Abstract
Innovative approaches are needed to increase engagement in HIV treatment and prevention services, particularly in HIV hotspots. Here, we detail our design, training approach, and early implementation experiences with a community-based HIV intervention called “Health Scouts”. The intervention, utilizing a novel theory-based approach, trained 10 community residents in an HIV hotspot fishing community to use motivational interviewing strategies and a mobile phone-based counseling application. During the first three months, 771 residents (median 82/Health Scout, range 27–160) were counseled. A directly observed Motivational Interviewing Treatment Integrity scale-based evaluation found adequate performance (median score 20 out of 25, range 11–23). The Health Scout intervention was feasible to implement in a high HIV prevalence fishing community, and its impact on HIV care outcomes will be evaluated in an ongoing cluster-randomized trial. If found to be effective, it may be an important strategy for responding to HIV in high burden settings.
Keywords: HIV, community health workers, motivational interviewing, antiretroviral therapy, mHealth
Introduction
Innovative approaches are needed to increase HIV treatment and prevention service uptake and adherence, particularly in high HIV prevalence hotspots. In Uganda, the overall national HIV prevalence is ~7.4%; however, HIV prevalence is as high as 43% in some fishing communities on Lake Victoria.1 The complex social-structural nature of these fishing communities, which includes dangerous work conditions, mobile populations, high rates of sex work, alcohol use, drug use, and fatalism, has created challenging environments in which to prevent and treat HIV.2
PEPFAR, UNAIDS, and WHO have recognized the importance of HIV transmission in hotspots and made them a priority of their HIV response action frameworks.3,4 The Ugandan Ministry of Health has also designated fisherfolk as a key population in their national guidelines and recommended treatment regardless of CD4 count.5 However, there is limited rigorous evidence on effective strategies for implementing and sustaining HIV treatment and prevention services for hotspots, making this is a priority research need.6
We designed a community-based intervention to promote HIV treatment and prevention services in one of the largest and highly HIV prevalent fishing communities in Uganda. The intervention utilized a novel, theory-based approach that enabled community health workers (CHWs), called “Health Scouts”, to leverage motivational interviewing (MI) strategies and mobile health technology (mHealth) tools. This paper describes our experience designing and evaluating the initial implementation of the Health Scout intervention as part of an ongoing cluster-randomized trial.
Methods
Study Setting
The study setting is a Lake Victoria fishing community (area ~2km2, adolescent/adult population ~4400) in Rakai District in south-central Uganda. Rakai is bordered to the south by Tanzania and to the east by Lake Victoria. Rakai has two primary highways, one highway connecting Kampala (capital of Uganda) to Tanzania and the Trans-African Highway which connects Kampala to the Democratic Republic of Congo. The fishing community is ~235 km from Kampala and is accessed via an untarmacked road off of the Kampala-Tanzania highway. The intervention is being implemented and supervised by staff from the Rakai Health Sciences Program (RHSP), a well-established community-based HIV research and health services organization.
Cluster-Randomized Trial Overview
The Health Scout intervention is being tested in an ongoing cluster-randomized trial called mLAKE (mHealth Lakefolk Actively Keeping Engaged) which is registered on ClinicalTrials.gov (NCT02556957). For this trial, the fishing community was divided into 40 clusters which were randomized, with 20 clusters allocated to the Health Scout intervention arm and 20 clusters to the standard-of-care, control arm (see Figure 1). The intervention began September 2015, and follow-up is planned until 2018. This paper reports on a process-focused evaluation of the initial three months of implementation which was conducted to assess intervention fidelity so that, if needed, modifications could be made early in the course of the trial.
Figure 1.
Example mLAKE Trial Cluster Map (Intervention-Red, Control-Grey)
Health Scout Intervention Description
Conceptualization
The general approach to the design and implementation of the Health Scout intervention was pragmatically-oriented.7 That is, a general framework for Health Scout recruitment, training, tasks, quality assurance, and monitoring was developed, but the intervention was allowed flexibility to adapt to the needs, constraints, and secular changes of the setting during implementation. The general framework included the following core components: (i) CHW (Health Scout)-based delivery; (ii) counseling using MI strategies; (iii) home-based; (iv) mHealth-supported.
