Abstract
Introduction
A number of locations have been considering sugar-sweetened beverage point of purchase warning label policies to help address rising adolescent overweight and obesity prevalence.
Methods
To explore the impact of such policies, in 2016 detailed agent-based models of Baltimore, Philadelphia, and San Francisco were developed, representing their populations, school locations, and food sources, using data from various sources collected between 2005 and 2014. The model simulated, over a 7-year period, the mean change in BMI and obesity prevalence in each of the cities from sugar-sweetened beverage warning label policies.
Results
Data analysis conducted between 2016 and 2017 found that implementing sugar-sweetened beverage warning labels at all sugar-sweetened beverage retailers lowered obesity prevalence among adolescents in all three cities. Point of purchase labels with 8% efficacy (i.e., labels reducing probability of sugar-sweetened beverage consumption by 8%) resulted in the following percentage changes in obesity prevalence: Baltimore: −1.69% (95% CI= −2.75, −0.97, p<0.001); San Francisco: −4.08% (95% CI= −5.96, −2.2, p<0.001); Philadelphia: −2.17% (95% range= −3.07, −1.42, p<0.001).
Conclusions
Agent-based simulations showed how warning labels may decrease overweight and obesity prevalence in a variety of circumstances with label efficacy and literacy rate identified as potential drivers. Implementing a warning label policy may lead to a reduction in obesity prevalence. Focusing on warning label design and store compliance, especially at supermarkets, may further increase the health impact.
INTRODUCTION
Given evidence that sugar-sweetened beverage (SSB) consumption contributes to childhood obesity, several locations are considering legislative strategies to reduce the consumption of SSBs.1–4 In the spring of 2015, San Francisco passed an ordinance mandating the placement of SSB warning labels.5 Similarly, Baltimore and Philadelphia leaders have made curbing SSB consumption a priority as evidenced by a previous bill proposing point of purchase SSB warning labels in Baltimore and the recent passage of an SSB tax in Philadelphia.6 Although the specific efficacy of SSB warning labels (i.e., its impact in reducing the probability of SSB consumption) is not known and may vary from person to person and neighborhood to neighborhood, several studies have suggested that the efficacy may fall in the 6%–19% range.6–10
With SSB warning labels currently under consideration in multiple cities, decision makers cannot wait for results from long-standing observational and intervention studies and would benefit immediately from a clear understanding of the potential measurable range of benefits resulting from such a policy. Testing SSB warning labels on a meaningfully large scale requires considerable time, effort, and resources. Even though emerging research suggests that labels do influence behavior, the downstream impact on obesity can take years to manifest. Moreover, decision makers may want to know how different location-specific factors and roll-out strategies may affect the policy’s impact.
Computational simulation modeling can help overcome these challenges by serving as a virtual laboratory to explore an intervention’s complex potential impact. The class of simulation modeling used here is agent-based modeling, where individuals are represented by computational agents that have autonomous decision-making abilities and complex emergent behavior.11–13 Agent-based models for three cities that have considered or implemented policies to curb SSB consumption are developed: Baltimore, Philadelphia, and San Francisco. Each model includes adolescents in their food environments. Study results may help stakeholders understand how such a mandate would affect adolescent SSB consumption, BMI, and obesity and overweight prevalence.
METHODS
Study Population
The modeling software platform, Virtual Population for Obesity Prevention (VPOP), was developed in 2016 using the programming language Python.14 VPOP is an agent-based model that includes geospatially explicit virtual representations of adolescents, their households, schools, and food and beverage sources (supermarkets, corner store/small grocers, convenience stores, sit-down restaurants, and fast food/carry outs; Figure 1). The location of each individual came from a previously described synthetic population that used an extended iterative proportional fitting method to generate a synthesized, geospatially explicit, human agent database from a variety of census files and represents the U.S. population.14–17
Figure 1.
Model diagram.
Notes: Illustrative representation of food store availability to agents in their environment. Pr(eating) = probability that agent eats at location type; Pr(SSB) = probability that agent consumes an SSB from location type. Letter following agent characteristics, Pr(eating) and Pr(SSB) corresponds to references for these values in Table 1.
