and from wells with . Better sampling is needed to improve this estimate but most important for now is to appreciate its magnitude. Although research finds the probability of finding arsenic above MCL in groundwater is governed by a set of hydrogeochemical factors and can increasingly be predicted by geostatistical modeling at regional and local scales, the concentration of arsenic in individual wells can only be determined by a test (Zheng and Ayotte 2015). Given the high degrees of spatial variability whereby neighboring wells are not consistently safe or unsafe, every well must be tested.
Figure 2.
Top: location and arsenic concentration of 31,350 USGS groundwater samples (Gronberg 2011). Bottom: state-level requirements for private well testing, at what occasion, and whether arsenic is included.
As a nation, should we be content with not knowing the extent of water-related health risks and consequences faced by the private well population? Screening, a critical tool widely used in public health for preventative care, can be similarly applied to identify risks associated with unsafe private well water, and followed by actions to improve water quality. Through research into the testing and treatment behaviors of arsenic-affected private well communities, we and others have identified reasons for persistent exposure, along with socioeconomic, situational, and psychological barriers to reducing that exposure (Chappells et al. 2015; Flanagan et al. 2015b). At the same time, we have demonstrated that testing requirements can help alleviate some of these initial barriers and result in exposure reduction (Flanagan et al. 2016a). We argue there is an undeniable case for universal screening of private well water quality as the necessary first step to protecting public health and ensuring the safety of private well water; below, we use the example of arsenic to illustrate why enacting local government testing requirements combined with greater community engagement will be necessary to achieve that goal.
Discussion
Reasons for Persistent Exposure
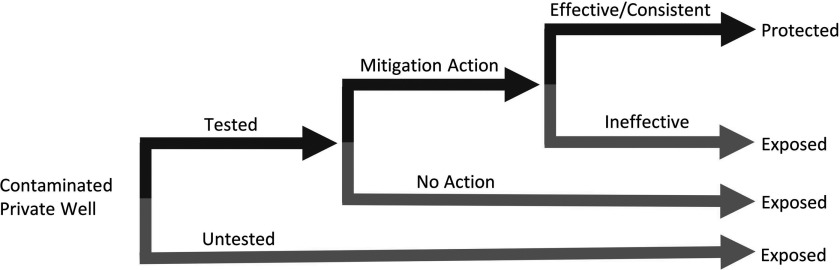
Because the responsibility to ensure water safety continues to fall on private well owners, individual health protective behavior is essential to exposure reduction. We have identified three reasons for persistent arsenic exposure (Figure 1): households a) who are unaware of arsenic in their water because they have not tested; b) who have tested for arsenic but are not taking action to reduce exposure; and c) who have taken action to test and reduce exposure, but remain exposed from inconsistent behavior or failing treatment systems (Zheng and Ayotte 2015). It is important to note that well testing serves as a screening because the act itself does not reduce the exposure without corrective action to follow.
Figure 1.
Reasons for persistent exposure among affected households.
Our recent surveys of about 2,000 randomly selected private well households in arsenic-affected areas of central Maine (Flanagan et al. 2015b) and northern New Jersey (Flanagan et al. 2016a) reveal that more than half of households have never tested their well water for arsenic. We expect this is the case in other areas with frequent arsenic occurrence (Figure 2). For example, only 30% of households in Nevada (Shaw et al. 2005) and only 21% of surveyed private well households in Wisconsin reported having tested for arsenic (Schultz and Malecki 2015). These low testing rates suggest that the largest share of current population exposure to drinking water arsenic comes from households who are unaware of the arsenic in their drinking water (Figure 1).