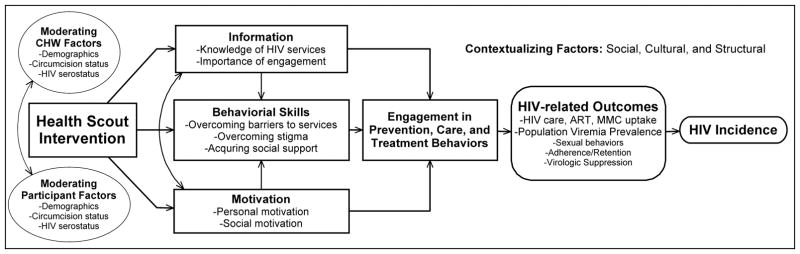
The Health Scout intervention was informed by formative mixed methods research carried out in Rakai fishing communities and a broader literature review. A situated Information, Motivation, and Behavioral Skills (sIMB) theory-based conceptual framework was developed whereby Health Scouts would promote relevant information, motivation, and behavioral skills to improve clients’ engagement in HIV treatment and prevention services, ultimately leading to improved HIV-related outcomes and decreased HIV incidence (Figure 2).8 The intervention was “situated” by Health Scout training which took into consideration the social, cultural, and structural environment and incorporated MI strategies. An mHealth application, which tailored counseling to individual contextual considerations, was an additional situating element. Moderating factors which might influence the impact of the Health Scouts were also considered, e.g. differential impact of males counseling males versus females.
Figure 2.
Health Scout Intervention Conceptual Framework
Health Scout Tasks
Using the conceptual framework, specific Health Scout tasks were outlined. Health Scouts were to attempt to visit all households within their clusters within 3 months of study initiation and follow-up with each “client” within their cluster every 3 months for ~3 years. Eligible clients for counseling were any persons age ≥15 years. During each visit, Health Scouts would counsel clients with assistance from an mHealth application on a smartphone. The application included an individual risk screener and tailored MI-informed counseling modules on HIV treatment and prevention based on the client’s needs and current health status. Health Scouts would provide psychosocial support, encouragement, information, and education, and troubleshoot barriers to HIV service uptake and adherence. Each Health Scout would be assigned two clusters which together contained ~215 potential eligible clients. Visits were anticipated to take ~30–45 minutes each.
Eligibility of Health Scouts
To become a Health Scout, individuals needed to have 7+ years of education, be literate, and know their HIV status. Male HIV-negative Health Scouts had to be circumcised, and HIV-infected Health Scouts needed to be actively engaged in care.
Community Sensitization and Health Scout Recruitment
Approximately 15 community leaders, such as boat owners and prominent business owners (e.g. landlords), were convened in a meeting by RHSP study staff through personal invitations and sensitized to the Health Scout intervention and mLAKE study. A subsequent meeting was held with about 30 potential Health Scout candidates, both self-identified and identified through community leaders. A vote was conducted by these candidates amongst themselves. The 10 individuals who received the most votes were selected as Health Scouts and the 5 remaining individuals were named as alternates.
Training Program
The conceptual framework was used to design a training program which included mHealth application/smartphone use, confidentiality, disclosure, MI-informed interaction strategies, HIV-related knowledge, mock counseling role play, cluster boundary walk-throughs, and filling out home visit forms. A detailed training manual for Health Scouts was also produced. Peer mentoring during training was encouraged. Initial training consisted of four days of classroom work and one day of field activities. Training activities were led by a multidisciplinary team of RHSP staff and members of the Johns Hopkins University study team.
Incorporation of Motivational Interviewing (MI) Principles
MI is a communication strategy that takes considerable time, practice and ongoing supervision to achieve optimal performance.9 However, given its effectiveness in behavioral change and cross cultural application, we elected to incorporate basic MI principles into the Health Scout training. Central to the MI-informed training was to describe, discuss, and model the fundamental importance of a nonjudgmental, non-confrontational approach that invites and guides the client to consider behavior change. The Health Scout role was described as a warm, empathic, and respectful “partnership” to help the client identify strengths, barriers, and facilitators to engaging in HIV treatment or prevention. To develop this dialogue, four strategies were taught: open-ended questions, affirmations, reflections, and summaries. We incorporated exercises described in the MI training manual such as differential effects of using close- versus open-ended questions, modeling by study staff, and role plays of potential client situations.10
Health Scout Smartphone Application and Web Dashboard
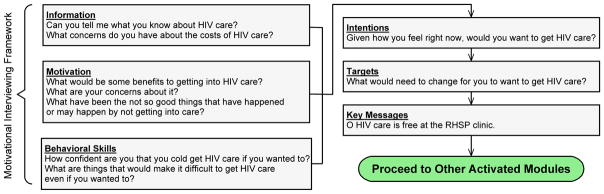
The custom-designed Health Scout smartphone application functioned as a decision support tool to guide Health Scouts through the sIMB-model informed counseling session (emocha Mobile Health Inc., Baltimore, MD). Using simple forms (see Figure 3), the application takes the Health Scout through 3 steps: (1) Household screening-household members are screened for eligibility; (2) Individualized triage-individual household members are asked a series of triage screening questions, e.g. age, gender, HIV status; and, (3) MI Counseling-using responses provided during the individualized triage, tailored counseling modules with MI-informed prompts and messages are provided for the Health Scout to review with the client.