Each agent possesses the following characteristics: gender, race and ethnicity, household assignment, school assignment, height, and lean and fat tissue masses (attribute statistics summarized in Appendix Table 1). Lean and fat mass tissue was calculated by the Rahmandad et al.18 metabolic model equations which converted agent’s weights from National Health and Nutrition Examination Survey (NHANES; 2013–2014) into lean and fat mass.
For each simulated day, each agent begins the day at home and proceeds to move throughout the virtual city to school and other locations, making decisions for meals and snacks. Agents have the opportunity to consume breakfast and lunch either at home or school, one snack from home, school, or a retail location, and lastly, dinner and two snacks from either home or a nearby retail location. The choices are made according to probabilities correlated with each location’s attractiveness and inversely proportional to the location’s geographic distance squared.
Of primary interest to this study, each adolescent has the opportunity to consume an SSB with each meal or snack. The choice of whether or not to consume an SSB at a particular meal is made according to probabilities determined from surveys of adolescent behavior. At home, agents may consume SSBs if the family chose to buy them from supermarkets. For this study, SSBs are defined as a unit of 150 calories, determined by averaging calorie composition of various SSBs, weighted by their contribution to total calories from SSBs among adolescents.19,20
Measures
Each agent includes an embedded metabolic model specific to their gender, weight, and age, which converts daily caloric intake and expenditure into a corresponding change in weight.21 Each agent’s metabolic model is adapted from a dynamic mathematical model developed by Hall and colleagues.21 Appendix File 1 provides a more detailed description of the weight change algorithm. Besides SSB consumption, their other daily food and beverage consumption, and physical activity tends to maintain their BMI percentile. The following formula calculates BMI: weight (kg) divided by height squared (m2). Standard Centers for Disease Control and Prevention recommended BMI percentile ranges were used to define overweight and obesity (overweight: BMI ≥ 85th percentile and <95th percentile for adolescents of same age and sex; obesity: a BMI ≥95th percentile for adolescents of same age and sex.)
Each adolescent agent in the synthetic population has city-specific sociodemographic characteristics including age, race, gender, household locations, and school assignment (Table 1, and cross-referenced in Figure 1). Each youth’s height and weight were sampled from youth with matching demographics from the 2013–2014 NHANES dataset.
Table 1.
Summary of Input Source Data
| Category | Source | Year |
|---|---|---|
| Agent characteristics | ||
| Gender | U.S. Census Bureau. American Community Survey, Response Rates. www.census.gov/acs/www/methodology/sample-size-and-data-quality/response-rates/. | 2010 |
| Race | U.S. Census Bureau | 2010 |
| Household location | U.S. Census Bureau | 2010 |
| School assignment | Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. DHHS, CDC, 2013. | 2010–2011 |
| Height, weight | National Health and Nutrition Examination Survey Data. NCHS, editor. Hyattsville, MD: U.S. DHHS, CDC, 2013–2014. | 2013–2014 |
| Food sources | ||
| Locations | Reference USA | 2011 |
| Pr(eating at location) | National Health and Nutrition Examination Survey Data. NCHS, editor. Hyattsville, MD: U.S. DHHS, CDC; 2010–2012. | 2010–2012 |
| Pr(purchasing SSB at location) | National Health and Nutrition Examination Survey | 2010–2012 |
| Validation | ||
| Derived obesity prevalence (Baltimore) | Baltimore City: Demographics and Social Determinants of Health (2005–2009). Maryland Department of Health and Mental Hygiene. | 2005–2009 |
| Derived overweight and obesity rate (SF) | Babey SH, Wolstein J, Diamant AL, Bloom A, Goldstein H. Overweight and Obesity among Children by California Cities–2010. UCLA Center for Health Policy Research and California Center for Public Health Advocacy, 2012. | 2010 |
| Derived overweight and obesity rate (Philadelphia) | Overview of Chronic Disease and Healthy Eating and Active Living Indicators for Philadelphia Adults and Children, 2011. www.phila.gov/health/pdfs/Philadelphia_obesity_chronic_disease812.pdf. | 2011 |
| Daily energy intake from SSBs | Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98(1):180–188. https://doi.org/10.3945/ajcn.112.057943. | 1999–2010 |
Retail food source locations came from a commercially available dataset, ReferenceUSA, categorized using standard industrial classification codes. Supermarkets were further subclassified from retail grocery standard industrial classification codes to match known supermarket chains.22 Consumption behavior from NHANES was used to assign the proportion of the population that consumes SSBs on a daily basis (Table 1 and Appendix Table 1). Additionally, a gravity model (the probability of an agent going to each store was inversely proportional to the agent’s distance from the store) determined which food source each agent may go to each day. Comparing the resulting frequencies with real world data from NHANES 2010–2012 helped validate this model (Table 1 and Appendix Table 2).