In the states and towns where attention has been paid to private well water quality as a public health concern, the focus to date has been primarily on motivating well owners to test, assuming that they will subsequently take action on their own to reduce exposure. We find this is largely true. We conducted a follow-up survey of 256 private well households in Maine who had received high arsenic test results during a water sampling program 3–6 y prior (Flanagan et al. 2015a). We found that 43% of households had installed some kind of water treatment, 31% switched to drinking bottled water or took some other mitigation action, but the remaining 27% took no protective action. Common reasons for not taking action included lack of concern and expense of treatment; those with higher arsenic levels were more likely to act. Similarly, among a subset of surveyed New Jersey households with known or reported arsenic problems (), 56% were using some kind of treatment for arsenic, 10% were drinking bottled water, and 34% were not taking any action (Flanagan et al. 2016a). A study of 545 private well households in Wisconsin who participated in a well testing program in 2000 and received results of arsenic found 40% had not taken action (Severtson et al. 2006). Thus, although many households will take action on their own after receiving test results of arsenic above MCL, about a third of households will not to act to reduce exposure.
The third reason for persistent arsenic exposure is when households have tested and taken action to reduce their exposure but their method is not entirely effective. Once a decision has been made to treat water for arsenic, well owners are left to a private sector that is unregulated even though the spent treatment media can be highly toxic. Furthermore, local water treatment providers and homeowners may not have the expertise to handle the technical challenges in correctly installing and maintaining an arsenic treatment system. Although more studies are desirable, we have identified treatment failure as a serious risk: 15% of tested home treatment systems in Maine () (Flanagan et al. 2015a) and 23% of New Jersey treatment systems () (Flanagan et al. 2016b) were failing to produce water below their respective MCLs. In all cases the well owner was unaware of the failure, indicating regular monitoring of treated water quality is rare. In Nevada treated water concentrations exceeded the MCL in 31% of households with reverse-osmosis (RO) systems installed to remove arsenic () (Walker et al. 2008). In Wisconsin the actions taken by 42% of well owners intending to reduce arsenic exposure did not lower the arsenic level to below MCL (Severtson et al. 2006). When households depend on bottled water or point-of-use treatment to reduce their arsenic exposure, consistent behavior change is also required—the occasional use of untreated water for drinking and cooking also contributes to continuing arsenic exposure (Smith et al. 2016; Spayd et al. 2015).
Given low rates of testing, the majority of Americans currently exposed to arsenic through their private drinking water are unaware of their exposure. Households with an arsenic problem are unlikely to be a majority in any local community because the occurrence rate of arsenic in an affected town rarely if ever exceeds 50% of wells and is more likely to be between 10% and 20% (Zheng and Ayotte 2015). Although this explains the difficulty in establishing a social norm for arsenic testing, it also means that those households who face an arsenic problem after testing become a silent minority left to the struggle of maintaining the safety of their drinking water alone. Households failing to install or maintain an effective treatment system remain exposed to arsenic. As well screening identifies more households with problems, remediation will be a continuing challenge for exposure reduction. For some households, the upfront cost of installing an arsenic treatment system can seem prohibitive and does remain a barrier to action (Flanagan et al. 2015a). Linking homeowners to already available, yet often unknown, assistance programs such as the interest-free loans for water treatment of up to over 10 y available in New Jersey, is a start to overcoming these concerns, but more should be done. Several states, such as Florida and New Jersey, already have established funds to support homeowners with remediation of anthropogenic chemical contaminants when the contamination is through no fault of their own. Yet naturally occurring contaminants such as arsenic, which also present risks to residents through no fault of their own, are often explicitly excluded from such programs. Reconsidering these exclusions could greatly contribute to reducing arsenic exposure. A licensing requirement for water treatment professionals that includes handling disposal of hazardous material could also reduce the use of ineffective arsenic treatment methods and exposure risks from the spent media. The advantage of a screening requirement is that public resources and efforts can be redirected towards supporting affected households to effectively reduce their exposure.