Figure 3.

Example Screenshots from Health Scout Application.
The application, which incorporated guided, collaborative dialogues composed of open-ended questions and exploration of pros and cons of engagement in care, was meant to further incorporate MI principles and provide Health Scouts with the necessary prompts to successfully complete MI-informed counseling sessions. Application queries were tailored to potential replies by clients allowing the Health Scouts to provide the necessary direction and structure that is consistent with MI counseling style. The application also provided a standardized MI-informed counseling approach across the Health Scouts. The application contained 9 tailored counseling modules as shown in Table 1. Figure 4 provides a schematic of the content for the counseling module for someone who knows they are HIV-positive, but is not yet in care.
Table 1.
Health Scout Application Counseling Modules.
| # | Module description |
|---|---|
| 1 | HIV serostatus unknown or no recent HIV test, male or not pregnant female |
| 2 | HIV serostatus unknown or no recent HIV test, pregnant female |
| 3 | Male, not circumcised |
| 4 | HIV+, not in care |
| 5 | HIV+, in care, not on ART |
| 6 | HIV+, on ART |
| 7 | HIV+, pregnant |
| 8 | Male having condomless sex |
| 9 | Female having condomless sex |
Figure 4.
Example of Counseling Module Content: HIV-positive, Not in Care.
Application development followed the principles of agile software development--a method that emphasizes flexibility, pragmatism, and iterative testing.11 The study team and software developers held several requirement specification meetings and maintained regular communication during the application development and testing process to identify and address bugs and make improvements to the content and flow of the application. Health Scouts contributed suggestions to improve usability prior to the official start of the trial.
A browser-based dashboard was developed in conjunction with the mobile application. The dashboard provides secure access to the mobile phone data as well as analytic tools to aid in implementation, monitoring, and evaluation. Analytic features include tools to track the geographic location, number, and timing of counseling visits, as well as visual and quantitative summaries of client responses (Figure 5).
Figure 5.
Example Screenshots from Web Dashboard: (1) Map of Health Scout Visits (2) Summary Figures of Clients’ Responses.
Support/Compensation
Health Scouts were provided with a mobile phone, airtime, backpacks, and uniforms. Health Scouts were also provided a modest base compensation and could earn additional compensation based on the number of participants visited. Average total compensation for Health Scouts was about 1 USD per day.
Run-In and Initial Implementation Process Evaluation
Health Scout competency was assessed using multiple methods. To ensure they understood the boundaries of their assigned clusters, the study team observed Health Scouts as they independently walked along their clusters’ boundaries. Study staff observed and critiqued Health Scout performance in role playing exercises, with a focus on their ability to adhere to the MI-approach. Staff accompanied Health Scouts on their initial client visits. Staff observed Health Scouts as they approached clients, described the study, obtained oral consent, navigated the smartphone application, and completed the necessary documentation for client visits. The team noted deficiencies and provided individualized feedback and additional training as necessary.
As a run-in period, Health Scouts counseled ten clients in week one and debriefed and trouble-shooted with the study team prior to further counseling. After the run-in period, two RHSP study staff also observed and formally evaluated one counseling session per Health Scout. The evaluation included a checklist to document successful completion of each Health Scout task, from proper greeting to application use and visit form completion. The evaluation also included a modified MITI 3.1.1 scale, an evaluation instrument used to provide structured feedback to interviewers on their use of MI.12 The MITI is the most widely used MI fidelity instrument and has demonstrated reliability as well as concurrent and predictive validity. Counselor-client interactions are rated on an objective five-point Likert scale evaluating the following MI domains: Evocation, Collaboration, Autonomy/Support, Direction, and Empathy.12 An average score of 3.5–4.0 indicates beginning proficiency and >4.0 indicates competency. The number of visits Health Scouts had completed during the initial three-month period were also analyzed descriptively.