Statistical Analysis
In VPOP, each scenario was simulated 100 times, with each simulation lasting for 365 days x 7 years. Results for each scenario include the variation observed over the course of the 100 simulations. Each simulation followed a cohort of children aged 11 years (6,784 adolescents in Baltimore, 5,497 in San Francisco, and 20,171 in Philadelphia) through age 18 years. Children aged 11 years were examined because this is a pivotal time when most children start secondary school, begin making more autonomous dietary decisions, and become more vulnerable to rapid weight gain.23 The various point of purchase SSB warning label intervention scenarios are compared against the baseline, no intervention scenario. Probabilistic sensitivity analyses were performed and involved randomly sampling the values of each parameter from parameter-specific distributions. A Welch’s t-test was performed to determine statistical significance. All simulations and data analysis was conducted in 2016 and 2017.
In addition to the baseline scenario where no point of purchase SSB warning labels were implemented, sensitivity analyses were performed on the following parameters:
Warning label efficacy
As recent studies estimate that warning labels may decrease the frequency of SSB purchases by 6%–19%, the immediate effect of warning labels when present in an SSB retailer was varied from a more conservative 4% to 12%.6–10 An 8% decrease in SSB purchase frequency was used in subsequent sensitivity analyses and tests of alternative policy roll-out strategies. Consumers purchasing SSBs in a store that did not display a warning label were not impacted by warning labels.
Illiteracy rates
Scenarios were tested in which the labels had no effect on illiterate adolescents because the warning label requires a basic reading level to understand (Appendix Figure I shows a sample warning label). The illiteracy rate was varied from 0% to 49%, based on 2015 reports from the National Center for Education Statistics that 49% of eighth grade students in Baltimore, 30% in San Francisco, and 42% in Philadelphia had below basic reading level.24–26
Compliance of food retailers
For both supermarket and corner stores, proportion of stores complying with the warning label policy was varied from 50% to 100%.
SES
Scenarios in which warning label efficacy was lower for adolescents of low SES, (i.e. those living in households of income below the U.S. poverty line were tested).27 The efficacy of warning labels on low-SES agents were varied from 0% to 33%.
Compensatory eating
Agents who do not consume SSBs because of the warning label compensate between 0% and 75% of the calories from SSBs.28,29
The model was able to recreate overweight and obesity prevalence distributions for the Baltimore (27.5% vs 25.8% observed for children aged 6–18 years),30 San Francisco, (34.7% vs 31.7% for children aged 10–15 years),31 and Philadelphia (40.2% vs 40.7% for children aged 6–17 years).32 Table 1 provides additional validation information. Note that for each validation run, the age range of the cohort in the model was expanded to match that of the age range for the data used for validation. The model generated population