Socioeconomic and Biological Vulnerabilities
Through our household surveys we have identified significant disparities in testing behavior and beliefs about testing by socioeconomic status (SES) when private well testing is not required. Ever testing a well and testing for arsenic are both significantly predicted () by income and education in Maine and New Jersey (Flanagan et al. 2016c). This adds a new dimension of environmental justice to exposure reduction. Although the probability to have naturally occurring arsenic in well water is no different for lower income and less-educated households, they are less likely to be aware of the hazard and to take action against it. Further, higher income and better educated households benefit more than lower income and less-educated households from public health interventions intended for the whole community. For example, although town-level testing promotion activities in New Jersey have succeeded in testing more wells for arsenic, they may have exacerbated disparities in testing as higher SES families may be more receptive to risk information and more likely to take advantage of testing programs, even when testing is free (Flanagan et al. 2016b). Better targeting of interventions towards those socioeconomically vulnerable to exposure is needed.
We also see missed opportunities to better protect biologically vulnerable groups among private well households, that is, children and the unborn. At present, pregnant women on private well water are not being advised to test their water for exposure to arsenic. This is worrisome considering evidence for potential damages due to in utero exposure and developmental impacts among children. Exposure is well documented; in Maine arsenic has been detected in 99% of blood samples from children aged 1–6, and at higher levels in areas with a greater prevalence of wells with arsenic (Rice et al. 2010). A recent study found significant reductions in IQ among Maine schoolchildren consuming well water with arsenic compared to those drinking from wells with arsenic (Wasserman et al. 2014). Despite the recommendation of the American Academy of Pediatrics, our surveys find that only 14% of households with children cite their children as a main reason for having tested their well water, indicating that testing recommendation may not be passed along by pediatricians.
Benefits of State and Local Regulations
There is potential for policy to make a significant contribution towards universal screening. Our random household survey in New Jersey was an opportunity to investigate the effects of a policy intervention, the New Jersey Private Well Testing Act (PWTA), which since 2002 has required arsenic testing during real estate transactions. We find that the testing requirement results in identification of significantly more wells with arsenic; the proportion of wells identified by respondents as having an arsenic problem was five times higher among those who faced PWTA requirements (20% vs. 4%), in an area where an estimated 21% of wells exceed MCL (Flanagan et al. 2016a). An added benefit of requiring testing at real estate transaction is that families who purchased houses since the law went into effect in 2002 are younger and disproportionately more likely to include pregnant women and children (Flanagan et al. 2016a), who are particularly vulnerable to arsenic effects. However, such a requirement is not the full answer. Despite more wells being tested under the PWTA, we find post-PWTA well owners are more likely to misremember their arsenic test results, are more likely to not know what kind of treatment they are using, and do not report better maintenance or monitoring of treatment systems, suggesting challenges to reducing exposure remain even when testing is required. Furthermore, in 14 y only a fraction of wells (25%) have been tested under the PWTA due to the slow pace of housing turnover. Therefore, sustained community engagement efforts and additional public resources to support private well testing and follow-up actions among socially and biologically vulnerable groups in particular are still necessary. New Jersey’s database of over 35,000 PWTA well tests for arsenic, geocoded at fine-scale, is now a significant resource for targeting these efforts.
Given the benefits of state and local regulations on private well water, we conducted an Internet search and found that 13 states require water to be tested for at least coliform bacteria when new private wells are constructed; Oregon requires water to be tested during a real estate transaction, and Rhode Island and New Jersey require testing during both occasions (Figure 2). However, only 5 states include arsenic as a parameter in these testing requirements: New Jersey, Oregon, Minnesota, Wisconsin, and North Carolina. Other states have attempted to introduce testing regulations; for example, Vermont passed a private well testing act that was vetoed by its governor, and private well testing bills in New York and Maine never made it out of the state legislatures. Local governments have been more proactive; in 22 states (13 with no known state-wide regulation) we have found examples where local ordinances are stricter than state regulations, requiring testing at specific occasions or even requiring water to meet quality standards prior to its use as a source for drinking. Yet such regulations are still the exception. In their absence the stance of state and local authorities varies, ranging from actively encouraging private well owners to test their water, to remaining hands off and leaving responsibility to the private market and to the individuals who must be aware, willing, and capable to take the actions required to ensure safe drinking water for their household.