Supervision and Continuing Education
After deployment, RHSP staff conducted ongoing training and supervision, which included regular in-person follow-ups with the Health Scouts and the development of brief group and/or individualized trainings as needed. RHSP staff were also available via mobile phone to troubleshoot problems with the smartphone, the counseling application, or to answer general questions about study protocols.
On-Going Community Sensitization
Before deployment of the Health Scouts, the RHSP health education and community mobilization team conducted three informational public drama shows in the fishing community. These drama shows used music, short plays, and role modeling to inform the study community about the purpose of the Health Scouts as well as the parent study.
Results
During the first three months of the Health Scout intervention implementation, 771 community residents (median 82 per Health Scout, range 27–160) were approached and successfully counseled. This number was below the initial goal of ~215 client visits by each Health Scout within the first three months of implementation. However, due to the run-in period, interruptions for further training. and technical troubleshooting, Health Scouts were not fully deployed and recruiting clients during significant periods of the initial start-up phase. Additionally, clients were often not at home during attempted visits due to high mobility and varied work hours.
The MITI results for 9 of the 10 Health Scouts are shown in Table 2. Health Scouts completing the MITI evaluation mostly demonstrated beginning proficiency in most domains with a mean composite score of 18.6 out of 25 (median 20, range 11–23). One MITI evaluation was not completed because the Health Scout was unable to properly conduct basic smartphone and visit tasks and was subsequently replaced by an alternate candidate. All Health Scouts successfully identified their cluster boundaries.
Table 2.
Health Scout MITI Scale Performance (n=9).*
| Domain | Mean | Range |
|---|---|---|
| Evocation | 3.7 | 2–5 |
| Collaboration | 3.4 | 2–4 |
| Autonomy/Support | 4.2 | 3–5 |
| Direction | 3.6 | 2–5 |
| Empathy | 3.7 | 2–5 |
| Composite Score | 18.6 | 11–23 |
Five-point Likert scale with higher scores indicating greater integrity with MI principles; maximum score of 25.
Key additional training needs that arose from these evaluations was the need for additional guidance on using the smartphone application. Health Scouts also needed assistance with building rapport with clients, and gaining community trust. Some Health Scouts who did not perform as well had difficulty balancing phone use and counseling and didn’t exhibit a full understanding of MI principles during their sessions. These Health Scouts primarily read straight from the mobile application prompts and didn’t give clients an opportunity to take control of their own health. These issues were addressed with Health Scouts individually following their evaluation session as well as with group-based continuing education sessions.
Discussion
This paper describes the design, implementation, and initial process evaluation of the Health Scouts, a novel, community-based intervention for HIV treatment and prevention. Health Scouts were successfully trained to beginning proficiency in MI-informed counseling through a multi-faceted program and were able to complete counseling sessions with a substantial number of clients. However, a number of deficiencies and wide variability in Health Scout performance signal the need for continued supervision, training, and support for this intervention to fulfill its potential.13
Several important lessons were learned from this study. First, community residents, most of whom had never used a smartphone before, can be recruited and trained to use a smartphone application to provide MI-style counseling in a very challenging and remote setting. Key to accomplishing this was a flexible, multi-method training approach.14 Role play, proficiency testing, peer mentoring, regular feedback sessions, and direct observations were incorporated into the Health Scout training process. On a cautionary note, a minority of the Health Scouts demonstrated marginal proficiency, an indication of how challenging it can be to rapidly train lay counselors to an acceptable standard.15 These individuals likely need additional support or eventual replacement if they are unable to achieve proficiency.16 More stringent selection criteria and verification of candidates’ credentials may also be helpful. Turnover of Health Scouts and a trial run-in period should be considered in similar programmatic deployments.
The development of an evaluation form that utilized the standardized MITI scale outlined expected performance targets and helped increase Health Scouts’ awareness and understanding of expectations. The creation of specific behavioral benchmarks for proficiency as well as for probation or dismissal helped to establish concrete and transparent standards. MITI scales, adapted to local settings, may be a useful tool for training and evaluation of MI approaches in international settings.15 The MITI was originally developed and used for evaluation in resourced settings after several MI training sessions with proficient counselors. The beginning proficiency achieved by most of the Health Scouts appears to be a reasonable level of achievement given the comparatively less intense training they received.
This study had a number of limitations. This study describes the initial implementation of this intervention; therefore it is unknown how relevant the findings will be to outcomes later in the study. However, we felt it was critical to evaluate early intervention fidelity to ensure that it was being implemented as originally intended. Future evaluations will consist of formal mixed methods, incorporating individual and population-level outcomes, qualitative methods, and detailed process evaluations.