level BMI distributions that were comparable to the 2014 California Health Interview Survey and the National Health Interview Survey (NHIS).33,34 For example, in the model 5.2% of the Baltimore population was between tenth and 20th BMI percentile, (compared to 5.57% in the Northeast region of NHIS); 14.4% between 60th and 70th BMI percentile (compared to 12.54%); and 8.21% between 97th and 100th BMI percentile (compared to 8.2%). In San Francisco, 4.37% of the population was below the tenth BMI percentile (compared to 4.09% in 2014 California Health Interview Survey), 11.76% between 70th and 80th BMI percentile (compared to 13.12%) and 9.93% between 90th and 95th BMI percentile (compared to 8.08%). In Philadelphia, 4.73% were below the tenth BMI percentile (compared to 3.1% in the Northeast region of NHIS), 10.63% between 60th and 70th BMI percentile (compared to 12.54%) and 16.83% in between the 80th and 90th BMI percentile (compared to 15.33%; Appendix Figure 2). Additionally, validation runs showed that the daily average caloric intake from SSBs for the baseline model were comparable to reported data (123.6 for San Francisco, 134.25 for Baltimore, and 132.45 for Philadelphia compared to the reported national average of 155 calories).35
RESULTS
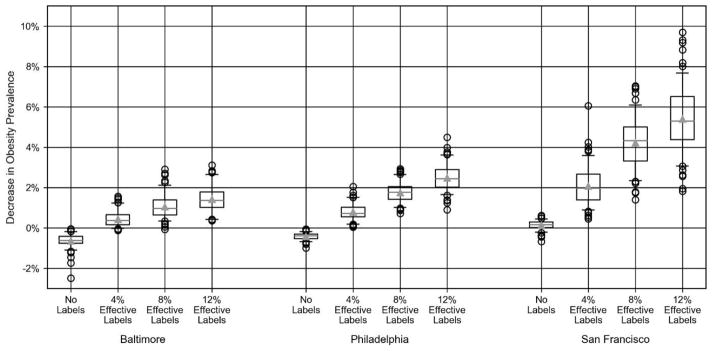
Universal application of SSB warning labels reduces obesity prevalence up to 4.08%. With an SSB warning label policy implemented at all retailers and a warning label efficacy of 8%, multiple measures of overweight and obesity decreased across all three cities in comparison with no intervention (Appendix Table 3). The obesity prevalence across the cohort was reduced by 1.69% (95% CI=0.97, 2.75, p<0.001) in Baltimore; 4.08% (95% CI=2.2, 5.96, p<0.001) in San Francisco; and 2.17%(95% CI=1.42, 3.07, p<0.001) in Philadelphia (Figure 2). Numbers were also markedly reduced in the overweight category: a reduction of 1.39% (95% CI%=0.49, 3.59, p<0.001) in Baltimore; 3.1% (95% CI%=0.97, 5.2, p<0.001) in San Francisco; and 0.36% (95% CI=1.39, 0.83, p<0.001) in Philadelphia. The warning labels also reduced the mean BMI for the obese population by 0.25 kg/m2 (95% CI= −1.7, 1.17, p<0.001) in Baltimore, 0.2 kg/m2 (95% CI= −0.69, 0.5, p<0.001) in San Francisco, and 0.18 kg/m2 (95% CI= −0.97, 0.46, p<0.001) in Philadelphia.
Figure 2.
Decrease in obesity prevalence across cities.
Different scenarios varied the warning label efficacy from 4% to 12% (Figure 3, Appendix Table 3). Even with the efficacy cut in half to 4%, implementing warning labels at all SSB retailers still reduced mean BMI for the obese population by 0.09 kg/m2 (95% CI= −1.75, 1.53, p<0.001) and obesity prevalence by 1.08% (95% CI= −1.87, −0.62), p<0.001) in Baltimore (Appendix Table 3). Some scenarios (e.g., 4% efficacy in San Francisco) led to increases in overweight prevalence, because more obese individuals moved into the overweight category than overweight individuals moving into the normal weight category. When looking instead at the combined number of overweight or obese individuals, the value is reduced by 0.47% (95% CI= −1.47, 0.12, p<0.001; Appendix Table 3).
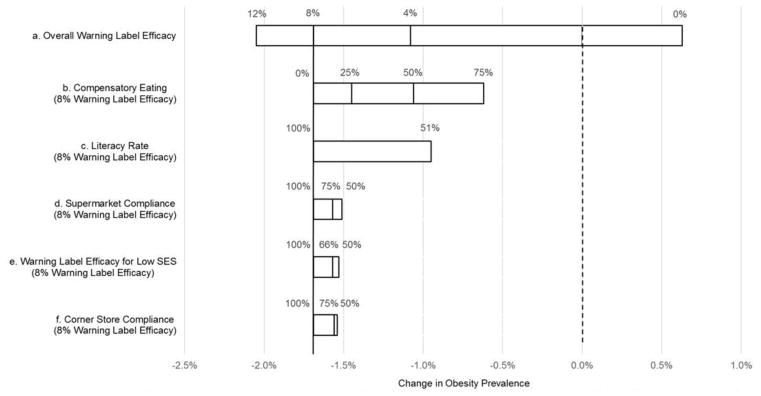
Figure 3.