The Case for Regulation to Achieve Universal Arsenic Screening
In the absence of regulation, low risk awareness, optimistic beliefs of one’s own risk, and several other perceived or real barriers are persistent obstacles to universal testing of private well water (Flanagan et al. 2015b; Flanagan et al. 2016a; Flanagan et al. 2016c). Even well users generally aware of arsenic risks and the problems in their area display persistent optimistic biases against testing, as observed for other protective behaviors such as radon testing (Weinstein et al. 1988). In our surveys the respondents perceived significantly greater risk that wells in their town are contaminated with arsenic than that their own well is contaminated, regardless of whether they had ever actually tested. Furthermore, we have found that other barriers beyond risk awareness can have a greater effect on testing behavior, including the perceived time and financial costs of testing, the difficulty in finding a well testing service and arranging for a test, not being confident in one’s ability to carry out testing, and forgetting to follow through with a desired test. Cost alone can be a barrier; our follow-up experiment with New Jersey survey respondents found that offering arsenic tests for free to well owners who had not previously tested yielded a greater than three times higher response rate (42% vs. 12%) than offering tests at the market cost of () (Flanagan et al. 2016b). Thus while more effective at generating well tests, the availability of free tests alone will not achieve universal screening.
Given these barriers, we posit that relying on traditional public health outreach and community engagement approaches alone will never achieve universal arsenic screening. In the absence of policy change the status quo will persist and a majority of the population at risk will remain exposed. Periodic testing events can be more effective at generating tests than publicity alone by acting as a trigger for the fraction of households already thinking about arsenic testing, or for those most receptive to well testing but unaware of local arsenic risks, but participation is never universal and sustaining local-level efforts remains a challenge (Renaud et al. 2011; Severtson et al. 2004). Shifting strategies towards regulation and subsidizing tests and treatment for low-income households and families with children will almost certainly have more impact in the long run.
The current patchwork of limited local and state government efforts highlights that much more can be done while providing models for practical and feasible policy actions. If every state at the very least enacted regulations requiring domestic wells be tested during real estate transaction and new construction, eventually universal screening would be achieved. Subsidizing testing based on income would ensure that these requirements are not an undue burden on individuals, as would providing subsidies or interest-free loans for treatment systems when arsenic is found. That this process is a slow one does not mean it is unnecessary. Entrusting and burdening individual households with the responsibility to ensure the safety of their private well water is not a prudent policy choice.
Conclusions
A National Strategy for Universal Well Water Screening
To substantially reduce drinking water exposures and improve health outcomes, more public resources, attention and energy than the current laissez-faire approach to private well water safety will be necessary. Achieving universal screening of private well water will require a renewed focus and new strategies; testing requirements will be a necessary component, as will greater community engagement and support targeted geographically and to the needs of the most socioeconomically and biologically vulnerable. A requirement to test water is not an undue burden, is not costly, and does not infringe on anyone’s privacy. To protect public health, ideally all wells need to be tested so that those with problems, such as households with elevated arsenic, have the opportunity to reduce their exposure and risk of adverse health outcomes. Testing requirements that include arsenic would reduce population exposure among private well households greater than any promotional efforts to date because in most cases those given test results will subsequently take protective actions on their own, it is likely even more may act if additional support is available. The advantage of universal screening is that it will allow community engagement and outreach efforts to move from urging all households to identify potential risks, to supporting affected private well users and linking them to service providers such as treatment companies and testing laboratories to reduce and monitor their actual risks. Universal screening of private well water quality will identify the dangers now hidden in America’s private drinking water supply and redirect attention to ensure safe water among affected households. This is only the first step towards ensuring safe drinking water for private well households in the United States.
Acknowledgments
This research was supported by the U.S. National Institutes of Health’s (NIH) National Institute of Environmental Health Sciences (NIEHS) Superfund Research Program 3 P42 ES10349 and Cooperative Agreement 1 UE2 EH001326-01 by the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, the CDC, or the Department of Health and Human Services. Additional support was provided by the Southern University of Science and Technology Grant Number G01296001.