In conclusion, initial implementation of a community-based HIV treatment and prevention intervention in a hotspot fishing community was feasible and modestly successful. The impact of this intervention on HIV care outcomes will be evaluated over the ensuing trial follow-up period. If found to be effective, this may be an important strategy for the HIV response in high burden settings.
Acknowledgments
We thank the Health Scouts and the participants of the Rakai Community Cohort Study (RCCS) and mHealth Lakefolk Actively Keeping Engaged (mLAKE) Study.
Funding
The author(s) received the following financial support for the research, authorship, and/or publication of this article: Funding for this research was contributed from grants from the National Institute of Mental Health (R01MH107275), Division of Intramural Research, National Institute for Allergy and Infectious Diseases, and Johns Hopkins University Center for AIDS Research (P30AI094189).
Footnotes
Declaration of Conflicting Interests
emocha Mobile Health Inc. is the company which developed and supported the phone application used in this protocol. LC is entitled to royalties on certain non-research revenue generated by this company and own company equity. Specific to this study, LC has and will receive no royalties or compensation from emocha Mobile Health Inc.. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies. All other study team members declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Chang LW, Grabowski MK, Ssekubugu R, et al. Heterogeneity of the HIV epidemic in agrarian, trading, and fishing communities in Rakai, Uganda: an observational epidemiological study. Lancet HIV. 2016;3(8):e388–96. doi: 10.1016/S2352-3018(16)30034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seeley JA, Allison EH. HIV/AIDS in fishing communities: challenges to delivering antiretroviral therapy to vulnerable groups. AIDS Care. 2005;17(6):688–97. doi: 10.1080/09540120412331336698. [DOI] [PubMed] [Google Scholar]
- 3. [accessed August 18, 2015];PEPFAR 3.0. http://www.pepfar.gov/documents/organization/234744.pdf.
- 4.Focus on location and population. UNAIDS; 2015. World AIDS Day 2015 Report. [Google Scholar]
- 5.Uganda AIDS Commission. HIV and AIDS Uganda Country Progress Report. 2013 [Google Scholar]
- 6.Tanser F, de Oliveira T, Maheu-Giroux M, Barnighausen T. Concentrated HIV subepidemics in generalized epidemic settings. Curr Opin HIV AIDS. 2014;9(2):115–25. doi: 10.1097/COH.0000000000000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ. 2015;350:h2147. doi: 10.1136/bmj.h2147. [DOI] [PubMed] [Google Scholar]
- 8.Rivet Amico K. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. Journal of health psychology. 2011;16(7):1071–81. doi: 10.1177/1359105311398727. [DOI] [PubMed] [Google Scholar]
- 9.Miller WR, Rollnick S. Motivational Interviewing. New York: Guilford; 1991. [Google Scholar]
- 10.Motivational Interviewing Training New Trainers Manual: Motivational Interviewing Network of Trainers. 2014 [Google Scholar]
- 11.Dybå T, Dingsøyr T. Empirical studies of agile software development: A systematic review. Information and Software Technology. 2008;50(9–10):833–59. [Google Scholar]
- 12.Moyers T, Martin T, Manuel J, Hendrickson S, Miller W. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005:28. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Foster AA, Tulenko K, Broughton E. Monitoring and Accountability Platform for national governments and global partners In developing, implementing, and managing CHW programs Global Health Workforce Alliance. 2013 [Google Scholar]
- 14.Dewing S, Mathews C, Schaay N, Cloete A, Simbayi L, Louw J. Improving the counselling skills of lay counsellors in antiretroviral adherence settings: a cluster randomised controlled trial in the Western Cape, South Africa. AIDS Behav. 2015;19(1):157–65. doi: 10.1007/s10461-014-0781-4. [DOI] [PubMed] [Google Scholar]
- 15.Evangeli M, Engelbrecht SK, Swartz L, Turner K, Forsberg L, Soka N. An evaluation of a brief motivational interviewing training course for HIV/AIDS counsellors in Western Cape Province, South Africa. AIDS Care. 2009;21(2):189–96. doi: 10.1080/09540120802002471. [DOI] [PubMed] [Google Scholar]
- 16.Dewing S, Mathews C, Cloete A, et al. From research to practice: lay adherence counsellors’ fidelity to an evidence-based intervention for promoting adherence to antiretroviral treatment in the Western cape, South Africa. AIDS Behav. 2013;17(9):2935–45. doi: 10.1007/s10461-013-0509-x. [DOI] [PubMed] [Google Scholar]