Comparing the impact of key model variables on change in obesity prevalence in Baltimore City.
Notes: This figure summarizes the sensitivity analyses, i.e., investigating how varying different unknown factors affects the change in obesity prevalence for Baltimore City. Each factor analyzed is represented by a horizontal bar, where the width of each bar represents the range of impact on obesity prevlance across a range of values for that factor (listed above the bar). Additional lines on the bar represent mean obesity prevalence from intermediate factor values. The dotted line marks 0% change in obesity prevalence, or the change in obesity prevalence at the beginning of each scenario.
Studies have shown that low literacy may impair comprehension and thus efficacy of warning labels.36 Figure 3 and Appendix Table 3 show how reducing the literacy rate of Baltimore adolescents from 100% to 51% increased SSB consumption by 0.033 points (95% CI=0.16, 0.46, p<0.001), and obesity prevalence from −1.69% (95% CI= −2.75, −0.97, p<0.001) to −0.95 (95% CI= −1.93, 0.09, p<0.001). The simulations demonstrate that while reduced, the health benefits persist in low literacy simulations even with a 4% warning label efficacy (Appendix Table 3).
The overall effects on obesity and BMI largely remained after reducing the compliance of different types of stores (Figure 3 and Appendix Table 3). For example, decreasing levels of compliance at supermarkets to 50% in Baltimore, resulted in reduced obesity prevalence (1.54% decrease, 95% CI= −2.65, −0.78, p<0.001), overweight prevalence (0.77% decrease, 95% CI= −2.79, 0.84, p<0.001), and population BMI (0.21 decrease, 95% CI= −0.52, 0.11, p<0.001).
Reduced efficacy on low-SES adolescents has limited effect on overall population health impact. After reducing the warning label efficacy 33%–50% for low-SES adolescents, declines in SSB consumption, overweight and obesity prevalence, and BMI were observed. Appendix Table 3 and Figure 3 also show how increased compensatory eating reduced warning label impact.
DISCUSSION
The study found that SSB warning labels can reduce SSB consumption, obesity/overweight prevalence, and BMI among adolescents. Although SSB warning labels alone are not enough to curb the obesity epidemic, the results are a first step in better understanding ultimate impact of SSB warning labels. A key finding is that SSB warning labels can have a positive impact over a wide variety of circumstances, including those that significantly reduce the label’s efficacy, such as when the efficacy dips as low as 4%, the label has no effect on children who don’t read at a basic level, or significant increases in compensatory eating occur.
San Francisco experienced the largest obesity prevalence reduction whereas Baltimore City experienced greater reductions in overweight and obesity prevalence (Figure 2), which may be due in part to differences in starting BMI distributions (Appendix Figure 2). Should a city not be able to implement the policy in all food retailers, supermarkets would be the most impactful subset of retailers to target (Appendix Table 3). For Baltimore City, nearly half of the SSB warning label impact was retained when targeting only supermarkets. Although studies have shown supermarket availability and access may vary in high- versus low-income neighborhoods, 90% of low-income and food-insecure households report shopping for household groceries at supermarkets and supercenters.37,38 Supermarket purchases comprise the majority of available food at homes, influencing, in turn, adolescent meal and snacking options. Monitoring compliance in just supermarkets versus all stores would likely be less costly.
Sensitivity analysis demonstrated that besides warning label efficacy, literacy rates had the largest effect on the policy’s impact, primarily because of the assumption that warning labels would have no effect on those below a basic reading level. However, this assumption may not necessarily be correct, especially when warning labels have more basic language and clear graphics. Moreover, those who can read the labels could potentially inform those who cannot. Therefore, designing labels easily understandable by all may be worthwhile. Additionally, the label efficacies used in the simulation experiments came from the limited available studies.6–10 As was demonstrated with tobacco warning labels, label enhancements (e.g., pictures of well-known people or memorable designs) or pairing other interventions (e.g., campaigns, menu labels, advertisements) could further increase label efficacy.39,40 Moreover, SSB warning labels could raise general attention to SSB consumption, which then could recursively enhance the labels’ efficacy. However, because combining interventions can have complex effects, future studies to determine the nature of the interactions among interventions and simulation experiments could help better understand the impact of combining interventions and choose the optimal combinations.