References
- AAP (American Academy of Pediatrics). 2009. Policy statement: drinking water from private wells and risks to children. Pediatrics 123:e1123–e1137. [DOI] [PubMed] [Google Scholar]
- Carlin DJ, Naujokas MF, Bradham KD, Cowden J, Heacock M, Henry HF, et al. 2015. Arsenic and environmental health: state of the science and future research opportunities. Environ Health Perspect 124(7):890–899, 10.1289/ehp.1510209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappells H, Campbell N, Drage J, Fernandez CV, Parker L, Dummer TJ. 2015. Understanding the translation of scientific knowledge about arsenic risk exposure among private well water users in Nova Scotia. Sci Total Environ 505:1259–1273, PMID: 24444512, 10.1016/j.scitotenv.2013.12.108. [DOI] [PubMed] [Google Scholar]
- Christen K. 2004. New Jersey proposes toughest arsenic standard worldwide. Environ Sci Technol 38:105A, 10.1021/es040419f. [DOI] [Google Scholar]
- Flanagan SV, Marvinney RG, Johnston RA, Yang Q, Zheng Y. 2015a. Dissemination of well water arsenic results to homeowners in Central Maine: influences on mitigation behavior and continued risks for exposure. Sci Total Environ 505:1282–1290, PMID: 24726512, 10.1016/j.scitotenv.2014.03.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan SV, Marvinney RG, Zheng Y. 2015b. Influences on domestic well water testing behavior in a Central Maine area with frequent groundwater arsenic occurrence. Sci Total Environ 505:1274–1281, PMID: 24875279, 10.1016/j.scitotenv.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan SV, Spayd S, Procopio N, Chillrud SN, Braman S, Zheng Y. 2016a. Arsenic in private well water part 1 of 3: impact of the New Jersey Private Well Testing Act on household testing and mitigation behaviors. Sci Total Environ 562:999–1009, PMID: 27118151, 10.1016/j.scitotenv.2016.03.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan SV, Spayd SE, Procopio NA, Chillrud SN, Ross J, Braman S, et al. 2016b. Arsenic in private well water part 2 of 3: who benefits most from traditional testing promotion? Sci Total Environ 562:1010–1018, PMID: 27142115, 10.1016/j.scitotenv.2016.03.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan SV, Spayd SE, Procopio NA, Marvinney RG, Smith AE, Chillrud SN, et al. 2016c. Arsenic in private well water part 3 of 3: socioeconomic vulnerability to exposure in Maine and New Jersey. Sci Total Environ 562:1019–1030, PMID: 27118035, 10.1016/j.scitotenv.2016.03.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Focazio MJ, Tipton D, Dunkle Shapiro S, Geiger LH. 2006. The chemical quality of self-supplied domestic well water in the United States. Ground Water Monit Remediat 26:92–104, 10.1111/j.1745-6592.2006.00089.x. [DOI] [Google Scholar]
- Gronberg JAM. 2011. Map of Arsenic Concentrations in Groundwater of the United States, 2nd ed. Reston, VA:U.S. Geological Survey. [Google Scholar]
- Maupin MA, Kenny JF, Hutson SS, Lovelace JK, Barber NL, Linsey KS. 2014. Estimated Use of Water in the United States in 2010. Reston, VA:U.S. Geological Survey. [Google Scholar]
- NRC (National Research Council). 2001. Arsenic in Drinking Water 2001 Update. Washington, DC:National Academies Press. [Google Scholar]
- NRC. 2014. Critical Aspects of EPA's IRIS Assessment of Inorganic Arsenic: Interim Report. Washington, DC:National Academies Press. [Google Scholar]
- Renaud J, Gagnon F, Michaud C, Boivin S. 2011. Evaluation of the effectiveness of arsenic screening promotion in private wells: a quasi-experimental study. Health Promot Int 26(4):465–475, PMID: 21393299, 10.1093/heapro/dar013. [DOI] [PubMed] [Google Scholar]
- Rice DC, Lincoln R, Martha J, Parker L, Pote K, Xing S, et al. 2010. Concentration of metals in blood of Maine children 1–6 years old. J Expo Sci Environ Epidemiol 20:634–643, 10.1038/jes.2010.42. [DOI] [PubMed] [Google Scholar]
- Schultz A, Malecki K. 2015. Reducing human health risks from groundwater: estimating private well testing behaviors and water use among private well owners in Wisconsin. Report to the Groundwater Coordinating Council. Department of Natural Resources Grant #221. October 15, 2015.