Limitations
All models are simplifications of reality and cannot include all possible factors affecting the impact of an SSB warning label policy. The simulation experiments did not account for potential reductions in warning label efficacy over time, in turn, reducing its impact. The experiments assumed that families would primarily stock their home refrigerators from supermarkets, which would favor those scenarios in which labels were used in supermarkets but work against those scenarios in labels were not used in supermarkets. This study assumed point of purchase labels would have the same efficacy, regardless of the store type or placement within the store, which could either overestimate (e.g., if the labels are not as prominently displayed) or underestimate (e.g., if the labels are displayed prominently) the impact. The experiments did not account for the impact of other concomitant interventions (e.g., menu labels or advertisements), which could underestimate impact if synergistic. Finally, the economic impact on store owners and other decision makers was not examined.
CONCLUSIONS
This study shows how implementing SSB warning labels can reduce obesity and overweight prevalence among adolescents in three cities, quantified the potential impact, and demonstrated how different roll-out strategies and factors may affect this impact. All of this provides important information for decision makers considering such a policy. Though taxes have been modeled to have a greater influence on consumption behavior, the empirical evidence is inconsistent and the tax may disproportionately burden the low-SES population.41 Because the impact is quite sensitive to warning label efficacy, researchers, policy makers, and decision makers may want to develop ways of enhancing label efficacy (e.g., adding visuals and basic language, making the label more prominent and coupling the label with other interventions).
Supplementary Material
Acknowledgments
The project described was supported by the Global Obesity Prevention Center and from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research. This project is also funded by NICHD via grant U01HD086861 and the Agency for Healthcare Research and Quality via grant R01HS023317. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD, Agency for Healthcare Research and Quality, or Office of Behavioral and Social Sciences Research. This study was approved by the Johns Hopkins Bloomberg School of Public Health IRB (IRB #00006667). None of the study sponsors had any role in the study design, collection, analysis, and interpretation of data, writing the report, nor the decision to submit the report for publication.
Footnotes
No financial disclosures were reported by the authors of this paper.
Author contributions are as follows: Bruce Y. Lee provided expert guidance and leadership throughout the project, involved in each stage of model development, data analysis, and writing the manuscript. Marie Ferguson focused on developing and parameterizing the model, analyzing output and writing the manuscript. Daniel Hertenstein focused on programming the model, running simulations, analyzing output, and contributing to manuscript writing. Atif Adam focused on parameterizing the model, analyzing output, and contributing to manuscript writing. Eli Zenkov focused on programming the model, providing support for synthetic population used in the model, data analysis and analyzing output, and contributing to manuscript writing. Peggy I. Wang focused on developing analyzing output, developing figures, and contributing to manuscript writing. Michelle S. Wong focused on developing the model and contributing to manuscript writing. Yeeli Mui focused on developing initial conceptual model and contributing to manuscript writing. Joel Gittelsohn provided expert guidance on appropriate experimental scenarios and various aspects of model design, and contributed to manuscript editing. Shawn T. Brown provided expert guidance and leadership throughout the project, involved at each stage of model development, parameterizing the model, running simulations, programming, data analysis, and writing the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Della Torre SB, Keller A, Depeyre JL, Kruseman M. Sugar-sweetened beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet. 2016;116(4):638–659. doi: 10.1016/j.jand.2015.05.020. https://doi.org/10.1016/j.jand.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 2.Stevens A, Hamel C, Singh K, et al. Do sugar-sweetened beverages cause adverse health outcomes in children? A systematic review protocol. Syst Rev. 2014;3:96. doi: 10.1186/2046-4053-3-96. https://doi.org/10.1186/2046-4053-3-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Graham WCK, Malhotra R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133(5):854–862. doi: 10.1542/peds.2014-0063. https://doi.org/10.1542/peds.2014-0063. [DOI] [PubMed] [Google Scholar]
- 4.Pomeranz JL. Advanced policy options to regulate sugar-sweetened beverages to support public health. J Public Health Policy. 2012;33(1):75–88. doi: 10.1057/jphp.2011.46. https://doi.org/10.1057/jphp.2011.46. [DOI] [PubMed] [Google Scholar]
- 5.Popova L. Sugar-Sweetened Beverage Warning Labels: Lessons Learned From the Tobacco Industry. J Calif Dent Assoc. 2016;44(10):633. [PMC free article] [PubMed] [Google Scholar]
- 6.Roberto CA, Wong D, Musicus A, Hammond D. The Influence of Sugar-Sweetened Beverage Health Warning Labels on Parents’ Choices. Pediatrics. 2016;137(2):e20153185. doi: 10.1542/peds.2015-3185. https://doi.org/10.1542/peds.2015-3185. [DOI] [PubMed] [Google Scholar]
- 7.VanEpps EM, Roberto CA. The Influence of Sugar-Sweetened Beverage Warnings: A Randomized Trial of Adolescents’ Choices and Beliefs. Am J Prev Med. 2016;51(5):664–672. doi: 10.1016/j.amepre.2016.07.010. https://doi.org/10.1016/j.amepre.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing sugar-sweetened beverage consumption by providing caloric information: how black adolescents alter their purchases and whether the effects persist. Am J Public Health. 2014;104(12):2417–2424. doi: 10.2105/AJPH.2014.302150. https://doi.org/10.2105/AJPH.2014.302150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bleich SN, Herring BJ, Flagg DD, Gary-Webb TL. Reduction in purchases of sugar-sweetened beverages among low-income black adolescents after exposure to caloric information. Am J Public Health. 2012;102(2):329–335. doi: 10.2105/AJPH.2011.300350. https://doi.org/10.2105/AJPH.2011.300350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bollard T, Maubach N, Walker N, Mhurchu CN. Effects of plain packaging, warning labels, and taxes on young people’s predicted sugar-sweetened beverage preferences: an experimental study. Int J Behav Nutr Phys Act. 2016;13:95. doi: 10.1186/s12966-016-0421-7. https://doi.org/10.1186/s12966-016-0421-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Railsback SF, Grimm V. Agent-based and individual-based modeling: a practical introduction. Princeton University Press; 2011. [Google Scholar]
- 12.Lee BY, Brown ST, Cooley P, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16(3):252–261. doi: 10.1097/PHH.0b013e3181ce594e. https://doi.org/10.1097/PHH.0b013e3181ce594e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee BY, Brown ST, Korch GW, et al. A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine. 2010;28(31):4875–4879. doi: 10.1016/j.vaccine.2010.05.002. https://doi.org/10.1016/j.vaccine.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee BY, Adam A, Zenkov E, et al. Modeling the Economic and Health Impact of Increasing Children’s Physical Activity in the United States. Health Aff (Millwood) 2017;36(5):902–908. doi: 10.1377/hlthaff.2016.1315. https://doi.org/10.1377/hlthaff.2016.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee BY, Brown ST, Bailey RR, et al. The benefits to all of ensuring equal and timely access to influenza vaccines in poor communities. Health Aff (Millwood) 2011;30(6):1141–1150. doi: 10.1377/hlthaff.2010.0778. https://doi.org/10.1377/hlthaff.2010.0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BY, Brown ST, Cooley PC, et al. A computer simulation of employee vaccination to mitigate an influenza epidemic. Am J Prev Med. 2010;38(3):247–257. doi: 10.1016/j.amepre.2009.11.009. https://doi.org/10.1016/j.amepre.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wheaton WD, Cajka JC, Chasteen BM, et al. Synthesized population databases: A U.S. geospatial database for agent-based models. Research Triangle Park, NC: RTI Press; 2009. RTI Press Publication No. MR-0010-0905. https://doi.org/10.3768/rtipress.2009.mr.0010.0905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahmandad H. Human growth and body weight dynamics: an integrative systems model. PloS One. 2014;9(12):e114609. doi: 10.1371/journal.pone.0114609. https://doi.org/10.1371/journal.pone.0114609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among U.S. children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–e1614. doi: 10.1542/peds.2007-2834. https://doi.org/10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 20.CDC. Cutting Calories. Atlanta, GA: Division of Nutrition, Physical Activity, and Obesity; 2015. Healthy Eating for a Healthy Weight. [Google Scholar]
- 21.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol. 2013;1(2):97–105. doi: 10.1016/s2213-8587(13)70051-2. https://doi.org/10.1016/S2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ReferenceUSA. [Accessed October 6, 2017];Historical Business Database. 2011 www.referenceusa.com/Home/Home.