- Severtson DJ, Baumann LC, Brown RL. 2006. Applying a health behavior theory to explore the influence of information and experience on arsenic risk representations, policy beliefs, and protective behavior. Risk Anal 26(2):353–368, 10.1111/j.1539-6924.2006.00737.x. [DOI] [PubMed] [Google Scholar]
- Severtson D, Baumann L, Shepard R. 2004. A utilization-focused and theory-based evaluation of an arsenic well testing program. In: Proceedings of the Best Education Practices (BEPs) Symposium for Water Outreach Professionals: Defining BEPs, Refining New Resources and Recommending Future Actions 2–4 June 2004 Symposium. University of Wisconsin-Madison; Madison, Wisconsin:University of Wisconsin, 269. [Google Scholar]
- Shaw WD, Walker M, Benson M. 2005. Treating and drinking well water in the presence of health risks from arsenic contamination: results from a U.S. hot spot. Risk Anal 25(6):1531–1543, 10.1111/j.1539-6924.2005.00698.x. [DOI] [PubMed] [Google Scholar]
- Smith AE, Lincoln RA, Paulu C, Simones TL, Caldwell KL, Jones RL, et al. 2016. Assessing arsenic exposure in households using bottled water or point-of-use treatment systems to mitigate well water contamination. Sci Total Environ 544:701–710, PMID: 26674699, 10.1016/j.scitotenv.2015.11.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spayd SE, Robson MG, Buckley BT. 2015. Whole-house arsenic water treatment provided more effective arsenic exposure reduction than point-of-use water treatment at New Jersey homes with arsenic in well water. Sci Total Environ 505:1361–1369, PMID: 24975493, 10.1016/j.scitotenv.2014.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2015. 2013 Housing Profile: United States AHS/13-1. (American Housing Survey Factsheets). Washington, DC:U.S. Census Bureau.
- U.S. EPA (U.S. Environmental Protection Agency). Summary of the Safe Drinking Water Act. 1974. https://www.epa.gov/laws-regulations/summary-safe-drinking-water-act [accessed 31 May 2017].
- U.S. Geological Survey. 2015. USGS National Water Quality Assessment (NWQA). http://cida.usgs.gov/nawqa_queries_public/jsp/gwmaster.jsp [accessed 28 October 2015].
- Walker M, Seiler RL, Meinert M. 2008. Effectiveness of household reverse-osmosis systems in a Western U.S. region with high arsenic in groundwater. Sci Total Environ 389:245–252, PMID: 17919687, 10.1016/j.scitotenv.2007.08.061. [DOI] [PubMed] [Google Scholar]
- Wasserman G, Liu X, Loiacono NJ, Kline J, Factor-Litvak P, van Geen A, et al. 2014. A cross-sectional study of well water arsenic and child IQ in Maine schoolchildren. Environ Health 13:23, 10.1186/1476-069X-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND, Klotz ML, Sandman PM. 1988. Optimistic biases in public perceptions of the risk from radon. Am J Public Health 78(7):796–800, PMID: 3381955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Ayotte JD. 2015. At the crossroads: hazard assessment and reduction of health risks from arsenic in private well waters of the northeastern United States and Atlantic Canada. Sci Total Environ 505:1237–1247, PMID: 25466685, 10.1016/j.scitotenv.2014.10.089. [DOI] [PMC free article] [PubMed] [Google Scholar]