- 23.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59(5):955–959. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 24.2015 Reading Trial Urban District Snapshot Report. Baltimore City, Grade 8, Public Schools: U.S. Department of Education; 2015. [Google Scholar]
- 25.2015 Mathematics & Reading Assessments, District Trends. Philadelphia: U.S. Department of Education; 2015. [Google Scholar]
- 26.The Nation’s Report Card. U.S. Department of Education; 2015. 2015 Reading State Snapshot Report, California, Grade 8, Public Schools. [Google Scholar]
- 27.US. DHHS. 2015 Poverty Guidelines. Office of the Assistant Secretary For Planning and Evaluation; 2015. [Google Scholar]
- 28.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318. doi: 10.2105/AJPH.2009.160226. https://doi.org/10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.James A, Adams-Huet B, Shah M. Menu labels displaying the kilocalorie content or the exercise equivalent: effects on energy ordered and consumed in young adults. Am J Health Promot. 2015;29(5):294–302. doi: 10.4278/ajhp.130522-QUAN-267. https://doi.org/10.4278/ajhp.130522-QUAN-267. [DOI] [PubMed] [Google Scholar]
- 30.Baltimore City. Demographics and Social Determinants of Health (2005–2009) Maryland Department of Health and Mental Hygiene; [Google Scholar]
- 31.Babey SH, Wolstein J, Diamant AL, Bloom A, Goldstein H. Overweight and Obesity among Children by California Cities-2010. UCLA Center for Health Policy Research and California Center for Public Health Advocacy; 2012. [Google Scholar]
- 32.Lin B-H, Smith TA, Lee J-Y, Hall KD. Measuring weight outcomes for obesity intervention strategies: the case of a sugar-sweetened beverage tax. Econ Hum Biol. 2011;9(4):329–341. doi: 10.1016/j.ehb.2011.08.007. https://doi.org/10.1016/j.ehb.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 33.California Health Interview Survey. CHIS 2014 Adolescent Public Use File. UCLA Center for Health Policy Research; http://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx. [Google Scholar]
- 34.National Center for Health Statistics. 2014 www.cdc.gov/nchs/nhis/nhis_2014_data_release.htm.
- 35.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98(1):180–188. doi: 10.3945/ajcn.112.057943. https://doi.org/10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen J, Scott KA, Zhao Z, Moran TH, Bi S. Characterization of the feeding inhibition and neural activation produced by dorsomedial hypothalamic cholecystokinin administration. Neuroscience. 2008;152(1):178–188. doi: 10.1016/j.neuroscience.2007.12.004. https://doi.org/10.1016/j.neuroscience.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. https://doi.org/10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 38.Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B. Where Do Americans Usually Shop for Food and how Do They Travel to Get There?: Initial Findings from the National Household Food Acquisition and Purchase Survey. U.S. Department of Agriculture, Economic Research Service; 2015. [Google Scholar]
- 39.Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.037630. https://doi.org/10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- 40.Gallopel-Morvan K, Gabriel P, Le Gall-Ely M, Rieunier S, Urien B. The use of visual warnings in social marketing: The case of tobacco. J Bus Res. 2011;64(1):7–11. https://doi.org/10.1016/j.jbusres.2009.09.012. [Google Scholar]
- 41.Andreyeva T, Chaloupka FJ, Brownell KD. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Prev Med. 2011;52(6):413–416. doi: 10.1016/j.ypmed.2011.03.013. https://doi.org/10.1016/j.ypmed.2011.03.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.